Abstract
After unilateral total knee arthroplasty (TKA), osteoarthritis (OA) in the non-operated often progresses. The altered gait mechanics exhibited by patients after TKA increase the loading on the non-operated knee and predispose it to disease progression. Therefore, our objective was to examine the potentially detrimental changes in frontal plane kinetics and kinematics during walking in patients who underwent unilateral TKA. Thirty one subjects six months after TKA, forty four subjects one year after unilateral TKA and twenty control subjects were recruited. All subjects underwent three dimensional gait analysis. In the TKA groups, the non-operated knee had a higher adduction angle and higher dynamic loading, knee adduction moment and impulse, compared to the operated knee. This increased loading may be an underlying reason for OA progression in the non-operated knee. Measures of loading in the control knee did not differ from that of the non-operated knee in the TKA group, but the TKA group walked with shorter step length. Whilst the non-operated knee loading was not different from controls, there may be greater risk of cumulative loading in the non-operated knee of the TKA group given their shorter step length.
Introduction
Total knee Arthroplasty (TKA) is a common surgical procedure for end stage osteoarthritis (OA). More than 500,000 primary TKA procedures are performed each year in the United States with 97% of these procedures being performed for OA 1. By 2030, it is estimated that the annual incidence of primary TKA will be 3.5 million 2. Despite long term pain relief and patient satisfaction after TKA 3, many patients continue to have impairments and functional limitations when compared with age matched controls 4–6. One year after TKA, patients walk 15% slower than age matched individuals without known knee pathology 7. During the timed stair-climbing task, individuals after TKA had even greater functional limitations as evidenced by a 50% slower performance compared to age matched healthy individuals 7.
After unilateral TKA, OA progresses in a non-random fashion throughout the lower extremity joints. The knee contralateral to the operated knee is likely to show evidence of disease progression more so than the ipsilateral or contralateral hip or ankle 8. Within ten years of the index surgery, 40% of individuals undergo contralateral TKA 9. This laterality in disease progression suggests that mechanical factors might be involved in the disease progression.
Patients after TKA present with altered gait mechanics that developed prior to, or soon after surgery 10. Patients with TKA walk slower, have less knee flexion excursion during stance, demonstrate lower peak knee flexion during swing phase and present with altered sagittal plane knee moments compared to controls 11, 12. The altered gait mechanics may increase loading on the contralateral joint and expedite the disease progression.
The external knee adduction moment is a biomechanical measure of loading in the medial knee compartment, with higher knee adduction moment indicating higher knee medial compartment loading13. The external knee adduction moment is related to the incidence 14 severity of OA 15, and is the best predictor of OA progression16 Despite the importance of this measure, most gait evaluations of patients after TKA solely evaluated sagittal plane mechanics of the operated knee 11, 12. Examining the frontal plane mechanics of the operated knee is important to elucidate the potential effect of joint loading on component loosening 17. However biomechanical analyses should also investigate the mechanics of the non-operated knee. Examining the contralateral limb may reveal how surgery on the affected limb results in compensatory strategies in the non-operated side, which may subsequently result in altered joint loading and progression of OA in the non-operated knee.
The purpose of this study was to examine the changes in frontal plane kinetics and kinematics during walking after TKA. To explicate these frontal plane biomechanical changes, frontal plane kinematics and kinetics of the operated and non-operated knees were examined in persons who underwent TKA either 6 months or 1 year prior to testing and persons who were still largely asymptomatic in other lower extremity joints. In addition, we planned to determine how post-operative frontal plane kinetics and kinematics, as well as temporospatial variables differ from individuals without known knee pathology or knee pain. We hypothesized that 1) the non-operated knee will have greater knee adduction angle, moment and impulse during stance compared to the operated knee; 2) the non-operated knee of the one year TKA group will show a larger adduction angle, moment and impulse during stance compared to the six month TKA group; 3) the non-operated knee of subjects who underwent TKA will demonstrate greater knee adduction angle, moment and impulse during stance compared to controls.
Methods
Subjects
Thirty-one subjects 6 months after primary unilateral TKA and forty-four subjects 1 year after primary unilateral TKA participated in this study (Table 1). Subjects were recruited from a local group of orthopedic surgeons who perform tricompartmental cemented TKA with medial parapatellar approach and used either posterior stabilized or posterior cruciate retaining prosthesis. Subjects with TKA were excluded if they had surgery in the lower extremities other than the unilateral TKA, pain in the non-operated knee rated of more than 4 out 10 on a verbal analog scale, musculoskeletal involvement in the lower extremities or the spine that limited their physical function. Subjects were also excluded if they had neurological impairments, uncontrolled blood pressure, altered sensation in the feet, or body mass index (BMI) of more than 50.
Table 1.
Subjects characteristics [mean (standard deviation)]
| Variable | TKA 6 months (N=31) | TKA 1 year (N=44) | Control (N=20) |
|---|---|---|---|
| Sex (women/men) | 10/21 | 23/21 | 9/11 |
| Age (year) | 70.03(7.6) | 63.25(12.4) | 62.6(6.5) |
| Height (m) | 1.73(0.1) | 1.69(0.11) | 1.73(0.11) |
| Weight (kg) | 94.46(21.94) | 87.73(17.41) | 85.11(12.87) |
| BMI (kg/m²) | 31.5(6.3) | 30.5(4.5) | 28.8(5.1) |
The control group consisted of 20 subjects who reported no knee pain or injury (Table 1). The control group was matched by limbs to the TKA group. The TKA group consisted of 60% right TKA and 40% left TKA and this ratio was chosen for the limbs of the control group. The control subjects were excluded if they had surgery in the lower extremities, knee pain rated of more than 4 out 10 on a verbal analog scale, musculoskeletal involvement in the lower extremities or the spine that limited their physical function. Controls were also excluded if they had neurological impairment, uncontrolled blood pressure, altered sensation in the feet, or body mass index of more than 50. All subjects signed informed consent forms approved by the Human Subjects Review Board at the University of Delaware prior to participation.
Data Acquisition
Gait analysis was performed using a three dimensional, 8-camera motion capture system (VICON, Oxford Metrics, London, England) synchronized with two Bertec force platforms (Bertec Corp., Worthington, OH, USA). Sixteen millimeter spherical retro-reflective markers were placed bilaterally on iliac crest, greater trochanter, lateral femoral condyle, lateral malleolus, head of the 5th metatarsal, and two markers on the heel. Rigid thermoplastic shells with 4 markers were secured on the lower leg and thigh bilaterally. The pelvic motion was tracked using a rigid thermoplastic shell with 3 markers. Marker data were sampled at 120 Hz, while the force platforms data were collected at 1080 Hz. Data collection starts with standing calibration to identify joint centers and create segment impeded coordinate system. After standing calibration, subjects practiced walking until reaching a constant self-selected speed. The collected trials fell within 5% of the practiced speed with clear contact of only one foot on each force plate. Seven walking trials were collected for each subject.
Subjects also underwent clinical examination which included Knee Outcome Survey-Activities of Daily Living Scale (KOS-ADLS), knee flexion and extension range of motion (ROM), quadriceps muscle strength, Timed Up and Go Test (TUG), Stair Climbing Test (SCT), and Six-Minute Walk Test (6MW)18. Knee pain was also assessed on a scale from zero to 5 using a question from the KOS-ADLS questionnaire4. Zero indicated no pain while 5 indicated pain that prevents the subject from all daily activities.
Data Management
Marker trajectories were low pass filtered at 6 Hz, and force platforms data were filtered at 40 Hz using a second order phase-corrected butterworth filter. Knee Joint angles were calculated using Euler X-Y-Z sequence corresponding to flexion/extension, abduction/adduction then rotation sequences. Knee joint moments were calculated using three dimensional inverse dynamics and were expressed as external moments normalized to body mass and height. Kinematics and kinetics calculations were done using Visual 3D software (C-motion, Inc, Rockville, MD). Dependent variables were the peak knee adduction moment during the first 50% of stance (PKAM), knee adduction impulse, and knee frontal angle at PKAM. These variables were determined during the stance phase of the gait cycle which was time normalized with 0 being heel strike and 100% being toe off to create the group ensemble average. Spatial and temporal parameters were also computed.
Knee adduction impulse was calculated by integrating the knee adduction moment curve during stance phase. Knee adduction impulse was calculated because it has been suggested that peak knee moment and knee adduction impulse represent different aspects of medial knee joint loading 19, 20. Dependent variables were determined for every trial, then these points were averaged to create the subject’s mean and this mean was used in the analysis.
Statistical Analysis
A two-way mixed model analysis of variance (ANOVA) (group x side) was used to examine between subjects (6 months versus 1 year) and within subjects (operated versus non-operated) differences for the TKA subjects. A two-way mixed model ANOVA was used to examine group by side differences between the TKA group and the control group. For this analysis, the 6 month and 1 year TKA groups were grouped together and compared to the control group. Independent t-tests or paired t-tests were used to for post hoc testing when the interaction effect was significant. All statistical analyses were performed with SPSS 16. Significance level was set at 0.05.
Results
The 6 month TKA group was older than the 1 year TKA group (p=0.01), but no differences were detected between the two groups in height, weight, BMI or sex proportion (Table 1). When the 6 month and 1 year subjects from the TKA group were collapsed into one group, no differences were seen in age, height, weight, and BMI and sex proportion when compared to the control group (P>0.10) (Table 1).
For the analysis of the persons who underwent TKA, there was no group by side interaction (F 1,73 = 0.22, P=0.64) and no effect of group (F 1,73 = 0.48, P=0.49), but effect of side was significant (F 1,73 = 16.23, P<0.001) for the knee angle at PKAM, with the non-operated knee being more adducted than the operated knee (Table 2) (Fig. 1). PKAM showed no group by side interaction (F 1,73 = 0.061, P=0.81), no effect of group (F 1,73 = 0.81, P=0.37), but the effect of side was significant (F 1,73 = 13.22, P=0.001) with the non-operated knee having larger moment (Fig. 2). Knee adduction impulse showed no group by side interaction (F 1,73 = 0.72, P=0.4), no group effect of (F 1,73 = 0.91, P=0.34), but effect of side was significant (F 1,73 = 5.25, P=0.02) with the non-operated knee having larger impulse. Examining stance time revealed no group by side interaction (F 1,73 = 0.56, P=0.46), no effect of side (F 1,73 =0.85, P=0.36), but there was a significant group effect (F 1,73 = 6.1, P=0.016) with the 6 month group having longer stance time. Step length comparison revealed no group by side interaction (F 1,73 = 1.47, P=0.23), no group effect (F 1,73 = 0.01, P=0.91), but the effect of side was significant (F 1,73 = 5.81, P=0.02) with the operated limb having longer step length than the non-operated limb. Patients 6 months and 1 year after TKA walked with similar speed (independent t-test equal variance not assumed; t= 1.06, df = 48.66, P= 0.29).
Table 2.
Gait parameters [mean (standard deviation)]
| Variable | TKA 6 months | TKA 1 year | Control | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Operated | Non-operated | Operated | Non-operated | Operated | Non-operated | |
|
|
||||||
| knee angle at PKAM (degree) | –0.01 (4.16) | 2.96 (5.32) | 0.9 (4.69) | 3.28 (4.98) | 2.79 (5.07) | 2.33 (4.12) |
| PKAM (Nm/kg*m) | –0.28 (0.13) | –0.35 (0.14) | –0.30 (0.10) | –0.36 (0.12) | –0.41 (0.13) | –0.38 (0.13) |
| Adduction impulse ((Nm/kg*m)*s) | –0.11 (0.05) | –0.12 (0.05) | –0.09 (0.04) | –0.12 (0.05) | –0.14 (0.05) | –0.12 (0.03) |
| Stance time (second) | 0.70 (0.07) | 0.70 (0.07) | 0.66 (0.06) | 0.66 (0.05) | 0.65 (0.05) | 0.65 (0.06) |
| Step length (meter) | 0.69 (0.08) | 0.68 (0.08) | 0.69 (0.06) | 0.68 (0.06) | 0.75 (0.06) | 0.74 (0.07) |
| Walking speed (m/s) | 1.27 (0.19) | 1.31 (0.13) | 1.43 (0.14) | |||
Sign Convention: for knee angle, adduction is positive; for knee moment, external adduction moment is negative.
Figure 1.
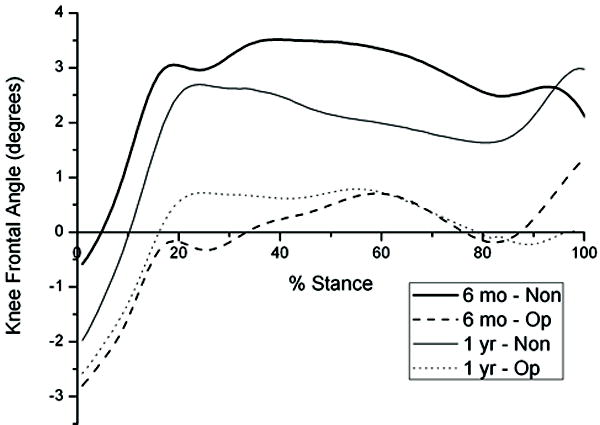
Average curves for knee frontal plane angle for the Operated (Op), non-operated (Non) knee of the 6 months (6 mo) and 1 year (1 yr) TKA groups.
Figure 2.
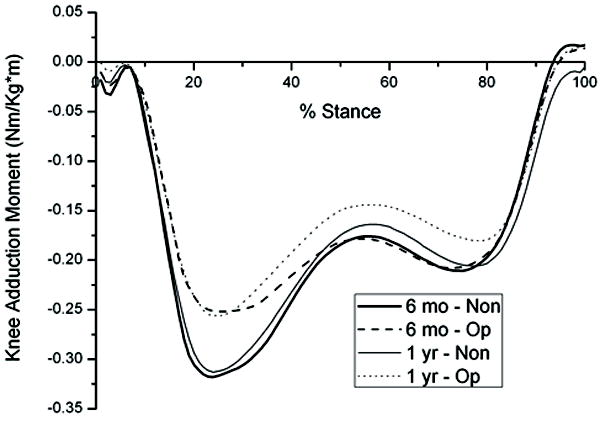
Average curves for knee adduction moment for the Operated (Op), non-operated (Non) knee of the 6 months (6 mo) and 1 year (1 yr) TKA groups.
The control group walked faster than the TKA group (P=0.001) (Table 2). Comparisons between the control group and the TKA group in knee angle at PKAM, PKAM and adduction impulse are presented without controlling for speed because using speed as a covariate did not change the results. For knee angle at PKAM, there was a group by side interaction (F 1,93 = 5.42, P=0.02), no effect of side (F 1,93 = 2.64, P=0.11), and no effect of group (F 1,93 = 0.51, P=0.48). Post hoc tests revealed no interlimb difference for the control group (P=0.56), no difference between control limbs and the operated limb (P=0.055) and non-operated limb (P=0.51), but in the TKA group the non-operated knee was more adducted than the operated knee (P<0.001) (Figure 3). There was a significant group by side interaction (F 1,93 = 6.79, P=0.01) and significant group effect (F 1,93 = 7.13, P=0.009) for PKAM, but there was no significant differences between limbs (F 1,93 = 0.82, P=0.36). Post hoc tests revealed no difference between control knees (P=0.25), between controls and the non-operated knee (P=0.25), but the operated knee had reduced moment compared to the non-operated knee and controls (P<0.001) (Figure 4). Examining knee adduction impulse revealed group by side interaction (F 1,93 = 4.88, P=0.03), group effect (F 1,93 = 5.91, P=0.017), but effect of side was not significant (F 1,93 = 0.003, P=0.95). Post hoc tests revealed no difference between control knees (P=0.25), between controls and the non-operated knee (P=0.59), but controls had larger impulse than the operated knee (P=0.001), and the non-operated knee had larger impulse than the operated knee (P=0.01). Step length comparisons showed no group by side interaction (F 1,93 = 0.07, P=0.79), no effect of side (F 1,93 = 3.38, P=0.07), but effect of group was significant (F 1,93 = 9.8, P=0.002) with the control group having longer step length. Stance time showed no group by side interaction (F 1,93 = 0.18, P=0.67), no effect of side (F 1,93 = 1.48, P=0.23), and no effect of group (F 1,93 = 2.86, P=0.09).
Figure 3.
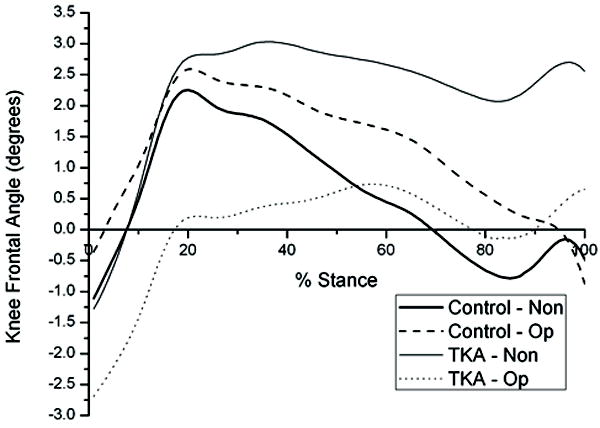
Average curves for knee frontal plane angle for the non-operated (Non) and operated (Op) limbs of the control and TKA groups.
Figure 4.
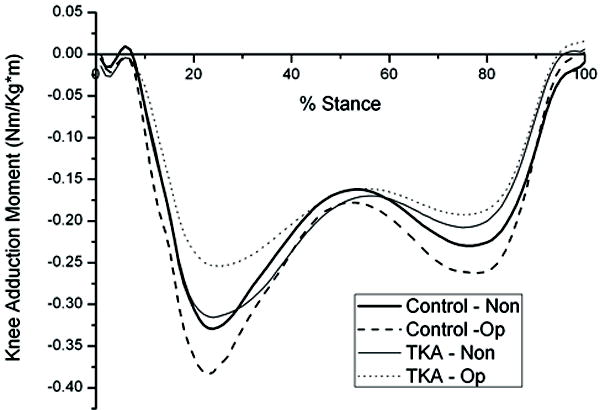
Average curves for knee adduction moment for the non-operated (Non) and operated (Op) limbs of the control and TKA groups.
Discussion
The results of this study support our hypothesis that the non-operated knee would show larger knee adduction angle and dynamic loading during stance compared to the operated knee. The non-operated knee in both TKA groups, 6 months and 1 year, showed larger knee adduction angle at PKAM, larger peak knee adduction moment and larger adduction impulse. Higher peak knee adduction moment and adduction impulse indicate higher dynamic loading experienced by the non-operated knee and that would place the non-operated knee at high risk for OA incidence and progression 14, 16. Knee adduction angle during stance has been shown to be related to dynamic loads during gait with higher adduction angles associated with higher dynamic loads 21. Static knee adduction alignment has been shown to increase the odds of OA progression by four fold 22. With greater knee adduction angle, moment, and impulse during stance, the non-operated knee is subjected to higher loads after TKA. This increased loading may be an underlying biomechanical reason for the non-random progression of OA in the contralateral knee and the high incidence rate of contralateral TKA.
Our second hypothesis was that the non-operated knee of one year TKA group will show larger adduction angle and dynamic loading during stance compared to the six month TKA group. We believed that knee dynamic loading will increase over time and that will be reflected in the loading measures, adduction moment and impulse, but the results of this study do not support this hypothesis. The age difference between the two TKA groups is not likely to influence our results since both groups walked with similar speed and both groups are similar in all clinical measures (Table 3). The non-operated knee did not show changes over the first post-operative year for knee adduction angle, PKAM and adduction moment. This suggests that loading of the non-operated knee did not change between 6 months and 1 year after TKA.. Peak adduction moment is associated with OA disease severity 15. Therefore, if OA progressed in the non-operated knee this progression would most likely be exemplified by an increase in the magnitude of the peak knee adduction moment. Since the magnitude of the adduction moment was the similar at 6 months and 1 year after surgery, this time frame might not be long to show signs of the expected OA progression in the non-operated knee 8, 9. Subjects in this study were also excluded if they reported maximal pain in the non-operative knee greater than 4 out of 10. As a result, subjects with more advanced disease in the non-operative knee may have been excluded from the analysis.
Table 3.
Clinical Measure [mean (standard deviation)
| Variable | TKA 6 months | TKA 1 year | Control | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Operated | Non-operated | Operated | Non-operated | Operated | Non-operated | |
|
|
||||||
| KOS | 0.86 (0.09) | 0.93 (0.06) | 0.85 (0.11) | 0.91 (0.12)# | 0.99(0.02) | 0.99(0.02)γ |
| Knee pain | 0.86 (0.70) | 0.50 (0.73) | 0.77 (0.96) | 0.65 (1.02)# | 0.1(0.31) | 0.05(0.23)γ |
| Flexion ROM (°) | 118 (8) | 131(9) | 120 (9) | 130(10)* | 134.4(7.46) | 135.95(6.85) |
| Extension ROM (°)§ | 0 (4) | –2 (3) | 0 (3.56) | –1 (3)* | –0.5(2.76) | –0.55(2.98) |
| Quadriceps strength (N/BMI) | 18.81 (6.65) | 21.86 (8.67) | 18.07 (7.8) | 21.09 (8.53) | 30.08(10.22) | 29.04(9.17) |
| TUG (seconds) | 8.21 (1.62) | 7.93 (1.84) | 6.55(1.19) | |||
| SCT (seconds) | 13.28 (3.14) | 12.51 (3.26) | 8.85(1.37) | |||
| 6MW (meter) | 563.74 (82.94) | 558.52 (88.71) | 685.23(112.12) | |||
Data from 26 subjects;
data from 27 subjects;
data from 19 subject;
negative values indicate knee hyperextension.
Our third hypothesis was that the non-operated knee of the TKA group will show higher dynamic loading and adduction angle during stance compared to controls. The results of this study partially support our hypothesis. The non-operated knee of the TKA group did not show higher adduction angle at PKAM compared to controls. It is important to note that the knee adduction angle at a single point where PKAM occurs does not capture the characteristics of the adduction angle over the whole stance phase (Fig. 3). The non-operated limb remains substantially more adducted after peak adduction angle, while the operated limb and control limbs move into a more abducted position. The adduction angle from the operated limb and control limbs demonstrate a biphasic pattern of both adduction and abduction, while the non-operated limb remains in adduction throughout the stance cycle. Measuring adduction angle at a discrete time point may not be truly reflective of the medial versus lateral joint loading that occurs in the knee joint throughout the stance phase.
Measures of loading were not different between the control knee and the non-operated knee. If these measures were analyzed without examining differences in temporospatial parameters between groups, it would be concluded that patients after TKA load their non-operated knee similar to the control subjects. However, in light of the differences between groups in step length, this conclusion may not be justified. Subjects in the TKA group walked with shorter step length compared to the control group and tended to have a longer stance time, particularly 6 months after TKA. The TKA group will take more steps to cover the same distance compared to the control group. With increasing the number of steps and duration of the step, the exposure of the TKA group to repetitive loading will increase compared to the control group. Assuming similar amount of daily activity between groups, the daily exposure of the TKA group to the adduction moment will be higher and this might put the non-operated knee at a higher risk for OA initiation and progression23. Measurement of the amount of daily activity of the control and TKA groups is needed to support this argument.
In this study, the control and non-operated knees had higher peak knee adduction moment and adduction impulse compared to the operated knee. Previous comparisons of the adduction moment between the operated knee after TKA and control knees are conflicting24–26. Milner and O’Bryan compared peak knee adduction moment of the operated knee and the non-operated knee of subjects after TKA to a control group 25. They reported higher moment in the non-operated knee compared to both the operated and control knees while no difference was found between the operated and control knee. In our study, no difference was found in adduction moment between the non-operated knee and the control knee. Excluding patients with symptomatic non-operated knees and testing our subjects early after surgery, 6 months or 1 year, compared to Milner’s and O’Bryan’s could explain differences between both reports.
Altered walking pattern and higher knee loading demonstrated by the TKA group in this study could not be attributed to poor clinical outcomes achieved by this cohort (Table 3). The TKA cohort in this study achieved clinical outcomes comparable to the best reported outcomes after TKA7, 27–29. They had good self-report of function, functional knee ROM, minimal knee pain, good quadriceps strength, and excellent functional performance.
Several limitations exist with this study. The cross-sectional nature of the study prevents any cause and effect inference from the data. However, using the cross-sectional design we could provide evidence of abnormal movement and loading patterns in subjects after TKA compared to age matched controls. Subjects in this study were only tested 6 months or 1 year after TKA and examination of patients later in the post-operative period may reveal different or more dramatic differences in frontal plane kinetics, particularly because knee strength on the non-operated limb begins to decline 1 year after TKA and by 3 years strength and pain in the non-operated limb are the best determinants of functional ability4, 30 In this study, we did not control for the subjects’ footwear which might influence the results. However, most of the subjects wore the same general type of footwear, so we believe that not controlling footwear did not greatly influence our results. In addition, this study lacks pre-operative gait data, which precludes the examination of how surgical intervention affected frontal plane mechanics. To have a complete picture of how TKA affects loading in the non-operated knee, pre-operative loading should also be quantified. In future studies, we are planning to collect data before surgery and to follow-up subjects after surgery to examine the effect of surgery on the operated and non-operated knee mechanics.
In summary, the non-operated knee of the TKA group had higher knee adduction angle, and dynamic loading compared to the operated knee indicating higher loading in the non-operated knee. This increased loading may be an underlying reason for OA progression in the non-operated knee. Measures of loading in the control knee did not differ from that of the non-operated knee in the TKA group, but the TKA group walked with shorter step length. Whilst the non-operated knee loading was not different from controls, there may be greater risk of cumulative loading in the non-operated knee of the TKA group given their shorter step length.
Acknowledgments
This study was supported by NIH grants (P20RR016458, S10RR022396) and a scholarship from King Saud University to Mr. Alnahdi.
Contributor Information
Ali H Alnahdi, Graduate Program in Biomechanics and Movement Science, University of Delaware, 301 McKinly Lab, Newark, DE 19716; Rehabilitation Sciences Department, College of Applied Medical Sciences, King Saud University, Riyadh, Saudi Arabia.
Joseph A Zeni PT, Department of Physical Therapy; University of Delaware, 301 McKinly Lab, Newark, DE 19716.
Lynn Snyder-Mackler, Department of Physical Therapy; University of Delaware, 301 McKinly Lab, Newark, DE 19716.
References
- 1.Jacobs JJ. The burden of musculoskeletal diseases in the United States : prevalence, societal and economic cost. American Academy of Orthopaedic Surgeons; Rosemont, IL: 2008. [Google Scholar]
- 2.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of Primary and Revision Hip and Knee Arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 3.Loughead JM, Malhan K, Mitchell SY, Pinder IM, McCaskie AW, Deehan DJ, Lingard EA. Outcome following knee arthroplasty beyond 15 years. The Knee. 2008;15:85–90. doi: 10.1016/j.knee.2007.11.003. [DOI] [PubMed] [Google Scholar]
- 4.Farquhar S, Snyder-Mackler L. The Chitranjan Ranawat Award: The Nonoperated Knee Predicts Function 3 Years after Unilateral Total Knee Arthroplasty. Clin Orthop Relat Res. 2009;468:37–44. doi: 10.1007/s11999-009-0892-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Huang CH, Cheng CK, Lee YT, Lee KS. Muscle strength after successful total knee replacement: a 6- to 13-year followup. Clin Orthop Relat Res. 1996;328:147–154. doi: 10.1097/00003086-199607000-00023. [DOI] [PubMed] [Google Scholar]
- 6.Noble PC, Gordon MJ, Weiss JM, Reddix RN, Conditt MA, Mathis KB. Does total knee replacement restore normal knee function? Clin Orthop Relat Res. 2005;431:157–165. doi: 10.1097/01.blo.0000150130.03519.fb. [DOI] [PubMed] [Google Scholar]
- 7.Walsh M, Woodhouse LJ, Thomas SG, Finch E. Physical impairments and functional limitations: a comparison of individuals 1 year after total knee arthroplasty with control subjects. Phys Ther. 1998;78:248–258. doi: 10.1093/ptj/78.3.248. [DOI] [PubMed] [Google Scholar]
- 8.Shakoor N, Block JA, Shott S, Case JP. Nonrandom evolution of end-stage osteoarthritis of the lower limbs. Arthritis Rheum. 2002;46:3185–3189. doi: 10.1002/art.10649. [DOI] [PubMed] [Google Scholar]
- 9.McMahon M, Block JA. The risk of contralateral total knee arthroplasty after knee replacement for osteoarthritis. J Rheumatol. 2003;30:1822–1824. [PubMed] [Google Scholar]
- 10.Smith AJ, Lloyd DG, Wood DJ. Pre-surgery knee joint loading patterns during walking predict the presence and severity of anterior knee pain after total knee arthroplasty. Journal of Orthopaedic Research. 2004;22:260–266. doi: 10.1016/S0736-0266(03)00184-0. [DOI] [PubMed] [Google Scholar]
- 11.McClelland JA, Webster KE, Feller JA. Gait analysis of patients following total knee replacement: A systematic review. The Knee. 2007;14:253–263. doi: 10.1016/j.knee.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 12.Milner CE. Is gait normal after total knee arthroplasty? Systematic review of the literature. J Orthop Sci. 2009;14:114–120. doi: 10.1007/s00776-008-1285-8. [DOI] [PubMed] [Google Scholar]
- 13.Zhao D, Banks SA, Mitchell KH, D’Lima DD, Colwell CW, Jr, Fregly BJ. Correlation between the knee adduction torque and medial contact force for a variety of gait patterns. J Orthop Res. 2007;25:789–797. doi: 10.1002/jor.20379. [DOI] [PubMed] [Google Scholar]
- 14.Baliunas AJ, Hurwitz DE, Ryals AB, Karrar A, Case JP, Block JA, Andriacchi TP. Increased knee joint loads during walking are present in subjects with knee osteoarthritis. Osteoarthritis and Cartilage. 2002;10:573–579. doi: 10.1053/joca.2002.0797. [DOI] [PubMed] [Google Scholar]
- 15.Sharma L, Hurwitz DE, Thonar EJ, Sum JA, Lenz ME, Dunlop DD, Schnitzer TJ, Kirwan-Mellis G, Andriacchi TP. Knee adduction moment, serum hyaluronan level, and disease severity in medial tibiofemoral osteoarthritis. Arthritis Rheum. 1998;41:1233–1240. doi: 10.1002/1529-0131(199807)41:7<1233::AID-ART14>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 16.Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61:617–622. doi: 10.1136/ard.61.7.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andriacchi TP. Dynamics of knee malalignment. Orthop Clin North Am. 1994;25:395–403. [PubMed] [Google Scholar]
- 18.Yoshida Y, Mizner RL, Ramsey DK, Snyder-Mackler L. Examining outcomes from total knee arthroplasty and the relationship between quadriceps strength and knee function over time. Clinical Biomechanics. 2008;23:320–328. doi: 10.1016/j.clinbiomech.2007.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Robbins SMK, Maly MR. The effect of gait speed on the knee adduction moment depends on waveform summary measures. Gait & Posture. 2009;30:543–546. doi: 10.1016/j.gaitpost.2009.08.236. [DOI] [PubMed] [Google Scholar]
- 20.Thorp LE, Sumner DR, Block JA, Moisio KC, Shott S, Wimmer MA. Knee joint loading differs in individuals with mild compared with moderate medial knee osteoarthritis. Arthritis Rheum. 2006;54:3842–3849. doi: 10.1002/art.22247. [DOI] [PubMed] [Google Scholar]
- 21.Barrios JA, Higginson JS, Royer TD, Davis IS. Static and dynamic correlates of the knee adduction moment in healthy knees ranging from normal to varus-aligned. Clinical Biomechanics. 2009;24:850–854. doi: 10.1016/j.clinbiomech.2009.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The Role of Knee Alignment in Disease Progression and Functional Decline in Knee Osteoarthritis. JAMA. 2001;286:188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 23.Robbins SM, Birmingham TB, Jones GR, Callaghan JP, Maly MR. Developing an estimate of daily cumulative loading for the knee: examining test-retest reliability. Gait Posture. 2009;30:497–501. doi: 10.1016/j.gaitpost.2009.07.118. [DOI] [PubMed] [Google Scholar]
- 24.Brugioni DJ, Andriacchi TP, Galante JO. A functional and radiographic analysis of the total condylar knee arthroplasty. J Arthroplasty. 1990;5:173–180. doi: 10.1016/s0883-5403(06)80237-8. [DOI] [PubMed] [Google Scholar]
- 25.Milner CE, O’Bryan ME. Bilateral frontal plane mechanics after unilateral total knee arthroplasty. Arch Phys Med Rehabil. 2008;89:1965–1969. doi: 10.1016/j.apmr.2008.02.034. [DOI] [PubMed] [Google Scholar]
- 26.Saari T, Tranberg R, Zügner R, Uvehammer J, Kärrholm J. Changed gait pattern in patients with total knee arthroplasty but minimal influence of tibial insert design: gait analysis during level walking in 39 TKR patients and 18 healthy controls. Acta Orthopaedica. 2005;76:253–260. doi: 10.1080/00016470510030661. [DOI] [PubMed] [Google Scholar]
- 27.Mizner RL, Petterson SC, Snyder-Mackler L. Quadriceps strength and the time course of functional recovery after total knee arthroplasty. Journal of Orthopaedic & Sports Physical Therapy. 2005;35:424–436. doi: 10.2519/jospt.2005.35.7.424. [DOI] [PubMed] [Google Scholar]
- 28.Petterson SC, Mizner RL, Stevens JE, Raisis L, Bodenstab A, Newcomb W, Snyder-Mackler L. Improved function from progressive strengthening interventions after total knee arthroplasty: A randomized clinical trial with an imbedded prospective cohort. Arthritis Rheum. 2009;61:174–183. doi: 10.1002/art.24167. [DOI] [PubMed] [Google Scholar]
- 29.Steffen TM, Hacker TA, Mollinger L. Age- and Gender-Related Test Performance in Community-Dwelling Elderly People: Six-Minute Walk Test, Berg Balance Scale, Timed Up & Go Test, and Gait Speeds. Phys Ther. 2002;82:128–137. doi: 10.1093/ptj/82.2.128. [DOI] [PubMed] [Google Scholar]
- 30.Zeni JA, Jr, Snyder-Mackler L. Most patients gain weight in the 2 years after total knee arthroplasty: comparison to a healthy control group. Osteoarthritis Cartilage. 2010;18:510–514. doi: 10.1016/j.joca.2009.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]


