Abstract
Objectives
The study examined the long-term course of posttraumatic stress disorder (PTSD) by analyzing rates of recurrence and the predictive value of comorbid psychiatric disorders and psychosocial functioning.
Methods
This study is based on diagnostic assessments administered at intake and subsequent follow-up interviews over a period of 15 years in a sample of 90 anxiety-disordered patients with comorbid PTSD who participated in the Harvard Brown Anxiety Research project (HARP). Kaplan–Meier life table analysis revealed a 0.20 probability of full remission during the 15 years of follow-up.
Results
Latent growth model (LGM) analysis revealed that the number of trauma exposures was a predictor of a worse course of PTSD but only during some intervals of the 15-year follow-up. Subjects with full social phobia were more likely to experience worsening of PTSD over time in comparison with subjects with less severe social phobia. Role functioning in the areas of household and employment was a significant predictor of a declining course of PTSD.
Conclusions
These findings revealed the dynamic nature of the predictive value of traumatic experiences, the deleterious effect of social phobia and the long term effect of psychosocial functioning on the course of PTSD. Implications for treatment planning and development of interventions for PTSD are discussed.
Keywords: PTSD, longitudinal studies, long-term course, clinical predictors of PTSD, social anxiety, psychosocial functioning
Introduction
Posttraumatic stress disorder (PTSD) is a common and chronic disorder with lifetime prevalence in the US ranging from 8.5 to 17.7% for women and 3.4 to 9.8% for men depending on the epidemiological survey [1-3]. Several prospective longitudinal studies have documented a chronic course of this disorder [4-5]. Although the course of PTSD can be chronic, many patients fully or partially recover within 3–6 months after exposure to trauma [6-7]. The only previous long term (14 years of follow-up) longitudinal prospective study of PTSD conducted with non-civilian populations [8] showed that combat exposure in Vietnam Veterans was the most salient risk factor for chronic PTSD and that recovery from PTSD was significantly related to perceived social support.
The current study examined the 15-year course of comorbid PTSD in a clinical sample of anxiety-disordered patients participating in the Harvard/Brown Anxiety Research Project (HARP), and in particular, the rates of recurrence of PTSD. The study also explored baseline and time-varying predictors of the recovery of PTSD, such as Axis I comorbidity: major depressive disorder (MDD), panic disorder with or without agoraphobia (PD-PDA), generalized anxiety disorder (GAD), and social phobia, and impairment in psychosocial functioning. These clinical variables have been proposed as significant predictors of the course of PTSD based on previous findings [9-11].
Methods
Subjects
HARP is a prospective, naturalistic, longitudinal, multicenter study of 711 adults with a current or past history of anxiety disorders. Subjects entered this study from over 30 clinicians’ practices at 11 different clinical treatment facilities in the New England area. These methods are described in detail elsewhere [12]. Inclusion criteria were that subjects must have been at least 18 years of age at intake and have had a past or current diagnosis of PD, PDA, GAD, or social phobia. Insufficient for inclusion but frequently seen as comorbid conditions were diagnoses of simple phobia, PTSD, obsessive-compulsive disorder, or anxiety disorder not otherwise specified. Exclusion criteria were the presence of an organic brain syndrome, a history of schizophrenia, or current psychosis within the six months before intake.
Intake and follow-up assessments
The present data were derived from a structured diagnostic interview administered at intake and subsequent follow-up interviews over a period of 15 years. The initial diagnostic evaluation assessed current and lifetime history of relevant psychiatric conditions, using a combination of the Structured Clinical Interview of DSM-III-R Non-Affective Disorder, Patient Version (SCID-P) [13], and the Research Diagnostic Criteria (RDC) Schedule for Affective Disorders-lifetime (SADS-L) [14]. Traumatic events at baseline were assessed using the SCID PTSD trauma probe. Participants were asked about lifetime traumatic events and were asked to identify their most stressful trauma. PTSD was assessed in response to that event. Participants were not reevaluated for new traumatic experiences at the follow-up interviews.
Follow-up interviews were conducted at six-month intervals for the first 2 years and annually thereafter using the Longitudinal Interval Follow-up Evaluation-Upjohn (LIFE-UP) [15] which is a structured interview that uses a change-point method with a three or six point psychiatric status rating (PSR) scale that is scored for each week of the follow-up interval. PTSD was assessed at each follow-up interval using a three-point psychiatric status rating (PSR) to identify if the participant met full (PSR 3) or partial DSM-III-R criteria (PSR 2) for PTSD. The other disorders were rated using a six-point rating. Psychosocial functioning was assessed using the LIFE-Up psychosocial functioning composite scores, of areas such as employment, household activities, relationship with friends and family and life satisfaction. Information regarding pharmacological treatment was collected directly from subjects’ reports at baseline. Because this was a naturalistic study, treatment was not controlled. Subjects sought treatment in their local areas.
Statistical analyses
Frequency counts for clinical and demographic variables were run for the 90 subjects who had either full criteria (n = 48) or less than full criteria (n = 5) PTSD at baseline, or who developed PTSD during follow-up (n = 37). To examine time to full remission over 15 years (each subject had at least 26 weeks and up to 780 weeks of data), survival analyses were conducted using the Kaplan–Meier life tables. Full remission was defined as 8 weeks at a PSR 1. To examine whether there was a linear trend in PTSD PSRs over 15 years and to evaluate the predictive value of baseline and time-varying variables, we conducted latent growth modeling (LGM) (proc mixed) analyses. Unlike conventional repeated measures analyses such as analysis of variance, LGM enables researchers to test for differences in developmental trajectories across time [16].
Demographic and clinical variables included gender, marital status, education, and age, number of traumatic experiences; DSM-III-R diagnoses of MDD, current diagnosis of alcohol abuse or dependence, drug abuse and dependence, number of anxiety disorders (GAD, PD, PDA, and Social Phobia) and psychosocial treatment participation. The time varying variables included the aforementioned disorders and LIFE psychosocial functioning ratings. The PSRs of the psychiatric diagnoses corresponded to the rates of PTSD PSRs 4 weeks prior. To examine whether a given PTSD course (PSRs) was getting better or worse over the 15 years, and whether there was a significant time by predictor effect of the time–varying variables, the mean PSR for PTSD was calculated every 6 months. Ratings of psychosocial functioning measures were taken a month prior to the follow-up interview. Separate models were run for each of the areas of functioning. To be included in the analysis, subjects were required to have at least two data points.
Results
Of the 90 subjects with a DSM III-R diagnosis of PTSD with at least two follow up data points in 15 years of follow-up, 69% were female, 40% were married, 70% had a least some college, and they had a mean age of 39.5 (SD = 12.55). Physical abuse was the most often reported trauma (32%), followed by rape (15.6%), war related trauma (11.1%), witnessing violence as a child (11.1%), assault (8.9%), witnessing violence as an adult (5.6%), and accidents (4.4%). In total, 56.7% of patients reported one type of trauma, 18.9% reported two, and 14.4% reported three or more. At intake, 50.0% of the patients had at least one comorbid anxiety disorder, 32.2% had two, and 12.2% had three. The most common comorbid Axis I disorder was panic with agoraphobia (47.8%) followed by GAD (33.3%) and social phobia (33. 3%). Four subjects did not have a comorbid anxiety disorder while seven (6.2%) were diagnosed with current alcohol abuse or dependence, 2 (2.2%) with drug abuse or dependence, and 37 (43.5%) had a PD. During the first month after the intake, 21.1% reported using SSRIs, 48.9% reported using benzodiazepines, and 64.7% reported participating in psychosocial treatment in the 12 months prior to the intake interview. At year 5 (n = 76), 46.1% of the subjects reported using SSRIs and 51.3% benzodiazepines; at year 10 (n = 61), 57.4% reported using SSRIs and 52.5% benzodiazepines, and at year 15 (n = 49), 65.3% reported using SSRIs and 63.3%, benzodiazepines.
Kaplan–Meier life tables analysis revealed a 0.20 probability of full remission during the 15 years of follow-up for the 90 subjects experiencing PTSD at the time of intake. Because only 13 patients recovered from their baseline episode, it was not feasible to examine probability of recurrence after the first recovery period.
Longitudinal LGM with baseline variables revealed a significant interaction effect (baseline predictors × time) on PTSD severity, of having a high number of traumas, F(30,1876) = 3.42, P< 0.001. Figure 1 shows that for most of the follow-up, a higher number of traumas was associated with higher PTSD PSRs. Subjects with three traumas or more reported a worsening of PTSD in comparison with subjects reporting one or two traumas; however, this relationship seems to be reversed in the last 4 years of the period: Subjects with more traumas showed improvement in PTSD symptoms in the last 4 years. Analyses over all time periods revealed that demographic variables and comorbid anxiety disorders, mood disorders, substance use disorders and psychosocial treatment participation did not have a significant relationship with PTSD PSRs.
Figure 1.
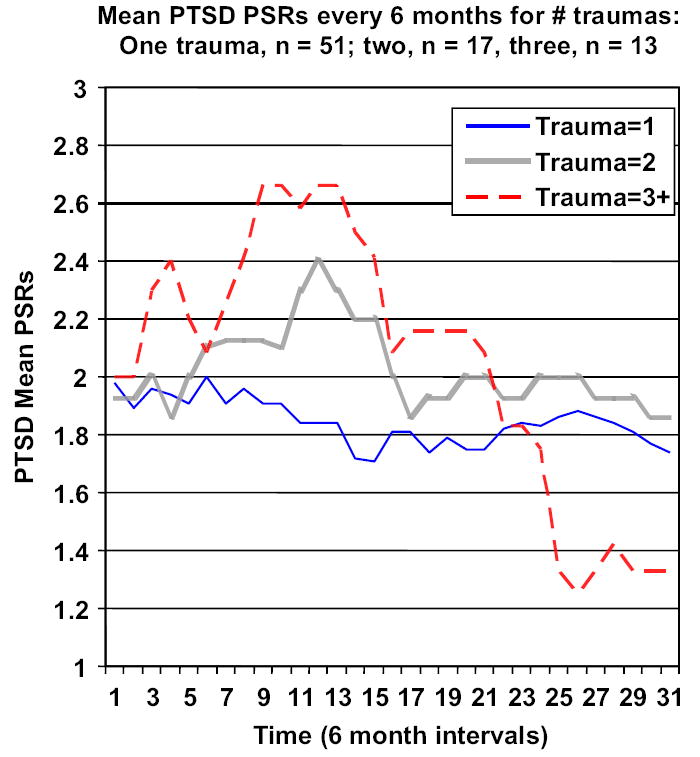
Growth model showing relationship between number of traumas and PTSD severity over 15 years.
Using longitudinal LGM separate analyses for each time-varying predictor (comorbid anxiety disorders, mood disorders, substance use disorder, and psychosocial functioning) revealed a significant interaction effect of social phobia, F(30,967) = 2.18, P< 0.001. Figure 2 shows that PTSD PSRs consistently increased (worsened) over time for those subjects with full criteria social phobia (PSRs 5 and 6), in comparison with those subjects who had limited social phobia symptoms (PSR 3 and 4) and with those who only meet criteria A (fear) (PSR 2), (n = 16), or did not have criteria (PSR 1).
Figure 2.
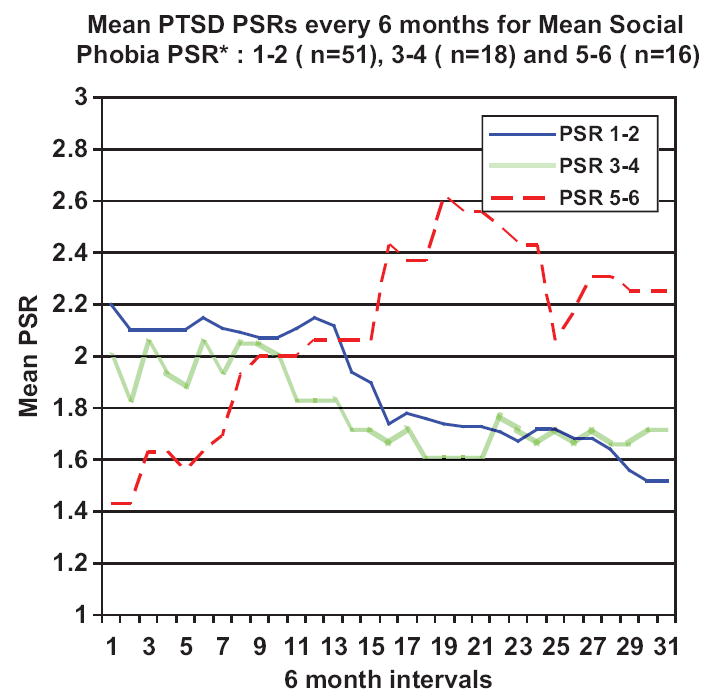
Time varying growth model showing relationship between social phobia and PTSD severities over 15 years. Social PSRs: 6 = meets all DSM-R criteria and the symptoms cause extreme impairment in functioning; 5 = meets DSM-II-R criteria for definite; 4 = meet all criteria excluding criteria E (interference or marked distress about having the phobia); 3 = meets criterion A (fear); fails more than 1 but less than all of criteria B, C, D, E, and F; 2 = meets criterion A (fear) and exclusionary criteria only; and 1 = no criteria.
In regard to psychosocial functioning, LGM revealed a significant time interaction effect of work and household functioning, F(15,617) = 2.63, P= 0.007 and F(15,897) = 2.21, P= 0.005, respectively. Ratings of unctioning in the area of employment were grouped in three categories as well: group 1, subjects showing no impairment, very good functioning; group 2, satisfactory, good, mild impairment; and group 3, poor, very poor functioning – severe impairment. Figure 3 shows that all subjects, regardless of level of functioning, showed a growing level of worsening in the PTSD course but subjects in group 3, moderate and severe impairment, had a trajectory with higher PTSD PSRs overtime compared to the other two groups, suggesting that lower functioning in employment functioning preceded PTSD decline. A similar trajectory was observed in household functioning (not shown).
Figure 3.
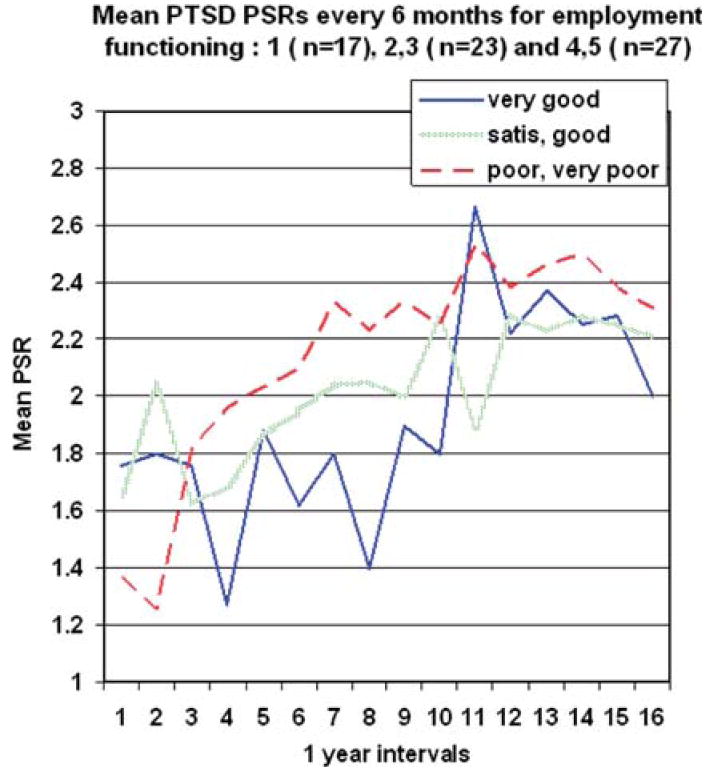
Time varying growth model showing relationship between psychosocial functioning (employment activities) and PTSD severities over 15 years.
Discussion
The present study is the first to examine the long-term course of PTSD for more than 14 years in a clinical sample of non-combat individuals using a longitudinal, prospective design. This study found that PTSD is a chronic disorder. The probability of PTSD remission over 15 years of follow up was low, 0.20. Of the initial 90, only 13 patients fully recovered. We found that having more than two traumas was a significant predictor of a worse course of PTSD. This finding is consistent with several studies [17-19]. For example, a community study showed that individuals exposed to more childhood traumas have greater risk for developing PTSD than those with fewer childhood traumas (20). A recent study with Rwandan refugees also showed that higher trauma exposure is associated with a lower probability of spontaneous remission from PTSD and with higher current and lifetime PTSD symptom severity [18]. However, in the HARP study, during the last four years of the follow-up period, subjects with a higher number of traumas showed an improvement in comparison with those who reported fewer traumatic events. Since the present study only assessed for trauma exposure at baseline and did not assess for new traumatic events over time, it is possible that new traumatic events during the follow-up period influenced the course of the disorder, given the long period of follow-up. We also found that that subjects who met full criteria for social phobia showed a worsening of PTSD symptoms over time, while subjects who reported a sub-threshold level of social phobia symptoms or with social phobia symptoms in remission showed an improvement of PTSD. PTSD and social phobia are frequently comorbid in studies using samples of civilians and non civilians [21-23]. Because both disorders share avoidant symptoms that may include avoidance of social interactions [24], the anxiety caused by social situations can exacerbate or perpetuate avoidant behaviors related to traumatic experiences. It is also possible that avoidance of new social interactions may also preclude individuals with PTSD from developing a stronger social supportive network that can help them alleviate their symptoms [25,26].
In regard to the predictive value of psychosocial functioning, current findings are consistent with a previous study covering a 2-year course of PTSD using data from the same project [9], and with a recent cross-sectional study using a national sample [27] that reported that PTSD was associated with greater past-month psychosocial dysfunction, as well as with an earlier study of a representative sample of individuals with full and partial PTSD [28]. These findings emphasize the need for treatments for PTSD that explicitly target psychosocial functioning as an outcome of treatment.
Because PTSD was a comorbid disorder, it is unclear how representative the data are for people who have PTSD as primary diagnosis. The study results also may not generalize to non-clinical samples, as almost all subjects were recruited through their mental health providers and were receiving psychopharmacological treatment at the time of intake. Attrition in the sample was moderate (43%), which was expected considering that this study covered 15-years of follow-up participation. It is possible that those subjects who left the study may have experienced worse anxiety symptoms than those who remained in the study and therefore the current results underestimate PTSD chronicity. Another limitation of the study is that it failed to assess whether patients were exposed to new traumatic events during the follow-up period. Since psychiatric disorders in this study were based on DSM-III-R guidelines, it is unknown whether findings would generalize to participants with DSM-IV based PTSD criteria, given that the more recent diagnostic criteria for PTSD has a more restrictive definition of trauma. Another limitation of the study is that we were unable to control for treatment due to the naturalistic nature of the study. Hence, the role of treatment in the course of comorbid PTSD was unknown. Treatment seeking has been associated with PTSD remission [1] however, another recent epidemiological study with prospective data revealed no relationship between treatment seeking at baseline (and at the follow up periods) with PTSD remission rates [29]. A previous HARP study did not find a relationship between treatment and the course of primary anxiety disorders, such as GAD, social and panic disorder [30]. Treatment bias effects may be significant in naturalistic studies given that patients with most severe symptomatology usually receive more aggressive treatments than those with less severe symptoms.
Being able to trace the relationship between several clinical variables in PTSD over a long-term period allowed us to see the complexity of the course of PTSD and have a better understanding of the dynamic nature of the predictive value of clinical variables on PTSD. Clinicians are encouraged to pay attention to the course of the disorder and to consider how variables may play different roles during the course of the disorder over time.
Key points.
PTSD is a chronic disorder. The probability of remission is low
Having more than one trauma is a significant predictor of having a worsening of PTSD over time
Patients with social phobia and PTSD may experience a worsening of PTSD symptoms if social phobia worsens as well
People with higher levels of impairment in areas of functioning such as household duties and employment may show a subsequent worsening of PTSD symptoms
Acknowledgments
The Harvard/Brown Anxiety Disorder Research Program (HARP) was supported by NIMH Grant MH51415. In the past, HARP received financial support from Wyeth-Ayerst Laboratories, through its Global Research Program on Anxiety and Depression, and Eli Lilly Laboratories. Dr Carlos Perez Benitez is supported by NIMH Grant MH080942. This study was conducted with the current participation of the following collaborators: M.B. Keller, M.D. (Chairperson); R.B. Weisberg, Ph.D.; R.L. Stout, Ph.D.; I.R. Dyck, M.P.H.; P. Leduc; B.F. Rodriguez, Ph.D.; C. Perez- Benitez, Ph.D.; B.A. Marcks; Ph.D; H.J. Ramsawh, Ph.D.; L.A. Uebelacker, Ph.D.; C. Beard, Ph.D.; A.S. Bjornsson, Ph.D.; N.J. Sibrava, Ph.D.; E. Moitra, Ph.D.; and, R.G. Vasile, M.D. The manuscript was reviewed by the Publication Committee of HARP and has its endorsement. The original principal and co-investigators included M.B. Keller, M.D. (Chairperson); J. Eisen, M.D.; E. Fierman, M.D.; R.M. Goisman, M.D.; I. Goldenberg, Psy.D.; G. Mallya, M.D.; A. Massion, M.D.; T. Mueller, M.D.; K. Phillips, M.D.; F. Rodriguez-Villa, M.D.; M.P. Rogers, M.D.; C. Salzman, M.D.; M.T. Shea, Ph.D.; G. Steketee, Ph.D.; R.L. Stout, Ph.D.; R.G. Vasile, M.D.; M.G. Warshaw, M.S.S., M.A.; R.B. Weisberg, Ph.D.; K. Yonkers, M.D.; and, C. Zlotnick, Ph.D. Additional contributions from: P. Alexander, M.D.; J. Cole, M.D; J. Ellison, M.D., M.P.H.; A. Gordon, M.D.; R. Hirschfeld Ph.D.; P. Lavori, Ph.D.; J. Perry, M.D.; L. Peterson; S. Rasmussen, M.D.; J. Reich, M.D., M.P.H.; J. Rice, Ph.D.; H. Samuelson, M.A.; D. Shera, M.S.; N. Weinshenker, M.D.; M. Weissman, Ph.D.; and, K. White, M.D.
Risa Weisberg receives grant funding from Pfizer Pharmaceuticals and in the past three years has served as a consultant for Sci Med and received honoraria from Astra Zeneca, Eli Lilly and company, and from Bristol Myers Squibb. Martin Keller: In the past three years, Dr. Keller has served as a consultant and received honoraria from CENERX, Forest Laboratories, Medtronic, Organon, Pfizer, Sierra Neuropharmaceuticals and Wyeth. He has received research grants from Pfizer and Wyeth. He has been on advisory boards for CENEREX, Forest laboratories, and Organon. No major stockholders.
Footnotes
Statement of Interest
Carlos I. Perez Benitez: The author reports no declaration of interests. Caron Zlotnick: Stock holder in Pfizer. Ingrid Dyck: The author reports no declaration of interests. Robert Stout: The author reports no declaration of interests. Erica Angert: The author reports no declaration of interests.
References
- 1.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52(12):1048–60. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- 2.McLean CP, Asnaani A, Litz BT, Hofmann SG. Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res. 2011;45(8):1027–1035. doi: 10.1016/j.jpsychires.2011.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Breslau N, Peterson EL, Poisson LM, Schultz LR, Lucia VC. Estimating post-traumatic stress disorder in the community: lifetime perspective and the impact of typical traumatic events. Psychol Med. 2004;34(5):889–98. doi: 10.1017/s0033291703001612. [DOI] [PubMed] [Google Scholar]
- 4.Peleg T, Shalev AY. Longitudinal studies of PTSD: overview of findings and methods. CNS Spectr. 2006;11(8):589–602. doi: 10.1017/s109285290001364x. [DOI] [PubMed] [Google Scholar]
- 5.Port CL, Engdahl B, Frazier P. A longitudinal and retrospective study of PTSD among older prisoners of war. Am J Psychiatry. 2001;158(9):1474–9. doi: 10.1176/appi.ajp.158.9.1474. [DOI] [PubMed] [Google Scholar]
- 6.Blanchard EB, Hickling EJ, Vollmer AJ, Loos WR, Buckley TC, Jaccard J. Short-term follow-up of post-traumatic stress symptoms in motor vehicle accident victims. Behav Res Ther. 1995;33(4):369–77. doi: 10.1016/0005-7967(94)00067-t. [DOI] [PubMed] [Google Scholar]
- 7.Rothbaum BO, Foa EB, Riggs DS, Murdock T, Walsh W. A prospective examination of post-traumatic stress disorder in rape victims. J Traumatic Stress. 1992;5(3):455–75. [Google Scholar]
- 8.Koenen KC, Stellman JM, Stellman SD, Sommer JF., Jr Risk factors for course of posttraumatic stress disorder among Vietnam veterans: a 14-year follow-up of American Legionnaires. J Consult Clin Psychol. 2003;71(6):980–6. doi: 10.1037/0022-006X.71.6.980. [DOI] [PubMed] [Google Scholar]
- 9.Zlotnick C, Warshaw M, Shea M, Allsworth J, Pearlstein T, Keller MB. Chronicity in posttraumatic stress disorder (PTSD) and predictors of course of comorbid PTSD in patients with anxiety disorders. J Traumatic Stress. 1999;12(1):89–100. doi: 10.1023/A:1024746316245. [DOI] [PubMed] [Google Scholar]
- 10.Zlotnick C, Rodriguez BF, Weisberg RB, Bruce SE, Spencer MA, Culpepper L, et al. Chronicity in posttraumatic stress disorder and predictors of the course of posttraumatic stress disorder among primary care patients. J Nerv Ment Dis. 2004;192(2):153–9. doi: 10.1097/01.nmd.0000110287.16635.8e. [DOI] [PubMed] [Google Scholar]
- 11.Koenen KC, Stellman SD, Sommer JF, Jr, Stellman JM. Persisting posttraumatic stress disorder symptoms and their relationship to functioning in Vietnam veterans: a 14-year follow-up. J Trauma Stress. 2008;21(1):49–57. doi: 10.1002/jts.20304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Keller MB, Yonkers KA, Warshaw MG, Pratt LA, Gollan JK, Massion AO, et al. Remission and relapse in subjects with panic disorder and panic with agoraphobia: a prospective short-interval naturalistic follow-up. J Nerv Ment Dis. 1994;182(5):290–6. doi: 10.1097/00005053-199405000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Spitzer R, Williams J, Gibbon M, First M. Structured Clinical Interview for DSM-III-R Patient Version (SCID-P) New York, NY: Biometrics Research Department, New York State Psychiatric Institute; 1988. [Google Scholar]
- 14.Endicott J, Spitzer R. A diagnostic interview: the Schedule for Affective Disorders and Schizophrenia (SADS-L) Arch Gen Psychiatry. 1978;35:837–44. doi: 10.1001/archpsyc.1978.01770310043002. [DOI] [PubMed] [Google Scholar]
- 15.Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott P, et al. The longitudinal interval follow-up evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry. 1987;44(6):540–8. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- 16.Byrne BM, Lam WWT, Fielding R. Measuring patterns of change in personality assessments An annotated application of latent growth curve modeling. J Pers Assess. 2008;90(6):536–46. doi: 10.1080/00223890802388350. [DOI] [PubMed] [Google Scholar]
- 17.Mollica RF, McInnes K, Poole C, Tor S. Dose-effect relationships of trauma to symptoms of depression and post-traumatic stress disorder among Cambodian survivors of mass violence. Br J Psychiatry. 1998;173:482–8. doi: 10.1192/bjp.173.6.482. [DOI] [PubMed] [Google Scholar]
- 18.Kolassa I-T, Ertl V, Eckart C, Kolassa S, Onyut LP, Elbert T. Spontaneous remission from PTSD depends on the number of traumatic event types experienced. Psychol Trauma Theory Res Pract Policy. 2010;2(3):169–74. [Google Scholar]
- 19.Neuner F, Schauer M, Karunakara U, Klaschik C, Robert C, Elbert T. Psychological trauma and evidence for enhanced vulnerability for posttraumatic stress disorder through previous trauma among West Nile refugees. BMC Psychiatry. 2004;4:34. doi: 10.1186/1471-244X-4-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ullman SE, Brecklin LR. Sexual assault history, PTSD, and mental health service seeking in a national sample of women. J Community Psychol. 2002;30(3):261–79. [Google Scholar]
- 21.Collimore KC, Carleton RN, Hofmann SG, Asmundson GJG. Posttraumatic stress and social anxiety: The interaction of traumatic events and interpersonal fears. Depress Anxiety. 2010;27(11):1017–26. doi: 10.1002/da.20728. [DOI] [PubMed] [Google Scholar]
- 22.Roszell DK, McFall ME, Malas KL. Frequency of symptoms and concurrent psychiatric disorder in Vietnam veterans with chronic PTSD. Hosp Community Psychiatry. 1991;42(3):293–6. doi: 10.1176/ps.42.3.293. [DOI] [PubMed] [Google Scholar]
- 23.Hofmann SG, Litz BT, Weathers FW. Social anxiety, depression, and PTSD in Vietnam veterans. J Anxiety Disord. 2003;17(5):573–82. doi: 10.1016/s0887-6185(02)00227-x. [DOI] [PubMed] [Google Scholar]
- 24.Orsillo SM, Heimberg RG, Juster HR, Garrett J. Social phobia and PTSD in Vietnam veterans. J Traumatic Stress. 1996;9(2):235–52. doi: 10.1007/BF02110658. [DOI] [PubMed] [Google Scholar]
- 25.Markowitz JC, Milrod B, Bleiberg K, Marshall RD. Interpersonal factors in understanding and treating posttraumatic stress disorder. J Psychiatr Pract. 2009;15(2):133–40. doi: 10.1097/01.pra.0000348366.34419.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Declercq F, Vanheule S, Markey S, Willemsen J. Posttraumatic distress in security guards and the various effects of social support. J Clin Psychol. 2007;63(12):1239–46. doi: 10.1002/jclp.20426. [DOI] [PubMed] [Google Scholar]
- 27.Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Anxiety Disord. 2011;25(3):456–65. doi: 10.1016/j.janxdis.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Breslau N, Peterson EL, Poisson LM, Schultz LR, Lucia VC. Estimating post-traumatic stress disorder in the community: Lifetime perspective and the impact of typical traumatic events. Psychol Med. 2004;34(5):889–98. doi: 10.1017/s0033291703001612. [DOI] [PubMed] [Google Scholar]
- 29.Cougle JR, Resnick H, Kilpatrick DG. Factors associated with chronicity in posttraumatic stress disorder: A prospective analysis of a national sample of women. Psychol Trauma Theory Res Pract Policy. 2011 doi: 10.1037/a0025954. [DOI] [Google Scholar]
- 30.Yonkers KA, Bruce SE, Dyck IR, Keller MB. Chronicity, relapse, and illness – Course of panic disorder, social phobia, and generalized anxiety disorder: Findings in men and women from 8 years of follow-up. Depress Anxiety. 2003;17(3):173–9. doi: 10.1002/da.10106. [DOI] [PubMed] [Google Scholar]


