Abstract
The objective is to determine short and long-term cardiovascular (CV) outcomes in unselected diabetic patients with acute ischemic chest pain (AICP). For diabetic patients presenting to the emergency department with AICP, the short-term CV outcomes remain discordant between trials and registries, whereas the long-term outcomes are not well-described. A consecutive cohort of all residents of Olmsted County, Minnesota, presenting with AICP during the period January 1, 1985 through December 31, 1992 were followed for a median duration of 16.6 years. The primary outcome was long-term all-cause mortality. Other outcomes included a composite of death, MI, stroke, and revascularization (MACCE); and heart failure (HF) events at 30 days and a median of 7.3 years respectively. Of the 2271 eligible patients, 336 (14.8%) were classified with diabetes mellitus (DM). The crude 30-day MACCE rate was 10.1% in diabetic patients and 6.1% in non-diabetic patients (p=0.007). HF events were more common in diabetic patients at 30 days (9.8%, vs.3.1%, p<0.001). At 7.3 years, diabetic patients were more likely to experience MACCE and HF events than non-diabetic patients (71.2% vs. 45.1%, unadjusted HR 2.15, 95 % CI 1.87-2.48, p<0.001) and (45.1%, vs. 18.2%, p<0.001) respectively. Over the follow-up period, 272 (81.9%) diabetic patients died compared to 936 (49.2%) non-diabetic patients (p<0.001). In conclusion, DM is associated with a higher short-term risk of MACCE and HF and a higher long-term risk of mortality in unselected patients with AICP. DM should be included as a high-risk variable in national acute coronary syndrome guidelines.
Keywords: Diabetes, Outcomes, ACS, Chest Pain, Guidelines
In long-term follow-up, data from a pooled analysis of TIMI trials demonstrated that diabetes mellitus (DM) was associated with a higher mortality at 1 year than patients without DM 1. This increased risk of death was also observed in a large international registry at 2-years which also documented a higher risk of subsequent heart failure (HF) 2. The longest follow up of mortality for diabetic patients with non ST elevation acute coronary syndrome (NSTE ACS) is 4 years 3. Despite this evidence, and the recognition that DM is one of the most important risk variables in the causation of coronary heart disease (CHD), DM is currently not included as an independent high-risk variable in the national and international risk assessment guidelines for patients presenting with suspected ACS 4, 5. We present findings from a unique community-based cohort of consecutive NSTE ACS patients, with and without DM, who were followed for more than 15 years.
Methods
Using written screening logs, we retrospectively identified all residents of Olmsted County, Minnesota (OC) presenting to one of the County's three emergency rooms with acute chest pain during the period January 1, 1985 through December 31, 1992. The complete medical records of all County residents presenting with their first episode of acute chest pain, consistent with an unstable coronary syndrome, in during the study period were reviewed by an experienced nurse abstractor. This was defined according to the Diamond classification as follows: new onset or worsening pattern of ischemic chest pain, occurring at rest or with minimal exertion, and alleviated by sublingual nitroglycerin and/or rest 6.
Patients were excluded if they had an electrocardiogram suggestive of ST segment elevation myocardial infarction (STEMI), or a definitive alternate etiology for the chest pain, including pulmonary embolism, pneumonia, musculoskeletal pain, pericarditis and dissecting aortic aneurysm. Diabetic patients were identified from notations in the medical record that included a recorded diagnosis in the past medical history and use of anti-hyperglycemic medication. Both patients with type 1 and type 2 DM were included.
For all eligible patients, the complete medical record was abstracted to determine the history of the qualifying episode, including detailed physical examination findings, as well as past medical history. This was carried out through the resources of the Rochester Epidemiology Project 7. The qualifying electrocardiogram was interpreted by a staff cardiologist from the Mayo Clinic and verified by one of the study physicians. Using the Agency for Health Care Policy and Research (AHCPR) criteria, which form the basis for chest pain clinical risk stratification in the current American College of Cardiology/American Heart Association guideline 4, 8, patients were classified into high-, intermediate-, and low-risk categories. Patients subsequently ruling-in for myocardial infarction, with a CK-MB or CK level greater than twice the upper limit of normal anytime within the first 24-hours of ED presentation, were classified as the evolving myocardial infarction group. Troponins were not available during the study period.
Long-term data were collected in two phases. In the first phase, major cardiovascular (CV) adverse events and cerebrovascular events (MACCE) including death, MI, stroke and need for revascularization were measured. Study subjects who did not have ongoing medical care visits in OC were contacted to determine vital status. The first phase of long-term patient follow-up ended September 29, 1998.
In the second phase, last known alive dates or death dates as of January 2007 were added. Death dates were obtained through the State of Minnesota and OC death records. Thirty-seven patients were excluded at this time for refusal to allow use of their records for research purposes.
Continuous data are presented as mean and range and compared between diabetics and non-diabetics with Student's t-test. Categorical data are summarized as frequency (percentage) and compared with Pearson's chi-squared test. Survival rates are estimated using Kaplan-Meier (KM) methods and compared with the log-rank test. Logistic regression models were used to estimate unadjusted and partial (adjusted) odds ratios between DM and other risk factors and 30 day events. Cox proportional hazards models were used to estimate the marginal and partial effects of DM and other risk factors on follow-up mortality and MACCE. Interactions between age and DM and gender and DM were investigated and retained if statistically significant and omitted if not. Covariate risk factors were included if they had significant unadjusted associations with the endpoint. No variable selection was done except for the aforementioned testing for interactions.
Results
There were 6,801 residents of OC who presented to an emergency room with their first episode of acute chest pain during the study period, January 1, 1985 through December 31, 1992. Of these, 2,271 (33.4%) met eligibility criteria for NSTE ACS and were followed as study subjects for a median of 7.3 years for MACCE. Of the ineligible patients, cardiac causes accounted for 6.7% of patients including STEMI in 5.5%, stable angina in 1.0% and aortic dissection in 0.2%. Non-cardiac causes of chest pain accounted for 36.2% of patients, 23.9% of patients were excluded because of an indeterminate cause, 17.6% because they were non-residents, and 15.6% for other reasons. After extending the follow-up data for vital status, 2234 study subjects were followed for a median of 16.6 years.
Of the 2271 patients, 336 (14.8%) patients had previously diagnosed DM. Table 1 lists the baseline characteristics in diabetic patients compared to non-diabetic patients. Diabetic patients were older, more likely to have had an MI, or NSTE ACS, or chronic stable angina. Diabetic patients were also more likely to have hypertension, use aspirin, and have an electrocardiogram abnormality. However, they were less likely to be smokers.
Table 1. Baseline Characteristics of Diabetic vs. Non-Diabetic Patients.
| Characteristics | Total | Diabetes Mellitus | P Value | |
|---|---|---|---|---|
| 2271 | Yes 336 (14.8%) | No 1935 (85.2%) | ||
| Mean Age in Years (Range) | 63 (21-101) | 68 (31-95) | 62 (21-101) | <.001 |
| Men | 1306 (57.5%) | 178 (53.0%) | 1128 (58.3%) | 0.07 |
| Previous Myocardial Infarction | 490 (21.6%) | 113 (33.6%) | 377 (19.5%) | <.001 |
| Previous Unstable Angina | 201 (8.9%) | 47 (14.0%) | 154 (8.0%) | <.001 |
| Previous Stable Angina | 679 (29.9%) | 146 (43.5%) | 533 (27.5%) | <.001 |
| Incidence Cases* | 1352 (59.5%) | 145 (43.2%) | 1207 (62.4%) | <.001 |
| Current Smoking | 490 (21.6%) | 41 (12.2%) | 449 (23.2%) | <.001 |
| Hypertension** | 1039 (45.8%) | 228 (67.9%) | 811 (41.9%) | <.001 |
| Hypercholesterolemia*** | 794 (35.0%) | 119 (35.4%) | 675 (34.9%) | 0.85 |
| Aspirin Use (pre) | 395 (17.4%) | 74 (22.0%) | 321 (16.6%) | 0.015 |
| Admitted | 2174 (95.7%) | 327 (97.3%) | 1847 (95.5%) | 0.12 |
| Any Electrocardiogram Abnormality | 1257 (55.4%) | 232 (69.0%) | 1025 (53.0%) | <.001 |
| Left Bundle Branch Block | 102 (4.5%) | 18 (5.4%) | 84 (4.3%) | 0.41 |
| Family History of Coronary Heart Disease | 588 (25.9%) | 95 (28.3%) | 493 (25.5%) | 0.28 |
| Mean (range) Systolic Blood Pressure @ Index Date (mmHg) | 153 (60-300) | 158 (80-230) | 152 (60-300) | <.001 |
| Mean (range) Diastolic Blood Pressure @ Index Date (mmHg) | 87 (34-170) | 86 (43-150) | 88 (34-170) | 0.035 |
| Unstable Angina as Discharge Diagnosis | 260 (11.4%) | 65 (19.4%) | 195 (10.1%) | <.001 |
| Non ST Elevation Myocardial Infarction as Discharge Diagnosis | 479 (21.1%) | 90 (26.8%) | 389 (20.1%) | 0.006 |
Index episode as first presentation with chest pain
Defined by systolic blood-pressure >140 mmHg or diastolic blood-pressure>90 mmHg
Defined by total cholesterol > 220 mg/dL
In unadjusted analysis, diabetic patients were more likely to suffer a MACCE in the short-term (Table 2). At 30 days, 14 (4.2%) diabetic patients versus 43 (2.2%) non-diabetic patients (p=0.035) had died and were also more likely to suffer a stroke. No stroke events were related to percutaneous coronary intervention (PCI). Thirty-three diabetic patients had heart failure (HF) at 30 days (9.8%) versus 60 non-diabetic patients (3.1%, p <0.001) at 30 days, with HF defined as a clinical diagnosis based on symptoms of dyspnea on exertion, orthopnea and fatigue. In multivariate modeling, diabetes was no longer associated with 30-day MACCE (OR 1.72; 95% CI 1.15-2.56; p=0.008). However, diabetes remained associated with HF after controlling for age, prior MI, prior unstable angina, prior stable angina, hypertension, an abnormal index electrocardiogram, and left bundle branch block (OR 2.42; 95% CI 1.52-3.85; p<.001).
Table 2. 30-day Unadjusted Major Adverse Cardiovascular and Cerebrovascular Events in Diabetic versus Non-Diabetic Patients.
| Event | Total | Diabetes Mellitus | P-value | |
|---|---|---|---|---|
| (n=2271) | Yes (n=336) | No (n=1935) | ||
| Total death | 57 (2.5%) | 14 (4.2%) | 43 (2.2%) | 0.035 |
| Cardiovascular death | 50 (2.2%) | 11 (3.3%) | 39 (2.0%) | 0.147 |
| Myocardial Infarction | 47 (2.1%) | 6 (1.8%) | 41 (2.1%) | 0.692 |
| Stroke | 14 (0.6%) | 6 (1.8%) | 8 (0.4%) | 0.003 |
| Revascularization | 59 (2.6%) | 11 (3.3%) | 48 (2.5%) | 0.399 |
| Percutaneous Coronary Intervention | 26 (1.1%) | 4 (1.2%) | 22 (1.1%) | 0.932 |
| Coronary Artery Bypass Graft Surgery | 35 (1.5%) | 7 (2.1%) | 28 (1.4%) | 0.382 |
| Heart Failure | 93 (4.1%) | 33 (9.8%) | 60 (3.1%) | <.001 |
| Major Adverse Cardiovascular and Cerebrovascular Events | 153 (6.7%) | 34 (10.1%) | 119 (6.1%) | 0.007 |
| Major Adverse Cardiovascular and Cerebrovascular Events or Heart Failure | 230 (10.1%) | 62 (18.5%) | 168 (8.7%) | <.001 |
Diabetic patients were at greater risk (unadjusted HR 2.15; 95% CI 1.87-2.48; p<0.001) for MACCE on long-term follow-up (Figure 1). At seven years of follow-up, there were 227 MACCE among diabetic patients (71%; 95% CI 66-76%) and 779 MACCE in non-diabetic patients (45%; 95% CI 43-48%, Table 3). In a multivariable model, the significant association between DM and long-term MACCE persisted (Table 4). There was a significant interaction (p=0.032) between age and DM such that the effect of DM on long-term MACCE was more pronounced in younger patients (HR 3.19; 95% CI 1.65-6.18, age<50 years) than in older patients (HR 0.80; 95% CI 0.45-1.41, age≥90 years). In addition, the adverse effect of DM on MACCE was more pronounced in women. This gender effect was not secondary to differences in the rates of revascularization. At 7.3 years, diabetic patients were also significantly more likely to suffer with HF (121 events, 45.1%, vs. 285 events, 18.2%, p<0.001).
Figure 1.
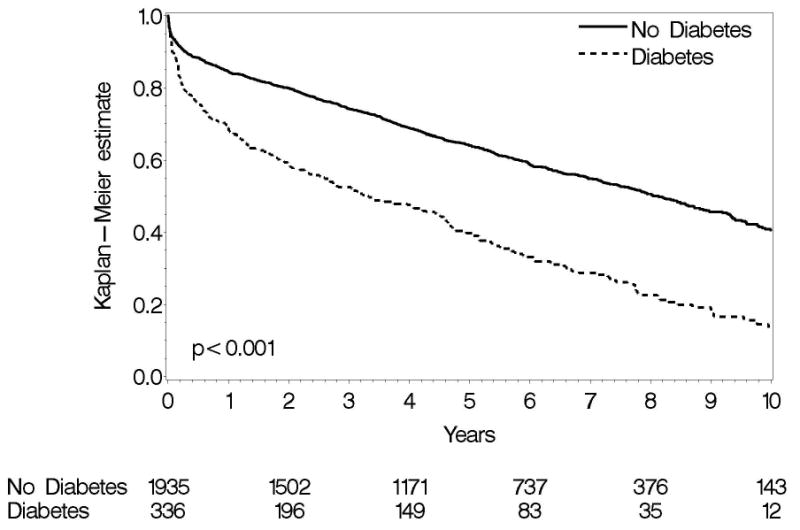
MACCE Events, DM vs. no DM. The number at risk is reported at 0, 2, 4, 6, 8, and 10 years.
Table 3. Long-Term Unadjusted Major Adverse Cardiovascular and Cerebrovascular Events in Diabetic versus Non-Diabetic Patients.
| Diabetes Mellitus | No Diabetes Mellitus | ||||
|---|---|---|---|---|---|
| Event | Total Events | K-M (95% CI) | Total Events | K-M (95% CI) | P-value |
| Death | 151 | 48.4 (42.4, 53.9) | 437 | 26.4 (24.1, 28.5) | <.001 |
| Cardiac Death | 83 | 29.7 (23.8, 35.1) | 215 | 13.5 (11.8, 15.3) | <.001 |
| Myocardial Infarction | 69 | 27.5 (21.4, 33.1) | 225 | 14.0 (12.2, 15.8) | <.001 |
| Stroke | 45 | 21.0 (14.9, 26.6) | 117 | 8.2 (6.7, 9.7) | <.001 |
| Revascularization | 74 | 27.9 (22.0, 33.3) | 320 | 20.3 (18.2, 22.4) | <.001 |
| Heart Failure | 121 | 45.1 (38.5, 51.1) | 285 | 18.2 (16.2, 20.1) | <.001 |
| Major Adverse Cardiovascular and Cerebrovascular Events | 227 | 71.2 (65.5, 76.0) | 779 | 45.1 (42.6, 47.5) | <.001 |
| Major Adverse Cardiovascular and Cerebrovascular Events or Heart Failure | 248 | 76.9 (71.6, 81.3) | 831 | 47.7 (45.2, 50.1) | <.001 |
Table 4. Model for Major Adverse Cardiovascular and Cerebrovascular Events in Diabetic Patients at a Median Follow-Up Period of 7.3 Years.
| Variable | Hazard Ratio | 95% Confidence Interval | P-value | |
|---|---|---|---|---|
| Age (years) | <.001 | |||
| <50 | 1.000 | ref. | ||
| 50-59 | 1.669 | 1.194 | 2.333 | 0.003 |
| 60-69 | 2.327 | 1.696 | 3.192 | <.001 |
| 70-79 | 3.542 | 2.585 | 4.854 | <.001 |
| 80-89 | 5.467 | 3.949 | 7.570 | <.001 |
| 90+ | 9.812 | 6.788 | 14.182 | <.001 |
| DM effect by age group | 0.032 | |||
| <50 | 3.192 | 1.648 | 6.184 | <.001 |
| 50-59 | 1.430 | 0.846 | 2.418 | 0.182 |
| 60-69 | 1.814 | 1.321 | 2.492 | <.001 |
| 70-79 | 1.406 | 1.063 | 1.860 | 0.017 |
| 80-89 | 1.373 | 0.986 | 1.911 | 0.061 |
| 90+ | 0.796 | 0.450 | 1.407 | 0.432 |
| Female gender | 0.691 | 0.598 | 0.798 | <.001 |
| Diabetes*Female gender | 1.371 | 1.025 | 1.832 | 0.033 |
| Prior Myocardial Infarction | 1.394 | 1.215 | 1.600 | <.001 |
| Unstable Angina Pectoris | 1.229 | 1.024 | 1.474 | 0.026 |
| Stable Angina Pectoris | 1.179 | 1.036 | 1.342 | 0.013 |
| Current Smoker | 1.289 | 1.094 | 1.519 | 0.002 |
| Hypertension | 1.307 | 1.150 | 1.486 | <.001 |
| Abnormal Electrocardiogram | 1.257 | 1.097 | 1.440 | <.001 |
| Left Bundle Branch Block | 1.449 | 1.145 | 1.834 | 0.002 |
| Systolic Blood Pressure | 1.000 | 0.998 | 1.002 | 0.805 |
In multivariable analysis, DM was not associated with a significant effect on 30-day mortality (OR 1.43; 95% CI 0.75-2.72; p=0.28). In multivariable analysis, after controlling for age, prior MI, stable angina, hypertension, abnormal electrocardiogram, systolic blood pressure, and index MI, DM was not associated with a significant effect on 30-day mortality (OR 1.28, CI 0.85-1.95, p=0.24). At intermediate and long-term follow up, DM adversely impacted survival. The median survival among diabetic patients (Figure 2) was 7.5 years compared with 16.5 years among non-diabetic patients (HR 2.45; 95% CI 2.14-2.81; p<0.001). At the end of follow-up, 272 (81.9%) diabetic patients compared to 936 (49.2%) non-diabetic patients had died (p<0.001). In a multivariable model, DM was associated with a significant increase in long-term mortality, with different effect depending on age (Table 5). Similar to the model results for MACCE, this effect was less pronounced in older patients compared with patients <50 years old, in whom there was a strong association with follow-up mortality (HR 4.70; 95% CI 1.56-14.1; p=0.006), which decreased with increasing age. In patients 90 years and older, the association was not significant (HR 1.08; 95% 0.71-1.63; p=0.73).
Figure 2.
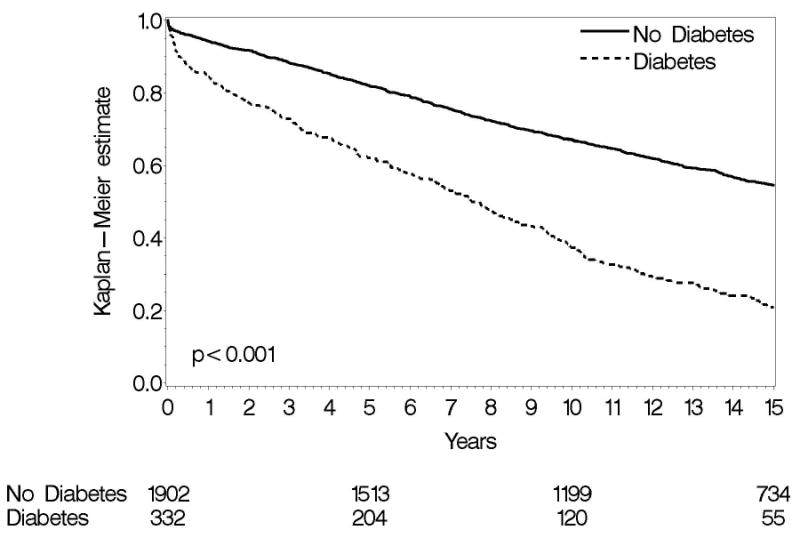
Mortality, DM vs. no DM. The number at risk is reported at 0, 5, 10, and 15 years.
Table 5. Model for Mortality at a Median of 16.6 Years in Diabetic Patients Compared to Non-Diabetic Patients.
| Variable | Hazard Ratio | 95% Confidence Interval | P-value | |
|---|---|---|---|---|
| Age (years) | <.001 | |||
| <50 | 1.000 | ref. | ||
| 50-59 | 1.356 | 0.749 | 2.453 | 0.314 |
| 60-69 | 3.024 | 1.779 | 5.139 | <.001 |
| 70-79 | 6.372 | 3.807 | 10.664 | <.001 |
| 80-89 | 16.217 | 9.701 | 27.112 | <.001 |
| 90+ | 39.446 | 23.242 | 66.948 | <.001 |
| DM effect by age group | 0.003 | |||
| <50 | 4.695 | 1.562 | 14.117 | 0.006 |
| 50-59 | 2.318 | 1.072 | 5.009 | 0.033 |
| 60-69 | 2.761 | 1.923 | 3.964 | <.001 |
| 70-79 | 2.257 | 1.769 | 2.879 | <.001 |
| 80-89 | 1.654 | 1.315 | 2.081 | <.001 |
| 90+ | 1.077 | 0.713 | 1.627 | 0.725 |
| Ever Smoked | 1.440 | 1.265 | 1.639 | <.001 |
| Female gender | 0.947 | 0.831 | 1.079 | 0.410 |
| Hypertension | 1.294 | 1.144 | 1.464 | <.001 |
| Systolic Blood Pressure | 0.997 | 0.995 | 0.999 | <.001 |
| Hypercholesterolemia | 0.999 | 0.999 | 1.000 | 0.268 |
| Family History of Coronary Heart Disease | 1.125 | 0.980 | 1.292 | 0.095 |
| Prior Aspirin | 0.903 | 0.781 | 1.044 | 0.167 |
| Prior Revascularization | 1.340 | 1.125 | 1.596 | 0.001 |
| Prior Myocardial Infarction or History of Coronary Heart Disease | 1.572 | 1.365 | 1.812 | <.001 |
| ST-segment Depression ≥1mm | 1.432 | 1.186 | 1.728 | <.001 |
| Extracardiac Vascular Disease | 1.726 | 1.354 | 2.200 | <.001 |
| Pulmonary Edema Related to Ischemia | 1.714 | 1.402 | 2.096 | <.001 |
In an unadjusted comparison of diabetic patients with low-to-moderate AHCPR risk and non-diabetic patients with high AHCPR risk, survival was similar for the first 8 years (Figure 3). A divergence in the KM curve after this time resulted in a significant difference between the two groups (HR 1.29; 95% CI 1.07-1.56; p=0.009) with low-to-moderate risk diabetic patients fairing worse than non-diabetic high risk patients. Diabetic patients with high AHCPR criteria performed consistently worse than both groups.
Figure 3.
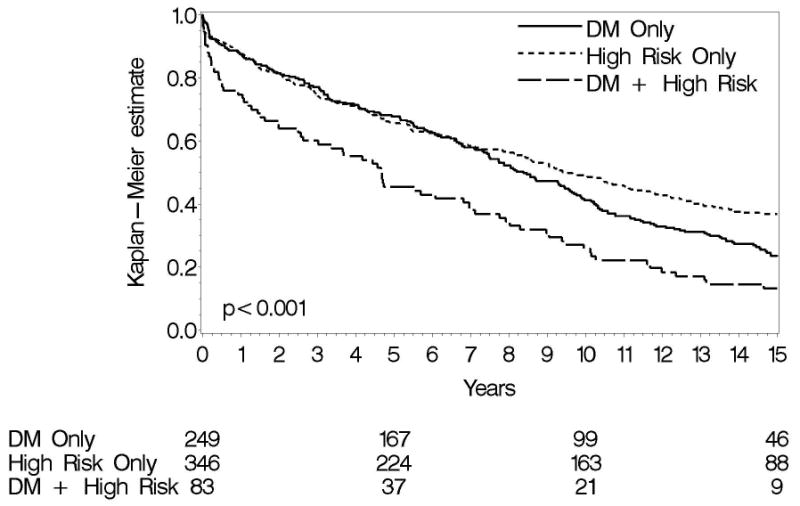
Mortality, DM vs. AHCPR High-Risk Patients. The number at risk is reported at 0, 5, 10, and 15 years.
Discussion
Cardiovascular outcomes in diabetic patients presenting with ACS have been described in data from trials and registries 1-3, 9-12, have focused primarily on short-term outcomes and reported conflicting results. Diabetic patients with ACS managed invasively have also demonstrated higher rates of composite ischemia and major bleeding, as evidenced by an analysis from the ACUITY trial 13. Our study is unique in that it consists of a large, consecutive, community-based cohort of patients with both short- and long-term follow up, and is largely free of selection bias.
On short-term follow up at 30 days, we found that unselected diabetic patients presenting with AICP had a higher crude rate of death and stroke. The baseline characteristics and short-term findings from large ACS registries are similar to our study, suggesting that registry data provide a good representation of day-to-day practice and outcomes. In-hospital data from the OASIS registry reveal a higher crude rate of death and stroke in diabetic patients, without any increase in MI 1. The GRACE registry reported that younger diabetic patients and those on insulin were more likely to die 10. The Euro Heart Survey of ACS demonstrated increased in-hospital mortality in diabetic women, but not in diabetic men 11. This variable effect of gender on short-term mortality and MACCE was not observed in our cohort.
In a multivariate model, the 30-day data from our cohort of diabetic patients did not demonstrate an independent effect of DM on MACCE. However, multivariate analysis in diabetic patients can potentially underestimate the inherent CV risk posed by DM. This is likely the result of unintended statistical over-adjustment for variables such as hypertension, obesity, prior revascularization, chronic kidney disease, and other co-morbidities, present more frequently in diabetic patients. The higher risk of stroke in our cohort of diabetic patients in the short-term may be explained by the higher coexisting rates of hypertension, coronary bypass, and extensive atherosclerosis. Unlike our study, multivariable-adjusted pooled trial data from 11 TIMI studies revealed that diabetic patients with ACS had a higher risk of death at 30 days 3. This difference may be explained by the preferential enrollment of higher-risk populations in the constituent TIMI trials.
The higher incidence of new-onset HF at 30 days in diabetic patients in our study has been previously observed in the GRACE and OASIS registries 1, 10. This excess risk of HF in diabetic patients has been postulated to result from disturbances in microvascular circulation, abnormalities in myocardial glucose and free fatty acid metabolism and by hyperglycemia-induced myocyte necrosis, apoptosis, and fibrosis 14.
Longer-term follow up data in unselected diabetic patients presenting with an index episode of ACS are non-existent. Our study is unique in that it provides long-term follow up, to a median of 7.3 years for MACCE and 16.6 years for mortality in diabetic patients with NSTE ACS. The longest previous follow up of 4 years in 170 diabetic patients with ACS from the PRAIS-UK registry failed to find a significant independent effect of DM on mortality. Pooled data from five TIMI studies did not reveal DM to be an independent predictor of death at 1 year 12. The heterogeneous and generally higher-risk studies pooled for analysis limits their generalizability. However, 2-year findings of the unselected OASIS registry showed that DM was associated with a significantly higher mortality, similar to our study.
It was also evident from our analysis that the adverse CV effect of DM was most pronounced in younger patients. The absence of an independently adverse CV effect of DM in patients older than 90 is likely to have resulted from a higher burden of co-morbid CV conditions. The increased long-term MACCE rate associated with DM in women in the long-term are consistent with findings from the OASIS registry 1. Also critically important was the diabetic patients' prognosis, comparable to non-diabetic patients classified at high-risk by AHCPR criteria. These data emphasize the need for aggressive risk assessment and management in diabetic patients, institution of evidence-based therapies, and development of diabetes-specific treatments that can ameliorate accelerated atherosclerosis and exaggerated thrombosis.
We acknowledge some limitations in our study. The diagnosis of DM was based on review of medical records. Information about the duration and control of DM, baseline LV function, prior history of heart failure, and renal function was unavailable. Since data was collected retrospectively, undiagnosed diabetic patients may have been misclassified at the outset. This misclassification likely resulted in an overestimation of MACCE rates in non-diabetic patients. In addition, no data was available on patients who may have developed DM during the course of the long follow up. It can be argued that the demographic and patient compliance patterns in OC are not entirely representative of epidemiologic and disease patterns in other parts of the US. Although this is well-recognized, evidence from international studies argues against perceived differences in the impact of risk factors for CHD between different racial and cultural groups 15, 16 Another important limitation to our study is the lack of data on treatment modalities in diabetic patients, as it has been well reported that evidence-based therapies remain underutilized in diabetic patients with acute coronary syndromes 17, 18. Finally, the lack of troponin assay at the time of the study likely underestimated the proportion of patients with NSTE-MI.
Acknowledgments
Supported by NIH Grant AR30582-43, The Rochester Epidemiology Project.
Footnotes
Disclosures: The authors have no conflict of interests to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Malmberg K, Yusuf S, Gerstein HC, Brown J, Zhao F, Hunt D, Piegas L, Calvin J, Keltai M, Budaj A. Impact of diabetes on long-term prognosis in patients with unstable angina and non-Q-wave myocardial infarction: results of the OASIS (Organization to Assess Strategies for Ischemic Syndromes) registry. Circulation. 2000;102:1014–1019. doi: 10.1161/01.cir.102.9.1014. [DOI] [PubMed] [Google Scholar]
- 2.Bakhai A, Collinson J, Flather MD, de Arenaza DP, Shibata MC, Wang D, Adgey JA, for the PRAIS-UK Investigators Diabetic patients with acute coronary syndromes in the UK: high risk and under treated. Results from the prospective registry of acute ischaemic syndromes in the UK (PRAIS-UK) Int J Cardiol. 2005;100:79–84. doi: 10.1016/j.ijcard.2004.08.035. [DOI] [PubMed] [Google Scholar]
- 3.Donahoe SM, Stewart GC, McCabe CH, Mohanavelu S, Murphy SA, Cannon CP, Antman EM. Diabetes and mortality following acute coronary syndromes. JAMA. 2007;298:765–775. doi: 10.1001/jama.298.7.765. [DOI] [PubMed] [Google Scholar]
- 4.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Jr, Chavey WE, II, Fesmire FM, Hochman JS, Levin TN, Lincoff AM, Peterson ED, Theroux P, Wenger NK, Wright RS, Smith SC, Jr, Jacobs AK, Adams CD, Anderson JL, Antman EM, Halperin JL, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura R, Ornato JP, Page RL, Riegel B. American College of Cardiology; American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2007;50:e1–157. doi: 10.1016/j.jacc.2007.02.013. Erratum in: J Am Coll Cardiol 2008;51:974. [DOI] [PubMed] [Google Scholar]
- 5.Bassand JP, Hamm CW, Ardissino D, Boersma E, Budaj A, Fernández-Avilés F, Fox KA, Hasdai D, Ohman EM, Wallentin L, Wijns W. Guidelines for the diagnosis and treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J. 2007;28:1598–1660. doi: 10.1093/eurheartj/ehm161. [DOI] [PubMed] [Google Scholar]
- 6.Diamond GA. A clinically relevant classification of chest discomfort. J Am Coll Cardiol. 1983;1:574–575. doi: 10.1016/s0735-1097(83)80093-x. [DOI] [PubMed] [Google Scholar]
- 7.Kurland LT, Molgaard CA. The patient record in epidemiology. Sci Am. 1981;245:54–63. doi: 10.1038/scientificamerican1081-54. [DOI] [PubMed] [Google Scholar]
- 8.Braunwald E, Mark DB, Jones RH. Clinical practice guideline: Unstable Angina diagnosis and management. AHCPR Publication No 94-0602. 1994 Mar; [Google Scholar]
- 9.Mak KH, Moliterno DJ, Granger CB, Miller DP, White HD, Wilcox RG, Califf RM, Topol EJ. Influence of diabetes mellitus on clinical outcome in the thrombolytic era of acute myocardial infarction: GUSTO-I Investigators (Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries) J Am Coll Cardiol. 1997;30:171–179. doi: 10.1016/s0735-1097(97)00118-6. [DOI] [PubMed] [Google Scholar]
- 10.Franklin K, Goldberg RJ, Spencer F, Klein W, Budaj A, Brieger A, Marre M, Steg PG, Gowda N, Gore JM. GRACE Investigators. Implications of diabetes in patients with acute coronary syndromes. The Global Registry of Acute Coronary Events. Arch Intern Med. 2004;164:1457–1463. doi: 10.1001/archinte.164.13.1457. [DOI] [PubMed] [Google Scholar]
- 11.Dotevall A, Hasdai D, Wallentin L, Battler A, Rosengren A. Diabetes mellitus: clinical presentation and outcome in men and women with acute coronary syndromes. Data from the Euro Heart Survey ACS. Diabet Med. 2005;22:1542–50. doi: 10.1111/j.1464-5491.2005.01696.x. [DOI] [PubMed] [Google Scholar]
- 12.Ahmed S, Cannon CP, Giugliano RP, Murphy SA, Morrow DA, Antman EM, Braunwald E, Gibson CM. The independent and combined risk of diabetes and non-endstage renal impairment in non-ST-segment elevation acute coronary syndromes. Int J Cardiol. 2008;131:105–112. doi: 10.1016/j.ijcard.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 13.Feit F, Manoukian SV, Ebrahimi R, Pollack CV, Ohman EM, Attubato MJ, Mehran R, Stone GW. Safety and efficacy of bivalirudin monotherapy in patients with diabetes mellitus and acute coronary syndromes: a report from the ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) trial. J Am Coll Cardiol. 2008;51:1645–1652. doi: 10.1016/j.jacc.2007.11.081. [DOI] [PubMed] [Google Scholar]
- 14.Aneja A, Tang WH, Bansilal S, Garcia M, Farkouh ME. Diabetic Cardiomyopathy: Insights into Pathogenesis, Diagnostic Challenges, and Therapeutic Options. Am J Med. 2008;121:748–757. doi: 10.1016/j.amjmed.2008.03.046. [DOI] [PubMed] [Google Scholar]
- 15.Gaziano TA, Young CR, Fitzmaurice G, Atwood S, Gaziano JM. Laboratory-based versus non-laboratory-based method for assessment of cardiovascular disease risk: the NHANES I Follow-up Study cohort. Lancet. 2008;371:923–931. doi: 10.1016/S0140-6736(08)60418-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L, INTERHEART Study Investigators Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 17.Yan RT, Yan AT, Tan M, McGuire DK, Leiter L, Fitchett DH, Lauzon C, Lai K, Chow CM, Langer A, Goodman SG, Canadian Acute Coronary Syndrome Registry Investigators Underuse of evidence-based treatment partly explains the worse clinical outcome in diabetic patients with acute coronary syndromes. Am Heart J. 2006;152:676–683. doi: 10.1016/j.ahj.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 18.Franklin K, Goldberg RJ, Spencer F, Klein W, Budaj A, Brieger D, Marre M, Steg PG, Gowda N, Gore JM, GRACE Investigators Implications of diabetes in patients with acute coronary syndromes. The Global Registry of Acute Coronary Events. Arch Intern Med. 2004;164:1457–1463. doi: 10.1001/archinte.164.13.1457. [DOI] [PubMed] [Google Scholar]


