Abstract
AIM
To compare visual performance of wavefront-guided laser in situ keratomileusis (LASIK) with iris-registration (Wg-LASIK group) and conventional LASIK (LASIK group) one year after surgery and analyze the correlation between wavefront aberrations and visual performance.
METHODS
Eight hundred and fifty-two myopic eyes of 430 patients were enrolled in this prospective study and divided into two groups: Wg-LASIK group (436 eyes) and LASIK group (416 eyes). A Wavescan Wavefront aberrometer was used to analyze Zernike coefficients and the root-mean-square (RMS) of higher order aberrations, and Optec 6500 visual function instrument was used to measure contrast sensitivity (CS) before and 3, 6, 12 months after surgery.
RESULTS
The mean spherical equivalent (SE) in Wg-LASIK group was significantly better than those in LASIK group one year after surgery (P=0.024). Wg-LASIK eyes showed better CS values than LASIK eyes at all spatial frequencies with and without glare after surgery (P all<0.01). Moreover, the increase of higher RMS (RMSh), coma, RMS3, RMS4, RMS5 in Wg-LASIK group were significantly lower than those in LASIK group 1 year after surgery (P all<0.05). The increase of coma, spherical aberration (SA), RMS3 and RMS4 in Wg-LASIK and coma and RMS3 in LASIK group were negatively correlated with reduction of contrast sensitivity 1 year after surgery.
CONCLUSION
A significant better visual performance is got in Wg-LASIK group compared with LASIK group 1 year after surgery, and the Wg-LASIK is particularly suitable for eyes with high-magnitude RMSh.
Keywords: aberration, contrast sensitivity, visual performance, laser in situ keratomileusis
INTRODUCTION
Although conventional laser in situ keratomileusis (LASIK) has become an efficient and safe way in reducing spherocylindrical refractive errors, there are concerns about a decrement of visual performance after the refractive surgery, such as glare and halos under dim conditions and poor night vision despite the fact that visual acuity has been improved[1]-[5]. Recent studies show that the increase in ocular optical aberrations which degraded the retinal image may account for most of the decrease in contrast sensitivity and symptoms described above[6]-[8]. Wavefront-guided LASIK with iris-registration may improve visual performance by reducing or eliminating existing ocular aberrations. Some studies reported that contrast sensitivity and visual performance were improved after wavefront-guided LASIK and most authors agreed with the apparent superiority of wavefront-guided laser ablations over conventional surgery[9]-[11].
Apart from Snellen acuity, contrast sensitivity is a more reliable parameter in assessing visual performance. Contrast sensitivity measurement at 6 and 12cpd is considered to be the most useful in the assessment of patients who have undergone laser refractive surgery[12]. There have been reports of at least temporary losses of contrast sensitivity, and this loss may persist through 6 months after LASIK[13]-[15]. However, to our knowledge, an in-depth and large cohort statistical comparison of corneal aberrations and visual performance between conventional LASIK (LASIK group) and wavefront-guided LASIK with iris-registration (Wg-LASIK group) continued for more than one year has not been performed.
The aim of this study was to compare the visual acuity, higher-order aberrations and contrast sensitivity of Wg-LASIK group and conventional LASIK one year after the surgery and evaluate the long-term effect of wavefront-guided LASIK and conventional LASIK treatments on contrast sensitivity and visual acuity, so we hope to provide a proposition for refractive surgical treatments.
SUBJECTS AND METHODS
Subjects
This study included 852 eyes of 430 consecutive patients who were scheduled for LASIK from January 2007 to June 2010 in the Tongren Ophthalmic Center of Capital Medical University (Beijing, China) and all the patients completed one year of postoperative follow-up examinations. During the period from April to July 2010, 436 eyes of 220 patients were treated with wavefront-guided LASIK with iris-registration. To better evaluate the outcome of the wavefront-guided LASIK, a comparable group of 210 patients treated with conventional LASIK during the period from June to September 2009 was identified retrospectively. All patients were thoroughly informed about the examinations and surgical procedure and subscribed written consents.
Examinations of Visual Performance
Higher-order aberrations (HOAs) were measured by WaveScan Wavefront aberrometer (VISX Inc., Santa Clara, USA) based on the principle of the Hartmann-Shack wavefront sensor technique[16]. All HOAs were measured in the scotopic condition (3cd/m2) after 10-min dark adaptation. A skilled technician performed three examinations on the same eye with a 6mm pupil diameter. The following parameters were recorded and analyzed: 1) The root mean square of HOAs from 3rd to 6th orders (RMS3-6); 2) RMS of 3rd coma (square root of the sum of the squared coefficients of Z3−1 and Z31), trefoil (Z3−3 and Z33), 4th order spherical aberration (SA) (Z40) and RMS of total higher order aberrations (RMSh).
Contrast sensitivity with and without glare was measured by using Optec 6500 Vision Tester (Stereo Optical Co. Inc, USA) under scotopic lighting conditions (3cd/m2). All patients were examined for monocular contrast sensitivity and were measured with corrected spherical and cylindrical lens according to the manifest refraction in the natural scotopic condition after dark adaptation. The spatial frequencies at which contrast sensitivity was examined were 1.5, 3, 6, 12, 18 cycles per degree (cpd), and contrast sensitivity was expressed in logarithmic units.
Surgical Technique
All surgeries were performed by the same experienced surgeon using VISX STAR S4 excimer laser system (VISX Inc., Santa Clara, USA) with variable spot scanning and the M2 automated microkeratome (Moria, France). The wavefront data were transferred by floppy disk from the WaveScan Wavefront aberrometer (Zernike software) to the STAR S4 excimer laser system. The Moria M2 automated microkeratome was used to create an 8.5 diameter corneal flap with a 6.0mm optical zone and 0.5mm transition zone. After photoablation, the flap was repositioned and the interface was washed with balanced salt solution. After the operation, patients were instructed to instill fluorometholone 0.1% four times per day for 3 days, and then tapered over for two weeks, levofloxacin and artificial tears fours per day for 2 weeks.
Statistical Analysis
Data were expressed as mean±standard deviation (SD) and analyzed with the SPSS 13.0 statistical software (SPSS Inc, Chicago, Illinois, USA). Paired Student's t-test was used for the evaluation of measurement data between post- and pre-treatment. Between the two groups, Independent-samples t-test was used to analyze measurement data conform to normal distribution and Wilcoxon signed rank test was applied for measurement data not conforming to normal distribution, and Chi-square test was used to enumeration data. A multiple stepwise regression analysis model was applied to analyze the relationship between HOAs and contrast sensitivity. P<0.05 was considered statistically significant.
RESULTS
Preoperative Characteristics
The preoperative characteristics of patients are shown in Table 1. No significant differences were observed between the Wg-LASIK group and LASIK group.
Table 1. Preoperative characteristics of eyes undergoing Wg-LASIK and LASIK.
| Characteristic | Wg- LASIK Mean±SD (Range) |
LASIK Mean±SD (Range) |
1P |
| n | 436 | 416 | -- |
| Age (a) | 28.56±4.76 (18 to 40) | 29.12±5.23 (20 to 40) | 0.279 |
| M/F | 95/125 | 79/131 | 0.328 |
| Spherical lens (D) | -5.42±1.68 (-1.85 to -7.65) | -5.29±1.74D (-1.35 to -7.85) | 0.587 |
| Cylindric lens (D) | -0.75±0.39 (0.00 to -4.20) | -0.68±0.54 (0.00 to -3.85) | 0.319 |
| SE (D) | -5.26±1.59 (-1.86 to -7.50) | -5.41±1.76 (-1.50 to -8.25) | 0.296 |
| UCVA (logMAR) | 1.36±0.24 ( 0.15 to 1.70) | 1.39±0.27 (0.1 to 1.70) | 0.289 |
| BSCVA (logMAR) | -0.13±0.05 (-0.08 to 0) | -0.12±0.06 (-0.08 to 0) | 0.612 |
SE: Spherical equivalent; UCVA: Uncorrected visual acuity; BSCVA: Best spectacle-corrected visual acuity. 1Analyzed by Independent-samples t-test (Age, Spherical and Cylindric lens, SE, UCVA, BCVA) and χ2 test (Sex).
Visual Acuity
Effectiveness
Uncorrected visual acuity (UCVA) was measured at each visit for each group. Ninety-six point one percent, 96.6% and 94.4% of Wg-LASIK group were ≥20/20 at 3 months, 6 months and one year after surgery, compared to 92.3%, 89.6% and 88.2% for the conventional LASIK group respectively (P all>0.05).
Predictability
The SE of 95.1% and 92.6% eyes in Wg-LASIK and 90.6% and 86.3% eyes in conventional LASIK group were within ±0.50D three months and one year after surgery. The mean preoperative SE (-5.42±1.68)D was significantly reduced to (-0.21±0.38)D at 3 months and (-0.24±0.41)D at one year after surgery in Wg-LASIK group, while (-5.29±1.74)D decreased to (-0.43±0.54)D at 3 months and (-0.46±0.52)D at 1 year in conventional LASIK group. The differences between two groups for SE at 3 months and one year after surgery were statistically significant (P=0.015, P=0.024).
Safety
Three months after surgery, 29.6% of the treated eyes gained one line of Snellen best corrected visual acuity (BCVA), and 17.2% gained two lines in Wg-LASIK group. After one year 22.3% gained one line and 13.5% gained two lines. None of the eyes lost line at 3 and 6 months after Wg-LASIK, but 0.8% of the eyes lost one line at 1 year after surgery. Seventeen point eight percent and 12.1% of the eyes gained one line 3 months and one year after surgery in conventional LASIK group. None of the eyes gained two lines, while 8.9% of the eyes lost one line at one year after surgery (Figure 1). No intra- or postoperative complications were noted during the study. No eye underwent retreatment during the follow-up period.
Figure 1. Changes in best spectacle corrected visual acuity (BSCVA) 3, 6 and 12 months after surgery in Wg-LASIK group and conventional LASIK.
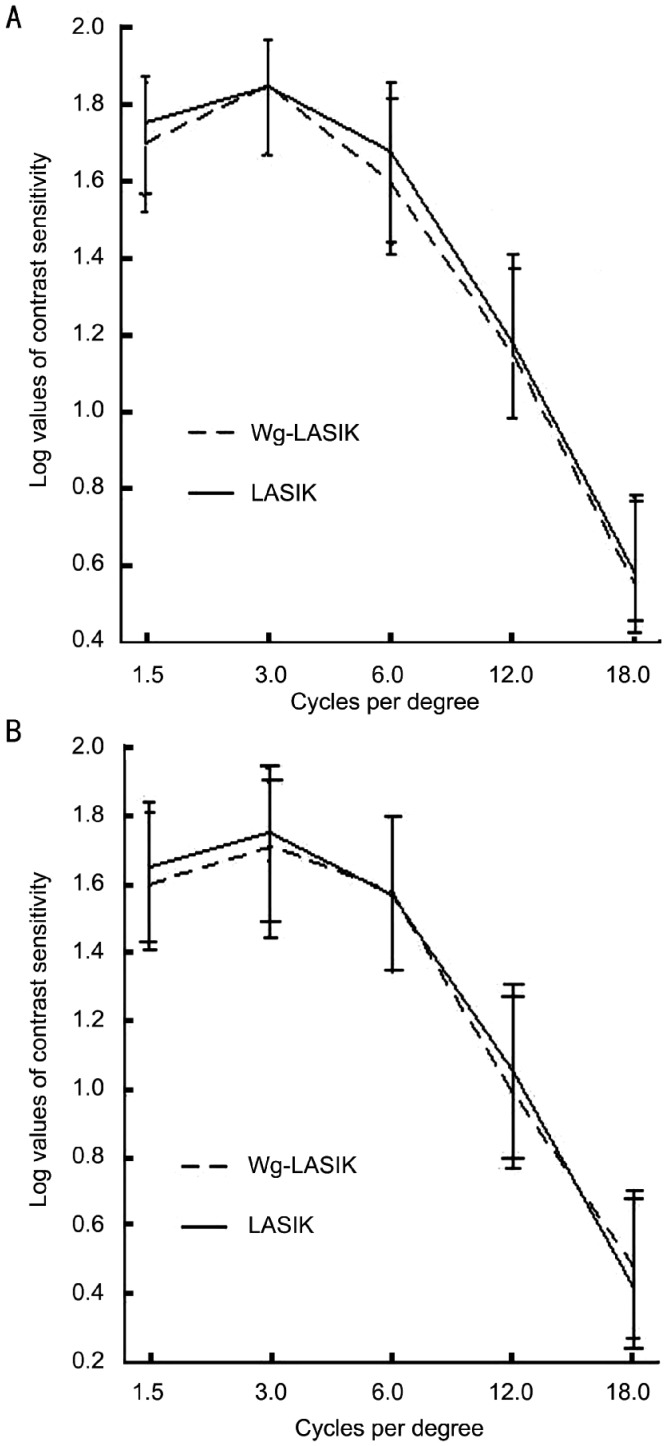
Contrast sensitivity
Contrast sensitivity with and without glare was compared before surgery and 3, 6 and 12 months after treatment. The preoperative contrast sensitivity log values were not significantly different between the two groups (P>0.05) (Figure 2). The differences between the two groups were statistically significant at 3, 6 and 12 months (P all<0.01) (Figure 3). Moreover the magnitude of improvement was greater at higher spatial frequencies (12 and 18cpd) than lower spatial frequencies (1.5 and 3cpd) under all lighting conditions (Figure 3).
Figure 2. Preoperative contrast sensitivity (CS) for Wg-LASIK and conventional LASIK.
A: Preoperative CS without glare; B: Preoperative CS with glare. Analyzed by Independent-Samples t-test.
Figure 3. Postoperative contrast sensitivity(CS) for Wg-LASIK and conventional LASIK.
A: 3-month CS without glare; B: 3-month CS with glare; C: 6-month CS without glare; D: 6-month CS with glare; E: 1-year CS without glare; F: 1-year CS with glare. Analyzed by Independent-samples t-test. aP<0.05.
Contrast sensitivity in Wg-LASIK eyes improved significantly (P all<0.01) at all spatial frequencies (1.5-18cpd) 3, 6 and 12 months after surgery, while conventional LASIK group displayed significantly reduced CS values at most spatial frequencies except for 1.5cpd with glare (P<0.01) at 3 months after surgery. Then the CS values in conventional LASIK group rose to the same level as preoperative CS at 6 and 12 months, except that CS values at 12 and 18cpd both with and without glare remained worse than preoperative values (P<0.01).
Higher-order aberration
There were no statistically significant differences in RMSh, 3rd coma, trefoil, 4thSA and RMS3-6 between Wg-LASIK and conventional LASIK (P all >0.05) preoperatively. The RMS values of higher order aberrations increased significantly in both groups (P all <0.01) after surgery except for trefoil and RMS6 in Wg-LASIK group and trefoil in conventional LASIK group (P all >0.05). RMS values of HOAs in Wg-LASIK were lower than those in conventional LASIK group at 3, 6 and 12 months after the surgery. The differences were not statistically significant at 3 months, while at 1 year RMSh, coma, RMS3, RMS4 and RMS5 in Wg-LASIK eyes were significantly lower than those in conventional LASIK group(P all <0.05) (Table 2).
Table 2. Preoperative and postoperative higher-order aberrations.
| Parameter | Preop. |
3 months Postop. |
6 months Postop. |
12 month Postop. |
||||
| wgLASIK | LASIK | wgLASIK | LASIK | wgLASIK | LASIK | wgLASIK | LASIK | |
| RMSh | 0.33±0.11 | 0.32±0.17 | 0.57±0.19 | 0.57±0.17 | 0.52±0.14a | 0.68±0.25a | 0.52±0.20a | 0.64±0.21a |
| Coma | 0.17±0. 01 | 0.17±0.10 | 0.34±0.18 | 0.368±0.19 | 0.30±0.14a | 0.40±0.25a | 0.28±0.19a | 0.42±0.21a |
| Trefoil | 0.17±0.10 | 0.15±0.09 | 0.16±0.11 | 0.17±0.10 | 0.14±0.09a | 0.21±0.19a | 0.15±0.14 | 0.16±0.09 |
| SA | 0.11±0.09 | 0.10±0.08 | 0.27±0.15 | 0.27±0.17 | 0.31±0.16 | 0.35±0.17 | 0.31±0.15 | 0.32±0.21 |
| RMS 3 | 0.25±0.11 | 0.23±0.11 | 0.40±0.17 | 0.42±0.17 | 0.34±0.13a | 0.48±0.27a | 0.34±0.20a | 0.46±0.20a |
| RMS4 | 0.16±0.08 | 0.16±0.11 | 0.31±0.14 | 0.31±0.15 | 0.34±0.14 | 0.38±0.17 | 0.26±0.16a | 0.39±0.19a |
| RMS5 | 0.08±0.03 | 0.09±0.11 | 0.12±0.05 | 0.13±0.05 | 0.11±0.05a | 0.15±0.07a | 0.11±0.05a | 0.13±0.07a |
| RMS6 | 0.06±0.03 | 0.06±0.04 | 0.09±0.04 | 0.10±0.04 | 0.09±0.05a | 0.11±0.04a | 0.09±0.04 | 0.09±0.04 |
Analyzed by independent-samples t-test, aP<0.05.
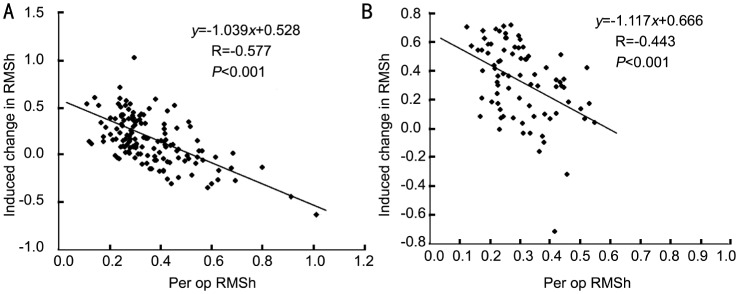
The correlation between induced changes in RMSh and preoperative RMSh in Wg-LASIK and conventional LASIK is shown in Figure 4. A significant negative correlation was found in both groups; that means, when the preoperative RMSh was higher, the induced changes in RMSh were lower. The correlation coefficient in Wg-LASIK group was -0.628 (r=-0.628) while that in conventional LASIK was -0.486 (r=-0.486), and the coefficients in each group achieved statistical significance (P<0.01).
Figure 4. Correlation between induced changes in RMSh and preoperative RMSh.
A: Wavefront-guided LASIK group; B: Conventional LASIK group.
Multiple Stepwise Regression Analysis on Higher-Order Aberrations and Contrast Sensitivity
Correlation between higher-order aberrations and contrast sensitivity
Multiple Stepwise Regression analysis was applied to analyze the influence of preoperative higher-order aberrations on the five spatial frequencies contrast sensitivity and the regression equations are shown in Table 3 (P<0.05). Preoperatively, the reduction in contrast sensitivity at 1.5 and 3cpd spatial frequencies was correlated significantly with the increase of SA. Highly significant positive correlation between RMS6 and 1.5cpd contrast sensitivity were observed, while significant negative correlations between RMS5 and 6cpd contrast sensitivity were seen. The reduction in 18cpd contrast sensitivity was significantly correlated with the increase of RMS6. After surgery, we found that the changes of SA, RMS3 and RMS4 were negatively correlated with the changes of CS at 1.5 and 3cpd spatial frequencies while the reduction in CS at 6 and 12cpd was correlated significantly with the increase of RMS3 and SA.
Table 3. Regression equations of HOAs and contrast sensitivity.
| Spatial frequency | Regression function | F | P |
| 1.5c/d (a) | a=1.835+0.642RMS6-0.421SA | 6.377 | 0.011 |
| 3c/d (b) | b=1.899-0.358 SA | 6.200 | 0.014 |
| 6c/d (c) | c=1.732-0.384 RMS5 | 5.262 | 0.023 |
| 12c/d (d) | d=1.557-0.826RMS3-0.645SA | 7.063 | 0.009 |
| 18c/d (e) | e=0.643+0.641RMS6 | 4.699 | 0.031 |
DISCUSSION
In the present study, long-term efficacy and safety of wavefront-guided LASIK with iris-registration were excellent. By 1 year, 94.4% eyes of Wg-LASIK group were ≥20/20, while 88.2% eyes of conventional group were ≥20/20. In Wg-LASIK group 22.3% eyes gained one line and 13.5% gained two lines while 12.1% eyes gained one line and no eyes gained two lines in conventional LASIK group one year after surgery. The predictability of refractive results was also encouraging. The mean residual SE in Wg-LASIK group was significantly lower than those in conventional LASIK group one year after surgery. The outcomes obtained in current study were generally consistent with previous studies [17],[18]. The quality of vision after wavefront-guided LASIK with iris-registration was remarkable. Although some studies have revealed that conventional LASIK leads to loss of contrast sensitivity and 12 and 18cpd under dim condition are the most affected frequencies, others have shown that this effect recovers with 1 month to 1 year after surgery[19]-[25]. In the current clinical study, it was found that Wg-LASIK eyes showed better CS values than correspondingly preoperative values at all spatial frequencies with and without glare at 3, 6 and 12 months after surgery while conventional LASIK displayed reduced CS values at 3 months, which was similar to the results that got with the same vision tester 3 months after surgery[26]. Then the CS values in conventional LASIK group rose to the same level as preoperative CS at 6 and 12 months, except that CS values at 12 and 18cpd both with and without glare remained worse than preoperative values.
The values of higher-order aberrations and Zernike coefficients in Wg-LASIK were lower than those in conventional LASIK group at 3, 6 and 12 months after surgery. This might be due to the eye-tracking and iris-registration systems which precisely establish the spatial relationship between the optics of the eye and the natural features of the iris can recognize and compensate for ocular torsional movements and sub-clinical decentration when patients changed from sitting position to clinostatism and for pupil center shift from scotopic condition to photopic condition. Our study also showed that when the preoperative RMSh was higher, the induced RMSh changes by both types of treatments were lower. Furthermore, the correlation coefficient in Wg-LASIK group was -0.628 while that in conventional LASIK was -0.486, and the coefficients in both groups achieved statistical significance (P all<0.01). Our results were similar to results of Padmanabhan, more importantly, the coefficients in both groups achieved statistical significance[27]. That means eyes with a significantly high magnitude RMSh are more likely to benefit from wavefront-guided treatment than eyes with low-magnitude RMSh.
Several studies reported that the increase in ocular aberrations correlated with loss of visual acuity and accounted for most of the decrease in contrast sensitivity[3],[24]. But Wang et al[28] reported that changes in corneal aberrations did not correlate with the changes of contrast sensitivity at daytime and nighttime, with and without glare. In the current study, the changes of SA and RMS4 were negatively correlated with the changes of 1.5 and 3cpd contrast sensitivity while the reduction in 6 and 12cpd contrast sensitivity was correlated significantly with the increase of RMS3 in Wg-LASIK group 1 year after surgery. The results in conventional LASIK group were slightly different from the results in Wg-LASIK group. The reduction of corresponding spatial frequencies CS was correlated with the increase of coma, SA, RMS3 and decrease of RMS5.
Hence we can see that not all HOAs could reduce the contrast sensitivity, most components of the HOAs could reduce the contrast sensitivity, such as the coma, SA, RMS3 and RMS5, while a small number of components of aberrations would increase the contrast sensitivity, such as the RMS6. It further confirmed that the overall aberration was not a major factor for the changes of contrast sensitivity, and higher overall aberration did not mean lower contrast sensitivity, while the composition of the aberrations would play an important role on the changes of contrast sensitivity. On the whole, SA played a major role on contrast sensitivity preoperatively and these results were similar to the research of Moshirfar who reported SA was a major factor for changes of contrast sensitivity in a large dark adaptation pupil. And RMSh, coma and SA were the main factors on contrast sensitivity after surgery[29]. However, the correlation between higher-order aberrations and contrast sensitivity were far more complex than imagined. By analyzing the results of this study, we could note that the influence of every high-order aberrations on contrast sensitivity for every individual was different and it could be concluded that every component of higher-order aberrations was interacted and constrained with each other on the role of contrast sensitivity.
In conclusion, wavefront-guided LASIK with iris-registration is highly effective to improve spherical equivalent and contrast sensitivity and to get better visual performance compared with conventional LASIK. And the wavefront-guided LASIK with iris-registration is particularly suitable for eyes with high-magnitude RMSh. SA and RMS5 were primarily negatively correlated with the contrast sensitivity prior to surgery while increase of coma, SA, RMS3, RMS4 in Wg-LASIK and coma, RMS3 in conventional LASIK group were negatively correlated with reduction of contrast sensitivity one year after surgery.
REFERENCES
- 1.Sandoval HP, Fernandez de Castro LE, Vroman DT, Solomon KD. Refractive surgery survey 2004. J Cataract Refract Surg. 2005;31(1):221–233. doi: 10.1016/j.jcrs.2004.08.047. [DOI] [PubMed] [Google Scholar]
- 2.Oshika T, Miyata K, Tokunaga T, Samejima T, Amano S, Tanaka S, Hirohara Y, Mihashi T, Maeda N, Fujikado T. Higher-order wavefront aberrations of cornea and magnitude of refractive correction in laser in situ keratomileusis. Ophthalmology. 2002;109(6):1154–1158. doi: 10.1016/s0161-6420(02)01028-x. [DOI] [PubMed] [Google Scholar]
- 3.Marcos S. Aberrations and visual performance following standard laser vision correction. J Refract Surg. 2001;17(5):S596–S601. doi: 10.3928/1081-597X-20010901-19. [DOI] [PubMed] [Google Scholar]
- 4.Alió JL, Ortiz D, Muftuoglu O, Garcia MJ. Ten years after photorefractive keratectomy (PRK) and laser in situ keratomileusis (LASIK) for moderate to high myopia (control-matched study) Br J Ophthalmol. 2009;93(10):1313–1318. doi: 10.1136/bjo.2007.131748. [DOI] [PubMed] [Google Scholar]
- 5.McAlinden C, Moore JE. Comparison of higher order aberrations after LASIK and LASEK for myopia. J Refract Surg. 2010;26(1):45–51. doi: 10.3928/1081597X-20101215-07. [DOI] [PubMed] [Google Scholar]
- 6.Villarrubia A, Palacín E, Bains R, Gersol J. Comparison of custom ablation and conventional laser in situ keratomileusis for myopia and myopic astigmatism using the Alcon excimer laser. Cornea. 2009;28(9):971–975. doi: 10.1097/ICO.0b013e31819ce213. [DOI] [PubMed] [Google Scholar]
- 7.Kosaki R, Maeda N, Hayashi H, Fujikado T, Okamoto S. Effect of NIDEK optimized aspheric transition zone ablation profile on higher order aberrations during LASIK for myopia. J Refract Surg. 2009;25(4):331–338. doi: 10.3928/1081597X-20090401-06. [DOI] [PubMed] [Google Scholar]
- 8.Serrao S, Lombardo G, Ducoli P, Lombardo M. Optical performance of the cornea six years following photorefractive keratectomy for myopia. Invest Ophthalmol Vis Sci. 2011;52(2):846–857. doi: 10.1167/iovs.10-5905. [DOI] [PubMed] [Google Scholar]
- 9.Fares U, Suleman H, Al-Aqaba MA, Otri AM, Said DG, Dua HS. Efficacy, predictability, and safety of wavefront-guided refractive laser treatment: meta analysis. J Cataract Refract Surg. 2011;37(8):1465–1475. doi: 10.1016/j.jcrs.2011.02.029. [DOI] [PubMed] [Google Scholar]
- 10.Yamane N, Miyata K, Samejima T, Hiraoka T, Kiuchi T, Okamoto F, Hirohara Y, Mihashi T, Oshika T. Ocular higher-order aberrations and contrast sensitivity after conventional laser in situ keratomileusis. Invest Ophthalmol Vis Sci. 2004;45(11):3986–3990. doi: 10.1167/iovs.04-0629. [DOI] [PubMed] [Google Scholar]
- 11.Miraftab M, Seyedian MA, Hashemi H. Wavefront-guided vs wavefront-optimized LASIK: a randomized clinical trial comparing contralateral eyes. J Refract Surg. 2011;27(4):245–250. doi: 10.3928/1081597X-20100812-02. [DOI] [PubMed] [Google Scholar]
- 12.Awwad ST, Bowman RW, Cavanagh HD, McCulley JP. Wavefront-guided LASIK for myopia using the LADAR CustomCornea and the VISX CustomVue. J Refract Surg. 2007;23(1):26–38. doi: 10.3928/1081-597X-20070101-06. [DOI] [PubMed] [Google Scholar]
- 13.Lorente-Velázquez A, Nieto-Bona A, Collar CV, Mesa AG. Straylight and contrast sensitivity after corneal refractive therapy. Optom Vis Sci. 2011;88(10):1245–1251. doi: 10.1097/OPX.0b013e3182271449. [DOI] [PubMed] [Google Scholar]
- 14.Arbelaez MC, Aslanides IM, Barraquer C, Carones F, Feuermannova A, Neuhann T, Rozsival P. LASIK for myopia and astigmatism using the SCHWIND AMARIS excimer laser: an international multicenter trial. J Refract Surg. 2010;26(2):88–98. doi: 10.3928/1081597X-20100121-04. [DOI] [PubMed] [Google Scholar]
- 15.Kim TW, Wee WR, Lee JH, Kim MK. Contrast sensitivity after LASIK, LASEK, and wavefront-guided LASEK with the VISX S4 laser. J Refract Surg. 2007;23(4):355–361. doi: 10.3928/1081-597X-20070401-07. [DOI] [PubMed] [Google Scholar]
- 16.Thibos LN. Principles of Hartmann-Shack aberrometry. J Refract Surg. 2000;16(5):S563–565. doi: 10.3928/1081-597X-20000901-14. [DOI] [PubMed] [Google Scholar]
- 17.Bahar I, Levinger S, Kremer I. Wavefront-guided LASIK for myopia with the Technolas 217z: results at 3 years. J Refract Surg. 2007;23(6):586–591. doi: 10.3928/1081-597X-20070601-09. [DOI] [PubMed] [Google Scholar]
- 18.Kulkamthorn T, Silao JN, Torres LF, Lim JN, Purcell TL, Tantayakom T, Schanzlin DJ. Wavefront-guided laser in situ keratomileusis in the treatment of high myopia by using the CustomVue wavefront platform. Cornea. 2008;27(7):787–790. doi: 10.1097/ICO.0b013e31816a3554. [DOI] [PubMed] [Google Scholar]
- 19.Townley D, Kirwan C, O'Keefe M. One year follow-up of contrast sensitivity following conventional laser in situ keratomileusis and laser epithelial keratomileusis. Acta Ophthalmol. 2012;90(1):81–85. doi: 10.1111/j.1755-3768.2009.01822.x. [DOI] [PubMed] [Google Scholar]
- 20.Hori-Komai Y, Toda I, Yamamoto T, Tsubota K. Comparison of LASIK with the OPDCAT or OATz algorithm using the NIDEK EC5000CXII excimer laser. J Refract Surg. 2010;26(6):411–422. doi: 10.3928/1081597X-20090617-14. [DOI] [PubMed] [Google Scholar]
- 21.Mutyala S, McDonald MB, Scheinblum KA, Ostrick MD, Brint SF, Thompson H. Contrast sensitivity evaluation after laser in situ keratomileusis. Ophthalmology. 2000;107(10):1864–1867. doi: 10.1016/s0161-6420(00)00355-9. [DOI] [PubMed] [Google Scholar]
- 22.Chan JW, Edwards MH, Woo GC, Woo VC. Contrast sensitivity after laser in situ keratomileusis one-year follow-up. J Cataract Refract Surg. 2002;28(10):1774–1779. doi: 10.1016/s0886-3350(02)01499-2. [DOI] [PubMed] [Google Scholar]
- 23.Montés-Micó R, España E, Menezo JL. Mesopic contrast sensitivity function after laser in situ keratomileusis. J Refract Surg. 2003;19(5):353–356. doi: 10.3928/1081-597X-20030501-13. [DOI] [PubMed] [Google Scholar]
- 24.Neeracher B, Senn P, Schipper I. Glare sensitivity and optical side effects 1 year after photorefractive keratectomy and laser in situ keratomileusis. J Cataract Refract Surg. 2004;30(8):1696–1701. doi: 10.1016/j.jcrs.2003.12.058. [DOI] [PubMed] [Google Scholar]
- 25.Ghosh S, Couper TA, Lamoureux E, Jhanji V, Taylor HR, Vajpayee RB. Evaluation of iris recognition system for wavefront-guided laser in situ keratomileusis for myopic astigmatism. J Cataract Refract Surg. 2008;34(2):215–221. doi: 10.1016/j.jcrs.2007.09.022. [DOI] [PubMed] [Google Scholar]
- 26.Zhang J, Zhou YH, Wang NL, Li R. Comparison of visual performance between conventional LASIK and wavefront-guided LASIK with iris-registration. Chin Med J (Engl) 2008;121(2):137–142. [PubMed] [Google Scholar]
- 27.Padmanabhan P, Mrochen M, Basuthkar S, Viswanathan D, Joseph R. Wavefront-guided versus wavefront-optimized laser in situ keratomileusis: contralateral comparative study. J Cataract Refract Surg. 2008;34(3):389–397. doi: 10.1016/j.jcrs.2007.10.028. [DOI] [PubMed] [Google Scholar]
- 28.Wang IJ, Sum YC, Lee YC, Hon YC, Hu FR. The relationship between anterion lorneed aberration and contrast sensitivity in conventional LASIK. Curr Eye Res. 2006;31(5):563–568. doi: 10.1080/02713680600814761. [DOI] [PubMed] [Google Scholar]
- 29.Moshirfar M, Schliesser JA, Chang JC, Oberg TJ, Mifflin MD, Townley R, Livingston MK, Kurz CJ. Visual outcomes after wavefront-guided photorefractive keratectomy and wavefront-guided laser in situ keratomileusis: Prospective comparison. J Cataract Refract Surg. 2010;36(8):1336–1343. doi: 10.1016/j.jcrs.2010.02.012. [DOI] [PubMed] [Google Scholar]