Abstract
AIM
To evaluate the possible effects of phacoemulsification cataract surgery on ocular hemodynamics.
METHODS
In this prospective study, intraocular pressure (IOP), pulsatile ocular blood flow (POBF), and ocular pulse amplitude (OPA) were measured pre-operatively (baseline) and at 1 week and 3 weeks postoperation in 52 eyes of 26 patients (mean age 63.15±10.25 years) scheduled for unilateral phacoemulsification cataract surgery with intraocular lens implantation. In all of the eyes, a blood flow analyzer (Paradigm DICON; Paradigm Medical Industries Inc.; USA) was used to obtain measurements of IOP, POBF, and OPA. The data obtained from operated eyes were compared statistically to untreated fellow phakic eyes of the patients.
RESULTS
For operated eyes, the mean baseline IOP, POBF, and OPA values were 15.9±4.64mmHg, 17.41±4.84µL/s, and 2.91±1.12mmHg, respectively. The IOP, POBF, and OPA values were 17.19±4.34mmHg, 17.56±6.46µL/s, and 3.12±1.1mmHg, respectively, in the nonoperated control eyes. Statistically significant differences from baseline measurements were not observed 1 week and 3 weeks postoperation for the operated or nonoperated eyes. There were also no statistically significant differences in any measurements between the operated and nonoperated eyes in all the examination periods (P>0.05 for all).
CONCLUSION
Uncomplicated phacoemulsification surgery does not affect ocular hemodynamics in normotensive eyes with cataracts.
Keywords: cataract, cataract extraction, intraocular pressure, phacoemulsification, regional blood flow
INTRODUCTION
Intraocular pressure (IOP) and ocular volume changes occur depending on the blood flow variations related to the stage of the cardiac cycle. Based on this information, tools have been developed to calculate the pulsatile ocular blood flow (POBF) by deriving data from continuously monitored IOP values[1],[2]. The POBF is thought to be caused by the blood volume pumped into the eye primarily in the choriocapillary layer during each cardiac cycle. Therefore, the POBF may only be affected by IOP changes due to low choroidal vascular autoregulation[3]-[5].
POBF is responsible for the pathogenesis of many diseases in the eyes. A variety of recent studies evaluated POBF changes in several diseases such as glaucoma, age-related macular degeneration, diabetic retinopathy, and Graves ophthalmopathy[3],[6]-[11]. Furthermore, in a study performed by Hopkins[12], the POBF values in cases with cataracts were decreased compared with healthy cases.
In recent years, the success ratio in cataract surgery has significantly increased as a result of advances in surgical methods and equipment[13]-[16]. The effects of cataract surgery on ocular hemodynamics were analyzed in several previous studies. However, these studies reported conflicting results. Whether ocular hemodynamics changes are caused by IOP changes or changes in existing autoregulation mechanisms in cases with cataracts has not been determined[5],[12],[17],[18]. Moreover, POBF values can be affected by demographic factors such as age, gender, IOP, corneal thickness, and refraction error[19]-[22]. Therefore, this study was designed to prospectively evaluate ocular hemodynamics in patients with cataracts to elucidate the effects of phacoemulsification surgery on ocular hemodynamics rather than comparing measurements from different individuals subjected to phacoemulsification surgery.
SUBJECTS AND METHODS
Subjects
This prospective clinical study was performed at the Karadeniz Technical University, School of Medicine, Trabzon, Turkey. The consent of the Medical Ethical Committee was obtained for the study protocol. All patients provided written informed consent to participate. The tenets of the Declaration of Helsinki were followed.
All the patients included in the study provided written consent after being informed about the study plan. The patients included in the study had no ophthalmological diseases besides uncomplicated cataracts of Grade II-III based on the Emery Classification[23]. The following exclusion criteria were used in the study; high-degree myopia (≥6.00 diopters), a single eye, ocular hypertension, glaucoma, pseudoexfoliation, uveitis, and a history of previous surgery for either eye. The cases in which complications occurred during phacoemulsification surgery, and the cases in which cortical material or ocular viscoelastic devices used in the operation could not be completely cleaned were excluded from the study.
The study included 52 eyes belonging to 26 patients. All the patients underwent a detailed ophthalmologic examination before surgery. A foldable posterior chamber lens was implanted into a single eye of all the patients by applying phacoemulsification surgery with a 3.25mm superior clear corneal incision using the same method.
Methods
Ocular blood flow measurements
During the study, ocular blood flow measurements were performed three times in each of both eyes of the patients. The first measurement was performed one day before the cataract surgery (baseline), the second measurement was performed one week after the cataract surgery, and the third measurement was performed three weeks after the cataract surgery. The measurements were performed in all the patients in a sitting position because the ocular blood flow is affected by the body posture[24]. Local anesthesia was administered into the eyes in which the measurements were performed using one drop of 0.5% proparacaine (Alcaine; Alcon Laboratories Inc., Fort Worth, TX, USA) into the conjunctival sac. The blood flow measurements were performed five minutes after local anesthesia was administered using a blood flow analyzer. The same device (Paradigm DICON Blood Flow Analyzer; Paradigm Medical Industries Inc.; Salt Lake City, Utah; USA) was used in the blood flow and IOP measurements of all the eyes. All the measurements were performed by the same investigator using disposable probes contacting the central cornea. Five sequential ocular blood flow measurements performed within approximately 20s were recorded by the device, and detailed device printouts were recorded. The mean intraocular pressure (IOP; mmHg), pulsatile ocular blood flow (POBF; µL/s), and ocular pulse amplitude (OPA; mmHg) values for each measurement were recorded.
Statistical Analysis
The measurement data of the operated eyes (Group 1) and the nonoperated control eyes (Group 2) of the patients are presented as mean±standard deviation. Repeated measures of variance analysis were used to compare the repeated measurements within the group, and independent-sample t-tests were used to compare the measurements between the groups. The relationship between the measurements was analyzed using Pearson correlation analysis. P<0.05 was assumed to be statistically significant.
RESULTS
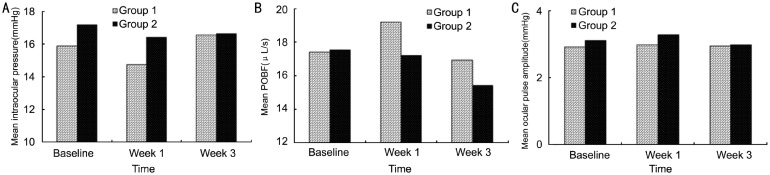
The mean age of the patients (12 female, 14 male) included in the study was 63.15±10.25 years. In baseline examination, there were no clinical signs of shallow anterior chamber and narrow angle in both operated and control eyes. They had deep anterior chambers and wide angles. For group 1, the mean baseline IOP, POBF, and OPA values were 15.9±4.64mmHg, 17.41±4.84µL/s, and 2.91±1.12mmHg, respectively. The mean baseline IOP, POBF, and OPA values were 17.19±4.34mmHg, 17.56±6.46µL/s, and 3.12±1.1mmHg, respectively, for group 2 (control). No statistically significant variation was found within any group compared with the baseline measurements (P>0.05 for all) in the postoperative measurements repeated at week one and week three. No groups showed any significant differences between the measurements performed postoperatively on week one and week three (P>0.05 for all). There were also no statistically significant differences in any of the measurements between the groups for the entire study period (P>0.05 for all) (Figure 1, Tables 1, 2).
Figure 1. Comparison of measurement results obtained at various times in eyes undergoing phacoemulsification surgery (group 1) and in eyes without undergoing phacoemulsification surgery (group 2).
A: IOP; B: POBF; C: OPA.
Table 1. Comparison of the measurement results obtained at various times with the blood flow analyzer device in eyes undergoing phacoemulsification surgery (group 1) and in eyes without undergoing phacoemulsification surgery (group 2).
| Time | Group | IOP (mmHg) | POBF (µL/s) | OPA (mmHg) |
| Preop. | 1 | 15.9±4.64 | 17.41±4.84 | 2.91±1.12 |
| 2 | 17.19±4.34 | 17.56±6.46 | 3.12±1.1 | |
| 1P | 0.753 | 0.278 | 0.511 | |
| Postop. 1 week |
1 | 14.75±4.55 | 19.2±6.03 | 2.99±0.94 |
| 2 | 16.42±2.96 | 17.21±4.8 | 3.28±0.76 | |
| 1P | 0.125 | 0.194 | 0.223 | |
| Postop. 3 weeks |
1 | 16.55±4.62 | 16.93±4.82 | 2.95±0.99 |
| 2 | 16.66±3.05 | 15.4±4.4 | 2.99±0.86 | |
| 1P | 0.916 | 0.236 | 0.882 |
IOP: Intraocular pressure; POBF: Pulsatile ocular blood flow; OPA: Ocular pulse amplitude; 1Independent samples t-test.
Table 2. Comparison of the repeated measurement results obtained with the blood flow analyzer device in eyes undergoing phacoemulsification surgery (group 1) and in eyes without undergoing phacoemulsification surgery (group 2).
| Group | Time | IOP (mmHg) | POBF (µL/s) | OPA (mmHg) |
| 1 | Preop. | 15.9±4.64 | 17.41±4.84 | 2.91±1.12 |
| Postop. 1 week |
14.75±4.55 | 19.2±6.03 | 2.99±0.94 | |
| Postop. 3 weeks |
16.55±4.62 | 16.93±4.82 | 2.95±0.99 | |
| 1P | 0.17 | 0.26 | 0.936 | |
| 2 | Preop. | 17.19±4.34 | 17.56±6.46 | 3.12±1.1 |
| Postop. 1 week |
16.42±2.96 | 17.21±4.8 | 3.28±0.76 | |
| Postop. 3 weeks |
16.66±3.05 | 15.4±4.4 | 2.99±0.86 | |
| 1P | 0.33 | 0.164 | 0.206 |
IOP: Intraocular pressure; POBF: Pulsatile ocular blood flow; OPA: Ocular pulse amplitude; 1Repeated measures of variance analysis.
Correlation analyses of the measurement parameters are presented in Table 3. IOP and POBF values of group 1 had significant positive correlation for preoperative and post operative first week only, while this correlation was significant for only postoperative first week in group 2. The correlation between POBF and OPA was significant only for preoperative period and postoperative 3rd week for the group 1, while this correlations were significant for all measurement points for the group 2. When the entire study group (n=52) was considered, a statistically significant correlation was observed between IOP and POBF for all the measurement periods (for the preoperative period: r=-0.37, P=0.007; for week 1 postoperation: r=-0.564, P<0.0001; and for week 3 postoperation: r=-0.348, P=0.012. Statistically significant positive correlations were observed between the groups for POBF and OPA for all the measurement periods (for the preoperative period: r=0.573, P<0.0001; for week 1 postoperation: r=0.285, P<0.04; and for week 3 postoperation: r=0.525, P<0.0001. The relationship between IOP and OPA was not statistically significant for all the study periods.
Table 3. Correlation analyses of the measurement results obtained at various time periods with the blood flow analyzer device in eyes undergoing phacoemulsification surgery (group 1) and in eyes without undergoing phacoemulsification surgery (group 2).
| Time | Group | POBF |
OPA |
||||
| r | 1P | r | 1P | ||||
| Preop. | 1 | IOP | -0.455 | 0.019 | 0.105 | 0.608 | |
| POBF | 1 | 0.508 | 0.008 | ||||
| 2 | IOP | -0.324 | 0.106 | -0.077 | 0.708 | ||
| POBF | 1 | 0.635 | <0.0001 | ||||
| Postop. 1 week |
1 | IOP | -0.554 | 0.003 | 0.072 | 0.727 | |
| POBF | 1 | 0.284 | 0.159 | ||||
| 2 | IOP | -0.539 | 0.004 | 0.158 | 0.44 | ||
| POBF | 1 | 0.394 | 0.047 | ||||
| Postop. 3 weeks |
1 | IOP | -0.349 | 0.08 | 0.308 | 0.126 | |
| POBF | 1 | 0.528 | 0.006 | ||||
| 2 | IOP | -0.363 | 0.068 | 0.071 | 0.73 | ||
| POBF | 1 | 0.547 | 0.004 | ||||
1Pearson correlation analysis.
DISCUSSION
The IOP-lowering effect of cataract surgery has been reported in the literature[25]-[27]. The effect is believed to result from the widening of the anterior chamber[28], [29]. In a study performed by Bhallil et al[30], the mean IOP decreased by 2.1mmHg at day 15 and 2.26mmHg at month 1 postoperation after a phacoemulsification surgery compared with the preoperative period. Although the postoperative mean IOP change in our study was not statistically significant, the change was -1.15mmHg at day 7 and 0.65mmHg at week 3. The anterior chamber biometric factors possibly contributed to the IOP decrease after phacoemulsification[31]. Therefore, the lack of a significant IOP decrease in our cases may be due to the diversity of the group properties. All eyes included our study had deep anterior chambers and wide angles. In a study by Rainer et al[18], no significant change was observed in the IOP levels in the first one-month period after cataract surgery.
Several studies have focused on alteration in the ocular hemodynamics after cataract surgery. In a study by Hopkins[12], the POBF values of pseudophakic eyes that underwent cataract surgery were lower compared with the healthy control group. A study by Hilton et al[5] compared the POBF examinations of 25 cataract patients with the POBF examinations of 25 control cases from the same age group. The POBF values of the cases in the cataract group were significantly lower both preoperatively and postoperatively at the first month compared with the POBF values of the control group. The IOP values decreased and the POBF values increased by 8.3% after cataract surgery in the same study. In our study, 52 eyes of 26 patients were included, and the other eyes of the same patients were chosen as the control group. Thus, personal differences that may affect the POBF measurements were reduced. In our study, no significant difference was found between the eyes undergoing cataract operations and phakic eyes regarding the POBF and IOP values both preoperatively and postoperatively. POBF values can be affected by personal factors such as gender, age, corneal thickness, IOP, refractive errors and systemic hypertension[19]-[22],[32]-[34]. The results of our study likely differ from the results of Hilton et al[5] because we used unoperated eyes from the same patient as controls rather than healthy individuals from a similar age group. We also found that the IOP decreased, and the POBF increased[5],[35],[36]. A statistically significant negative correlation was determined between the IOP and POBF levels in our study.
In a study performed by Spraul et al[17], the POBF changes in 51 patients that underwent cataract surgery were compared with the healthy eyes of the same cases, which is similar to our study design. However, the POBF values measured postoperatively on day 3 decreased in the eyes that underwent cataract surgery, while there was no significant change in the control group. The study reported that no significant change in the IOP occurred both in the surgery group and the control group at day 3. The POBF decrease at day 3 in the eyes that underwent cataract surgery disappeared at the end of the first year. It was suggested that temporary hemodynamics disorders may have developed due to a neural mechanism induced by the cataract surgery[17]. In our study, we performed measurements one week after the surgery to prevent possible POBF measurement distortion arising from corneal thickness and biomechanical changes secondary to cataract surgery. Because previous studies reported that improvement of biomechanical changes secondary to phacoemulsification surgery by post-operative first week [37], [38].
In another study performed using the laser interferometric method, Rainer et al[18] examined the effect of the surgical treatment on the pulsatile choroidal blood flow in 33 cataract cases. Similar to our study, the aforementioned study also reported that no significant change occurred in the ocular blood flow according to the postoperative first-week and first-month measurements[18].
In a study conducted by Plange et al[39], the effect of cataract surgery on the OPA was examined. Plange et al[39] used different devices to measure the OPA and performed OPA measurements one day before and after the cataract surgery. They concluded that the OPA changes were associated with IOP changes[39]. Similar to this study, a correlation between the OPA and IOP was also observed in a study conducted by Breusegem et al[40] reported that the OPA decreased along with decreases of the IOP. In another study including 311 cataract patients, OPA and IOP measurements were performed one week before and two week after cataract surgery, and a positive correlation between the OPA and IOP was observed[41]. In contrast to the aforementioned studies, we did not observe any relationship between the OPA and IOP, which may be due to the small number of study cases, individual factors in our cases, or the use of a different device. Another important factor may be the lack of a difference between the IOP measurements in all the study periods in our study.
The main result of our study is that the effect of phacoemulsification surgery on ocular hemodynamics in the first three-week period was not significant in normotensive eyes with cataracts. Because POBF is representative of choroidal blood flow, our results suggest that choroidal circulation was not affected by the uncomplicated phacoemulsification surgery.
REFERENCES
- 1.Silver DM, Farrell RA, Langham ME, O'Brien V, Schilder P. Estimation of pulsatile ocular blood flow from intraocular pressure. Acta Ophthalmol Suppl. 1989;191:25–29. doi: 10.1111/j.1755-3768.1989.tb07083.x. [DOI] [PubMed] [Google Scholar]
- 2.Silver DM, Farrell RA. Validity of pulsatile ocular blood flow measurements. Surv Ophthalmol. 1994;38:S72–80. doi: 10.1016/0039-6257(94)90049-3. [DOI] [PubMed] [Google Scholar]
- 3.Savage HI, Hendrix JW, Peterson DC, Young H, Wilkinson CP. Differences in pulsatile ocular blood flow among three classifications of diabetic retinopathy. Invest Ophthalmol Vis Sci. 2004;45(12):4504–4509. doi: 10.1167/iovs.04-0077. [DOI] [PubMed] [Google Scholar]
- 4.Langham ME, Farrell RA, O'Brien V, Silver DM, Schilder P. Blood flow in the human eye. Acta Ophthalmol Suppl. 1989;191:9–13. doi: 10.1111/j.1755-3768.1989.tb07080.x. [DOI] [PubMed] [Google Scholar]
- 5.Hilton EJ, Hosking SL, Gherghel D, Embleton S, Cunliffe IA. Beneficial effects of small-incision cataract surgery in patients demonstrating reduced ocular blood flow characteristics. Eye (Lond) 2005;19(6):670–675. doi: 10.1038/sj.eye.6701620. [DOI] [PubMed] [Google Scholar]
- 6.Geyer O, Neudorfer M, Snir T, Goldstein M, Rock T, Silver DM, Bartov E. Pulsatile ocular blood flow in diabetic retinopathy. Acta Ophthalmol Scand. 1999;77(5):522–525. doi: 10.1034/j.1600-0420.1999.770507.x. [DOI] [PubMed] [Google Scholar]
- 7.Janulevičiene I, Ehrlich R, Siesky B, Nedzelskienė I, Harris A. Evaluation of hemodynamic parameters as predictors of glaucoma progression. J Ophthalmol. 2011;2011:164320. doi: 10.1155/2011/164320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Janulevicienë I, Harris A, Kagemann L, Siesky B, McCranor L. A comparison of the effects of dorzolamide/timolol fixed combination versus latanoprost on intraocular pressure and pulsatile ocular blood flow in primary open-angle glaucoma patients. Acta Ophthalmol Scand. 2004;82(6):730–737. doi: 10.1111/j.1600-0420.2004.00358.x. [DOI] [PubMed] [Google Scholar]
- 9.Sandhu R, Sivaprasad S, Shah SP, Adewoyin T, Chong NV. Pulsatile ocular blood flow in asymmetric age-related macular degeneration. Eye (Lond) 2007;21(4):506–511. doi: 10.1038/sj.eye.6702242. [DOI] [PubMed] [Google Scholar]
- 10.Chen SJ, Cheng CY, Lee AF, Lee FL, Hsu WM, Liu JH. Pulsatile ocular blood flow of choroidal neovascularization in asymmetric age-related macular degeneration after transpupillary thermotherapy. Eye (Lond) 2004;18(6):595–599. doi: 10.1038/sj.eye.6700723. [DOI] [PubMed] [Google Scholar]
- 11.Tsai CC, Kau HC, Tsai HH, Kao SC, Hsu WM. Pulsatile ocular blood flow change after treatment with systemic steroid in patients with Graves' ophthalmopathy. Eye (Lond) 2006;20(9):1025–1029. doi: 10.1038/sj.eye.6702070. [DOI] [PubMed] [Google Scholar]
- 12.Hopkins SD. Ocular haemodynamics in cataractous eyes. A pilot study. Acta Ophthalmol Suppl. 1989;191:43–48. doi: 10.1111/j.1755-3768.1989.tb07087.x. [DOI] [PubMed] [Google Scholar]
- 13.Rainer G, Menapace R, Findl O, Kiss B, Petternel V, Georgopoulos M, Schneider B. Intraocular pressure rise after small incision cataract surgery: a randomised intraindividual comparison of two dispersive viscoelastic agents. Br J Ophthalmol. 2001;85(2):139–142. doi: 10.1136/bjo.85.2.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yang H, Zheng D, Huang J, Huang Y, Zhang Z. The clinical study of Healon 5 in phacoemulsification and IOL implantation. Yan Ke Xue Bao. 2001;17(3):186–190. [PubMed] [Google Scholar]
- 15.Franchini A, Frosini S, Boddi V. Standard coaxial phaco vs microincision cataract surgery: a corneal endothelium study. Int J Ophthalmol. 2008;1(4):344–350. [Google Scholar]
- 16.Jiang T, Jiang J, Zhou Y, Zhao GQ, Li H, Zhao SY. Cataract surgery in aged patients: phacoemulsification or small-incision extracapsular cataract surgery. Int J Ophthalmol. 2011;4(5):513–518. doi: 10.3980/j.issn.2222-3959.2011.05.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Spraul CW, Amann J, Lang GE, Lang GK. Effect of cataract extraction with intraocular lens implantation on ocular hemodynamics. J Cataract Refract Surg. 1996;22(8):1091–1096. doi: 10.1016/s0886-3350(96)80123-4. [DOI] [PubMed] [Google Scholar]
- 18.Rainer G, Kiss B, Dallinger S, Menapace R, Findl O, Schmetterer K, Georgopoulos M, Schmetterer L. Effect of small incision cataract surgery on ocular blood flow in cataract patients. J Cataract Refract Surg. 1999;25(7):964–968. doi: 10.1016/s0886-3350(99)00077-2. [DOI] [PubMed] [Google Scholar]
- 19.Benavente-Pérez A, Hosking SL, Logan NS, Broadway DC. Ocular blood flow measurements in healthy human myopic eyes. Graefes Arch Clin Exp Ophthalmol. 2010;248(11):1587–1594. doi: 10.1007/s00417-010-1407-9. [DOI] [PubMed] [Google Scholar]
- 20.Gunvant P, Baskaran M, Vijaya L, Joseph IS, Watkins RJ, Nallapothula M, Broadway DC, O'Leary DJ. Effect of corneal parameters on measurements using the pulsatile ocular blood flow tonograph and Goldmann applanation tonometer. Br J Ophthalmol. 2004;88(4):518–522. doi: 10.1136/bjo.2003.019331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saleh TA, Adams M, McDermott B, Claridge KG, Ewings P. Effects of central corneal thickness and corneal curvature on the intraocular pressure measurement by Goldmann applanation tonometer and ocular blood flow pneumatonometer. Clin Experiment Ophthalmol. 2006;34(6):516–520. doi: 10.1111/j.1442-9071.2006.01266.x. [DOI] [PubMed] [Google Scholar]
- 22.Ravalico G, Toffoli G, Pastori G, Crocè M, Calderini S. Age-related ocular blood flow changes. Invest Ophthalmol Vis Sci. 1996;37(13):2645–2650. [PubMed] [Google Scholar]
- 23.Emery JM. Kelman phacoemulsification; Emery technique. In: Emery JM, McIntyre DJ, editors. Extracapsular Cataract Surgery. St Louis: MO, CV Mosby; 1983. pp. 95–100. [Google Scholar]
- 24.Kothe AC. The effect of posture on intraocular pressure and pulsatile ocular blood flow in normal and glaucomatous eyes. Surv Ophthalmol. 1994;38:S191–197. doi: 10.1016/0039-6257(94)90066-3. [DOI] [PubMed] [Google Scholar]
- 25.Tennen DG, Masket S. Short-and long-term effect of clear corneal incisions on intraocular pressure. J Cataract Refract Surg. 1996;22(5):568–570. doi: 10.1016/s0886-3350(96)80010-1. [DOI] [PubMed] [Google Scholar]
- 26.Shingleton BJ, Gamell LS, O'Donoghue MW, Baylus SL, King R. Long-term changes in intraocular pressure after clear corneal phacoemulsification: normal patients versus glaucoma suspect and glaucoma patients. J Cataract Refract Surg. 1999;25(7):885–890. doi: 10.1016/s0886-3350(99)00107-8. [DOI] [PubMed] [Google Scholar]
- 27.Schwenn O, Dick HB, Krummenauer F, Krist R, Pfeiffer N. Intraocular pressure after small incision cataract surgery: temporal sclerocorneal versus clear corneal incision. J Cataract Refract Surg. 2001;27(3):421–425. doi: 10.1016/s0886-3350(00)00577-0. [DOI] [PubMed] [Google Scholar]
- 28.Greve EL. Primary angle closure glaucoma: extracapsular cataract extraction or filtering procedure? Int Ophthalmol. 1988;12(3):157–162. doi: 10.1007/BF00129999. [DOI] [PubMed] [Google Scholar]
- 29.Yang CH, Hung PT. Intraocular lens position and anterior chamber angle changes after cataract extraction in eyes with primary angle-closure glaucoma. J Cataract Refract Surg. 1997;23(7):1109–1113. doi: 10.1016/s0886-3350(97)80089-2. [DOI] [PubMed] [Google Scholar]
- 30.Bhallil S, Andalloussi IB, Chraibi F, Daoudi K, Tahri H. Changes in intraocular pressure after clear corneal phacoemulsification in normal patients. Oman J Ophthalmol. 2009;2(3):111–113. doi: 10.4103/0974-620X.57309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Huang G, Gonzalez E, Lee R, Chen YC, He M, Lin SC. Association of biometric factors with anterior chamber angle widening and intraocular pressure reduction after uneventful phacoemulsification for cataract. J Cataract Refract Surg. 2012;38(1):108–116. doi: 10.1016/j.jcrs.2011.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fontana L, Poinoosawmy D, Bunce CV, O'Brien C, Hitchings RA. Pulsatile ocular blood flow investigation in asymmetric normal tension glaucoma and normal subjects. Br J Ophthalmol. 1998;82(7):731–736. doi: 10.1136/bjo.82.7.731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mori F, Konno S, Hikichi T, Yamaguchi Y, Ishiko S, Yoshida A. Factors affecting pulsatile ocular blood flow in normal subjects. Br J Ophthalmol. 2001;85(5):529–530. doi: 10.1136/bjo.85.5.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Esgin H, Alimgil ML, Erda S. The effect of systemic hypertension on pulsatile ocular blood flow in diabetic patients. Acta Ophthalmol Scand. 2001;79(2):160–162. doi: 10.1034/j.1600-0420.2001.079002160.x. [DOI] [PubMed] [Google Scholar]
- 35.Quaranta L, Manni G, Donato F, Bucci MG. The effect of increased intraocular pressure on pulsatile ocular blood flow in low tension glaucoma. Surv Ophthalmol. 1994;38:S177–181. doi: 10.1016/0039-6257(94)90064-7. [DOI] [PubMed] [Google Scholar]
- 36.Dastiridou AI, Ginis HS, De Brouwere D, Tsilimbaris MK, Pallikaris IG. Ocular rigidity, ocular pulse amplitude, and pulsatile ocular blood flow: the effect of intraocular pressure. Invest Ophthalmol Vis Sci. 2009;50(12):5718–5722. doi: 10.1167/iovs.09-3760. [DOI] [PubMed] [Google Scholar]
- 37.Salvi SM, Soong TK, Kumar BV, Hawksworth NR. Central corneal thickness changes after phacoemulsification cataract surgery. J Cataract Refract Surg. 2007;33(8):1426–1428. doi: 10.1016/j.jcrs.2007.04.010. [DOI] [PubMed] [Google Scholar]
- 38.Kamiya K, Shimizu K, Ohmoto F, Amano R. Evaluation of corneal biomechanical parameters after simultaneous phacoemulsification with intraocular lens implantation and limbal relaxing incisions. J Cataract Refract Surg. 2011;37(2):265–270. doi: 10.1016/j.jcrs.2010.08.045. [DOI] [PubMed] [Google Scholar]
- 39.Plange N, Rennings C, Herr A, Weber A, Roessler GF, Mazinani BE, Kaup M, Remky A. Ocular pulse amplitude before and after cataract surgery. Curr Eye Res. 2012;37(2):115–119. doi: 10.3109/02713683.2011.626910. [DOI] [PubMed] [Google Scholar]
- 40.Breusegem C, Fieuws S, Zeyen T, Stalmans I. The effect of trabeculectomy on ocular pulse amplitude. Invest Ophthalmol Vis Sci. 2010;51(1):231–235. doi: 10.1167/iovs.09-3712. [DOI] [PubMed] [Google Scholar]
- 41.Tabuchi H, Kiuchi Y, Ohsugi H, Nakakura S, Han Z. Effects of corneal thickness and axial length on intraocular pressure and ocular pulse amplitude before and after cataract surgery. Can J Ophthalmol. 2011;46(3):242–246. doi: 10.1016/j.jcjo.2011.05.015. [DOI] [PubMed] [Google Scholar]