Abstract
The 13th St Gallen International Breast Cancer Conference (2013) Expert Panel reviewed and endorsed substantial new evidence on aspects of the local and regional therapies for early breast cancer, supporting less extensive surgery to the axilla and shorter durations of radiation therapy. It refined its earlier approach to the classification and management of luminal disease in the absence of amplification or overexpression of the Human Epidermal growth factor Receptor 2 (HER2) oncogene, while retaining essentially unchanged recommendations for the systemic adjuvant therapy of HER2-positive and ‘triple-negative’ disease. The Panel again accepted that conventional clinico-pathological factors provided a surrogate subtype classification, while noting that in those areas of the world where multi-gene molecular assays are readily available many clinicians prefer to base chemotherapy decisions for patients with luminal disease on these genomic results rather than the surrogate subtype definitions. Several multi-gene molecular assays were recognized as providing accurate and reproducible prognostic information, and in some cases prediction of response to chemotherapy. Cost and availability preclude their application in many environments at the present time. Broad treatment recommendations are presented. Such recommendations do not imply that each Panel member agrees: indeed, among more than 100 questions, only one (trastuzumab duration) commanded 100% agreement. The various recommendations in fact carried differing degrees of support, as reflected in the nuanced wording of the text below and in the votes recorded in supplementary Appendix S1, available at Annals of Oncology online. Detailed decisions on treatment will as always involve clinical consideration of disease extent, host factors, patient preferences and social and economic constraints.
Keywords: surgery, radiation therapy, systemic adjuvant therapies, early breast cancer, St Gallen Consensus, subtypes
introduction
The 2 years since the 2011 St Gallen Consensus [1] have seen substantial progress in evidence relevant to various aspects of the treatment of early invasive breast cancer. The genomic atlas of the disease [2] has emphasized its heterogeneity, and suggested that genomic studies may potentially inform treatment decisions such as the use of aromatase inhibitors [3, 4]. Further data became available reducing the necessity for axillary dissection [5, 6]. Studies presented at the 2012 ESMO meeting clarified the optimal duration of adjuvant trastuzumab in HER2-positive disease [7, 8]. The duration of adjuvant tamoxifen was addressed by the ATLAS study, which suggested a significant benefit for extending such treatment to 10 years rather than 5 years [9].
St Gallen 2013: news and progress
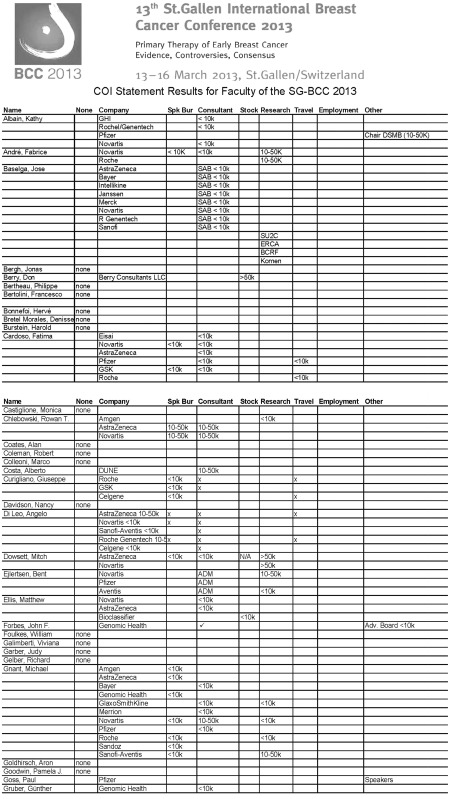
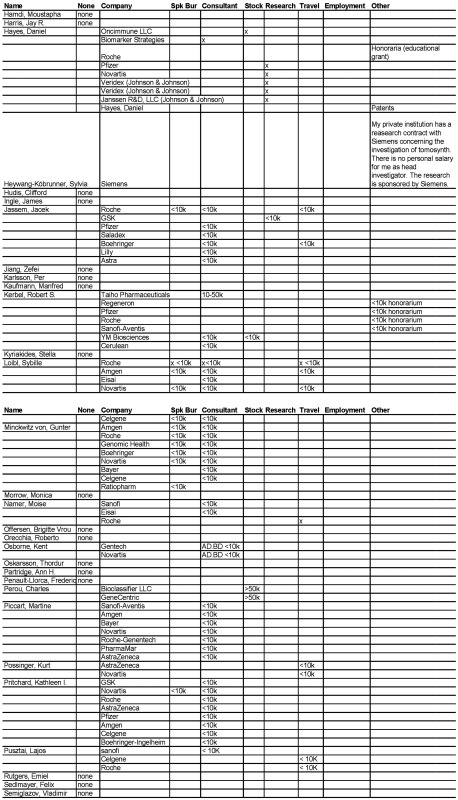
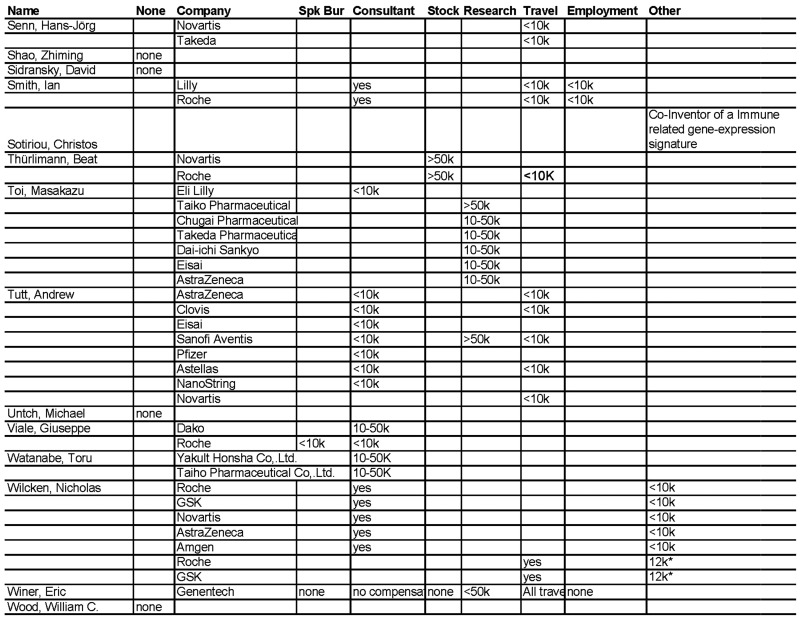
The 13th International Breast Cancer Conference held in St Gallen in March 2013 involved some 3700 participants from 95 countries and heard presentations from a faculty widely representative of disciplines and geographical areas. An Expert Panel, which included 51 members from 21 countries, chaired by Aron Goldhirsch and Eric P. Winer met at the conclusion of the conference to review the new information presented and consider treatment recommendations for broad application over the next 2 years. As in the past, this conference included an explicit approach to management of conflicts of interest (see Appendix 2).
Table 1 summarizes the information presented during the conference.
Table 1.
Recent research findings presented at the 13th International Conference on Primary Therapy of Early Breast Cancer and their implications for patient care
| Field or treatment | Status of research/implications for patient care |
|---|---|
| Targeted treatments | Proof of concept of mTOR pathway inhibition in metastatic disease was provided by the Bolero study [10]. The PI3K-alpha inhibitors, such as GDC-0032, have shown strong interaction with ER signalling in laboratory studies. Another PI3K-alpha inhibitor, BYL719, showed preclinical evidence of synergy with fulvestrant. The strong preclinical evidence for favourable interaction between endocrine therapy and various inhibitors of the PI3 kinase pathway (AKT inhibitors or MEK inhibitors) points to the need for clinical trials of such combinations [11]. In triple-negative breast cancer, PI3K inhibition impairs BRCA1/2 expression, thus sensitizing cells to PARP inhibition [12, 13]. |
| A frequently mutated gene is TP53, which is abnormal in the majority of cases of HER2 overexpressing and triple-negative disease [2, 14]. Although, p53 has been studied for decades, its clinical utility remains limited due to the absence of standardization and the heterogeneity of the studies. Wild-type p53 activity impairs the preclinical response to anthracyclines [15], and there is an interaction with ER such that ER prevents p53-dependent apoptosis [16]. However, p53 was not predictive of preferential sensitivity to an anthracycline-based versus a taxane-based chemotherapy in a large phase III neoadjuvant study [17]. | |
| Messages from the EBCTCG Overview | The Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) meta-analysis showed efficacy of adjuvant chemotherapy compared with no chemotherapy, superiority of anthracycline-based regimens over CMF and of taxane-containing regimens over those based on anthracycline. The relative magnitude of benefit from anthracycline or anthracycline-taxane combinations resulted in similar reductions of breast cancer mortality irrespective of age, stage, histopathological grade and ER status, although the absolute gain for a low disease burden Luminal A-type of cancer will be very small [18, 19]. |
| Mutational analysis of breast cancer | Detailed analysis of the entire genome of breast cancers offers the potential for more precisely personalizing therapy [20]. Application is currently limited by the availability of suitably targeted therapeutic agents and by limited understanding of the roles and functions of many of the identified abnormalities, and clarification of which genomic alterations are functional and which are merely passenger mutations. |
| Personalizing treatment | Analytic validity, clinical (or biologic) validity, and clinical utility are all required for optimal clinical application of tumour biomarkers [21]. |
| Intrinsic subtypes | Identification of intrinsic subtypes is most precise using molecular technologies [22]. Where such assays are unavailable, surrogate definitions of subtype can be obtained by IHC measurements of ER, PgR, Ki-67 and HER2 with in situ hybridization confirmation, where appropriate [23]. Moderate or strong expression of PgR has been proposed as an additional restriction in the surrogate definition of ‘Luminal A-like’ disease [24]. Ki-67 level as a marker of proliferation is also important for this distinction [23]. Both of these markers require quality control. In particular, Ki-67 measurement is not currently standardized among laboratories [25–27] (see panel deliberations below). |
| Lifestyle issues | Epidemiological evidence suggests that a ‘Mediterranean’ diet is associated with a modest reduction in the risk of the occurrence of breast cancer [28]. Several recent meta-analyses have confirmed the association of physical activity with reduced breast cancer incidence and improved prognosis [29]. |
| Hormonal influences | Sex hormones, particularly estrogens, are recognized as important in defining the risk of occurrence of breast cancer, and may be important in particular treatment situations, such as the use of aromatase inhibitors. However, analytical issues still limit the measurement of estrogen at low but clinically relevant levels [30, 31]. |
| Hereditary breast cancer | Factors to be considered regarding recommendation for genetic testing include known mutation in the family, patient or close relative with breast cancer diagnosis <35, patient or close relatives with ovarian or fallopian tube cancers, multiple pancreatic cancers, and some pathological features. However, intrinsic subtype cannot safely be used to exclude the need for genetic testing [32]. |
| Obesity and fat | Obesity is widely recognized as a risk factor for both occurrence and worsened prognosis of breast cancer [33]. Obesity is not clearly predictive of AI (versus Tam) benefit in postmenopausal women [34–36], but may be predictive of reduced AI benefit in premenopausal women [37]. |
| Evidence exists that adipose tissue contains pluripotent stem cells, which might be responsible for tumour angiogenesis [38, 39]. Such cells have been shown to promote breast cancer growth in preclinical models [40], raising the hypothetical concern that use of adipose tissue in breast reconstruction might increase the risk of recurrence. | |
| Metastasis, microenvironment, bone and bisphosphonates | Metastasis is a complex event governed by host interactions. Characteristics of the microenvironment are important in the metastatic process. In preclinical models, tenascin C promotes the aggressiveness of metastasis [41] and autocrine tenascin C is required for early colonization [42]. |
| Bisphosphonates may have beneficial effects in estrogen-deprived women [43–45]. This benefit, which remains uncertain, does not appear to be limited to the inhibition of bone metastases. | |
| Metronomic chemotherapy | Metronomic chemotherapy demonstrates activity in the neoadjuvant setting [46] and in preclinical studies is effective in combination with anti-angiogenic treatments [47]. |
| Risk assessment and prediction | Use of genomic prognostic tests is increasing and has led to altered treatment recommendations in 25%–30% of cases. This has been associated with an overall decreased use of adjuvant chemotherapy [48]. One prospective non-randomized cohort study confirmed the prognostic value of the 70-gene signature in terms of 5-year distant recurrence free interval, and noted an excellent outcome for patients classified as ‘low risk’ and treated without cytotoxic therapy [49]. ER and proliferation define cohorts of patients with early and late recurrence risks. It is noteworthy that first-generation tests are largely calibrated on early recurrence, while the risk of recurrence in luminal disease persists for many years and may be better addressed by newer assays [50–53]. |
| Following neoadjuvant chemotherapy, assessment of residual tumour burden appears prognostically useful, but validation and standardization of this as a prognostic marker is just as important as for IHC or molecular assays [54]. Residual disease after neoadjuvant chemotherapy appears less important in patients with Luminal A or hormone receptor positive, HER2-positive disease, but pCR seems to be prognostically highly important for non-luminal HER2-positive and triple-negative disease [55]. | |
| Following conventional adjuvant therapy, definition of residual risk may guide the need for further treatment or clinical trials. While baseline tumour staging and conventional biological parameters are important, further information may be obtained from evaluations including genomic signatures and tumour infiltrating lymphocytes [56–58]. | |
| Immunity and vaccines | Therapeutic vaccination remains elusive because of tumour heterogeneity and immune escape mechanisms. Agents, such as ipilimumab, which suppress regulatory T cells, may tip the immune balance to cause tumour regression [59]. The presence of tumour-associated lymphocytes in breast cancer is a new independent predictor of response to anthracycline/taxane neoadjuvant chemotherapy [60]. In node-positive, ER-negative, HER2-negative breast cancer, increasing lymphocytic infiltration is associated with an excellent prognosis [56]. |
| Surgery of the primary | Although the risk of local regional relapse is related to the biological aggressiveness of the disease as reflected in its intrinsic subtype, there is no evidence that more extensive surgery will overcome this risk [61]. Effective systemic therapy decreases loco-regional recurrence [62]. Not all women prefer breast conservation. For those who do, the only absolute contraindications are positive margins after multiple resections, and the inability to deliver indicated radiotherapy [63, 64]. |
| Surgery of the axilla | Substantial new data were presented about the role of and necessity for completion axillary dissection after positive sentinel nodes for patients with clinically node-negative disease. The IBCSG 23-01 trial found no benefit of axillary dissection in patients with micrometastatic disease in one or more sentinel lymph nodes [65]. There was increasing acceptance of the omission of axillary dissection also in patients similar to those included in the ACOSOG Z0011 trial that is with one or two involved nodes following breast conservation surgery with whole breast radiation therapy [66]. Ongoing studies are examining the omission of even sentinel node biopsy in patients with ultrasound negative axilla, but this practice remains experimental [67]. |
| Radiation therapy | Clinical trial evidence supports the validity of hypofractionated radiotherapy such as 40 Gy in 15 or 42.5 Gy in 16 fractions in many patients [68–70]. Such short course whole breast radiation therapy has obvious advantages in terms of patient convenience and cost. |
| Trials have demonstrated the safety and efficacy of some forms of partial breast irradiation in selected patients. The main questions are around the definition of a suitable group and variability of levels of evidence between several available intraoperative and postoperative partial breast techniques [71]. ASTRO [72] and ESTRO [73] provide similar guidelines based on factors such as age, BRCA 1/2, tumour size, margins, ER status, focality, histology, nodal factors, and neoadjuvant therapy. A number of large randomised clinical trials of partial breast irradiation await formal reporting and publication of mature outcome data. Partial breast re-irradiation following ‘in breast tumour recurrence’ can be considered as an alternative to salvage mastectomy in selected cases, although the long-term safety and efficacy of this approach have not been established [74]. | |
| Adjuvant chemotherapy | A major unresolved question is the threshold for use of adjuvant cytotoxic chemotherapy for patients with Luminal A or Luminal B disease. In prospective/retrospective studies, the 21- gene recurrence score (RS) identifies groups who do not benefit from the addition of chemotherapy in node-negative [75] or node-positive [76] disease. In both these studies based on randomised trials, chemotherapy benefit was confined to the group with high 21-gene RS. Another series using the 70-gene signature noted excellent 5-year distant recurrence free interval for the ‘good prognosis’ group without chemotherapy [49]. PAM50 classification showed no benefit of anthracycline-based chemotherapy (CEF) compared with CMF chemotherapy in patients with either Luminal A or Luminal B disease [77]. |
| For patients with triple-negative disease, optimal chemotherapy regimens have not been defined, but evidence supports the inclusion of anthracyclines and taxanes, but not bevacizumab, platinums, capecitabine, or gemcitabine [78]. | |
| No standard duration of adjuvant chemotherapy has yet been identified for patients with endocrine non-responsive disease [79]. | |
| Neoadjuvant chemotherapy | Because the goals of treatment are the same in terms of ultimate systemic control, the selection of regimen for neoadjuvant chemotherapy generally follows guidelines similar to those applying to the conventional adjuvant setting [80]. |
| A risk of recurrence (ROR) score based on PAM50 showed that there were no or very few pathological complete responses to neoadjuvant chemotherapy among patients with low ROR [22]. Other neoadjuvant studies have found that a 70-gene good prognosis signature and a low 21-gene RS predict low probability of pCR [81, 82]. | |
| HER2-targeted therapy | Clinical trial results support a standard duration of adjuvant trastuzumab of one year rather than longer [7] or shorter [8] [83]. |
| Endocrine therapy | For premenopausal women with hormone receptor positive breast cancer, the standard endocrine therapy is based on tamoxifen. Unresolved questions include the necessity for combining ovarian function suppression with tamoxifen, and the possible substitution of an aromatase inhibitor in combination with ovarian function suppression. The SOFT and TEXT trials addressing these questions will report results in the near future [46, 84]. |
| Recent evidence from the ATLAS trial suggests that durations of tamoxifen >5 years may be appropriate [9]. In postmenopausal women with endocrine responsive disease, letrozole therapy administered after 5 years of tamoxifen was established via the MA.17 study [85]. Recent analyses of this trial suggest that the benefit of letrozole might be even greater for patients who were premenopausal at the time of initial diagnosis but postmenopausal following completion of five years of tamoxifen [86]. | |
| Adverse effects of aromatase inhibitors limit their use in a substantial proportion of women, and particular concern may exist for those with pre-existing ischaemic cardiovascular disease [87, 88]. | |
| Young women | Women under 40 years of age have relatively higher incidence of triple-negative and HER2-positive disease [89]. One study suggests that very young women, aged ≤35, with triple-negative disease may have particularly high likelihood of achieving pCR with neoadjuvant chemotherapy [90]. |
| Social issues such as fertility, sexual functioning, and the care of young children may be particularly important for younger women [91]. | |
| Follow-up of survivors | A number of studies have failed to show benefit from more, compared with less intensive follow-up investigations. In at least some health care delivery settings, follow-up conducted by oncology nurses is feasible and might be a reasonable alternative to specialist clinical surveillance [92]. |
Recent research in local therapy supports the continued trend towards less extensive procedures. Thus, axillary dissection can safely be omitted for patients with micrometastatic disease in sentinel nodes [65] and for those undergoing breast-conserving surgery and whole breast radiation therapy with up to two macroscopically positive sentinel nodes [66] (Table 1).
Two large studies [68, 69] support the safety and efficacy of shorter courses of whole breast radiation therapy (40 Gy in 15 or 42.5 Gy in 16 fractions), which offer advantages of convenience and cost over the previous standard of 50 Gy in 25 fractions.
New information became available for several aspects of systemic adjuvant therapy. The ATLAS trial reported superiority for 10 years compared with 5 years of adjuvant tamoxifen [9]. Further follow-up of the extended adjuvant study (MA.17) suggested particular benefit of letrozole for patients who were premenopausal at diagnosis but became postmenopausal by the time of letrozole administration [86].
The optimal duration of trastuzumab therapy in HER2-positive disease was clarified by results from two trials. The HERA trial [7] showed no additional benefit of 2 years trastuzumab compared with 1 year, while the PHARE trial [8] failed to show non-inferiority of 6 months trastuzumab compared with 1 year. Thus, the de facto standard of care remains 1 year of trastuzumab in patients with HER2-positive disease.
The Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) meta-analysis of trials of chemotherapy versus no chemotherapy [18] failed to define any group for which chemotherapy did not offer an advantage. This conclusion is at odds with the results of individual trials and prospective/retrospective analyses of trials with assays such as the 21-gene recurrence score (RS). Furthermore, the control groups of trials included in the EBCTCG overview appear to exhibit much higher degrees of risk than that of patients with luminal disease seen in today's practice who receive modern endocrine therapy as the backbone for their treatment. The EBCTCG report noted that ‘information was lacking about tumour gene-expression markers or quantitative immunohistochemistry that might help to predict risk, chemosensitivity, or both’ [18]. Subsequent editorial comments [93, 94] drew differing interpretations of the EBCTCG conclusions.
breast cancer subtypes
The clinico-pathological surrogate definitions of subtypes as adopted by the Panel are summarized in Table 2, and their broad implications for systemic treatment selection are described in Table 3.
Table 2.
Surrogate definitions of intrinsic subtypes of breast cancer
| Intrinsic subtype | Clinico-pathologic surrogate definition | Notes |
|---|---|---|
| Luminal A |
‘Luminal A-like’ all of: ER and PgR positive HER2 negative Ki-67 ‘low’a Recurrence risk ‘low’ based on multi-gene-expression assay (if available)b |
The cut-point between ‘high’ and ‘low’ values for Ki-67 varies between laboratories.a A level of <14% best correlated with the gene-expression definition of Luminal A based on the results in a single reference laboratory [23]. Similarly, the added value of PgR in distinguishing between ‘Luminal A-like’ and ‘Luminal B-like’ subtypes derives from the work of Prat et al. which used a PgR cut-point of ≥20% to best correspond to Luminal A subtype [24]. Quality assurance programmes are essential for laboratories reporting these results. |
| Luminal B |
‘Luminal B-like (HER2 negative)’ ER positive HER2 negative and at least one of: Ki-67 ‘high’ PgR ‘negative or low’ Recurrence risk ‘high’ based on multi-gene-expression assay (if available)b |
‘Luminal B-like’ disease comprises those luminal cases which lack the characteristics noted above for ‘Luminal A-like’ disease. Thus, either a high Ki-67a value or a low PgR value (see above) may be used to distinguish between ‘Luminal A-like’ and ‘Luminal B-like (HER2 negative)’. |
|
‘Luminal B-like (HER2 positive)’ ER positive HER2 over-expressed or amplified Any Ki-67 Any PgR | ||
| Erb-B2 overexpression |
‘HER2 positive (non-luminal)’ HER2 over-expressed or amplified ER and PgR absent |
|
| ‘Basal-like’ |
‘Triple negative (ductal)’ ER and PgR absent HER2 negative |
There is an 80% overlap between ‘triple-negative’ and intrinsic ‘basal-like’ subtype. Some cases with low-positive ER staining may cluster with non-luminal subtypes on gene-expression analysis. ‘Triple negative’ also includes some special histological types such as adenoid cystic carcinoma. |
aA majority of the Panel voted that a threshold of ≥20% was indicative of ‘high’ Ki-67 status. Others, concerned about the high degree of inter-laboratory variation in Ki-67 measurement [26] and the possibility for undertreatment of patients with luminal disease who might benefit from chemotherapy, would use a lower (local laboratory specific) cut-point to define Ki-67 ‘high’ or use multi-gene-expression assay results, if available.
bThis factor was added during Panel deliberations after circulation of the first draft of the manuscript, to reflect a strong minority view. Although neither the 21-gene RS nor the 70-gene signature was designed to define intrinsic subtypes, a concordance study noted that over 90% of cases with a low RS and almost 80% of those with a 70-gene low-risk signature were classified as Luminal A [95].
Table 3.
Systemic treatment recommendations
| ‘Subtype’ | Type of therapy | Notes on therapy |
|---|---|---|
| ‘Luminal A-like’ | Endocrine therapy is the most critical intervention and is often used alone. | Cytotoxics may be added in selected patients. Relative indications for the addition of cytotoxics accepted by a majority of the Panel included:
|
| Studies suggest a wide geographical divergence in the threshold indications for the inclusion of cytotoxics for the treatment of patients with luminal disease [96]. | ||
| ‘Luminal B-like (HER2 negative)’ | Endocrine therapy for all patients, cytotoxic therapy for most. | |
| ‘Luminal B-like (HER2 positive)’ | Cytotoxics + anti-HER2 + endocrine therapy | No data are available to support the omission of cytotoxics in this group. |
| ‘HER2 positive (non-luminal)’ | Cytotoxics + anti-HER2 | Threshold for use of anti-HER2 therapy was defined as pT1b or larger tumour or node-positivity. |
| ‘Triple negative (ductal)’ | Cytotoxics | |
|
‘Special histological types’a A. Endocrine responsive |
Endocrine therapy | |
| B. Endocrine non-responsive | Cytotoxics | Adenoid cystic carcinomas may not require any adjuvant cytotoxics (if node negative). |
aSpecial histological types: endocrine responsive (cribriform, tubular and mucinous); endocrine non-responsive (apocrine, medullary, adenoid cystic and metaplastic).
Further evidence has accrued in the last 2 years to support the use of multi-gene signatures to make distinctions among patients with luminal disease. Many different multi-gene assays provide prognostic information, primarily derived from their sampling of proliferation genes [97], which emphasizes the need for some measure of proliferation in any surrogate classification.
The 21-gene RS is accepted as providing not only prognostic, but also predictive information regarding the utility of cytotoxic therapy in addition to endocrine therapy for patients with luminal disease. This and perhaps other multi-gene assays can help define a group of patients for whom chemotherapy is futile because the biological nature of the tumour is such that it is substantially unresponsive to such agents. Existing studies of the 21-gene RS involve retrospective analysis of previously conducted randomized clinical trials [75, 76], which included both HER2-positive and HER2-negative cohorts. A recent report demonstrated excellent 5-year outcome without chemotherapy for a ‘good prognosis’ 70-gene signature cohort [49].
In those areas of the world where multi-gene assays are readily available, clinical practice has developed to rely on the results to guide decisions about inclusion of chemotherapy in the treatment of patients with ER-positive, HER2-negative disease. The 70-gene assay returns a dichotomous result, while 21-gene RS is continuous. An unresolved question is the level of RS which should justify cytotoxic therapy: only high RS values (>31) were significantly associated with chemotherapy benefit in the prospective/retrospective studies [75, 76], while substantially lower values are being investigated in ongoing prospective trials and are being used in clinical practice. For many societies, the cost of these multi-gene assays remains prohibitive.
The possibility that multi-gene expression assays may become more widely available was discussed by some Panellists after the meeting during the preparation of this manuscript. Cost-effectiveness studies have been carried out in the United States [98, 99], Canada [100–104], Israel [105], the UK [106] and Germany [107, 108]. These studies have yielded varying estimates ranging from cost-saving to an incremental cost-effectiveness ratio (ICER) of ∼US $60 000 per quality-adjusted life year (QALY). One Japanese study of the 70-gene assay [109] found an ICER of US $40 000 per QALY. Such assessments will be sensitive not only to the cost of the test, but to the net proportion of patients in whom testing leads to the omission of cytotoxic therapy, and to the cost of the cytotoxic regimen which would otherwise have been given. These reports have largely worked from the perspective of the health care system or third-party payer, and thus offer hope that such bodies may increasingly support multi-gene testing. It has recently been reported that the UK National Institute for Clinical Excellence, having reached a confidential pricing arrangement with the supplier, has issued a draft recommendation that the 21-gene RS be used for women with node-negative disease for whom the indication for chemotherapy is otherwise uncertain1. Meanwhile, in many settings patients can only access multi-gene testing by large personal out-of pocket payments, and therefore, from a global perspective for the immediate future multi-gene testing remains inaccessible for the majority of women with early breast cancer. It is for these women that the Panel believed that the approach adopted by successive St Gallen Panels based on the available clinico-pathological testing, and now expressed in the surrogate IHC-based classification shown in Table 2 will be more widely applicable at lesser cost, notwithstanding its limited validation.
The main reason for attempting distinction between ‘Luminal A-like’ (more endocrine sensitive, indolent, better prognosis) and ‘Luminal B-like’ (less endocrine sensitive, more aggressive, worse prognosis) tumours was recognized to be the differing implications for the utility or futility of adjuvant cytotoxic therapy between these groups. Evidence was presented that the clarity of distinction between ‘Luminal A-like’ and ‘LuminalB-like’ tumours could be improved by the requirement for substantial PgR positivity in the definition of ‘Luminal A-like’ disease [24]. Adding this restriction will have the effect of reducing the number of patients classified as ‘Luminal A-like’ and thus increasing the number for whom cytotoxic therapy is generally recommended. Recognizing that high-quality pathology and quality assurance programmes are important for the interpretation of these tests, it was noted that the absolute values of each IHC parameter/cut-point may vary between laboratories, and that pending improved standardization local experience might best define the locally useful cut-points between ‘high’ and ‘low’ Ki-67 and PgR.
panel deliberations
The Panel reviewed a series of questions developed by iterative consultation over the months preceding the conference. Voting on most questions was in the format yes, no or abstain, where abstaining was recommended if the Panel member felt a conflict of interest in the question, that there was insufficient evidence to support an opinion either way or that he or she lacked the relevant expertise. Detailed voting records for each of the questions put to the Panel are provided in the supplementary Appendix S1, available at Annals of Oncology online.
surgery of the primary
The Panel found very few absolute contraindications to breast-conserving therapy. Margins involved with invasive carcinoma or DCIS after repeated resection were one such absolute contraindication. The minimal acceptable surgical margin was felt to be ‘no ink on invasive tumour’ (i.e. margins free of tumour) by nearly three quarters of the Panellists and most of the others would accept a minimum clearance of 1 mm. The Panel was almost unanimous that breast-conserving surgery should not be carried out unless postoperative radiation (if indicated, as described below in the radiation therapy section) could be delivered.
A majority of the Panel considered that relative but not absolute contraindications to breast-conserving therapy included very young age (<35 years); extensive or diffuse microcalcifications where the presence of malignancy cannot be reliably excluded without complete excision; multicentric disease; tumour location near the nipple and mutations of the BRCA1 or BRCA2 genes. Substantial minority support added multifocal disease, extensive vascular invasion and an extensive intraductal component to this list of relative contraindications. Positive family history and unfavourable biology based on genomic profiling were not considered to be contraindications to breast-conserving therapy.
Nipple-sparing surgery was considered acceptable, provided the margin close to the nipple was not involved. The vast majority of Panel members thought magnetic resonance imaging should not be routinely used in the assessment of newly diagnosed breast cancer.
surgery of the axilla
The Panel believed that axillary dissection could be safely omitted in patients with one or two positive sentinel nodes following breast-conserving surgery when whole breast radiation therapy is planned. The Panel was nearly equally divided whether this recommendation also applied to mastectomy followed by radiotherapy, but was almost unanimous in the need for axillary dissection if no radiotherapy was planned.
The Panel also considered that axillary dissection was required with three or more involved sentinel nodes or if nodes were clinically involved before surgery and confirmed by biopsy.
radiation therapy
The Panel strongly agreed that ‘short course’ radiotherapy, such as 40 Gy in 15 or 42.5 Gy in 16 fractions, could be offered as a standard for at least some patients, with a slim majority thinking that this would be suitable for almost all patients. The Panel agreed that short course radiotherapy was an option whether or not a boost to the tumour bed was planned. A large majority of Panel members thought that there were definable groups of patients not requiring radiotherapy following breast-conserving surgery, and that these might include the elderly and those with substantial comorbidity. The Panel could not reach a majority view regarding the current acceptability of the various techniques for partial breast radiation as definitive treatment.
Post-mastectomy radiotherapy was considered indicated by almost all Panel members for patients with four or more positive nodes, while the majority would not advise post-mastectomy irradiation for those with one to three positive nodes, except in the presence of adverse tumour pathology. The Panel was content to omit post-mastectomy radiotherapy with pathologic uninvolved nodes even when fewer than eight nodes had been examined and if the tumour was ≤5 cm. Two-thirds felt that radiation therapy should be given after mastectomy if positive sentinel nodes were not followed by axillary dissection.
Other indications recommended by the Panel for post-mastectomy radiotherapy included positive deep margins and, for two-thirds of the Panel, tumours greater than 5 cm regardless of the nodal status. However, the Panel strongly rejected needing radiotherapy solely based on Grade 3, lymphovascular invasion, HER2-positive status or triple-negative disease.
Areas to be irradiated following mastectomy and axillary dissection should not be influenced by any neoadjuvant systemic therapy or by the intrinsic subtype of the tumour. There was no clear agreement about the necessity to include the supraclavicular fossa, though trials have routinely included this area. Most Panel members would not include the internal mammary nodes and a strong majority felt that the axilla should not be radiated after dissection.
pathology
The Panel recognized substantial progress in the pathological characterization of tumour subtypes. There was little change in the classification of HER2-positive or triple-negative disease. The majority of the Panel accepted that a useful surrogate definition of Luminal A-like as distinct from Luminal B-like disease could be made using a combination of ER, PgR and Ki-67, without requiring molecular diagnostics. Ki-67 has been used for more than two decades as a prognostic marker in early breast cancer [110–118]. The Panel did not accept that distinction between Luminal A-like and Luminal B-like tumours could be made with ER and PgR alone, and a clear majority voted that grade 3 could not be used as a substitute for high Ki-67 for this purpose. The Panel noted that standardized cut-offs for Ki-67 have not been established and laboratory specific values should be used, but the majority of the Panel voted that a threshold of ≥20% was clearly indicative of ‘high’ Ki-67 status. A minority questioned the role of Ki-67 in breast cancer treatment decisions. The Panel stressed the need for standardization, and that laboratories should participate in quality assurance programmes.
The Panel was strongly of the opinion that intrinsic subtypes, including those defined by the clinico-pathological surrogates, should influence whether or not chemotherapy was used, but not the choice of the cytotoxic regimen. After clinico-pathological assessment, a slim majority of the Panel was in favour of requesting a multi-gene assay in node-negative, ER-positive and HER2-negative cases. The Panel considered that only the 21-gene RS was predictive of chemotherapy responsiveness, though a substantial minority would also endorse PAM50 or the 70-gene signature for this purpose. This led to a recommendation that selection of patients who might forego chemotherapy could be based on the 21-gene RS, but the Panel did not offer majority endorsement for PAM50, the 70-gene signature or EPClin as yet established for this purpose.
For patients with ER-positive, HER2-negative disease, the use of molecular diagnostics was felt to be unnecessary in low-risk patients such as those with a tumour size of ≤1 cm in the setting of negative lymph nodes, since chemotherapy would be unlikely to be given anyway. Similarly, patients with a higher risk such as those with a tumour size >5 cm, inflammatory breast cancer, those with four or more involved nodes, or a very low ER positivity (e.g. 5%) might not benefit from molecular diagnostics because chemotherapy would be likely to be offered in any case. Patients in whom chemotherapy was thought to be of uncertain indication and who might, therefore, benefit from molecular diagnostics were felt to include selected patients with node-negative disease, those with one to three positive nodes, and patients aged <35.
In the determination of HER2 status for treatment purposes, the Panel did not believe that polysomy of chromosome 17, or heterogeneity of expression of HER2 need to be considered.
adjuvant endocrine therapy in premenopausal women
The large majority of the Panel said that tamoxifen alone was the default adjuvant endocrine therapy for premenopausal patients. In light of recent trial evidence, it was felt that at least some patients should have a treatment duration of 10 years, although this may not be needed by all patients. Most Panellists thought ovarian suppression need not be added to tamoxifen, but Panellists were evenly divided for patients <40 years of age. Most of the Panel regarded both ovarian suppression alone without tamoxifen and its combination with aromatase inhibitors as inappropriate unless tamoxifen was contraindicated.
adjuvant endocrine therapy in postmenopausal women
The Panel strongly believed that some postmenopausal women could be treated with tamoxifen alone. If an aromatase inhibitor were included in the regimen, Panellists were equally divided whether treatment should start with the aromatase inhibitor, although this strategy was strongly preferred for patients at high risk. Most Panellists believed that initial aromatase inhibitor therapy could be replaced by tamoxifen after 2 years, if there were a reason to do so. Extension of aromatase inhibitor therapy beyond the first five years for patients with node-positive, but not node-negative disease was strongly supported, for patients whose initial treatment was tamoxifen or whose initial therapy was <5 years of an aromatase inhibitor. The Panel was equally divided concerning an extended duration of aromatase inhibitor therapy beyond 5 years of treatment with these agents. Extended adjuvant endocrine therapy using tamoxifen is a consideration after a 5-year course of an aromatase inhibitor, though this approach has not been directly studied.
adjuvant cytotoxic chemotherapy
The Panel was clearly of the opinion that factors arguing for the inclusion of chemotherapy were histological grade 3 tumours, high Ki-67, low hormone receptor status, HER2 positivity or triple-negative status, high 21-gene RS, high-risk 70-gene signature and the involvement of more than three lymph nodes. Most felt that nodal positivity per se was not an indication for chemotherapy but very few would forego chemotherapy for patients with four or more positive nodes. Lymphovascular invasion was not recognized as an indication, while the Panel was equally divided whether young age (<35 years) was an indication.
The Panel was of the strong opinion that patients with Luminal A-like disease were ‘less responsive to chemotherapy’, but this treatment could be added to endocrine therapy based on the large tumour volume, assessment of risk or patient preference. The Panel did not select a specific chemotherapy regimen for these patients and expressed the view that any of the standard regimens, including the first- and second-generation regimens (CMF, AC, TC), could be considered.
For patients with Luminal B (HER2-negative) disease, the majority of the Panel considered chemotherapy to be indicated. Chemotherapy regimens for Luminal B (HER2-negative) disease should generally contain anthracyclines and (by a slim majority) taxanes. Half the Panel agreed that such chemotherapy should be delivered for at least six cycles, but the Panel did not endorse the exclusive use of a dose dense regimen.
For patients with HER2-positive disease, the Panel strongly believed, while there was no specifically preferred regimen, chemotherapy should include a taxane and, for most Panel members, also an anthracycline.
For patients with ‘basal-like’ (triple-negative ductal) disease, the Panel strongly endorsed both anthracyclines and taxanes, and did not believe that platinum, or regimens emphasizing alkylating agents were specifically required. There was no clear consensus on the role of dose dense regimens, though a substantial minority expressed support for such treatment.
General considerations influencing the choice of chemotherapy regimen were thought to include a desire to preserve fertility, the avoidance of alopecia and the presence of co-morbidities, but not intrinsic subtype or the presence of BRCA1 or BRCA2 mutation. Older chronological age should not necessarily influence the choice of regimen [119], but assessment of co-morbidities and general health was considered, especially important in older patients.
anti-HER2 therapies
For patients whose tumours show amplification or overexpression of HER2, the Panel considered that trastuzumab therapy was indicated for patients with tumours >5 mm, while some Panellists would treat patients with such tumours of any size. Most felt that trastuzumab should be given concurrently with a taxane, but not with an anthracycline. The Panel was prepared to endorse trastuzumab (with endocrine therapy, if indicated) without chemotherapy only if chemotherapy were contraindicated. The Panel was unanimous that the duration of trastuzumab should be 1 year.
neoadjuvant cytotoxic chemotherapy
The Panel was split about whether neoadjuvant chemotherapy had benefits beyond local downstaging. The Panel did not support additional postoperative adjuvant chemotherapy following a full course of neoadjuvant chemotherapy, whether or not pCR were achieved. Most believe when neoadjuvant therapy is given outside of a clinical trial, the full course of chemotherapy should be completed before surgery. In the unusual situation in which a surgery is carried out after less than a full course of neoadjuvant chemotherapy most Panel members would complete the course postoperatively.
neoadjuvant anti-HER2 therapy
For patients with HER2-positive disease, the Panel was strongly of the opinion that neoadjuvant treatment should include anti-HER2 drugs, and the majority recommended the use of chemotherapy plus trastuzumab alone (without additional anti-HER agents).
neoadjuvant endocrine therapy
The Panel strongly endorsed endocrine therapy alone as neoadjuvant treatment for postmenopausal patients with strongly positive hormone receptors and low proliferating disease, and most thought that such treatment should be continued until maximal response.
bisphosphonates
The Panel considered several situations in which bisphosphonates might be used with the aim of improving disease-free survival, but did not endorse such treatment for this purpose in any group, though a substantial minority felt that premenopausal patients receiving an LHRH agonist plus tamoxifen or clearly postmenopausal patients might derive benefit from such treatment. Denosumab was not endorsed for adjuvant use.
follow-up
The majority of the Panel believed that regular follow-up after the completion of immediate treatment (excluding long-term endocrine therapy) was appropriate, but that this could be supervised by a nurse specialist, rather than a surgeon or oncologist. The majority of the Panel also believed that follow-up should be done in person and not by telephone.
summary of treatment recommendations
The conference endorsed recent trial evidence supporting less extensive local therapies. It refined and re-iterated the value of clinico-pathological surrogate definitions resembling intrinsic subtypes to guide selection of systemic adjuvant therapies. The Panel recognized the superior accuracy and reproducibility of multi-gene molecular assays, but recognized that these assays are not available in all parts of the world. The Panel also noted the variability in the current levels of evidence to support the use of the individual multi-gene assays. Ongoing trials will prospectively define the value of chemotherapy in addition to endocrine therapy in patients with luminal disease in the node-negative (TAILORx, MINDACT) and node-positive (MINDACT, RxPONDER) cohorts. It is therefore to be hoped that a future St Gallen Consensus conference will be able to provide more robustly supported recommendations for treatment of such patients.
funding
Support for the conference was provided by SONK from registration fees paid by the conference attendees and by Grant No. CA75362 from the United States National Cancer Institute (IBCSG Statistical Center, R. Gelber, PI).
disclosure
The full COI statements of all authors are included in appendix 2.
Supplementary Material
acknowledgements
We gratefully acknowledge the participants in the 13th St Gallen conference for their many useful suggestions. In addition to Panel members, we thank Drs. John Yarnold and Timothy J. Whelan for guidance in the development of the questions considered by the Panel. We thank Mrs. Sabina Briner, Dr. Carmen Criscitiello, and Mrs. Shari Gelber for their substantial assistance in the preparation of this report.
appendix 1
Members of the Panel are listed below. All had a significant input to the discussion and manuscript.
Kathy S. Albain, Loyola University Medical Center, Cardinal Bernardin Cancer Center, Maywood, USA
Fabrice André, Research Director, Department of Medical Oncology, Institut Gustave Roussy, Villejuif, France
Jonas Bergh, Radiumhemmet & Karolinska Oncology, Karolinska Institutet and University Hospital, Stockholm, Sweden
Hervé Bonnefoi, Institut Bergonié Cancer Center, Université de Bordeaux, Bordeaux, France
Denisse Bretel-Morales, GECOPERU, Lima, Peru
Harold Burstein, Department of Medical Oncology/Solid Tumour Oncology, Dana-Farber Cancer Institute, Boston, USA
Fatima Cardoso, Breast Unit, Champalimaud Cancer Center, Lisbon, Portugal
Monica Castiglione-Gertsch, Oncogynaecology Unit, University Hospital, Geneva, Switzerland
Alan S. Coates, International Breast Cancer Study Group and University of Sydney, Sydney, Australia
Marco Colleoni, Research Unit Medical Senology, European Institute of Oncology, Milan, Italy
Alberto Costa, ESO—European School of Oncology, Milan, Italy and Breast Unit of Southern Switzerland, Lugano, Switzerland
Giuseppe Curigliano, Division of Medical Oncology, European Insitute of Oncology, Milan, Italy
Nancy E. Davidson, Division of Hematology/Oncology, University of Pittsburgh Cancer Institute and UPMC Cancer Center, Pittsburgh, USA
Angelo Di Leo, ‘Sandro Pitigliani’ Medical Oncology Unit, Department of Oncology, Hospital of Prato, Prato, Italy
Bent Ejlertsen, Department of Oncology, Bldg 4262 Rigshospitalet, Copenhagen, Denmark
John F. Forbes, Department of Surgical Oncology, University of Newcastle, Calvary Mater Hospital, ANZ BCTG, Newcastle NSW, Australia
Richard D. Gelber, Department of Biostatistics and Computational Biology, Dana-Farber Cancer Institute, Boston, USA
Michael Gnant, Department of Surgery, Comprehensive Cancer Center Vienna, Medical University of Vienna, Wien, Austria
Aron Goldhirsch, Division of Medical Oncology, European Institute of Oncology, International Breast Cancer Study Group, Milan, Italy, and Ospedale Italiano, Viganello-Lugano, Switzerland (Chairman)
Pamela Goodwin, Department of Medicine, Division of Clinical Epidemiology, Samuel Lunenfeld Research Institute, Mount Sinai Hospital and Princess Margaret Hospital, University of TorontoToronto, Canada
Paul E. Goss, Department of Medicine, MGH Cancer Center, Boston, USA
Jay R. Harris, Department of Radiation Oncology, Dana-Farber Cancer Institute, Brigham and Women's Hospital, Boston, USA
Daniel F. Hayes, Department of Internal Medicine, Breast Care Center, University of Michigan, Comprehensive Cancer Center, Ann Arbor, USA
Clifford A. Hudis, Breast Cancer Medicine Service, Memorial Sloan-Kettering Cancer Center, Memorial Hospital, and Weill Cornell Medical College, New York
James N. Ingle, Mayo Clinic Cancer Center, Women's Cancer Programme, Rochester, USA
Jacek Jassem, Deptartment of Oncology & Radiotherapy, Medical University of Gdansk, Gdansk, Poland
Zefei Jiang, 307 Hospital, Academy of Military Medical Sciences, Beijing, China
Per Karlsson, Department of Oncology, Institute of Selected Clinical Sciences, Sahlgrenska Academy, Sahlgrenska University Hospital, Göteborg, Sweden
Sibylle Loibl, Unit Head of Medicine & Research, German Breast Group, GBG Forschungs GmbH, Neu-Isenburg, Germany
Monica Morrow, Memorial Sloan-Kettering Cancer Center, Evelyn Lauder Breast Center, New York, USA
Moise Namer, Medical Oncology, Center Antoine Lacassagne, Nice Cedex 2, France
C. Kent Osborne, Dan L. Duncan Cancer Center, Baylor College of Medicine, Houston, USA
Ann H. Partridge, Department of Medicine, Harvard Medical School, Dana-Farber Cancer Institute, Boston, USA
Frédérique Penault-Llorca, Service d'Anatomie Pathologie Moléculaire, Dépt. RIO, Center Jean Perrin, Clermont-Ferrand Cedex 1, France
Charles M. Perou, Departments of Genetics and Pathology, Lineberger Comprehensive Cancer Center, The University of North Carolina at Chapel HillChapel Hill, USA
Martine J. Piccart-Gebhart, Internal Medicine, Oncology, Institut Jules Bordet, Brussels, Belgium
Kathleen I. Pritchard, University of Toronto, Sunnybrook Odette Cancer Center, Ontario Clinical Oncology Group (OCOG), Toronto, Canada
Emiel J.T. Rutgers, Department of Surgery, The Netherlands Cancer Institute, Amsterdam, The Netherlands
Felix Sedlmayer, Department of Radiotherapy and Radiation Oncology, LKH Salzburg, Paracelsus Medical University Hospital, Salzburg, Austria
Vladimir Semiglazov, N.N. Petrov Research Institute of Oncology, St Petersburg, Russia
Zhi-Ming Shao, Fudan University, Cancer Hospital, Shanghai, China
Ian Smith, Breast Unit, Royal Marsden Hospital and Institute of Cancer Research, London, UK
Beat Thürlimann, Breast Center, Kantonsspital St Gallen, St Gallen, Switzerland
Masakazu Toi, Department of Breast Surgery, Kyoto University Hospital, Kyoto Japan
Andrew Tutt, Breast Oncology Unit, King's Health Partners AHSC, Guy's Hospital, London UK
Michael Untch, Department of Gynaecology and Obstetrics, Multidisciplinary Breast Cancer Center, Helios Klinikum Berlin-Buch, Academic Hospital of the University of Göttingen, Berlin, Germany
Giuseppe Viale, Department of Pathology, European Institute of Oncology and University of Milan, Milan, Italy
Toru Watanabe, Department of Medicine, Hamamatsu Oncology Center, Hamamatsu Japan
Nicholas Wilcken, Department of Medical Oncology, University of Sydney, Westmead Hospital, Wentworthville NSW, Australia
Eric P. Winer, Breast Oncology Center, Dana-Farber Cancer Institute, Boston, USA (Chairman)
William C. Wood, Department of Surgery, Winship Cancer Institute, Atlanta, USA
appendix 2
Footnotes
http://guidance.nice.org.uk/DT/4 accessed 3 May 2013
references
- 1.Goldhirsch A, Wood WC, Coates AS, et al. Strategies for subtypes—dealing with the diversity of breast cancer: highlights of the St Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol. 2011;22:1736–1747. doi: 10.1093/annonc/mdr304. doi:10.1093/annonc/mdr304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The Cancer Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature. 2012;490:61–70. doi: 10.1038/nature11412. doi:10.1038/nature11412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dunbier AK, Anderson H, Ghazoui Z, et al. Association between breast cancer subtypes and response to neoadjuvant anastrozole. Steroids. 2011;76:736–740. doi: 10.1016/j.steroids.2011.02.025. doi:10.1016/j.steroids.2011.02.025. [DOI] [PubMed] [Google Scholar]
- 4.Ellis MJ, Ding L, Shen D, et al. Whole-genome analysis informs breast cancer response to aromatase inhibition. Nature. 2012;486:353–360. doi: 10.1038/nature11143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Galimberti V, Botteri E, Chifu C, et al. Can we avoid axillary dissection in the micrometastatic sentinel node in breast cancer? Breast Cancer Res Treat. 2012;131:819–825. doi: 10.1007/s10549-011-1486-2. doi:10.1007/s10549-011-1486-2. [DOI] [PubMed] [Google Scholar]
- 6.Martelli G, Boracchi P, Ardoino I, et al. Axillary dissection versus no axillary dissection in older patients with T1N0 breast cancer: 15-year results of a randomized controlled trial. Ann Surg. 2012;256:920–924. doi: 10.1097/SLA.0b013e31827660a8. [DOI] [PubMed] [Google Scholar]
- 7.Goldhirsch A, Gelber RD, Piccart-Gebhart MJ, et al. 2 years versus 1 year of adjuvant trastuzumab for HER2-positive breast cancer (HERA): an open-label, randomised controlled trial. doi: 10.1016/S0140-6736(13)61094-6. The Lancet 2013 July 18 [epub ahead of print] doi: 10.1016/S0140-6736(13)61094-6. [DOI] [PubMed] [Google Scholar]
- 8.Pivot X, Romieu G, Debled M, et al. 6 months versus 12 months of adjuvant trastuzumab for patients with HER2-positive early breast cancer (PHARE): a randomised phase 3 trial. Lancet Oncol. 2013;14:741–748. doi: 10.1016/S1470-2045(13)70225-0. [DOI] [PubMed] [Google Scholar]
- 9.Davies C, Pan H, Godwin J, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 2013;381:805–816. doi: 10.1016/S0140-6736(12)61963-1. doi:10.1016/S0140-6736(12)61963-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baselga J, Campone M, Piccart M, et al. Everolimus in postmenopausalhormone-receptor-positive advanced breast cancer. N Engl J Med. 2012;366:520–529. doi: 10.1056/NEJMoa1109653. doi:10.1056/NEJMoa1109653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Osborne CK, Schiff R. Overcoming resistance to endocrine therapy due to PI3K/AKT pathway activation by combinations of mTOR, AKT or MEK inhibitors. The Breast. 2013;22(Supp 1):S2. Abstr. SP1.04) [Google Scholar]
- 12.Ibrahim YH, Garcia-Garcia C, Serra V, et al. PI3K Inhibition impairs BRCA1/2 expression and sensitizes BRCA proficient triple negative breast cancer to PARP inhibition. Cancer Discov. 2012;2:1036–1047. doi: 10.1158/2159-8290.CD-11-0348. doi:10.1158/2159-8290.CD-11-0348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Juvekar A, Burga LN, Hu H, et al. Combining a PI3K inhibitor with a PARP inhibitor provides an effective therapy for BRCA1-related breast cancer. Cancer Discov. 2012;2:1048–1063. doi: 10.1158/2159-8290.CD-11-0336. doi:10.1158/2159-8290.CD-11-0336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Varna M, Bousquet G, Plassa LF, et al. TP53 status and response to treatment in breast cancers. J Biomed Biotechnol. 2011 doi: 10.1155/2011/284584. May 9 [epub ahead of print] doi: 10.1155/2011/284584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jackson JG, Pant V, Li Q, et al. p53-mediated senescence impairs the apoptotic response to chemotherapy and clinical outcome in breast cancer. Cancer Cell. 2012;21:793–806. doi: 10.1016/j.ccr.2012.04.027. doi:10.1016/j.ccr.2012.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bailey ST, Shin H, Westerling T, et al. Estrogen receptor prevents p53-dependent apoptosis in breast cancer. Proc Natl Acad Sci USA. 2012;109:18060–5. doi: 10.1073/pnas.1018858109. doi:10.1073/pnas.1018858109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bonnefoi H, Piccart M, Bogaerts J, et al. TP53 Status for prediction of sensitivity to taxane versus non-taxane neoadjuvant chemotherapy in breast cancer (EORTC 10994/BIG 1–00): a randomised phase 3 trial. Lancet Oncol. 2011;12:527–539. doi: 10.1016/S1470-2045(11)70094-8. doi:10.1016/S1470-2045(11)70094-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Early Breast Cancer Trialists’ Collaborative Group. Comparisons between different polychemotherapy regimens for early breast cancer: meta-analyses of long-term outcome among 100 000 women in 123 randomised trials. Lancet. 2012;379:432–444. doi: 10.1016/S0140-6736(11)61625-5. doi:10.1016/S0140-6736(11)61625-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Di Leo A. The continued evidence from overviews: what is the clinical utility? The Breast. 2013;22(Supp 1):S2. doi: 10.1016/j.breast.2013.07.002. Abstr. SP1.02) [DOI] [PubMed] [Google Scholar]
- 20.Ellis MJ, Perou CM. The genomic landscape of breast cancer as a therapeutic roadmap. Cancer Discov. 2013;3:27–34. doi: 10.1158/2159-8290.CD-12-0462. doi:10.1158/2159-8290.CD-12-0462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hayes DF. From the genome to bedside: are we lost in translation? The Breast. 2013;22(Supp 1):S3. doi: 10.1016/j.breast.2013.07.004. Abstr. SP2.02) [DOI] [PubMed] [Google Scholar]
- 22.Parker JS, Mullins M, Cheang MC, et al. Supervised risk predictor of breast cancer based on intrinsic subtypes. J Clin Oncol. 2009;27:1160–1167. doi: 10.1200/JCO.2008.18.1370. doi:10.1200/JCO.2008.18.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cheang MCU, Chia SK, Voduc D, et al. Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst. 2009;101:736–750. doi: 10.1093/jnci/djp082. doi:10.1093/jnci/djp082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Prat A, Cheang MC, Martin M, et al. Prognostic significance of progesterone receptor-positive tumor cells within immunohistochemically defined luminal A breast cancer. J Clin Oncol. 2013;31:203–209. doi: 10.1200/JCO.2012.43.4134. doi:10.1200/JCO.2012.43.4134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dowsett M, Nielsen TO, A'Hern R, et al. Assessment of Ki67 in breast cancer: recommendations from the international Ki67 in breast cancer working group. J Natl Cancer Inst. 2011;103:1656–1664. doi: 10.1093/jnci/djr393. doi:10.1093/jnci/djr393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nielsen TO, Polley M-YC, Leung SCY, et al. An international Ki-67 reproducibility study. Presented at the 35th San Antonio Breast Cancer Symposium; December 4–8, 2012. Abstr S4–6. [Google Scholar]
- 27.Luporsi E, Andre F, Spyratos F, et al. Ki-67: level of evidence and methodological considerations for its role in the clinical management of breast cancer: analytical and critical review. Breast Cancer Res Treat. 2012;132:895–915. doi: 10.1007/s10549-011-1837-z. doi:10.1007/s10549-011-1837-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Buckland G, Travier N, Cottet V, et al. Adherence to the Mediterranean diet and risk of breast cancer in the European prospective investigation into cancer and nutrition cohort study. Int J Cancer. 2013;132:2918–2927. doi: 10.1002/ijc.27958. [DOI] [PubMed] [Google Scholar]
- 29.Chlebowski RT. Nutrition and physical activity influence on breast cancer incidence and recurrence. The Breast. 2013;22(Supp 1):S5. doi: 10.1016/j.breast.2013.07.006. Abstr. SP3.01) [DOI] [PubMed] [Google Scholar]
- 30.Folkerd EJ, Dixon JM, Renshaw L, et al. Suppression of plasma estrogen levels by letrozole and anastrozole is related to body mass index in patients with breast cancer. J Clin Oncol. 2012;30:2977–2980. doi: 10.1200/JCO.2012.42.0273. doi:10.1200/JCO.2012.42.0273. [DOI] [PubMed] [Google Scholar]
- 31.Dowsett M, Folkerd E. Sex hormones and breast cancer risk and prognosis. The Breast. 2013;22(Supp 1):S5. doi: 10.1016/j.breast.2013.07.007. Abstr. SP3.02) [DOI] [PubMed] [Google Scholar]
- 32.Mavaddat N, Barrowdale D, Andrulis IL, et al. Pathology of breast and ovarian cancers among BRCA1 and BRCA2 mutation carriers: results from the consortium of investigators of modifiers of BRCA1/2 (CIMBA) Cancer Epidemiol Biomarkers Prev. 2012;21:134–147. doi: 10.1158/1055-9965.EPI-11-0775. doi:10.1158/1055-9965.EPI-11-0775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Niraula S, Ocana A, Ennis M, et al. Body size and breast cancer prognosis in relation to hormone receptor and menopausal status: a meta-analysis. Breast Cancer Res Treat. 2012;134:769–781. doi: 10.1007/s10549-012-2073-x. doi:10.1007/s10549-012-2073-x. [DOI] [PubMed] [Google Scholar]
- 34.Sestak I, Distler W, Forbes JF, et al. Effect of body mass index on recurrences in tamoxifen and anastrozole treated women: an exploratory analysis from the ATAC trial. J Clin Oncol. 2010;28:3411–3415. doi: 10.1200/JCO.2009.27.2021. doi:10.1200/JCO.2009.27.2021. [DOI] [PubMed] [Google Scholar]
- 35.Ewertz M, Gray KP, Regan MM, et al. Obesity and risk of recurrence or death after adjuvant endocrine therapy with letrozole or tamoxifen in the Breast International Group 1–98 trial. J Clin Oncol. 2012;30:3967–3975. doi: 10.1200/JCO.2011.40.8666. doi:10.1200/JCO.2011.40.8666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goodwin PJ, Pritchard KI. Obesity and hormone therapy in breast cancer: an unfinished puzzle. J Clin Oncol. 2010;28:3405–3407. doi: 10.1200/JCO.2010.29.5113. doi:10.1200/JCO.2010.29.5113. [DOI] [PubMed] [Google Scholar]
- 37.Pfeiler G, Koenigsberg R, Fesl C, et al. Impact of body mass index on the efficacy of endocrine therapy in premenopausal patients with breast cancer: an analysis of the prospective ABCSG-12 trial. J Clin Oncol. 2011;29:2653–2659. doi: 10.1200/JCO.2010.33.2585. doi:10.1200/JCO.2010.33.2585. [DOI] [PubMed] [Google Scholar]
- 38.Bertolini F. Adipose tissue and breast cancer progression: a link between metabolism and cancer. The Breast. 2013;22(Supp 1):S6. doi: 10.1016/j.breast.2013.07.009. Abstr. SP4.01) [DOI] [PubMed] [Google Scholar]
- 39.Bertolini F, Lohsiriwat V, Petit JY, et al. Adipose tissue cells, lipotransfer and cancer: a challenge for scientists, oncologists and surgeons. Biochim Biophys Acta. 2012;1826:209–214. doi: 10.1016/j.bbcan.2012.04.004. [DOI] [PubMed] [Google Scholar]
- 40.Petit JY, Botteri E, Lohsiriwat V, et al. Locoregional recurrence risk after lipofilling in breast cancer patients. Ann Oncol. 2012;23:582–588. doi: 10.1093/annonc/mdr158. doi:10.1093/annonc/mdr158. [DOI] [PubMed] [Google Scholar]
- 41.Oskarsson T, Acharyya S, Zhang XH, et al. Breast cancer cells produce tenascin C as a metastatic niche component to colonize the lungs. Nat Med. 2011;17:867–874. doi: 10.1038/nm.2379. doi:10.1038/nm.2379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Oskarsson T. Extracellular matrix players in breast cancer progression and metastasis. The Breast. 2013;22(Supp 1):S7. doi: 10.1016/j.breast.2013.07.012. Abstr. SP4.04) [DOI] [PubMed] [Google Scholar]
- 43.Coleman RE, Marshall H, Cameron D, et al. Breast-cancer adjuvant therapy with zoledronic acid. N Engl J Med. 2011;365:1396–1405. doi: 10.1056/NEJMoa1105195. doi:10.1056/NEJMoa1105195. [DOI] [PubMed] [Google Scholar]
- 44.Coleman R, de Boer R, Eidtmann H, et al. Zoledronic acid (zoledronate) for postmenopausal women with early breast cancer receiving adjuvant letrozole (ZO-FAST study): final 60-month results. Ann Oncol. 2013;24:398–405. doi: 10.1093/annonc/mds277. doi:10.1093/annonc/mds277. [DOI] [PubMed] [Google Scholar]
- 45.Gnant M, Mlineritsch B, Stoeger H, et al. Adjuvant endocrine therapy plus zoledronic acid in premenopausal women with early-stage breast cancer: 62-month follow-up from the ABCSG-12 randomised trial. Lancet Oncology. 2011;12:631–641. doi: 10.1016/S1470-2045(11)70122-X. doi:10.1016/S1470-2045(11)70122-X. [DOI] [PubMed] [Google Scholar]
- 46.Goldhirsch A. Personalized adjuvant therapies: lessons from the past. The Breast. 2013;22(Supp 1):S1. doi: 10.1016/j.breast.2013.07.001. Abstr. SP0.01) [DOI] [PubMed] [Google Scholar]
- 47.Kerbel RS. Preclinical recapitulation of antiangiogenic drug clinical efficacies using models of early or late stage breast cancer metastasis. The Breast. 2013;22(Supp 1):S7. doi: 10.1016/j.breast.2013.07.011. Abstr. SP4.03)(manuscript in preparation. [DOI] [PubMed] [Google Scholar]
- 48.Hassett MJ, Silver SM, Hughes ME, et al. Adoption of gene expression profile testing and association with use of chemotherapy among women with breast cancer. J Clin Oncol. 2012;30:2218–2226. doi: 10.1200/JCO.2011.38.5740. doi:10.1200/JCO.2011.38.5740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Drukker CA, Bueno-de-Mesquita JM, Retel VP, et al. A prospective evaluation of a breast cancer prognosis signature in the observational RASTER study. Int J Cancer. 2013;131:929–936. doi: 10.1002/ijc.28082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pusztai L. Influence of genomics on adjuvant treatments for pre-invasive and invasive breast cancer. The Breast. 2013;22(Supp 1):S9. doi: 10.1016/j.breast.2013.07.015. Abstr. SP5.03) [DOI] [PubMed] [Google Scholar]
- 51.Nielsen TO, Parker JS, Leung S, et al. A comparison of PAM50 intrinsic subtyping with immunohistochemistry and clinical prognostic factors in tamoxifen-treated estrogen receptor-positive breast cancer. Clin Cancer Res. 2010;16:5222–5232. doi: 10.1158/1078-0432.CCR-10-1282. doi:10.1158/1078-0432.CCR-10-1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Dubsky P, Filipits M, Jakesz R, et al. Endopredict improves the prognostic classification derived from common clinical guidelines in ER-positive, HER2-negative early breast cancer. Ann Oncol. 2013;24:640–647. doi: 10.1093/annonc/mds334. doi:10.1093/annonc/mds334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sgroi D, Sestak I, Cuzick J, et al. Comparative performance of breast cancer index (BCI) versus oncotype DX and IHC4 in the prediction of late recurrence in hormonal receptor-positive lymph node negative breast cancer patients: a transATAC study. Presented at the 35th San Antonio Breast Cancer Symposium; December 4–8, 2012. Abstr S1–9. [Google Scholar]
- 54.Viale G. Characterization and clinical impact of residual disease after neoadjuvant chemotherapy. The Breast. 2013;22(Supp 1):S9. doi: 10.1016/j.breast.2013.07.016. Abstr. SP5.04) [DOI] [PubMed] [Google Scholar]
- 55.von Minckwitz G, Untch M, Blohmer JU, et al. Definition and impact of pathologic complete response on prognosis after neoadjuvant chemotherapy in various intrinsic breast cancer subtypes. J Clin Oncol. 2012;30:1796–1804. doi: 10.1200/JCO.2011.38.8595. doi:10.1200/JCO.2011.38.8595. [DOI] [PubMed] [Google Scholar]
- 56.Loi S, Sirtaine N, Piette F, et al. Prognostic and predictive value of tumor-infiltrating lymphocytes in a phase III randomized adjuvant breast cancer trial in node-positive breast cancer comparing the addition of docetaxel to doxorubicin with doxorubicin-based chemotherapy: BIG 02–98. J Clin Oncol. 2013;31:860–867. doi: 10.1200/JCO.2011.41.0902. doi:10.1200/JCO.2011.41.0902. [DOI] [PubMed] [Google Scholar]
- 57.Andre F. Risk stratification for treatment choice: opportunities, challenges and tools. The Breast. 2013;22(Supp 1):S10. Abstr. SP6.01) [Google Scholar]
- 58.Sotiriou C. Immune signatures: prognostic and predictive role in breast cancer. The Breast. 2013;22(Supp 1):S11. Abstr. SP6.04) [Google Scholar]
- 59.Curigliano G. Developing an effective breast cancer vaccine. The Breast. 2013;22(Supp 1):S10. doi: 10.1016/j.breast.2013.07.018. Abstr. SP6.02)(manuscript in preparation. [DOI] [PubMed] [Google Scholar]
- 60.Denkert C, Loibl S, Noske A, et al. Tumor-associated lymphocytes as an independent predictor of response to neoadjuvant chemotherapy in breast cancer. J Clin Oncol. 2010;28:105–113. doi: 10.1200/JCO.2009.23.7370. doi:10.1200/JCO.2009.23.7370. [DOI] [PubMed] [Google Scholar]
- 61.Morrow M. Personalizing extent of breast cancer surgery according to molecular subtypes. The Breast. 2013;22(Supp 1):S12. doi: 10.1016/j.breast.2013.07.020. Abstr. SP7.03) [DOI] [PubMed] [Google Scholar]
- 62.Kiess AP, McArthur HL, Mahoney K, et al. Adjuvant trastuzumab reduces locoregional recurrence in women who receive breast-conservation therapy for lymph node-negative, human epidermal growth factor receptor 2-positive breast cancer. Cancer. 2012;118:1982–1988. doi: 10.1002/cncr.26484. doi:10.1002/cncr.26484. [DOI] [PubMed] [Google Scholar]
- 63.Rutgers E. Who should not undergo breast conservation? The Breast. 2013;22(Supp 1):S13. doi: 10.1016/j.breast.2013.07.021. Abstr. SP7.04) [DOI] [PubMed] [Google Scholar]
- 64.Wood WC. Close/positive margins after breast-conserving therapy. The Breast. 2013;22(Supp 1):S13. doi: 10.1016/j.breast.2013.07.022. Abstr. SP7.05) [DOI] [PubMed] [Google Scholar]
- 65.Galimberti V, Cole BF, Zurrida S, et al. Axillary dissection versus no axillary dissection in patients with sentinel-node micrometastases (IBCSG 23–01): a phase 3 randomised controlled trial. Lancet Oncol. 2013;14:297–305. doi: 10.1016/S1470-2045(13)70035-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Giuliano AE, Hunt KK, Ballman KV, et al. Axillary dissection versus no axillary dissection in women with invasive breast cancer and sentinel node metastasis. JAMA. 2011;305:569–575. doi: 10.1001/jama.2011.90. doi:10.1001/jama.2011.90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gentilini O, Veronesi U. Abandoning sentinel lymph node biopsy in early breast cancer? A new trial in progress at the European Institute of Oncology of Milan (SOUND: sentinel node versus observation after axillary UltraSouND) Breast. 2012;21:678–681. doi: 10.1016/j.breast.2012.06.013. doi:10.1016/j.breast.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 68.Whelan TJ, Pignol JP, Levine MN, et al. Long-term results of hypofractionated radiation therapy for breast cancer. N Engl J Med. 2010;362:513–520. doi: 10.1056/NEJMoa0906260. doi:10.1056/NEJMoa0906260. [DOI] [PubMed] [Google Scholar]
- 69.Yarnold JR. The UK START (standardisation of breast radiotherapy) trials: 10-year follow-up results. Presented at the 35th San Antonio Breast Cancer Symposium; December 4–8, 2012. Abstr. S4–1. [Google Scholar]
- 70.Harris JR. Hypofractionation in the era of modulated radiotherapy. The Breast. 2013;22(Supp 1):S14. doi: 10.1016/j.breast.2013.07.024. Abstr. SP8.02) [DOI] [PubMed] [Google Scholar]
- 71.Orecchia R. Partial breast irradiation: targeting volume or breast molecular subtypes? The Breast. 2013;22(Supp 1):S14. doi: 10.1016/j.breast.2013.07.025. Abstr. SP8.01) [DOI] [PubMed] [Google Scholar]
- 72.Smith BD, Arthur DW, Buchholz TA, et al. Accelerated partial breast irradiation consensus statement from the American Society for Radiation Oncology (ASTRO) Int J Radiat Oncol Biol Phys. 2009;74:987–1001. doi: 10.1016/j.ijrobp.2009.02.031. doi:10.1016/j.ijrobp.2009.02.031. [DOI] [PubMed] [Google Scholar]
- 73.Polgar C, Van limbergen E, Potter R, et al. Patient selection for accelerated partial-breast irradiation (APBI) after breast-conserving surgery: recommendations of the Groupe Européen de Curiethérapie-European Society for Therapeutic Radiology and Oncology (GEC-ESTRO) breast cancer working group based on clinical evidence (2009) Radiother Oncol. 2010;94:264–273. doi: 10.1016/j.radonc.2010.01.014. doi:10.1016/j.radonc.2010.01.014. [DOI] [PubMed] [Google Scholar]
- 74.Sedlmayer F. Partial breast re-irradiation for local recurrence of breast carcinoma: benefit and potential long term side effects. The Breast. 2013;22(Supp 1):S15. doi: 10.1016/j.breast.2013.07.026. Abstr. SP8.04) [DOI] [PubMed] [Google Scholar]
- 75.Paik S, Tang G, Shak S, et al. Gene expression and benefit of chemotherapy in women with node-negative, estrogen receptor-positive breast cancer. J Clin Oncol. 2006;24:3726–3734. doi: 10.1200/JCO.2005.04.7985. doi:10.1200/JCO.2005.04.7985. [DOI] [PubMed] [Google Scholar]
- 76.Albain KS, Barlow WE, Shak S, et al. Prognostic and predictive value of the 21-gene recurrence score assay in postmenopausal women with node-positive, oestrogen-receptor-positive breast cancer on chemotherapy: a retrospective analysis of a randomised trial. Lancet Oncol. 2010;11:55–65. doi: 10.1016/S1470-2045(09)70314-6. doi:10.1016/S1470-2045(09)70314-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cheang MC, Voduc KD, Tu D, et al. Responsiveness of intrinsic subtypes to adjuvant anthracycline substitution in the NCIC.CTG MA.5 randomized trial. Clin Cancer Res. 2012;18:2402–2412. doi: 10.1158/1078-0432.CCR-11-2956. doi:10.1158/1078-0432.CCR-11-2956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Burstein HJ. Patients with triple-negative breast cancer: is there an optimal adjuvant treatment? The Breast. 2013;22(Supp 1):S16. doi: 10.1016/j.breast.2013.07.027. Abstr. SP9.02) [DOI] [PubMed] [Google Scholar]
- 79.Colleoni M. Extended adjuvant chemotherapy in endocrine non-responsive disease. The Breast. 2013;22(Supp 1):S17. doi: 10.1016/j.breast.2013.07.031. Abstr. SP10.01) [DOI] [PubMed] [Google Scholar]
- 80.von Minckwitz G. Selecting the neoadjuvant treatment by molecular subtype: how to maximise the benefit. The Breast. 2013;22(Supp 1):S16. doi: 10.1016/j.breast.2013.07.028. Abstr. SP9.03) [DOI] [PubMed] [Google Scholar]
- 81.Gianni L, Zambetti M, Clark K, et al. Gene expression profiles in paraffin-embedded core biopsy tissue predict response to chemotherapy in women with locally advanced breast cancer. J Clin Oncol. 2005;23:7265–7277. doi: 10.1200/JCO.2005.02.0818. doi:10.1200/JCO.2005.02.0818. [DOI] [PubMed] [Google Scholar]
- 82.Straver ME, Glas AM, Hannemann J, et al. The 70-gene signature as a response predictor for neoadjuvant chemotherapy in breast cancer. Breast Cancer Res Treat. 2010;119:551–558. doi: 10.1007/s10549-009-0333-1. doi:10.1007/s10549-009-0333-1. [DOI] [PubMed] [Google Scholar]
- 83.Piccart M. Patients with HER2 positive breast cancer: delivery, duration and combination therapies. The Breast. 2013;22(Supp 1):S16. doi: 10.1016/j.breast.2013.07.029. Abstr. SP9.04) [DOI] [PubMed] [Google Scholar]
- 84.Davidson NE. Optimal systemic therapy for premenopausal women with hormone receptor-positive breast cancer. The Breast. 2013;22(Supp 1):S18. doi: 10.1016/j.breast.2013.07.032. Abstr. SP10.02) [DOI] [PubMed] [Google Scholar]
- 85.Goss PE, Ingle JN, Martino S, et al. A randomized trial of letrozole in postmenopausal women after five years of tamoxifen therapy for early-stage breast cancer. N Engl J Med. 2003;349:1793–1802. doi: 10.1056/NEJMoa032312. doi:10.1056/NEJMoa032312. [DOI] [PubMed] [Google Scholar]
- 86.Goss PE, Ingle JN, Martino S, et al. Impact of premenopausal status at breast cancer diagnosis in women entered on the placebo-controlled NCIC CTG MA17 trial of extended adjuvant letrozole. Ann Oncol. 2013;24:355–361. doi: 10.1093/annonc/mds330. doi:10.1093/annonc/mds330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ingle JN. Postmenopausal women with hormone receptor-positive breast cancer: balancing benefit and toxicity from aromatase inhibitors. The Breast. 2013;22(Supp 1):S19. doi: 10.1016/j.breast.2013.07.035. Abstr. SP10.05) [DOI] [PubMed] [Google Scholar]
- 88.Amir E, Seruga B, Niraula S, et al. Toxicity of adjuvant endocrine therapy in postmenopausal breast cancer patients: a systematic review and meta-analysis. J Natl Cancer Inst. 2011;103:1299–1309. doi: 10.1093/jnci/djr242. doi:10.1093/jnci/djr242. [DOI] [PubMed] [Google Scholar]
- 89.Clarke CA, Keegan TH, Yang J, et al. Age-specific incidence of breast cancer subtypes: understanding the black-white crossover. J Natl Cancer Inst. 2012;104:1094–1101. doi: 10.1093/jnci/djs264. doi:10.1093/jnci/djs264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Loibl S, Jackisch C, Gade S. Neoadjuvant chemotherapy in the very young, 35 years of age or younger. Presented at the 35th San Antonio Breast Cancer Symposium; December 4–8, 2012. Abstr. S3–1. [Google Scholar]
- 91.Partridge AH. Management of breast cancer in the very young. The Breast. 2013;22(Supp 1):S18. Abstr. SP10.04) [Google Scholar]
- 92.Smith I. Follow-up tests to detect recurrent disease: patient's reassurance or medical need? The Breast. 2013;22(Supp 1):S17. doi: 10.1016/j.breast.2013.07.030. Abstr. SP9.05) [DOI] [PubMed] [Google Scholar]
- 93.Hayes DF. Targeting adjuvant chemotherapy: a good idea that needs to be proven! J Clin Oncol. 2012;30:1264–1267. doi: 10.1200/JCO.2011.38.4529. doi:10.1200/JCO.2011.38.4529. [DOI] [PubMed] [Google Scholar]
- 94.Coates AS, Colleoni M, Goldhirsch A. Is adjuvant chemotherapy useful for women with luminal A breast cancer? J Clin Oncol. 2012;30:1260–1263. doi: 10.1200/JCO.2011.37.7879. doi:10.1200/JCO.2011.37.7879. [DOI] [PubMed] [Google Scholar]
- 95.Prat A, Parker JS, Fan C, et al. Concordance among gene expression-based predictors for ER-positive breast cancer treated with adjuvant tamoxifen. Ann Oncol. 2012;23:2866–2873. doi: 10.1093/annonc/mds080. doi:10.1093/annonc/mds080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Regan MM, Pagani O, Walley B, et al. Premenopausal endocrine-responsive early breast cancer: who receives chemotherapy? Ann Oncol. 2008;19:1231–1241. doi: 10.1093/annonc/mdn037. doi:10.1093/annonc/mdn037. [DOI] [PubMed] [Google Scholar]
- 97.Wirapati P, Sotiriou C, Kunkel S, et al. Meta-analysis of gene expression profiles in breast cancer: toward a unified understanding of breast cancer subtyping and prognosis signatures. Breast Cancer Res. 2008;10:R65. doi: 10.1186/bcr2124. doi:10.1186/bcr2124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Reed SD, Dinan MA, Schulman KA, et al. Cost-effectiveness of the 21-gene recurrence score assay in the context of multifactorial decision making to guide chemotherapy for early-stage breast cancer. Genet Med. 2013;15:203–211. doi: 10.1038/gim.2012.119. doi:10.1038/gim.2012.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Vanderlaan BF, Broder MS, Chang EY, et al. Cost-effectiveness of 21-gene assay in node-positive, early-stage breast cancer. Am J Manag Care. 2011;17:455–464. [PubMed] [Google Scholar]
- 100.Davidson JA, Cromwell I, Ellard SL, et al. A prospective clinical utility and pharmacoeconomic study of the impact of the 21-gene recurrence score(R) assay in oestrogen receptor positive node negative breast cancer. Eur J Cancer. 2013 doi: 10.1016/j.ejca.2013.03.009. April 20 [epub ahead of print] doi: 10.1016/j.ejca.2013.03.009. [DOI] [PubMed] [Google Scholar]
- 101.Hannouf MB, Xie B, Brackstone M, et al. Cost-effectiveness of a 21-gene recurrence score assay versus Canadian clinical practice in women with early-stage estrogen- or progesterone-receptor-positive, axillary lymph-node negative breast cancer. BMC Cancer. 2012;12:447. doi: 10.1186/1471-2407-12-447. doi:10.1186/1471-2407-12–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Lamond NW, Skedgel C, Rayson D, et al. Cost-utility of the 21-gene recurrence score assay in node-negative and node-positive breast cancer. Breast Cancer Res Treat. 2012;133:1115–1123. doi: 10.1007/s10549-012-1989-5. doi:10.1007/s10549-012-1989-5. [DOI] [PubMed] [Google Scholar]
- 103.Tsoi DT, Inoue M, Kelly CM, et al. Cost-effectiveness analysis of recurrence score-guided treatment using a 21-gene assay in early breast cancer. Oncologist. 2010;15:457–465. doi: 10.1634/theoncologist.2009-0275. doi:10.1634/theoncologist.2009-0275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Hornberger J, Cosler LE, Lyman GH. Economic analysis of targeting chemotherapy using a 21-gene RT-PCR assay in lymph-node-negative, estrogen-receptor-positive, early-stage breast cancer. Am J Manag Care. 2005;11:313–324. [PubMed] [Google Scholar]
- 105.Klang SH, Hammerman A, Liebermann N, et al. Economic implications of 21-gene breast cancer risk assay from the perspective of an Israeli-managed health-care organization. Value Health. 2010;13:381–387. doi: 10.1111/j.1524-4733.2010.00724.x. doi:10.1111/j.1524-4733.2010.00724.x. [DOI] [PubMed] [Google Scholar]
- 106.Hall PS, McCabe C, Stein RC, et al. Economic evaluation of genomic test-directed chemotherapy for early-stage lymph node-positive breast cancer. J Natl Cancer Inst. 2012;104:56–66. doi: 10.1093/jnci/djr484. doi:10.1093/jnci/djr484. [DOI] [PubMed] [Google Scholar]
- 107.Blohmer JU, Rezai M, Kummel S, et al. Using the 21-gene assay to guide adjuvant chemotherapy decision-making in early-stage breast cancer: a cost-effectiveness evaluation in the German setting. J Med Econ. 2013;16:30–40. doi: 10.3111/13696998.2012.722572. doi:10.3111/13696998.2012.722572. [DOI] [PubMed] [Google Scholar]
- 108.Eiermann W, Rezai M, Kummel S, et al. The 21-gene recurrence score assay impacts adjuvant therapy recommendations for ER-positive, node-negative and node-positive early breast cancer resulting in a risk-adapted change in chemotherapy use. Ann Oncol. 2013;24:618–624. doi: 10.1093/annonc/mds512. doi:10.1093/annonc/mds512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kondo M, Hoshi SL, Ishiguro H, et al. Economic evaluation of the 70-gene prognosis-signature (MammaPrint(R)) in hormone receptor-positive, lymph node-negative, human epidermal growth factor receptor type 2-negative early stage breast cancer in Japan. Breast Cancer Res Treat. 2012;133:759–768. doi: 10.1007/s10549-012-1979-7. doi:10.1007/s10549-012-1979-7. [DOI] [PubMed] [Google Scholar]
- 110.Sahin AA, Ro J, Ro JY, et al. Ki-67 immunostaining in node-negative stage I/II breast carcinoma: significant correlation with prognosis. Cancer. 1991;68:549–557. doi: 10.1002/1097-0142(19910801)68:3<549::aid-cncr2820680318>3.0.co;2-j. doi:10.1002/1097-0142(19910801)68:3<549::AID-CNCR2820680318>3.0.CO;2-J. [DOI] [PubMed] [Google Scholar]
- 111.Railo M, Lundin J, Haglund C, et al. Ki-67, p53, ER-receptors, ploidy and S-phase as prognostic factors in T1 node negative breast cancer. Acta Oncol. 1997;36:369–374. doi: 10.3109/02841869709001282. doi:10.3109/02841869709001282. [DOI] [PubMed] [Google Scholar]
- 112.Jansen RL, Hupperets PS, Arends JW, et al. MIB-1 labelling index is an independent prognostic marker in primary breast cancer. Br J Cancer. 1998;78:460–465. doi: 10.1038/bjc.1998.515. doi:10.1038/bjc.1998.515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Mirza AN, Mirza NQ, Vlastos G, et al. Prognostic factors in node-negative breast cancer: a review of studies with sample size more than 200 and follow-up more than 5 years. Ann Surg. 2002;235:10–26. doi: 10.1097/00000658-200201000-00003. doi:10.1097/00000658-200201000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Trihia H, Murray S, Price K, et al. Ki-67 expression in breast carcinoma. Cancer. 2003;97:1321–1331. doi: 10.1002/cncr.11188. doi:10.1002/cncr.11188. [DOI] [PubMed] [Google Scholar]
- 115.de Azambuja E, Cardoso F, de CG, Jr, et al. Ki-67 as prognostic marker in early breast cancer: a meta-analysis of published studies involving 12 155 patients. Br J Cancer. 2007;96:1504–1513. doi: 10.1038/sj.bjc.6603756. doi:10.1038/sj.bjc.6603756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Dowsett M, Smith IE, Ebbs SR, et al. Prognostic value of Ki67 expression after short-term presurgical endocrine therapy for primary breast cancer. J Natl Cancer Inst. 2007;99:167–170. doi: 10.1093/jnci/djk020. doi:10.1093/jnci/djk020. [DOI] [PubMed] [Google Scholar]
- 117.Viale G, Regan MM, Mastropasqua MG, et al. Value of Ki-67 in two randomized trials of adjuvant chemo-endocrine therapies for node-negative breast cancer. J Natl Cancer Inst. 2008;100:207–212. doi: 10.1093/jnci/djm289. doi:10.1093/jnci/djm289. [DOI] [PubMed] [Google Scholar]
- 118.Viale G, Giobbie-Hurder A, Regan MM, et al. Prognostic and predictive value of centrally reviewed Ki-67 labeling index in postmenopausal women with endocrine-responsive breast cancer: results from Breast International Group trial 1–98 comparing adjuvant tamoxifen with letrozole. J Clin Oncol. 2008;26:5569–5575. doi: 10.1200/JCO.2008.17.0829. doi:10.1200/JCO.2008.17.0829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Muss HB, Berry DA, Cirrincione CT, et al. Adjuvant chemotherapy in older women with early stage breast cancer. N Engl J Med. 2009;360:2055–2065. doi: 10.1056/NEJMoa0810266. doi:10.1056/NEJMoa0810266. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


