Abstract
Objective:
The increasing use of point-of-care ultrasonography for targeted procedures justifies a device that helps both novices in training and experts perform the long-axis needle approach. The initial success of traditional needle guidance devices in reducing the time of target procedures is not universal and they can be cumbersome. We aim to investigate whether the less bulky and previously untested laser guide can succeed in reducing procedure time in novice ultrasonographers.
Methods:
82 medical students with no ultrasound experience volunteered. Random allocation determined whether, during a targeted procedure in a turkey breast and olive phantom, participants were assisted by the laser guide or not. The time taken to pierce the target was recorded at 1-cm depth.
Results:
The mean procedure time in the laser-assisted (LA) group was 25.1 s (14.0 s; 18.0–25.0 s). The mean procedure time in the free-hand group was 45.5 s (23.0 s; 7.0–55.0 s). The procedure time in the LA group was significantly reduced (p<0.01).
Conclusion:
The laser guide significantly improved procedure times. It is felt that the cheaper, smaller, easy to integrate, sterile and more user-friendly laser guidance unit may be a better alternative to the needle guide in improving procedure times for the novice ultrasonographer or to assist the expert, during training for, or performance of, ultrasound-guided targeted procedures.
Advances in knowledge:
Following from the prototype paper, this is the first study to investigate the effectiveness of attaching a laser-guidance device to an ultrasound probe. The device succeeded in reducing the procedure times of targeted procedures.
Over the past 20 years, the development of ultrasound equipment that is both affordable and compact has permitted the development of point-of-care ultrasonography, a technology that is increasingly used by a variety of medical specialities and performed by clinicians whose primary specialisation is not radiology [1]. Point-of-care ultrasonography in the form of ultrasound guidance can improve the success rate, and reduce the complication rate, of many clinical procedures [2].
This partnership of needle tip and imaging permits the clinician to achieve direct continuous observation of the needle tip and, more importantly, its relation to the target site and surrounding anatomy. However, although most novices master basic ultrasound skills easily, it was found that under ultrasound guidance, 70% of beginners failed accurately to locate an advancing needle tip. Education in basic needle insertion techniques is therefore a priority [3].
Needle insertion can be performed in one of two ways. The long-axis, or in-plane, approach, which aligns the needle and the long axis of the ultrasound beam, achieves a more complete view of the needle. By contrast, during the short-axis, or out-of-plane, approach, where the needle is aligned perpendicular to the ultrasound beam, the on-screen image of the needle is only a small white dot and therefore the exact location of the needle tip in relation to collateral structures is less certain.
However, even during the long-axis approach, the location of the needle tip is only a certainty if the clinician can align the needle within the short axis of the ultrasound beam, which may be only 0.3 mm wide. This difficult skill may be learned and/or performed more quickly by attaching one of the two types of assisting apparatus (a needle guide or a portable laser guide) down the midline of the ultrasound probe [4–8]; a line present on most probes, which marks the location and orientation of the ultrasound beam. By eliminating some of the potential planes of error, these devices can assist the operator in the long-axis alignment of the needle and the ultrasound beam.
The needle guide fixes the needle in place, whereas the portable laser guide, as used in this study (Figure 1), assists the operator by projecting onto the skin a laser line that mimics the invisible ultrasound beam. Using the laser, the operator can only remove two planes of error if, whilst keeping the probe stationary, they penetrate the skin, bisect the projected line and ensure that the length of the needle shaft remains within the projected laser beam at all times during the procedure. This requires more hand–eye co-ordination than the needle guide; however, the laser guide does permit some flexibility of movement which, over time, will improve the operator's hand–eye co-ordination (for use when assisting apparatus is unavailable) and also allows the laser guide to be ignored, should the more experienced operator prefer. With this in mind, the laser guide might not only be of use in training the novice but also appeal more than the needle guide to the specialist ultrasonographer. There are currently no published trials investigating the success of using an in-plane laser guide in either novices or experts.
Figure 1.
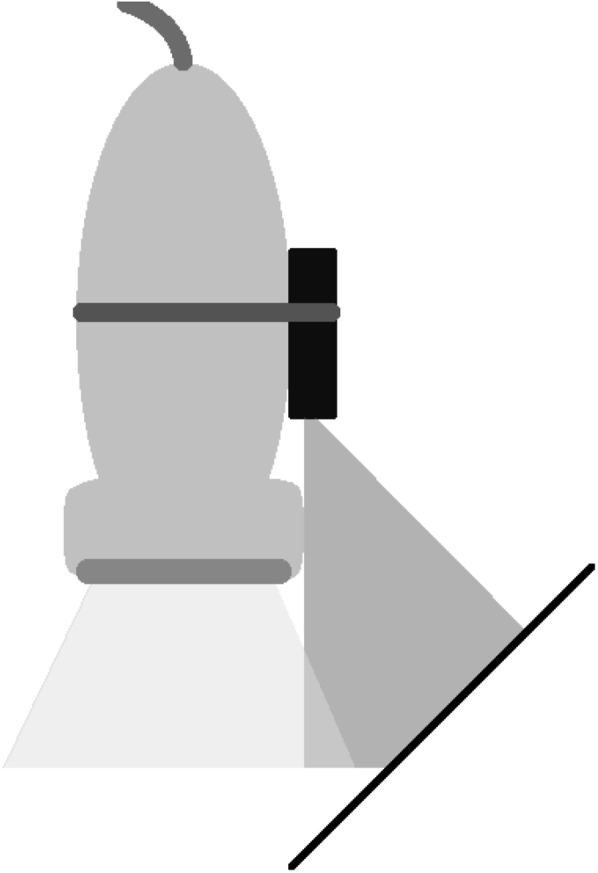
Diagram of ultrasound probe, laser and needle. The ultrasound probe (top left) is attached to the activated laser guidance device (bottom right), which is in-plane with the invisible ultrasound beam (bottom left). If the user bisects the projected laser beam (bottom right) when penetrating the skin with the needle and keeps the shaft of the needle (bottom right) within the laser beam during the procedure, then the laser can assist the user in keeping the needle in-plane with the ultrasound beam as demonstrated.
In this in vitro study, we investigate whether a portable laser guidance unit can assist novices in performing an in-plane ultrasound-guided targeted procedure using a turkey breast and olive phantom [9]. The null hypothesis is that the portable laser guidance unit does not significantly improve the time taken to puncture the target.
MATERIALS AND METHODS
A total of 82 pre-clinical and clinical medical students were voluntarily enrolled in the study. All participants were confirmed free from visual impairment and previous ultrasound experience. The subjects were randomly allocated to either the laser-assisted (LA) group or the free-hand (FH) group and, alongside an introduction to the long-axis approach, a demonstration of the basic handling of the equipment was provided. However, neither the previous participants nor the researcher were permitted to demonstrate the procedure to each participant before they began.
The set-up was assembled by a senior radiology registrar (Figure 2) and included the turkey breast and olive phantom [9], a 1.2×90 mm 18-gauge Quincke-type spinal needle (Becton Dickinson and Co., Franklin Lakes, NJ) and a Philips HD11 XE portable ultrasound machine (Philips Medical Systems Technologies Ltd, Bothell, WA) equipped with the Philips L12-3 3–12-MHz broadband linear array transducer (Philips Medical Systems, Eindhoven, Netherlands). Strapped vertically and centrally down the midline of the transducer was the laser unit (Line Generator Laser Diode Module LML; Apinex, Montreal, Canada), a battery operated small-line laser guidance unit that was adjusted until the 1-mm-wide laser guideline projected along the midline of the probe so as to be in-plane with the short axis of the invisible ultrasound beam as described previously by Tsui [5] (Figure 1).
Figure 2.
Diagram representing the relative positions of the participant, probe, ultrasound machine and phantom. Participants were seated in front of the ultrasound machine at a table, upon which rested the turkey breast and olive phantom, the needle and the ultrasound probe. With the probe in their non-dominant hand and the needle in the other, participants were timed as they performed the procedure.
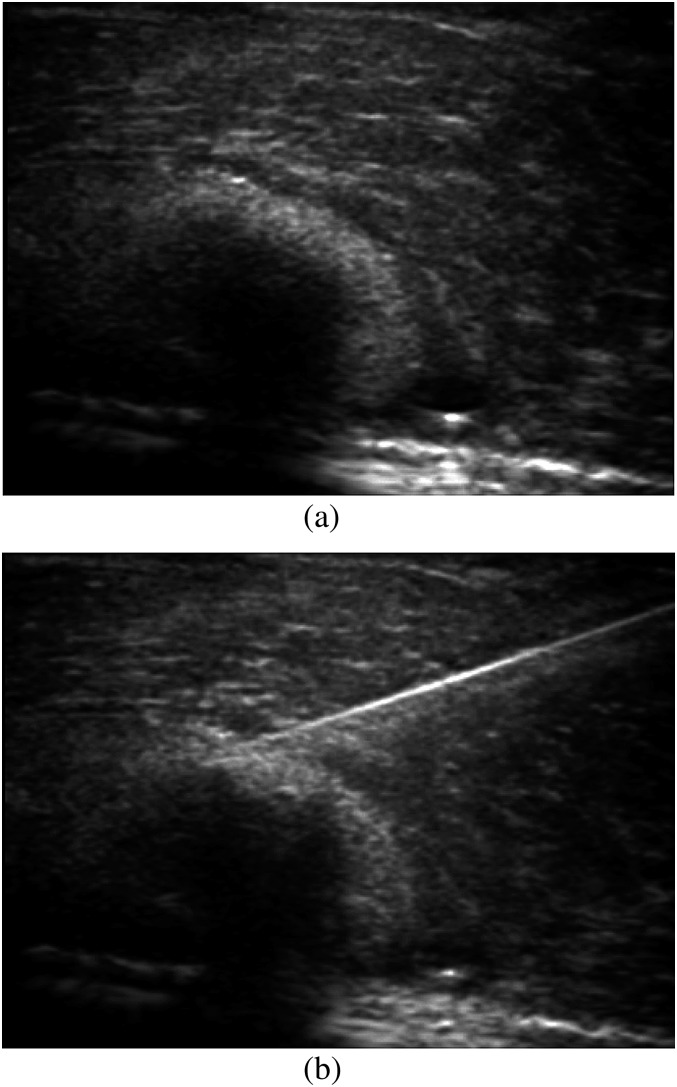
Once the participants had located the olive and localised it to the left side of the screen, the instructor optimised the image by altering the gain, depth and resolution settings. The measured variable was the time from needle insertion (Figure 3a) to visualisation of the entire in-plane needle on the screen, with the tip penetrating the olive (Figure 3b).
Figure 3.
Ultrasound image of the study start and end points. (a) The participant began and the timer was started when the needle was poised to begin the procedure and this image of the olive (bottom left) beneath the turkey breast was visible on the ultrasound screen. (b) The participant finished and the timer was stopped at the point when the needle pierced the olive.
The sample size calculation demonstrated that, for α=0.05, (1−β)=0.9 and Δ=0.5, approximately 42 subjects would be needed. The procedure times were recorded at 1-cm depth and then assembled into a spreadsheet for analysis. Wilcoxon's signed-rank tests were performed to compare the groups, with p<0.05 considered statistically significant. Data are provided as mean (median; interquartile range).
RESULTS
The mean procedure time in the LA group was 25.1 s (14.0 s; 18.0–25.0 s). By comparison, the mean procedure time in the FH group was 45.5 s (23.0 s; 7.0–55.0 s). The procedure time in the LA group was significantly reduced (p<0.01).
DISCUSSION
Our study is the first inquiry into the effect that attaching a portable laser guidance unit to an ultrasound probe has on the time taken to puncture a target with a needle during ultrasound-guided targeted procedures. We have demonstrated that in the novice ultrasound user, laser guidance significantly reduced the time taken to complete a targeted procedure.
It is well established that during ultrasound-guided targeted procedures, speed and accuracy are of paramount importance for patient safety and both are improved by enhancing the operator's ability to visualise the needle during the procedure [10,11]. Current methods to improve needle visualisation include echo-enhanced needles [12–16], the use of visualisation-enhancing ultrasound characteristics [17–19] and the use of the long-axis approach, which offers better needle visualisation than the short-axis approach [20,21]. However, in one study, novice ultrasonographers found the long-axis approach more difficult than the short-axis approach, with longer procedure times, more skin breaks and more needle redirections [22]. To reduce over-reliance on the operator's hand–eye co-ordination and to shorten the learning curve of the procedure, it has been suggested that two planes of human error be removed by the addition of assistance apparatus, of which the two main examples are the laser guide and the needle guide. Needle guide devices have been studied in multiple instances, but this study is the first to investigate the effectiveness of the laser guidance device. Although initially unpopular because they prevented re-angulation and fine adjustment of the needle during its approach to the target [23], three more recent studies have investigated improved needle guides that allow for re-angulation and fine adjustment [6–8]. In all studies, although needle visualisation with the needle guide was significantly improved, the time taken to puncture the target, when compared with the free-hand technique, was not universally improved.
In our study of novice ultrasonographers, the observed improvement in procedural time in the LA group disproves our null hypothesis; the portable laser guide does indeed significantly improve the time taken to puncture the target. As was alluded to in the prototype paper, the addition of a laser guidance device to the ultrasound probe does make the process of ultrasound guidance easier [5] and also speeds up the procedure; the addition of an in-plane laser guidance unit to the ultrasound probe may also reduce the level of patient discomfort. Finally, although perfect synchronicity between the probe hand and the needle hand may be seen as an advantage unique to needle guidance devices, personal preference in some expert users may perceive this inflexibility to be a burden, and therefore a disadvantage unique to the needle guide. Regardless, in comparison with portable laser guidance devices, needle guides are cumbersome, costly and require removal, sterilisation and re-attachment between uses. Therefore, in any safety and cost-conscious healthcare system, the cheap, small, easy to integrate, sterile and more user-friendly laser guidance unit may be a better alternative to the needle guide either to speed up ultrasound-guided procedures in novice ultrasonographers or to assist the expert, during training for, or performance of, in-plane ultrasound-guided targeted procedures. However, the efficacy of the laser guidance device in the experienced radiographer is beyond the scope of the current study.
Further limitations to our study include the following:
Depth of target: testing deeper targets would determine the effectiveness of the laser guidance device during more challenging punctures. As the laser guidance device does not control the needle angle but only the needle plane, it is possible that the laser guidance device is more useful at shallower depths.
Phantom selection: although the olive provides a reasonable phantom for a biopsy, it poorly represents other ultrasound-guided targeted procedures, such as regional anaesthesia, where a smaller, deeper target would be usual. Furthermore, turkey tissue is homogenous, thin, absent of features mimicking fascia, skin and fat and insensitive to pain; therefore, this study might be improved by using both larger and smaller phantoms that are porcine, cadaveric or the live human model. This would also provide an opportunity for our findings to be verified in more realistic and clinically relevant scenarios. In addition, a phantom of increased size and volume may provide a solution to the following limitation, the measured variable.
Time measurement: a longer procedure is not necessarily inferior to a shorter one; attention to detail, accuracy and clinical effectiveness are vital. As a primary end point, recording time is inferior to other measures like patient safety, satisfaction and outcomes. These are better recorded in the clinical setting. Also, for a more comprehensive picture of the laser guide’s effectiveness as well as for comparison with other needle guide studies, a useful improvement would be to measure the proportion of time that the needle tip is visualised and the number of needle redirections, both perpendicular to the surface, also at different specified angles of insertion, which is sometimes needed to optimise nerve visualisation.
Experience: it has been shown that even in experienced ultrasonographers, needle guides can significantly facilitate visualisation of needle passage in vitro [7]. However, the current study excluded participants with prior ultrasound experience. It is unusual for an ultrasonographer or a radiologist to perform such a procedure without significant experience handling ultrasound probes. In addition, testing in novices generates more randomness to the data. Therefore, although participants in the LA group did find the laser device straightforward to use, further investigations could be done in slightly more experienced users, either after a short demonstration of the procedure, after a period of practice, or indeed in fully trained specialist ultrasonographers or radiologists. This would reduce randomness and be of more clinical relevance and is also of particular importance when our long-term ambition of fully integrating a laser guidance device into an ultrasound probe is achieved. This is an ambition that, owing to the integration of probe and laser, would alleviate any of the aforementioned momentary minor misalignments that impair the ability of the laser guide to mimic the plane of the ultrasound beam.
Sterility: the concomitant use of a sterile sleeve and the portable laser guidance unit did not prove problematic in our model as the laser beam penetrates the loose sterile covers easily [5].
Comparison with other guidance devices: our anecdotal evidence that justified the testing of the laser guidance device over the needle guidance device should be formalised by comparing the efficacy of one against the other.
CONCLUSION
In conclusion, this study, the first to investigate whether the addition of an in-plane laser guidance device can assist long-axis ultrasound-guided targeted procedures, has demonstrated a significant reduction in procedure time with the laser guidance device, in comparison with the FH group, among novice ultrasonographers. Speedy and accurate in-plane alignment of the needle and the ultrasound beam is one of the more difficult tasks to master during ultrasound guidance training, and we have demonstrated that the laser guidance apparatus can speed up the procedure. Therefore, although the usefulness of the apparatus in professional radiologists remains to be seen, such a device could be beneficial for trainees and also those non-radiologists who are increasingly learning to perform point-of-care ultrasound-guided procedures across a variety of medical specialties.
REFERENCES
- 1.Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med 2011;364:749–57 10.1056/NEJMra0909487 [DOI] [PubMed] [Google Scholar]
- 2.Nicolaou S, Talsky A, Khashoggi K, Venu V. Ultrasound-guided interventional radiology in critical care. Crit Care Med 2007;35:186–97 10.1097/01.CCM.0000260630.68855.DF [DOI] [PubMed] [Google Scholar]
- 3.Sites BD, Gallagher JD, Cravero J, Lumdberg J, Blike G. The learning curve associated with a simulated ultrasound-guided interventional task by inexperienced anesthesia residents. Reg Anesth Pain Med 2004;29:544–8 [DOI] [PubMed] [Google Scholar]
- 4.Tsui BCH. Equipment for regional anesthesia in children. Tech Reg Anesth Pain Manage 2007;11:235–46 [Google Scholar]
- 5.Tsui BC. Facilitating needle alignment in-plane to an ultrasound beam using a portable laser unit. Reg Anesth Pain Med 2007;32:84–8 10.1016/j.rapm.2006.09.009 [DOI] [PubMed] [Google Scholar]
- 6.van Geffen GJ, Mulder J, Gielen M, Van Egmond J, Scheffer GJ, Bruhn J. A needle guidance device compared to free hand technique in an ultrasound-guided interventional task using a phantom. Anaesthesia 2008;63:986–90 10.1111/j.1365-2044.2008.05524.x [DOI] [PubMed] [Google Scholar]
- 7.Wang AZ, Zhang WX, Jiang W. A needle-guide can facilitate visualization of needle passage in ultrasound-guided nerve blocks. J Clin Anesth 2009;21:230–2 10.1016/j.jclinane.2008.08.014 [DOI] [PubMed] [Google Scholar]
- 8.Ball RD, Scouras NE, Orebaugh S, Wilde J, Sakai T. Randomized, prospective, observational simulation study comparing residents' needle-guided vs free-hand ultrasound techniques for central venous catheter access. Br J Anaesth 2012;108:72–9 [DOI] [PubMed] [Google Scholar]
- 9.Harvey JA, Moran RE, Hamer MM, DeAngelis GA, Omary RA. Evaluation of a turkey-breast phantom for teaching freehand, US-guided core-needle breast biopsy. Acad Radiol 1997;4:565–9 [DOI] [PubMed] [Google Scholar]
- 10.Chin KJ, Perlas A, Chan VW, Brull R. Needle visualization in ultrasound-guided regional anesthesia: challenges and solutions. Reg Anesth Pain Med 2008;33:532–44 [DOI] [PubMed] [Google Scholar]
- 11.Moak JH, Lyons MS, Wright SW, Lindsell CJ. Needle and guidewire visualization in ultrasound-guided internal jugular vein cannulation. Am J Emerg Med 2011;29:432–6 10.1016/j.ajem.2010.01.004 [DOI] [PubMed] [Google Scholar]
- 12.Vucevic M, Tehan B, Gamlin F, Berridge JC, Boylan M. The SMART needle. A new Doppler ultrasound-guided vascular access needle. Anaesthesia 1994;49:889–91 [DOI] [PubMed] [Google Scholar]
- 13.Hopkins RE, Bradley M. In-vitro visualization of biopsy needles with ultrasound: a comparative study of standard and echogenic needles using an ultrasound phantom. Clin Radiol 2001;56:499–502 10.1053/crad.2000.0707 [DOI] [PubMed] [Google Scholar]
- 14.Phelan MP, Emerman C, Peacock WF, Karafa M, Colburn N, Buchanan K. Do echo-enhanced needles improve time to cannulate in a model of short-axis ultrasound-guided vascular access for a group of mostly inexperienced ultrasound users? Int J Emerg Med 2009;2:167–70 10.1007/s12245-009-0114-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Venkatesan K. Echo-enhanced needles for short-axis ultrasound-guided vascular access. Int J Emerg Med 2010;3:205 10.1007/s12245-010-0164-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hebard S, Hocking G. Echogenic technology can improve needle visibility during ultrasound-guided regional anesthesia. Reg Anesth Pain Med 2011;36:185–9 [DOI] [PubMed] [Google Scholar]
- 17.Karstrup S, Brøns J, Morsel L, Juul N, von der Recke P. Optimal set-up for ultrasound guided punctures using new scanner applications: an in-vitro study. Eur J Ultrasound 2002;15:77–84 [DOI] [PubMed] [Google Scholar]
- 18.Schafhalter-Zoppoth I, McCulloch CE, Gray AT. Ultrasound visibility of needles used for regional nerve block: an in vitro study. Reg Anesth Pain Med 2004;29:480–8 [PubMed] [Google Scholar]
- 19.Maecken T, Zenz M, Grau T. Ultrasound characteristics of needles for regional anesthesia. Reg Anesth Pain Med 2007;32:440–7 10.1016/j.rapm.2007.07.002 [DOI] [PubMed] [Google Scholar]
- 20.Stone MB, Moon C, Sutijono D, Blaivas M. Needle tip visualization during ultrasound-guided vascular access: short-axis vs long-axis approach. Am J Emerg Med 2010;28:343–7 10.1016/j.ajem.2008.11.022 [DOI] [PubMed] [Google Scholar]
- 21.Sierzenski P, Polan DL, Baty G, Nichols WL, Kochert E, Bollinger M, et al. Junior emergency medicine residents demonstrate improved accuracy for the identification of a central venous needle-tip with a long-axis ultrasound transducer orientation. Ann Emerg Med 2008;52:5 [Google Scholar]
- 22.Blaivas M, Brannam L, Fernandez E. Short-axis versus long-axis approaches for teaching ultrasound-guided vascular access on a new inanimate model. Acad Emerg Med 2003;10:1307–11 [DOI] [PubMed] [Google Scholar]
- 23.Phal PM, Brooks DM, Wolfe R. Sonographically guided biopsy of focal lesions: a comparison of freehand and probe-guided techniques using a phantom. AJR Am J Roentgenol 2005;184:1652–6 10.2214/ajr.184.5.01841652 [DOI] [PubMed] [Google Scholar]