Abstract
The objective of this study was to establish the impact of three-dimensional conformal radiotherapy (3D-CRT) technique in post-operative radiotherapy of gastric cancer. A bibliographical research was performed using the PubMed. On the database, Search was carried out using Medical Subject Heading (MeSH) database; the algorithm for search was ‘‘Radiotherapy” (MeSH) AND ‘‘Stomach Neoplasms” (MeSH). Only planning comparative studies on conformal techniques vs standard techniques in post-operative radiotherapy of gastric cancer were included in the review process. We identified 185 papers, five of them fulfilling the inclusion criteria. A great inhomogeneity was observed regarding the analysed dosimetric end points. Three of the five studies reported a benefit in favour of 3D-CRT for target irradiation despite a minimal advantage in most cases. The liver was better spared from irradiation by the traditional technique in all studies. No univocal result was obtained for the right kidney: the traditional technique performed better in two studies, 3D-CRT yielded better results in two others, whereas in the fifth study, each technique was either better or worse according to the different considered end point. 3D-CRT, however, allowed for better sparing of the left kidney in four studies. There is no absolute reason to prefer 3D-CRT with multiple beams in every patient. It may be preferable to choose the technique based on individual patient characteristics. Because there is no proof of superiority for 3D-CRT, there is no absolute reason to exclude patients who are treated in centres equipped with only the two-dimensional technique from the potential benefit of post-operative chemoradiation.
Gastric cancer remains the second most common gastrointestinal malignancy internationally and is responsible for most gastrointestinal cancer-related deaths worldwide [1]. According to Jemal et al [2], there were 21 130 new cases of gastric cancer reported in the USA in 2009.
Surgical resection of adenocarcinoma of the stomach is curative in <40% of cases. Although adjunctive therapeutic strategies vary by region, each strategy has improved the cure rates compared with surgery alone by approximately 10% [3–5]; therefore, adjunctive therapies should be offered to all high-risk gastric cancer patients. In the Western world, most high-risk patients often receive post-operative chemoradiation [4] or pre-operative and post-operative chemotherapy [3], whereas in Japan, such patients receive adjuvant S-1 chemotherapy following a D2 dissection [5].
Locoregional recurrence is a significant problem with a reported rate of 23–38% [6–8], emphasising the need for adjuvant local therapy. Macdonald et al [4] investigated the effect of surgery plus post-operative (adjuvant) chemoradiation on the survival of patients with resectable adenocarcinoma of the stomach or gastroesophageal junction. A total of 556 patients with resected adenocarcinoma of the stomach or gastroesophageal junction were randomly assigned to surgery plus post-operative chemoradiation or surgery alone. The median overall survival was 27 months in the surgery alone group and 36 months in the chemoradiation group. The authors concluded that post-operative chemoradiation should be considered for all patients at high risk for recurrence by adenocarcinoma of the stomach or gastroesophageal junction who have undergone curative resection. However, of the 281 patients assigned to the chemoradiation group, only 181 (64%) completed treatment as planned; 49 (17%) stopped treatment because of toxic effects [4].
Given the poor overall prognosis and significant toxicity owing to chemotherapy administered concurrently with radiotherapy with large radiation fields, there is a need to improve the standard treatment. Several attempts to reduce toxicity by sparing organs at risk (OAR) with advanced techniques were carried out. In particular, several planning studies to compare the standard two-dimensional (2D) with the three-dimensional (3D) conformal technique have been performed [9–13]. However, the results are still sparse and frequently conflicting. Thus, the aim of this study was to collect all available published information to establish the impact of 3D conformal technique in post-operative radiotherapy of gastric cancer.
METHODOLOGY
Literature search strategy
A bibliographical research was performed using PubMed. On the database, a search was carried out using Medical Subject Heading (MeSH) database; the algorithm for search was ‘‘Radiotherapy” [MeSH] AND ‘‘Stomach Neoplasms” [MeSH]. In order to identify other possible studies of interest, this process was supplemented by manual examination of reference lists for the available review articles. The search was limited to the time interval of 1 January 2000 to 1 January 2012 for homogeneity reasons. It was restricted to English language journal papers. Titles, abstracts and keywords of found articles were independently read by the researcher and the supervisor. Potentially eligible studies were retrieved and a full-text evaluation was performed as to whether they satisfied the inclusion and exclusion criteria. Only studies that reported treatment plan comparison between conformal techniques and standard techniques in post-operative radiotherapy of gastric cancer were included in the review process. Studies including patients with treatment directed to metastatic sites were excluded as well as clinical studies.
RESULTS
Search results
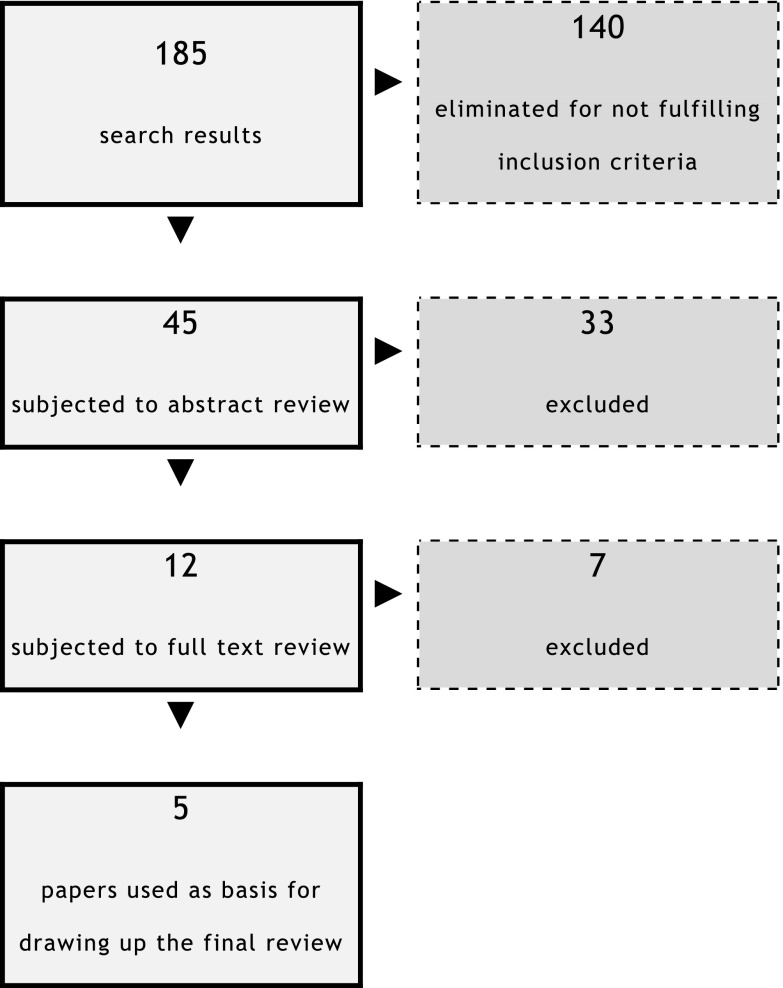
Through the literature search, performed as previously described, we identified 185 papers. Figure 1 describes the reasons for the exclusion of 180 articles. Therefore, five studies fulfilled the inclusion criteria and were included in this review [9–13].
Figure 1.
Publications selection.
Literature review
Wieland et al [9] published a dosimetric comparison to evaluate the relative merits of different approaches with intensity-modulated radiotherapy (IMRT). They performed a plan comparison between a step-and-shoot IMRT class solution, a set-up with two opposed anteroposterior–posteroanterior (AP–PA) fields, a conventional box technique and the Peacock tomotherapy approach. The study results showed that the median kidney dose generated from the IMRT plans is reduced individually by >50% for the kidney with the highest exposure (usually the left kidney) from 20 Gy to 30 Gy with conventional 3D planning and down to values between 8 and 10 Gy for IMRT. On average, the median dose to the right kidney was the same for the conventional box technique and IMRT (between 8 and 10 Gy) but lower for the AP–PA technique. Furthermore, the median dose to the liver was subcritical with all modalities but lowest with AP–PA fields.
Leong et al [10] described a multiple-field conformal radiotherapy technique and compared this technique with the more commonly used AP–PA technique that was used in the Intergroup study (INT0116) [4]. The two techniques were compared for target volume coverage and dose to normal tissues using dose–volume histogram (DVH) analysis. According to their findings, the conformal technique provides more adequate coverage of the target volume, with 99% of the planning target volume (PTV) receiving 95% of the prescribed dose compared with 93% using AP–PA fields. Comparative DVHs for the right kidney, left kidney and spinal cord demonstrated lower radiation doses using the conformal technique, and although the liver dose was higher, it was still well below liver tolerance. The authors concluded that 3D-conformal radiotherapy (3D-CRT) produces superior dose distributions and reduced radiation doses to the kidneys and spinal cord compared with the AP–PA technique, with the potential to reduce treatment toxicity.
Milano et al [11] compared IMRT planning with two-field (AP–PA) and three-field conventional 3D plans. When compared with either AP–PA or three-field plans, IMRT significantly reduced the volume exceeding the threshold dose of the liver and at least one kidney. Target coverage with IMRT was excellent, with 98±1% of the target receiving ≥100% of the dose. Compared with AP–PA and three-field plans, IMRT plans had a greater percentage of target receiving the prescribed dose, but also a greater volume receiving >110% of the dose. IMRT in the treatment of gastric malignancies reduces the mean and above threshold doses to critical normal tissues. In an initial cohort of seven patients, a dose of 50.4 Gy delivered by IMRT was well tolerated and safe.
Soyfer et al [12] investigated whether a better radiation distribution would be achievable with 3D conformal approaches than with the classic AP–PA opposed fields. The clinical target volume (CTV) was adequately covered in all three plans. In the greater-dose kidney group, all the differences were statistically significant with a benefit for the 3D plan. In the lower-dose kidney group, the differences in the mean radiation dose did not reach the level of statistical significance, whereas the differences in the kidney volume receiving a dose >20 Gy showed a statistically significant benefit for the 3D plan. The authors concluded that non-coplanar 3D-based conformal planning for post-operative radiotherapy for gastric cancer provided the best results regarding kidney and spinal cord exposure with adequate CTV coverage. This technique was readily implemented in clinical practice.
El-Hossiny et al [13] compared the multiple field conformal technique with the AP–PA technique with respect to target volume coverage and dose to normal tissues. The 3D-CRT technique consisted of a monoisocentric arrangement using four to six radiation fields. For each patient, a second radiotherapy treatment plan was carried out using AP–PA fields. Comparing different DVHs, it was found that the PTV was adequately covered in both (3D and 2D) plans, while the left kidney and spinal cord demonstrated lower radiation doses on using the conformal technique. The liver doses were higher in the 3D technique but still well below liver tolerance. The authors concluded that for both 3D-CRT and AP–PA conventional techniques, doses are within the range of normal tissues tolerance. Regarding the left kidney and spinal cord, the 3D-CRT is superior to the AP–PA conventional technique but with higher doses to the liver with 3D-CRT than with the AP–PA conventional techniques.
Analysis of the selected studies
Patients population
Five planning studies, each of which analysed 7–19 cases (median 15), were selected [9–13]. The location of the disease (cardia, body or antrum) was specified in two papers only [10,13]. The stage of the disease was not mentioned in one paper [12]; in another study, patients with T3–T4 gastric cancer were included [9], whereas in the other three studies, patients with Stages II–IV disease were enrolled [10,11,13]. The type of surgery was not specified in three studies [9,10,12] and the other two studies included both patients who underwent total and subtotal gastrectomy [11,13]. No study reported the volume of the target (Table 1).
Table 1.
Studies characteristics
| References | First author | Patients (n) | Tumour site | Stage | Type of surgery | PTV (ml) |
| 9 | Wieland et al | 15 | NR | T3/T4/Nt | NR | NR |
| 10 | Leong et al | 15 | 7: antrum | 2: Stage II | NR | NR |
| 6: body | 9: Stage III A | |||||
| 2: cardia | 2: Stage III B | |||||
| 2: Stage IV | ||||||
| 11 | Milano et al | 7 | NR | 5: Stage III A | 4: subtotal gastrectomy | NR |
| 1: Stage III B | 2: total gastrectomy | |||||
| 1: treated pre-operatively | ||||||
| 12 | Soyfer et al | 19 | NR | NR | NR | NR |
| 13 | El-Hossiny et al | 17 | 4: cardia | 5: Stage II | 5: subtotal gastrectomy | NR |
| 5: body | 9: Stage III | 12: total gastrectomy | ||||
| 8: antrum | 3: Stage IV |
NR, not reported; PTV, planning target volume.
Evaluated techniques
All studies tested a conventional technique with AP–PA fields. However, there was some variability. As an example, in one report, the AP–PA treatment was defined as based on “classic fields” [12], in another one conformed AP–PA fields were used [11] and in other two studies, the AP–PA fields were defined as “closely contoured” [10,13]. In one study, it was specified that the AP and PA fields were equally weighted [9], whereas in another study, the AP field was more heavily weighted [10].
The AP–PA technique, which was generically defined as “conventional”, was compared with a 3D conformal one. Many differences were also observed among the studies for the 3D technique. As an example, in one study, the three-field technique was used (AP–PA fields plus a left lateral one) [11], in a second study, three or four fields were used [9], in a third one, non-coplanar fields were used [12], and in the other two studies, a “split field” technique with a unique isocentre and up to six fields were applied [10,13]. In actual fact, it is not completely clear whether the two opposed AP–PA beams were defined by using a 2D or a 3D technique in at least three of the studies [10,11,13]. Furthermore, in one report, it was explicitly declared that in some cases, the so-called opposed beams were in point of fact slightly angled [9]. In two studies, it was also explicitly stated that the angle of the beams and their weight were optimised on individual patients and that the use of wedge filters was allowed [10,13]. In three studies, beams of different energy (6–18 MV) were used [10,11,13]. In another study, 23 MV beams were used [9], and in another study, the energy of the beams was not reported [12] (Table 2).
Table 2.
Study comparison
| References | Authors | Comparison | Notes |
| 9 | Wieland et al | AP–PA (equal beam weighting) vs 3D conformal three or four beams | AP–PA by 2D or 3D technique? AP–PA fields (also for box) in some cases angled minimally; 23 MV photons |
| 10 | Leong et al | Closely (contoured slightly anteriorly weighted) vs 3D conformal (split-field, mono-isocentric arrangement using six radiation fields) | AP–PA by 2D or 3D technique? Field weighting, beam angles and wedges individually optimised for each patient segmented fields, variable weighting of fields and wedges were used to optimise the plan; 6–18 photons |
| 11 | Milano et al | Conformal AP–PA vs conformal three-field technique (AP–PA+left lateral field) | 6–18 photons; all fields were coplanar |
| 12 | Soyfer et al | AP–PA (“classic fields”) vs four-field box vs non-coplanar 3D-conformal planning (experimental plan) | AP–PA by 2D or 3D technique? Experimental plan: one right lateral field, one left lateral field, one anterior craniocaudal oblique field and one anterior caudal-cranial oblique field; beam energy not reported |
| 13 | El-Hossiny et al | “Conventional” closely contoured AP–PA technique vs 3D conformal (monoisocentric arrangement using four to six radiation fields) | Field weightings, beam angles and wedges were optimised individually; 6–18 MV |
2D, two-dimensional; 3D, three-dimensional; AP–PA, anteroposterior–posteroanterior.
Target definition
The CTV was defined based on previous publications in two studies (Macdonald et al [4] in one case [9] and Smalley et al [14] in the other one [12]). In two reports, it was drawn based on the location and the locoregional spread of the tumour [10,13] as well as the type of surgery in one of these two studies [10]. The margin from the CTV to the PTV was not reported in one study [9]; it was an isotropic margin of 1 cm in all directions in three reports [10,11,13], whereas it was an anisotropic margin of 1 cm radially and 2 cm cranio-caudally in another report [12] (Table 3).
Table 3.
Target definition
| References | Authors | CTV definition | CTV to PTV margin |
| 9 | Wieland et al | Target volume defined in accordance with the Macdonald protocol | Target volume defined as PTV |
| 10 | Leong et al | Fields individualised depending upon extent and location of the primary tumour and involved lymph nodes and type of performed surgery | 1 cm |
| 11 | Milano et al | Original tumour volume operative bed and the draining lymphatics at risk | 1 cm |
| 12 | Soyfer et al | Based on Smalley et al [14] recommendations; upper one-third: subpyloric nodes included only in cases with extensive nodal involvement; middle third: according to pre-operative gastric silhouette to include peri-gastric nodes; lower third: splenic nodes excluded in the absence of extensive pathological involvement | 2 cm in cranio-caudal and 1 cm in the AP–PA and lateral axes |
| 13 | El-Hossiny et al | Fields individualised depending upon the extent and location of the primary tumour and involved lymphnodes | 1 cm |
CTV, clinical target volume; PTV, planning target volume.
Radiotherapy planning and dose–volume constraints
The dose prescription to the PTV was variable. In particular, two studies did not report any dose constraint for the PTV [12,13]. In one study, it was stated that at least 98% of the PTV should receive 95% of the prescribed dose (D95%>98%) [11]. In another study, it was required that the median dose to the PTV was equal to the prescribed dose [9]. In only one study, the dose was prescribed according to the ICRU50 recommendations [15], requiring that the dose to the PTV should range between +7% and −5% of the prescribed dose [10]. No study reported the conformity index and the homogeneity index. The prescribed dose was 45 Gy (1.8 Gy per fraction) in four studies [9,10,12,13] and 50.4 Gy (1.8 Gy per fraction) in the fifth [11] (Table 4). No study reported any dose constraint for the lungs and the small bowel, and four of five studies did not define any dose constraint for the spine, kidneys, liver and heart [9–11,13]. In only one study, dose constraints were given for the spine (the maximum dose should be <45 Gy), the kidneys (at least one-third of one kidney should receive <20 Gy), the liver (the volume of the liver receiving at least 30 Gy should be <60%) and the heart (the length of the cardiac silhouette receiving at least 40 Gy should be <30%) [12] (Table 5).
Table 4.
Planning
| References | Authors | PTV constraints | Conformity Index evaluation | Homogeneity Index evaluation (definition) | Prescribed dose |
| 9 | Wieland et al | Prescription dose=median dose to target (at % of maximum dose) | NE | NE | 45 Gy, 1.8 Gy per fraction |
| 10 | Leong et al | Dose in the PTV was kept within +7% and −5% of the prescribed dose | NE | NE | 45 Gy, 1.8 Gy per fraction |
| 11 | Milano et al | D95%>98% | NE | NE | 50.4 Gy, 1.8 Gy per fraction |
| 12 | Soyfer et al | ND | NE | NE | 45 Gy, 1.8 Gy per fraction |
| 13 | El-Hossiny et al | ND | NE | NE | 45 Gy, 1.8 Gy per fraction |
ND, not defined; NE, not evaluated; PTV, planning target volume.
Table 5.
Dose–volume constraints
| Reference | Authors | Spinal cord | Kidneys | Liver | Lung | Small bowel | Heart | Notes |
| 9 | Wieland et al | ND | ND | ND | NE | NE | NE | Constraints defined only for IMRT |
| 10 | Leong et al | ND | ND | ND | NE | NE | NE | |
| 11 | Milano et al | ND | ND | ND | NE | NE | NE | PTV constraints defined only for IMRT |
| 12 | Soyfer et al | Dmax<45 Gy | At least two-third of one kidney exposed to a dose <20 Gy | V30Gy<60% | NE | NE (“because total dose is tolerable”) | “Cardiac silhouette” exposed to 40 Gy≤30% | |
| 13 | El-Hossiny et al | ND | ND | ND | NE | NE | NE |
IMRT, intensity-modulated radiotherapy; ND, dose–volume constraints not defined; NE, organ at risk not evaluated; PTV, planning target volume.
Planning results: PTV
Results about PTV irradiation were reported in a very inhomogeneous manner among the studies. Only two studies reported the same parameter, the maximum dose to PTV [9,11]. The following parameters were also considered: V110%, V99%, V98%, V95%, V90%, V50%, mean dose, V55.4Gy and V50.4Gy. In only one study, an analysis of the statistical significance of differences was performed [11]. In most cases, only a little difference was observed between conventional and conformal techniques, particularly in terms of V110%, V99%, V98%, V95%, V90%, V50%, mean dose, V55.4Gy and V50.4Gy. The conformal technique yielded an advantage of >20% in terms of D98% in one study [10] and of >10% in terms of V50.4Gy in another one [11]. In one report, it was said only that the coverage of the CTV by the isodose of 95% was “satisfactory” [12] (Table 6). An optimal description of target coverage would require the reporting of the minimal dose (Dmin) to the target. However, no study reported the results based on this end point.
Table 6.
Planning results: planning target volume
| Reference | Authors | Planning target volume | |||
| Parameter | AP–PA | 3D | p-value | ||
| 9 | Wieland et al | Dmax (%) | 107.0 | 105.8 | NE |
| V110% | 0.0 | 0.0 | NE | ||
| D90% | 44.0 Gy | 43.4 Gy | NE | ||
| D95% | 43.4 Gy | 42.6 Gy | NE | ||
| 10 | Leong et al | D99% | 93 | 95 | NE |
| D98% | 71 | 95 | NE | ||
| 11 | Milano et al | Dmax | 109.0±3.0% | 108.0±3.0% | NS |
| Dmean | 102.0±0.7% | 103.5±1.6% | 0.044 | ||
| V55.4Gy | 1.3±2.4 | 0.7±1.6 | NS | ||
| V50.4Gy | 84.1±11.1 | 94.9±4.0 | 0.022 | ||
| 12 | Soyfer et al | “Satisfactory coverage by the 95% isodose of the CTV with all three plans” | |||
| 13 | El-Hossiny et al | D50% | 40.0 Gy | 41.5 Gy | NE |
3D, three-dimensional; AP–PA, anteroposterior–posteroanterior; NE, not evaluated; NS, not significant.
Planning results: organs at risk
Spinal cord
To evaluate the irradiation of the spinal cord, the maximum dose was used in three studies [9,12,13], and the V45Gy was used in the other two [10,11]. One study also reported the mean dose [13]. All studies showed a benefit in favour of the 3D technique. Two studies also reported the statistical significance of the differences [11,12]. In particular, all studies reported maximum dose values of >45 Gy with the AP–PA technique and of <45 Gy with the 3D technique (Table 7).
Table 7.
Planning results: organs at risk
| Reference | Authors | Spinal cord | Liver | Right kidney | Left kidney | ||||
| 9 | Wieland et al | AP–PA | 3D | AP–PA | 3D | AP–PA | 3D | AP–PA | 3D |
| Dmax, 47.3±0.9 Gy | 30.5±7.5 Gy | Dmod, 3.7±2.8 Gy | 23.4±5.0 Gy | Dmod, 4.7±4.8 Gy | 8.3±6.3 Gy | Dmod, 31.2 Gy (±17.6) | 19.5 Gy (±7.6) | ||
| D30%, 16.4±14.1 Gy | 26.4±5.2 Gy | D30% 9.5±9.6 Gy | 14.4±8.5 Gy | D30%, 39.0 Gy (±14.1) | 26.2 Gy (±5.6) | ||||
| D60%, 2.8±1.2 Gy | 21.1±4.6 Gy | D60% 3.8±3.5 Gy | 6.0±4.3 Gy | D60%, 5.9 Gy (±17.4) | 16.3 Gy (±8.4) | ||||
| 10 | Leong et al | AP–PA | 3D | AP–PA | 3D | AP–PA | 3D | AP–PA | 3D |
| V45Gy, 37% | <1% | D33% (M), 10 Gy | 31 Gy | D33% (M), 35 Gy | 18 Gy | D33% (M), 40 Gy | 18 Gy | ||
| D67% (M), 2 Gy | 10 Gy | D67% (M), 4 Gy | 6 Gy | D67% (M), 5 Gy | 5 Gy | ||||
| Dmean, 14 Gy | 22 Gy | ||||||||
| 11 | Milano et al | AP–PA | 3D | AP–PA | 3D | AP–PA | 3D | AP–PA | 3D |
| V45Gy, 55.0±22.3 | 4.1±7.3 | Dmean, 41.6±9.5% | 67.9±17.8% | Dmean, 24.8±14.9% | 26.7±13.0% | Dmean, 62.7±30.2% | 47.3±24.2% | ||
| p=0.00033 | p=0.0065 | p=NS | p=NS | ||||||
| V30Gy, 33.7±12.6 | 63.6±28.5 | V20Gy, 20.1±18.0% | 20.9±16.6% | V20Gy, 67.6±34.7% | 52.0±31.9% | ||||
| p=0.0062 | p=NS | p=NS | |||||||
| 12 | Soyfer et al | AP–PA | BOX Exp | AP–PA | BOX Exp | AP–PA | BOX Exp | AP–PA | BOX Exp |
| Dmax, 51.1 Gy | 39.0 Gy 37.9 Gy | Dmean, 15.5 Gy | 27.2 Gy 24.3 Gy | High dose kidney: Dmean, 24.6 Gy | 20.6 Gy 19.2 Gy | Low dose kidney: Dmean, 15.6 Gy | 13.8 Gy 12.6 Gy | ||
| (AP–PA vs Exp: p=0.01) | (AP–PA vs Exp: p=0.06) | ||||||||
| V20Gy, 52.5% | 55.2% 40.1% | V20Gy, 30.8 Gy | 30.6 Gy 20.2 Gy | ||||||
| (AP–PA vs Exp: p=0.019) | (AP–PA vs Exp: p=0.013) | (AP–PA vs Exp: p=0.0015) | (AP–PA vs Exp: p=0.004) | ||||||
| 13 | El-Hossiny et al | AP–PA | 3D | AP–PA | 3D | AP–PA | 3D | AP–PA | 3D |
| Dmax (A), 48 Gy | 44 Gy | Dmean (A), 13 Gy | 20 Gy | Dmean (A), 17 Gy | 13 Gy | Dmean (A), 26 Gy | 17 Gy | ||
| Dmean (A), 22 Gy | 15 Gy | V30Gy (A), 21% | 30% | V20Gy (A) 38% | 32% | V20Gy (A) 62% | 34% | ||
A, average; AP–PA, anteroposterior–posteroanterior; Dmean, mean dose; Dmed, median dose; Exp, experimental technique; M, mean.
Liver
To estimate the irradiation of the liver, the mean dose was used in four studies [10–13] and the median dose in the other one [9]. In addition, two papers reported the V30Gy [11,13] and two others reported the following parameters: D30%, D33%, D60% and D67% [9,10]. All studies reported better outcomes with the AP–PA technique than with the conformal one, and two of these studies showed the statistical significance of such comparison [11,12] (Table 7).
Kidneys
To evaluate the irradiation of the kidneys, the mean dose was used in three studies [11–13] and the median dose in another one [9]. Furthermore, three papers also considered the V20Gy [11–13], and other two trials reported the following parameters: D30%, D33% and D60%, D67% [9,10]. The right kidney was better spared from irradiation (lower median dose, D30% and D60%) with the AP–PA technique in one study [9]. Another study observed lower D33% values with the conformal technique and lower D67% values with the AP–PA technique [10]. A third trial showed that the AP–PA technique resulted in a lower mean dose, whereas V20Gy values were substantially comparable between the two techniques [11]. Another study reported a lower mean dose by using multiple fields and a lower V20Gy by using no-coplanar fields; both differences were statistically significant [12]. In the last trial, the conformal technique resulted in a lower mean dose and V20Gy [13] (Table 7).
The left kidney received a lower median dose and D30% but higher D60% with the conformal technique in one study [9]. Another trial showed that the conformal technique provided better results in terms of D33%, whereas the results were substantially comparable between the two techniques in terms of D67% [10]. A third study showed a benefit for the conformal technique both for the mean dose and for the V20Gy value [11]. In a fourth study, the conformal technique with both non-coplanar and box field arrangements provided a lower mean dose, whereas the V20Gy value was lower with non-coplanar fields and substantially comparable between the AP–PA and the box field techniques [12]. In the fifth trial, the conformal technique provided better organ sparing in terms of both the mean dose and the V20Gy value [13] (Table 7).
DISCUSSION
Theoretically, 3D-CRT allows for a better target coverage and OAR sparing than 2D radiotherapy, thus it is considered as the standard technique for the post-operative treatment of gastric cancer. With the aim of quantifying such an advantage, a systematic review of the literature was performed. Quite surprisingly, only little evidence was found to be available on this topic. In particular, only five studies were retrieved from within the last decade [9–13]. Furthermore, it was observed that these studies are biased by several important methodological limits.
In most studies, it is not completely clear whether the comparisons were made between 2D and 3D techniques rather than two opposed AP–PA and multiple field techniques. Moreover, it is well known that in gastric cancer, CTV definition depends on the location of the tumour, the type of surgery and the stage of the disease. Although results of a planning study may vary according to the characteristics of the target, such important information is lacking in the majority of the studies and, whenever present, contouring guidelines vary among studies. In addition the margin from CTV to PTV was different among studies. The dose prescription also varied and was required to comply with the ICRU50 criteria in only one trial [10]. In four of five studies, no indication about dose constraints to OAR was provided [9–11,13]. Furthermore, in one study, the dose prescribed to the target was higher than the standard (50.4 Gy) [11].
In many cases, the end points used for planning comparison were of poor clinical significance. For example, Milano et al [11] reported the values of V55.4Gy and V50.4Gy for the PTV, yet these parameters are rarely used in clinical practice owing to the lower dose, which is generally prescribed (45 Gy). Another end point used to evaluate the target coverage was D50% [13], which has a questionable clinical significance. Furthermore, the values of D50% that were reported (40 and 41.5 Gy) suggest an inadequate coverage of the target with both conventional and conformal techniques [13]. Although the spinal cord has a serial structure, and the maximum dose should be the main parameter to be evaluated, this end point was not considered in two studies [10,11], and the mean dose, which is of poor clinical relevance, was used in one study [13].
No measure was provided of other relevant end points. For instance, it should be noticed that post-operative chemoradiotherapy for gastric cancer is burdened by a high incidence of gastrointestinal side effects. Cardiovascular and pulmonary complications were also observed [4]. However, no studies performed a dosimetric analysis of the impact on bowel, heart and lung irradiation of various techniques.
Different dosimetric end points were used to evaluate target and OAR irradiation in the various trials, so it is impossible to make an overall quantitative assessment (meta-analysis).
Aside from these limitations, conclusions are also not homogeneous. Three of five studies reported a benefit in favour of the conformal technique for target irradiation [10–12], even if such advantage was of minimal entity in most cases. The liver was better spared from irradiation by the traditional technique in all studies. No univocal result was obtained for the right kidney: the traditional technique performed better in two studies [9,11], the conformal technique yielded better results in other two [12,13], whereas in the fifth study, each technique was either better or worse according to the different end points that were considered [10]. The conformal technique allowed for better sparing of the left kidney in four studies [10–13], whereas in the fifth study, each technique was either better or worse according to the end points [9].
Further analyses should be carried out to better quantify the potential benefit of 3D or other modern techniques (IMRT, tomotherapy, volumetric-modulated arc therapy) in the post-operative radiotherapy of gastric cancer. Such analyses should satisfy specific criteria. The dose prescription to the target should be made according to current guidelines; hence, schedules that differ from 45 Gy with 1.8 Gy daily fractionation should not be used. The dose constraints for the target should meet the ICRU62 criteria. In this way, it would be possible to evaluate the planning results for OAR in a homogenous manner. This evaluation should be based on consistent and clinically meaningful end points. These end points, if possible, should refer to the current dose–volume constraints [Quantative Analysis of Normal Tissue Effects in the Clinic (QUANTEC)] [16]. In particular, it would be interesting to know in what percentage of patients the different techniques are able to meet such dose constraints.
The conformal technique is the standard technique in most radiotherapy centres (50.4 Gy) [17]. So it is likely that it will also continue to be the most widely used technique in gastric cancer. Based on the results of our analysis, however, there is no absolute reason to prefer the 3D technique with multiple beams in every case. It may be preferable to choose the technique, in particular the number and arrangement of the fields, based on individual patient characteristics.
Finally, because there is no proof of the superiority of the conformal technique, there is no absolute reason to exclude patients referred to centres equipped with only the 2D technique from the potential benefit of post-operative chemoradiotherapy.
REFERENCES
- 1.Kamangar F, Dawsey SM, Blaser MJ, Perez-Perez GI, Pietinen P, Newschaffer CJ, et al. Opposing risks of gastric cardia and noncardia gastric adenocarcinomas associated with Helicobacter pylori seropositivity. J Natl Cancer Inst 2006;98:1445–52 10.1093/jnci/djj393 [DOI] [PubMed] [Google Scholar]
- 2.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer statistics. CA Cancer J Clin 2009;59:225–49 10.3322/caac.20006 [DOI] [PubMed] [Google Scholar]
- 3.Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde CJ, Nicolson M, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med 2006;355:11–20 [DOI] [PubMed] [Google Scholar]
- 4.Macdonald JS, Smalley SR, Benedetti J, Hundahl SA, Estes NC, Stemmermann GN, et al. Chemoradiiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or gastroesophageal junction. N Engl J Med 2001;345:725–30 10.1056/NEJMoa010187 [DOI] [PubMed] [Google Scholar]
- 5.Sakuramoto S, Sasako M, Yamaguchi T, Kinoshita T, Fujii M, Nashimoto A, et al. Adjuvant chemotherapy for gastric cancer with S-1, an oral fluoropyrimidine. N Engl J Med. 2007;357:1810–20 10.1056/NEJMoa072252 [DOI] [PubMed] [Google Scholar]
- 6.Gunderson LL, Sosin H. Adenocarcinoma of the stomach: areas of failure in a re-operation series (second or symptomatic look) clinicopathologic correlation and implications for adjuvant therapy. Int J Radiat Oncol Biol Phys 1982;8:1–11 [DOI] [PubMed] [Google Scholar]
- 7.Gunderson LL. Gastric cancer—patterns of relapse after surgical resection. Semin Radiat Oncol 2002;12:150–61 10.1053/srao.2002.30817 [DOI] [PubMed] [Google Scholar]
- 8.Landry J, Tepper JE, Wood WC, Moulton EO, Koerner F, Sullinger J. Patterns of failure following curative resection of gastric carcinoma. Int J Radiat Oncol Biol Phys 1990;19:1357–62 [DOI] [PubMed] [Google Scholar]
- 9.Wieland P, Dobler B, Mai S, Hermann B, Tiefenbacher U, Steil V, et al. IMRT for postoperative treatment of gastric cancer: covering large target volumes in the upper abdomen: a comparison of a step-and-shoot and an arc therapy approach. Int J Radiat Oncol Biol Phys 2004;59:1236–44 10.1016/j.ijrobp.2004.02.051 [DOI] [PubMed] [Google Scholar]
- 10.Leong T, Willis D, Joon DL, Condron S, Hui A, Ngan SY. 3D conformal radiotherapy for gastric cancer—results of a comparative planning study. Radiother Oncol 2005;74:301–6 10.1016/j.radonc.2005.01.006 [DOI] [PubMed] [Google Scholar]
- 11.Milano MT, Garofalo MC, Chmura SJ, Farrey K, Rash C, Heimann R, et al. Intensity-modulated radiation therapy in the treatment of gastric cancer: early clinical outcome and dosimetric comparison with conventional techniques. Br J Radiol 2006;79:497–503 10.1259/bjr/43441736 [DOI] [PubMed] [Google Scholar]
- 12.Soyfer V, Corn BW, Melamud A, Alani S, Tempelhof H, Agai R, et al. Three-dimensional non-coplanar conformal radiotherapy yields better results than traditional beam arrangements for adjuvant treatment of gastric cancer. Int J Radiat Oncol Biol Phys 2007;69:364–9 [DOI] [PubMed] [Google Scholar]
- 13.El-Hossiny HA, Diab NA, El-Taher MM. A comparative dosimetric study of adjuvant 3D conformal radiotherapy for operable stomach cancer versus AP-PA conventional radiotherapy in NCI-Cairo. J Egypt Natl Canc Inst 2009;21:197–202 [PubMed] [Google Scholar]
- 14.Smalley SR, Gunderson L, Tepper J, Martenson JA, Jr, Minsky B, Willett C, et al. Gastric surgical adjuvant radiotherapy consensus report: rationale and treatment implementation. Int J Radiat Oncol Biol Phys. 2002;52:283–93 [DOI] [PubMed] [Google Scholar]
- 15.International Commission on Radiation Units and Measurements. ICRU-50: Prescribing, recording and reporting proton beam theraphy (Report 50). Bethesda, MD: ICRU; 1993 [Google Scholar]
- 16.Marks LB, Yorke ED, Jackson A, Ten Haken RK, Constine LS, Eisbruch A, et al. Use of normal tissue complication probability models in the clinic. Int J Radiat Oncol Biol Phys 2010;76:S10–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tepper JE, Gunderson LL. Radiation treatment parameters in the adjuvant postoperative therapy of gastric cancer. Semin Radiat Oncol 2002;12:187–95 10.1053/srao.2002.30827 [DOI] [PubMed] [Google Scholar]