Abstract
Objective:
To determine whether the justification of CT examinations performed on young patients can be improved by various interventions and whether these have an effect on the total number of CTs performed.
Methods:
Specific interventions—education, guideline implementation and increased MRI capacity—were introduced at the Oulu University Hospital, Oulu, Finland, following a previous study demonstrating unjustified use of CT examination in young patients. In the present study, the justification of 177 CT examinations of the lumbar and cervical spine, head, abdomen, nasal sinuses and trauma performed on patients aged under 35 years in 2009 was analysed retrospectively by looking at requests and corresponding patient files. The indications of the examinations were compared with the referral guidelines recommended by the European Commission. Results from our previously published similar study carried out before the interventions were used as a reference.
Results:
The proportion of justified CT examinations increased from 71% (141/200) in 2005 to 87% (154/177) in 2009 (p<0.001), and in the lumbar spine group from 23% (7/30) to 81% (22/27) (p<0.001). In the case of most of the unjustified examinations, MRI could have been performed instead. The total number of CT examinations carried out on young patients decreased by 7% (p=0.012) and in the lumbar spine group by 79% (p<0.001).
Conclusion:
The implemented interventions decreased the number of CT examinations performed on young patients, and the justification of the examinations improved significantly.
Advances in knowledge:
This study demonstrates that it is possible to reduce the number of various CT examinations and to improve their justification in young patients by regular education, guideline implementation and increased MRI capacity.
By definition, a medical exposure is justified when the benefit to the patient is greater than the expected harm. In diagnostic imaging, justification inevitably includes consideration of any and all of the alternative procedures possibly available that require no or less exposure to ionising radiation [1,2]. Authoritative sources suspect that a considerable proportion of radiological examinations are inappropriate [3]. It is known that knowledge of radiation dose and related risks is poor among both physicians and radiologists, and risks are often underestimated [4–6]. The International Commission on Radiological Protection has emphasised that education, training and practice play a crucial role in improving the professionalism of justification [3].
CT examinations are an essential part of current diagnostic radiology practice. The radiation exposure and dose from CT for both individuals and population are among the highest in diagnostic radiology. Although the risk from ionising radiation caused by a CT examination to a single individual is small, the concern is related to the current rapid increase in CT use [7,8]. In 2008, CT represented approximately 10% of all ionising radiation-based imaging globally, but delivered approximately 43% of the total collective dose [9]. In many European countries, CT-induced dose accounts for the largest proportion of the collective effective dose: approximately 68% in the UK, 59% in Norway, 58% in Finland and 60% in Germany [10–13]. The risk of potential radiation damage is higher in patients aged approximately 35 years or younger, owing to longer life expectancy and a possibly increased number of repeat examinations [14]. Developing organs are also more sensitive to radiation than those that are fully mature [15–17].
We previously published a study demonstrating unjustified use of CT examinations in young patients at the Oulu University Hospital, Oulu, Finland, where 77% of CT examinations of the lumbar spine, 37% of the abdomen and 36% of the head were unjustified in 2005 [18]. After these results, we introduced various interventions involving provision of education, distribution of guidelines and increased MRI capacity. This study is therefore a re-audit, closing the audit loop [19]. Studies demonstrating the effects of different interventions on justification are sparse. The aim of the present study is to determine whether the justification of various CT examinations carried out on young patients has improved 4 years after the primary survey and whether the interventions applied have had an effect on the total number of CT examinations performed.
MATERIALS AND METHODS
The institutional review board at Oulu University approved this retrospective re-audit study. In 2009, a total of 148 666 examinations were performed in the Department of Diagnostic Radiology of Oulu University Hospital, Oulu, Finland (population base, 750 000). 19 046 (13%) of the examinations were carried out using CT. 2197 (12%) of the CT examinations were carried out on patients aged <35 years. In 2005, the corresponding number was 2367 (14%). The numbers of the different CT examinations performed on patients aged <35 years and on all age groups in 2005 and 2009 are shown in Table 1.
Table 1.
The total number (n) and changes in numbers of different CT examinations performed on patients aged <35 years and on all age groups in 2005 and in 2009 at the Oulu University Hospital, Oulu, Finland
| CT examination | <35 years | All age groups | |||||
| 2005 | 2009 | Change from 2005 to 2009 | 2005 | 2009 | Change from 2005 to 2009 | ||
| n | n | % | pa | n | n | % | |
| Head | 1063 | 843 | −21 | <0.001 | 8227 | 8469 | +3 |
| Thorax | 241 | 247 | +2 | 0.786 | 1809 | 2032 | +12 |
| Lumbar spine | 130 | 27 | −79 | <0.001 | 1250 | 316 | −75 |
| Abdomen or upper abdomen | 123 | 143 | +16 | 0.220 | 1658 | 2201 | +33 |
| Trauma | 117 | 126 | +8 | 0.564 | 221 | 251 | +14 |
| Cervical spine | 110 | 57 | −48 | <0.001 | 362 | 194 | −46 |
| Nasal sinuses | 100 | 79 | −21 | 0.117 | 369 | 265 | −28 |
| Body (thorax and abdomen) | 80 | 102 | +28 | 0.103 | 921 | 1645 | +44 |
| Other | 403 | 573 | +42 | <0.001 | 2158 | 3673 | +70 |
| Total | 2367 | 2197 | −7 | 0.012 | 16975 | 19046 | +12 |
χ2 goodness of fit test.
Interventions
As a consequence of our previous study, which revealed inadequate justification, we sought to change our practice and adopted various interventions. These interventions were introduced in 2006, and education was provided from 2006 to 2009.
We provided regular education on radiation protection for the Radiology Department staff, other personnel working with ionising radiation in our area and the referring practitioners in our hospital. Personnel in other hospitals in northern Finland were also reached through video connection. In 2006, four different 3-h lectures were implemented. The sessions were repeated; hence, altogether, eight sessions were provided annually. The education consisted of the risks and doses of radiation, the process of justification and legislation on radiation protection. It also focused on indications and interpretation of different radiological examinations and on special issues concerning the work of radiographers, such as projections and dose management of radiological examinations. Additionally, specific topics, e.g. orthopaedic, abdominal and paediatric imaging, were highlighted in each session, and the topics varied from year to year. The lectures were presented by radiologists, radiographers and physicists. Handout summaries were provided to participants. Attendance was voluntary, but the sessions were also part of official education on radiation protection, which is mandatory in Finland for both personnel working with ionising radiation and referring practitioners.
We also provided two-sided laminated info pocket cards for the referring practitioners in the Oulu area and people working with radiation in our hospital (Figure 1). These cards were handed out to medical students annually. The cards were made in 2006 and updated in 2008. These contain information on radiation and justification and radiation doses of the most frequently used X-ray, CT and isotope examinations, and the doses were compared with those of thorax posteroanterior X-ray and natural background radiation.
Figure 1.
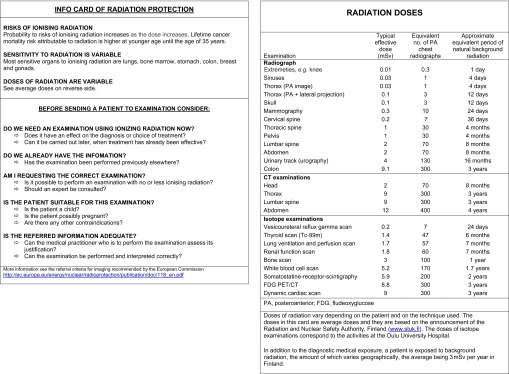
Two-sided info pocket card (updated version from 2008, translated into English).
The referral criteria for imaging recommended by the European Commission [20], and also accepted in Finland and translated into Finnish, are available online. The printed version was distributed to different areas of the Department of Diagnostic Radiology in 2006.
In addition, the following institutional recommendations were adopted to rationalise the use of CT by the referring practitioners and radiologists at our hospital: (1) MRI is the primary examination of the head. CT examination is indicated only in acute cases. (2) MRI is the preferred primary examination of the lumbar spine in young patients (except in trauma). (3) Clinicians are recommended to consult a radiologist before requesting an abdominal CT for a young patient. These recommendations were distributed by e-mail to the Radiology Department staff and the referring practitioners, after which they continued to be available on the hospital intranet.
Because most of the unjustified examinations revealed in the previous study could have been performed using MRI instead, the capacity of MRI was increased. In 2005, we had two 1.5-T and one 0.23-T MRI systems, and in 2009, we had an additional 1.5-T system in use.
Analysis
The analysis of this study was similar to that of the previous one [18]. The retrospective analysis for due justification was performed on patients aged <35 years for the CT of the lumbar spine, head, abdomen or upper abdomen, nasal sinuses, cervical spine and trauma. Trauma CT examination included CT of the head, neck, thorax, abdomen and pelvis. CT of the thorax, lungs or body (including thorax and abdomen) were excluded from the study because there is no good alternative imaging modality for thorax CT examination for most of the indications, and the number of thorax or mediastinal MRI examinations is generally rather low. The examinations included in this study were extracted from the electronic patient files of our hospital consecutively from the beginning of 2009. The number of analysed examinations was 30 in all categories except for lumbar spine CT; only 27 examinations of the lumbar spine were performed on that age group. We ended up having a similar number of examinations per category as in the previous study (except that the category of head CTs included 50 examinations in the 2005 study). The study therefore included 177 examinations. Of the 177 patients, 107 were males and 70 were females. The patients were aged between 5 and 34 years, and their average age was 23.7 years.
Patient files, clinicians' referrals and indications of the examinations were analysed by two radiologists (one specialist with 20 years of experience and one senior resident). Using that information and the referral criteria for imaging recommended by the European Commission [20], it was decided whether the examinations had been justified, and if not, whether there had been other more justifiable imaging modalities available.
In the evaluation, the following main categories were used:
Lumbar spine: CT is justified in trauma and control of fixation of the lumbar spine.
Head: CT is justified in trauma or in some other acute cases (see Results).
Abdomen or upper abdomen: the cases had to be considered case by case because they were so variable.
Nasal sinuses: each patient expected to have functional endoscopic sinus surgery should have CT of the sinuses.
Cervical spine: CT may be justified in the case of trauma.
Trauma CT is indicated in high-energy traumas (see Results).
Cases not falling into these categories were analysed individually using the same principles as in the previous study. After that, radiologists trained in neuroradiology or abdominal radiology went through all the data collected and evaluated justification. If necessary, consensus of the first and second reviewers was used. The results of the survey were compared with the results of the previous study [18].
Statistics
The difference between the total number of CTs and the number of justified CTs in 2005 and 2009 were calculated separately. Proportional changes from 2005 to 2009 of the total number of CTs were calculated, and the difference between the total number of CTs in 2005 and 2009 was tested using the χ2 goodness of fit test. The proportions of justified CTs in 2005 and 2009 were compared using Pearson's χ2 test or Fisher's test.
RESULTS
The number of radiological examinations performed in the Oulu University Hospital remained nearly constant from 2005 to 2009 (148 988 and 148 666, respectively). The total number of CT examinations increased by 12% (16 975 and 19 046, respectively) (Table 1). The number of CT examinations performed on patients aged <35 years decreased by 7% (p=0.012). In the group of patients aged <35 years, the number of lumbar CTs decreased by 79% (p<0.001), cervical spine CTs by 48% (p<0.001) and head CTs by 21% (p<0.001). The changes in the numbers of CT examinations concerning patients aged <35 years and all age groups are shown in Table 1. Table 2 reveals the total number and changes in numbers of different MRI examinations performed on these two groups in 2005 and in 2009 in the hospital.
Table 2.
The total number (n) and changes in numbers of different MRI examinations performed on patients under 35 years of age and on all age groups in 2005 and in 2009 at the Oulu University Hospital
| CT examination | Under 35 years | All age groups | ||||
| 2005 | 2009 | Change from 2005 to 2009 | 2005 | 2009 | Change from 2005 to 2009 | |
| n | n | % | n | n | % | |
| Head | 1023 | 1414 | +38 | 2357 | 2991 | +27 |
| Lumbar spine | 200 | 406 | +103 | 1206 | 1951 | +62 |
| Cervical spine | 90 | 92 | +2 | 642 | 637 | −0.8 |
| Abdomen or upper abdomen | 76 | 174 | +129 | 320 | 692 | +116 |
| Other | 1231 | 1908 | +55 | 4078 | 5387 | +32 |
| Total | 2620 | 3994 | +52 | 8603 | 11658 | +36 |
The number of justified CT examinations carried out on young patients in different categories in 2005 and in 2009 is shown in Table 3. The level of justification improved or remained unchanged in all categories. In 2009, 87% of the 177 analysed examinations were justified compared with 71% in 2005 (p<0.001). The indications of unjustified examinations and the possibility of using other modalities are shown in Table 4.
Table 3.
The number (n) and proportion (%) of justified CT examinations out of the total number of the cases analysed in 2005 and in 2009 (patients aged <35 years) and the difference between the proportions of justified CTs
| CT examination | 2005 | 2009 | Change | p-valuec |
| n (%) | n (%) | % | ||
| Lumbar spinea | 7 (23.3) | 22 (81.5) | +58 | <0.001 |
| Headb | 32 (64.0) | 22 (73.3) | +9 | 0.464 |
| Abdomen or upper abdomen | 19 (63.3) | 24 (80.0) | +17 | 0.252 |
| Nasal sinuses | 24 (80.0) | 27 (90.0) | +10 | 0.472d |
| Cervical spine | 29 (96.7) | 29 (96.7) | 0 | 1.000d |
| Trauma | 30 (100.0) | 30 (100.0) | 0 | — |
| Total | 141 (70.5) | 154 (87.0) | +17 | <0.001 |
Total number of cases is 30 in all categories except the lumbar spine and head.
27 in 2009.
50 in 2005.
Pearson's χ2 test.
Fisher's test.
Table 4.
The numbers (n) and indications of unjustified CT examinations and possibility of using other modalities
| CT examination | Possibility of other modalities to replace CT and indications of unjustified cases | |||
| Unjustified (n) | MRI | Ultrasound | Nothing | |
| Lumbar spine | 5 | 4 | 1 | |
| Symptoms of disk herniation | Leukaemia patient's back pain for a couple of days (at first follow-up) | |||
| Head | 8 | 8 | ||
| Postoperative dizziness | ||||
| Control of trauma patients (ventricular size, haemorrhagia) | ||||
| Control of hydrocephalus or shunt | ||||
| Migraine patient's transient aphasia | ||||
| Prolonged headache/suspicion of tumour | ||||
| Abdomen or upper abdomen | 6 | 5 | 1 | |
| Prolonged pain in lower abdomen | Abdominal pain in a few days | |||
| Lesions of liver or spleen | ||||
| Evaluation of pancreatic pseudocyst | ||||
| Nasal sinuses | 3 | 2 | 1 | |
| Control of sinusitis | Control of incidental finding in head CT without any symptoms | |||
| Cervical spine | 1 | 1 | ||
| Trauma patient with aphasia (head CT was also performed) | ||||
| Trauma | 0 | |||
| Total | 23 | 19 | 1 | 3 |
The proportion of justified lumbar CT examinations increased from 23% to 81% (p<0.001). In 2009, 5 out of the 27 lumbar spine examinations were unjustified. Four of the unjustified examinations should have been performed using MRI instead, and one patient did not need any radiological examination (Table 4). In particular, the number of CTs carried out for disc syndrome (disc herniation) decreased since 2005 (from 16 to 4). The justified cases were imaged owing to trauma or trauma follow-up.
8 out of the 30 head CT examinations were unjustified. All of the unjustified examinations could have been performed with MRI instead. The indications of the 22 justified CTs in this study group were trauma or other acute conditions: suspicion of intracranial bleeding, acute stroke, sinus thrombosis, and elevated intracranial pressure or first seizure.
In the abdominal CT group, the proportion of justified cases increased from 63% to 80%. CT was not justified in six cases. Five of the examinations could have been carried out with MRI instead, and one with ultrasound. The indications of the justified cases were suspicion of acute infection, malignancy, stone in the urinary tract, and intestinal occlusion. The examination was also indicated if there was an ambiguous finding in the ultrasound examination, such as suspicion of kidney trauma, intussusception or malignancy. In all patients with acute infection, ultrasound examination was performed before CT.
In the cervical spine CT group, the justification remained unchanged. Two of the justified CTs had been carried out as a follow-up treatment of osteolytic metastasis; all the others were traumas or control of a fracture. All the trauma CTs were justified, because the traumas were high-energy-associated: motor vehicle accidents, falling from heights or assaults.
26 of 177 examinations (15%) were carried out on children (aged ≤15 years). The proportion of justified CT examinations remained nearly constant from 2005 (21 children) to 2009, being 86% and 92%, respectively. Two cases were unjustified: one follow-up CT of the nasal sinuses performed on a patient without any symptoms and one CT of the cervical spine. The latter was a trauma patient, but with only intracranial neurological symptoms.
DISCUSSION
Over the past two decades, much successful work has been devoted to developing optimisation [21]. However, with respect to justification or its implementation, fewer attempts have been made, and those attempts have not yet been sufficiently successful [3,21]. Optimisation of the radiological examination protocols and dose is extremely important, but careful selection of patients for the examinations and, whenever possible, the use of imaging modalities without ionising radiation, may be equal or more effective tools towards reducing patient dose.
There are only a few other published studies on the justification of CT examinations, and studies on the effect of various interventions on the paradigm shifts of the justification process are sparse [22–26]. In the few earlier studies that viewed indications or request forms for CT examinations, a notable number of CT examinations were unjustified and could have been performed instead using MRI or ultrasound. In our studies, we evaluated all the corresponding patient files in addition to the request forms in order to have the same information as the referring physician had while requesting the examination. According to the Swedish national survey on justification of CT examinations [27], approximately 20% were not justified. The degree of justification varied strongly by organ; 42% of CTs of the spine and 29% of CTs of the abdomen were unjustified. There have been studies assessing the impact of the computerised physician order entry system with decision support on medical imaging services [28–31]. According to some of the reports, the number of CT examinations decreased and the use of guidelines in the test-ordering process improved. To our knowledge, there are no other studies on the impact of more traditional interventions on the level of justification of CT examinations.
Our present study shows that the justification of CT examinations performed on young patients improved or remained unchanged in all categories. The total improvement of justification was statistically significant. Justification remained nearly constant and high in children. It is likely that paediatricians pay more attention to justification and consult radiologists before requesting a CT examination. However, the total number of paediatric examinations was small in both surveys.
Although the total number of CT examinations increased between 2005 and 2009, as it did overall in Finland [32], the number of CTs performed on young patients decreased (Table 1). This was mostly because of a comprehensive decrease in CT examinations of the lumbar and cervical spine (a decrease of 79% and 48%, respectively). In Finland as a whole, the total number of CTs increased by 23% and the number of lumbar CTs decreased by 22% from 2005 to 2008 (national reports are available for these years) [32]. In our hospital, the number of lumbar CTs in all age groups decreased by 67% from 2005 to 2008 (1250 and 414, respectively) and by 75% from 2005 to 2009 (1250 and 316, respectively). Additionally, the number of lumbar MRIs in our hospital increased by 103% in young patients and by 62% in all age groups from 2005 to 2009 (Table 2). It should be noted that, during this time, the MRI capacity in our hospital increased by only 30%. There is a universal trend of increased usage and access to MRI. Exact reports concerning the change of the numbers of different MRIs in Finland during these years are not available. It is also notable that, in our present study, the proportion of justified lumbar CT examinations increased from 23% in 2005 to 81% in 2009. In our view, the trends of the results reflect a clear change in the clinical imaging request paradigm because of the interventions implemented.
The number of CTs of the head carried out on young patients decreased significantly while those of the abdomen increased slightly. There may be several reasons for the latter. First, despite the recommendation, our radiologists were not regularly consulted before abdominal CT was requested for a young patient. Second, routine checkup of the request is performed by a radiologist 1 or 2 days prior or immediately prior to the examination in the context of planning the protocol, but in the case of questionable justification, where the examination could typically be replaced by MRI, there may not be any time slot available for MRI scan. Third, the change may reflect an overall pattern of increased use of all cross-sectional imaging in this patient group. There was also a clear increase in the number of abdominal MRIs from 2005 to 2009 (Table 2). The analysis for justification of abdominal CT is also challenging because of multiple and variable indications. All the subgroups of different CT examinations in the national reports are not comparable to ours but, for example, the number of head CTs and abdominal CTs in all age groups increased more in Finland from 2005 to 2008 than in our hospital from 2005 to 2009 (10% vs 3% in head CTs and 45% vs 33% in abdominal CTs, respectively).
There are several limitations to this study. The major limitation is that this study contains information from one institution only. The patient number selected for the justification evaluation is also low. Inclusion of multiple institutions and a broader patient base might have provided more information. We did not measure the impact of various interventions separately. It is probable that certain interventions directed the referral practice more than others. In addition, we did not record the availability of MRI as a replacement examination, which would have increased the practical value of the study. As a process, the evaluation of justification is also complicated. We realise that, in practice, many different aspects, such as capacity, financing and expertise, may have an effect on the choice of an examination. There have also been national and international changes in imaging, which have occurred over the same time period and may also have influenced the results of this study.
In general, it is probably impossible to reach 100% justification. However, it is still essential to develop justification processes further. Regular updating of referral guidelines and their use and increased patient information concerning issues of radiological examinations could also contribute to increased justification.
In conclusion, we have shown that it is possible to reduce the number of various CT examinations and to improve their justification in young patients by regular education, guideline implementation and increased MRI capacity.
REFERENCES
- 1.International Commission on Radiological Protection. The 2007 recommendations of the ICRP. Annals of the ICRP, volume 37. Amsterdam, Netherlands: Elsevier Ltd; 2007. [Google Scholar]
- 2.European commission Council directive of 30 June 1997 on health protection of individuals against the danger of ionizing radiation in relation to medical exposure, and reapealing directive 84/466/Euratom. Official Journal 1997;180:22–7 [Google Scholar]
- 3.Malone J, Guleria R, Craven C, Horton P, Jarvinen H, Mayo J, et al. Justification of diagnostic medical exposures: some practical issues. Report of an International Atomic Energy Agency Consultation. Br J Radiol 2012;85:523–38 10.1259/bjr/42893576 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shiralkar S, Rennie A, Snow M, Galland RB, Lewis MH, Gower-Thomas K. Doctors' knowledge of radiation exposure: questionnaire study. BMJ 2003;327:371–2 10.1136/bmj.327.7411.371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee CI, Haims AH, Monico EP, Brink JA, Forman HP. Diagnostic CT scans: assessment of patient, physician, and radiologist awareness of radiation dose and possible risks. Radiology 2004;231:393–8 10.1148/radiol.2312030767 [DOI] [PubMed] [Google Scholar]
- 6.Heyer CM, Hansmann J, Peters SA, Lemburg SP. Paediatrician awareness of radiation dose and inherent risks in chest imaging studies–a questionnaire study. Eur J Radiol 2010;76:288–93 10.1016/j.ejrad.2009.06.014 [DOI] [PubMed] [Google Scholar]
- 7.Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation, National Research Council Health risks from exposure to low levels of ionizing radiation: BEIR VII phase 2. Washington, DC: The National Academies Press; 2006 [PubMed] [Google Scholar]
- 8.Hall EJ, Brenner DJ. Cancer risks from diagnostic radiology. Br J Radiol 2008;81:362–78 10.1259/bjr/01948454 [DOI] [PubMed] [Google Scholar]
- 9.United Nations Scientific Committee on the Effects of Atomic Radiation. Sources and effects of ionizing radiation. UNSCEAR 2008 Report to the General Assembly, with Scientific Annexes. 2008;Vol I [cited 9 July 2013]. Available from: http://www.unscear.org/docs/reports/2008/09-86753_Report_2008_Annex_A.pdf. [Google Scholar]
- 10.Hart D, Wall B, Hillier M, Shrimpton P. HPA-CRCE-012-frequency and collective dose for medical and dental X-ray examinations in the UK, 2008. Health Protection Agency Publications; 2010 [Google Scholar]
- 11.Borretzen I, Lysdahl KB, Olerud HM. Diagnostic radiology in Norway trends in examination frequency and collective effective dose. Radiat Prot Dosimetry 2007;124:339–47 [DOI] [PubMed] [Google Scholar]
- 12.Bundesamt fuer Strahlenschutz. Umweltradioaktivität und Strahlenbelastung im Jahr 2010: Unterrichtung durch die Bundesregierung. Bundesministerium Für Umwelt, Naturschutz und Reaktorsicherheit (BMU). 2012 [cited 9 July 2013]. Available from: http://doris.bfs.de/jspui/bitstream/urn:nbn:de:0221-201205118217/3/Parlamentsbericht_2010.pdf.
- 13.Bly R, Järvinen H, Korpela MH, Tenkanen-Rautakoski P, Mäkinen A. Estimated collective effective dose to the population from x-ray and nuclear medicine examinations in Finland. Radiat Prot Dosimetry 2011;147:233–6 10.1093/rpd/ncr334 [DOI] [PubMed] [Google Scholar]
- 14.Brenner DJ, Elliston CD, Hall EJ, Berdon WE. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 2001;176:289–96 10.2214/ajr.176.2.1760289 [DOI] [PubMed] [Google Scholar]
- 15.Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 2012;380:499–505 10.1016/S0140-6736(12)60815-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sodickson A, Baeyens PF, Andriole KP, Prevedello LM, Nawfel RD, Hanson R, et al. Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology 2009;251:175–84 10.1148/radiol.2511081296 [DOI] [PubMed] [Google Scholar]
- 17.Mathews JD, Forsythe AV, Brady Z, Butler MW, Goergen SK, Byrnes GB, et al. Cancer risk in 680 000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ 2013;346:f2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oikarinen H, Meriläinen S, Pääkkö E, Karttunen A, Nieminen MT, Tervonen O. Unjustified CT examinations in young patients. Eur Radiol 2009;19:1161–5 10.1007/s00330-008-1256-7 [DOI] [PubMed] [Google Scholar]
- 19.European Commission. European Commission Guidelines on Clinical Audit for Medical Radiological Practices (Diagnostic Radiology, Nuclear Medicine and Radiotherapy). Radiation protection No 159. 2009. [cited 9 July 2013]. Available from: http://ec.europa.eu/energy/nuclear/radiation_protection/doc/publication/159.pdf. [Google Scholar]
- 20.Radiation protection 118. Referral guidelines for imaging. 2001. [cited 9 July 2013]. Available from: http://ec.europa.eu/energy/nuclear/radioprotection/publication/doc/118_en.pdf. [Google Scholar]
- 21.International Atomic Energy Agency (IAEA) Report of a consultation on justification of patient exposures in medical imaging. Radiat Prot Dosimetry 2009;135:137–44 10.1093/rpd/ncp107 [DOI] [PubMed] [Google Scholar]
- 22.Clarke JC, Cranley K, Kelly BE, Bell K, Smith PH. Provision of MRI can significantly reduce CT collective dose. Br J Radiol 2001;74:926–31 [DOI] [PubMed] [Google Scholar]
- 23.Triantopoulou C, Tsalafoutas I, Maniatis P, Papavdis D, Raios G, Siafas I, et al. Analysis of radiological examination request forms in conjunction with justification of X-ray exposures. Eur J Radiol 2005;53:306–11 10.1016/j.ejrad.2004.02.012 [DOI] [PubMed] [Google Scholar]
- 24.Naik KS, Ness LM, Bowker AMB, Robinson PJA. Is computed tomography of the body overused? An audit of 2068 attendances in a large acute hospital. Br J Radiol 1996;69:126–31 [DOI] [PubMed] [Google Scholar]
- 25.Vassileva J, Rehani MM, Al-Dhuhli H, Al-Naemi HM, Al-Suwaidi JS, Appelgate K, et al. IAEA survey of pediatric CT practice in 40 countries in Asia, Europe, Latin America, and Africa: Part 1, frequency and appropriateness. AJR Am J Roentgenol 2012;198:1021–31 10.2214/AJR.11.7273 [DOI] [PubMed] [Google Scholar]
- 26.Lehnert BE, Bree RL. Analysis of appropriateness of outpatient CT and MRI referred from primary care clinics at an academic medical center: how critical is the need for improved decision support? J Am Coll Radiol 2010;7:192–7 10.1016/j.jacr.2009.11.010 [DOI] [PubMed] [Google Scholar]
- 27.Almén A, Leitz W, Richter S. National survey on justification of CT-examinations in Sweden. Swedish Radiation Safety Authority. 2009. [cited 9 July 2013]. Available from: http://www.stralsakerhetsmyndigheten.se/Global/Publikationer/Rapport/Stralskydd/2009/SSM-Rapport-2009-03.pdf. [Google Scholar]
- 28.Carton M, Auvert B, Guerini H, Boulard JC, Heautot JF, Landre MF, et al. Assessment of radiological referral practice and effect of computer-based guidelines on radiological requests in two emergency departments. Clin Radiol 2002;57:123–8 10.1053/crad.2001.0827 [DOI] [PubMed] [Google Scholar]
- 29.Ip IK, Schneider LI, Hanson R, Marchello D, Hultman P, Viera M, et al. Adoption and meaningful use of computerized physician order entry with an integrated clinical decision support system for radiology: ten-year analysis in an urban teaching hospital. J Am Coll Radiol 2012;9:129–36 10.1016/j.jacr.2011.10.010 [DOI] [PubMed] [Google Scholar]
- 30.Sistrom CL, Dang PA, Weilburg JB, Dreyer KJ, Rosenthal DI, Thrall JH. Effect of computerized order entry with integrated decision support on the growth of outpatient procedure volumes: seven-year time series analysis. Radiology 2009;251:147–55 10.1148/radiol.2511081174 [DOI] [PubMed] [Google Scholar]
- 31.Vartanians VM, Sistrom CL, Weilburg JB, Rosenthal DI, Thrall JH. Increasing the appropriateness of outpatient imaging: effects of a barrier to ordering low-yield examinations. Radiology 2010;255:842–9 10.1148/radiol.10091228 [DOI] [PubMed] [Google Scholar]
- 32.Tenkanen-Rautakoski P. Number of radiological examinations in Finland in 2008. STUK-B 121. 2010. [cited 9 July 2013]. Available from: http://www.stuk.fi/stuk/tiedotteet/2010/fi_FI/news_598/_files/83759228498675316/default/stuk-b121.pdf (in Finnish) [Google Scholar]


