Abstract
While much is known about the negative health implications of insufficient sleep, relatively little is known about risks associated with excessive sleep. However, epidemiological studies have repeatedly found a mortality risk associated with reported habitual long sleep. This paper will summarize and describe the numerous studies demonstrating increased mortality risk associated with long sleep. Although these studies establish a mortality link, they do not sufficiently explain why such a relationship might occur. Possible mechanisms for this relationship will be proposed and described, including (1)sleep fragmentation, (2)fatigue, (3)immune function, (4)photoperiodic abnormalities, (5)lack of challenge, (6)depression, or (7)underlying disease process such as (a)sleep apnea, (b)heart disease, or (c)failing health. Following this, we will take a step back and carefully consider all of the historical and current literature regarding long sleep, to determine whether the scientific evidence supports these proposed mechanisms and ascertain what future research directions may clarify or test these hypotheses regarding the relationship between long sleep and mortality.
Keywords: sleep, long sleep, sleep duration, mortality, depression
WHO ARE THE LONG SLEEPERS?
How much sleep do we need?
Whereas the answer to this question usually involves the determination of the minimum amount of sleep required for the maintenance of health, less attention has been directed to the question of the maximum amount of sleep for optimum health. This may be an equally important issue, given research suggesting that there are negative health consequences of excessive sleep1.
There is growing public awareness of the need for an adequate amount of sleep, and the myriad problems associated with insufficient sleep, which is consistent with a hypothesis that our society is chronically sleep-deprived as a whole. While this hypothesis has been debated throughout the scientific literature2,3, it has been widely reported that average sleep durations have decreased substantially4.
While obtaining too little sleep is certainly problematic, at least some argue that obtaining too much sleep may also be problematic. For example, an analogy between sleep and diet has been made, suggesting that moderation, rather than abundance, may be most healthy5.
A U-shaped relationship between sleep duration and mortality5 is consistent with other relationships between overall poor health and variables such as exercise, diet, and light exposure. As in these relationships, moderation in sleep quantity, rather than extreme low or high amounts, may be best for health. If that is the case, the increased desire for sleep beyond 8 or 8.5 hours may be less indicative of genuine sleep debt and more akin to the desire for more high-calorie foods. Thus, both short and long sleep are related to increased mortality risk; this raises the question: How much sleep do we need?
While the available scientific literature is currently unable to provide a definitive answer to this question, and the available studies have limitations, we will summarize and describe the numerous studies demonstrating increased mortality risk associated with long sleep, defined as a habitual reported sleep length of at least 9 hours and characteristically distinct from clinical hypersomnias. It will also be shown that although these studies establish a mortality link, they do not sufficiently explain why such a relationship might occur. Subsequently, possible mechanisms for this relationship will be proposed and described. Following this, we will take a step back and carefully consider all of the historical and current literature regarding long sleep, to determine whether the scientific evidence supports these proposed mechanisms and ascertain what future research directions may clarify or test these hypotheses regarding the relationship between long sleep and mortality.
Regarding this last goal, while there has been relatively little research on long sleep (as compared to restricted sleep), there is a sufficient body of work to formulate and evaluate hypotheses. First, differences between characterized long and short sleepers will be described, from physiological and psychological domains. Second, a summary of findings related to characteristics of variable-length sleepers (those who alternate between long and short sleep) is provided, so that we may understand what variables may relate to changes in habitual sleep pattern, possibly revealing the functions of long sleep. Also, understanding these factors may help clarify hypothesized mechanisms underlying development of long sleep patterns which might play a role in mortality risk. Finally, results of laboratory sleep extension are reviewed to document possible effects of mild and moderate lengthening of sleep time in controlled settings. These findings provide another perspective of physiological and psychological changes that occur when sleep is lengthened, and the changes may also elucidate mechanisms of the mortality relationship.
LONG SLEEP AND INCREASED MORTALITY
Increased mortality associated with long sleep
Although negative psychological and other health outcomes of extreme sleep lengths have been reported for over 45 years6,7, relatively little attention has been devoted to the study of long sleepers. A resurgence of interest in studying long sleep may be due to several recent studies relating long sleep to increased mortality.
A recent study of over 1 million American adults age 30–102 reported that sleep durations below 6.5 hours and above 7.5 hours were associated with increased mortality hazard5. Most of the increased mortality was associated with longer sleep (over 7.5 hours in this study), which was reported with 2.5 times the frequency of short sleep (less than 6.5 hours in this study). This finding persisted across age and gender, and the analysis controlled for over 30 other variables. A recent study of over 100,000 Japanese adults aged 40–79 found that sleep duration greater than 7 hours was associated with increased mortality. This report further controlled for “mental condition,” including stress and depressive symptomatology8.
Several other recent studies have also reported an association between long sleep and increased mortality9–18. These studies replicate similar findings in earlier studies of long sleep and mortality risk6,19–22. In fact, there is only one known survival study favoring long sleep over short or moderate sleep amounts,23 though long sleep was associated with increased risk of cardiovascular death in women in this study. These studies, spanning over 45 years, have repeatedly shown an association of long sleep with increased mortality risk. In addition to a direct relationship with sleep length, there have been a number of studies that show increased mortality risk associated with sleep complaints that are more common in long sleep. For example, Mallon and colleagues24 found that sleep duration complaints (short or long) and depression were both associated with increased mortality risk. Nilsson and colleagues 25 demonstrated a relationship between subjective sleep disturbance (e.g., problems falling asleep, early awakening) and increased mortality risk. Additionally, Dew and colleagues26 conducted an electroencephalographic (EEG) study of sleep duration and increased mortality and found that, controlling for psychiatric and medical problems, long sleep latency and poor sleep efficiency (which are more disturbed in long sleepers) were associated with increased mortality. Short sleep duration, however, was not associated with elevated mortality in this study. A summary of the results of all known mortality studies are presented in Table 1.
Table 1.
Epidemiologic association of self-reported long sleep with mortality
| Citation | Population studied (1. N, 2. Ages, 3. Years Study Duration) |
Number of covariates besides age |
Age-adjusted mortality rates RR: Relative Risk (95% confidence interval, when available) |
Mortality rates adjusted for all covariates RR: Relative Risk (95% confidence interval) |
||
|---|---|---|---|---|---|---|
| Amagai et al.18 |
|
8 | RR (ref 7–7.9 h; men, women) <6h: 2.3 (1.3, 3.9), 0.8 (0.3, 2.2) 6–6.9h: 1.1 (0.7, 1.8), 1.3 (0.8, 2.0) 7–7.9h: 1.0, 1.0 8–8.9h: 1.0 (0.7, 1.3), 1.0 (0.7, 1.5) >=9h: 1.3 (0.9, 1.8), 1.5 (1.0, 2.3) |
RR (ref 7–7.9 h; men, women) <6h: 2. 4 (1.3, 4.2), 0.7 (0.2, 2.3) 6–6.9h: 1.1 (0.7, 1.8), 1. 3 (0.8, 2.1) 7–7.9h: 1,0, 1.0 8–8.9h: 0.9 (0.6, 1.2), 1. 1 (0.8, 1.6) >=9h: 1.1 (0.8, 1.6), 1.5 (1.0, 2.4) |
||
| Ayas et al.42 |
|
15 | Fatal Coronary Heart Disease RR (Ref 8 h) <=5h: 1.67 (1.02–2.74) 6h: 1.05 (0.75–1.46) 7h: 0.80 (0.58–1.09) 8h: 1.00 >=9h: 1.71 (1.05–2.77) |
Fatal Coronary Heart Disease RR (Ref 8 h) <=5h: 1.12 (0.68–1.84) 6h: 0.91 (0.65–1.28) 7h: 0.83 (0.60–1.14) 8h: 1.00 >=9h: 1.45 (0.89–2.36) |
||
| Breslow & Enstrom19 |
|
0 | Mortality Rates | |||
| Women | Men | |||||
| <=6h: 0.097 | 0.156 | |||||
| 7h: 0.068 | 0.115 | |||||
| 8h: 0.084 | 0.111 | |||||
| >=9h: 0.104 | 0.139 | |||||
| Burazeri et al.9 |
|
24 | All-Cause Mortality Night Sleep RR (ref 6h) |
All-Cause Mortality Night Sleep RR (ref 6h) |
||
| Women | Men | Women | Men | |||
| <6h: 1.00 | 1.00 | <6h: 1.00 | 1.00 | |||
| 6–8h: 0.82 | 1.21 | 6–8h: 0.80 | 1.25 | |||
| (0.57–1.17) | (0.83–1.76) | (0.54–1.17) | (0.83–1.87) | |||
| >8h: 0.95 | 1.86 | >8h: 1.08 | 1.91 | |||
| (0.63–1.42) | (1.19–2.91) | (0.70–1.66) | (1.16–3.13) | |||
| Night Sleep + Napping RR (ref 6h) |
Night Sleep + Napping RR (ref 6h) |
|||||
| Women | Men | Women | Men | |||
| <6h: 1.00 | 1.00 | <6h: 1.00 | 1.00 | |||
| 6–8h: 0.68 | 1.03 | 6–8h: 0.64 | 1.41 | |||
| (0.46–1.01) | (0.65–1.64) | (0.42–0.97) | (0.83–2.39) | |||
| >8h: 0.84 | 1.81 | >8h: 0.80 | 2.13 | |||
| (0.56–1.27) | (1.12–2.93) | (0.51–1.24) | (1.23–3.71) | |||
| Chen & Foley10 |
|
6 | With no control for age or other covariates: All-Cause Mortality Mortality Rate (ref: 6–9h) |
No significant effect. | ||
| Data not reported | ||||||
| Subjects >=60 years <6h or >9h = 20% 6–9hr = 14.7% |
||||||
| Subjects <60 yrs: No Significant Effect | ||||||
| Gale & Martyn11 |
|
9 | All-Cause Mortality. RR (ref 9h) <=7h: 1.1 (0.8–1.4) 8h: 0.9 (0.7–1.0) 9h: 1.0 10h: 1.2 (1.0–1.4) 11h: 1.5 (1.2–1.8) >=12h: 1.9 (1.4–2.5) |
All-Cause Mortality RR (ref 9h) <=7h: 1.0 (0.7–1.4) 8h: 0.8 (0.7–1.0) 9h: 1.0 10 h: 1.2 (1.0–1.4) 11 h: 1.3 (1.0–1.7) >=12h: 1.7 (1.2–2.5) |
||
| Gottlieb et al.12 |
|
5 | Not Reported | All-Cause Mortality RR (ref 7–8h) |
||
| Women | Men | |||||
| <6=1.70 | 1.40 | |||||
| 6= 1.20 | 0.80 | |||||
| 7–8=1.00 | 1.00 | |||||
| 9=0.95 | 1.30 | |||||
| >9=1.8 | 1.5 | |||||
| Hammond6 |
|
0 | Death rate per 100 people lowest for 7 hrs in 17/18 age/gender groups |
|||
| Heslop et al.23 |
|
10 | Cardiovascular deaths RR (ref “always 7–8h”) |
Cardiovascular deaths RR (ref “always 7–8h”) |
||
| Women | Men | Women | Men | |||
| Always <7h: 2.32 (0.99, 5.42) |
1.33 (1.01,1.76) | Always <7h: 2.30 (0.94,5.60) |
1.19 (0.90,1.58) | |||
| Always >8h: 1.67 (0.22,1.25) |
0.73 (0.35,15.5) | Always >8h: 1.53 (0.20,1.18) |
0.63 (0.30,13.4) | |||
| Increase over time: 0.27 (0.04,2.00) |
0.82 (0.59,1.13) | Increase over time: 0.34 (0.04,2.56) |
0.72(0.52,1.01) | |||
| Decrease over time: 1.15 (0.47,2.84) |
1.07 (0.82,1.39) | Decrease over time: 1.34 (0.53,1.25) |
0.88 (0.67,1.16) | |||
| All-cause mortality RR (ref 7–8h) |
All-cause mortality RR (ref 7–8h) |
|||||
| Always <7h: 1.99 (1.16,3.41) |
1.30 (1.06,1.61) | Always <7h: 1.73 (0.99,3.03) |
1.15(0.99,1.42) | |||
| Always >8h: 0.60 (0.08,4.37) |
1.04 (0.65,1.66) | Always >8h: 0.58 (0.08,4.22) |
0.91 (0.57,1.46) | |||
| Increase over time: 0.49 (0.20,1.23) |
0.91 (0.72,1.15) | Increase over time: 0.47 (0.19,1.20) |
0.81 (0.64,1.02) | |||
| Decrease over time: 0.91 (0.50,1.66) |
1.17 (0.46,1.42) | Decrease over time: 0.98 (0.53,1.79) |
1.00 (0.82,1.21) | |||
| Huppert & Whittington13 |
|
Not reported |
All-Cause Mortality RR (Ref 6–9h) |
|||
| Women: NS, data not reported | ||||||
| Men <6h: 0.95 6–9h: 1.0 >9h: 2.25 | ||||||
| Kaplan19 |
|
6 | All-Cause Mortality RR (ref 7–8h) |
|||
| Sleeping >7–8 hr or <7–8 hrs Ages 38–49=1.23 (0.88–1.70) Ages 50–59=1.44 (1.08–1.91) Ages 60–69=0.95 (0.73–1.24) Ages >=70=1.05 (0.85–1.29) | ||||||
| 7–8 hrs per night not associated with different risk ratio vs not sleeping 7- 8 hrs across all groups. | ||||||
| Kojima et al.14 |
|
10 | All-Cause Mortality RR (ref 7–8.9h) |
All-Cause Mortality RR (ref:7–8.9h) |
||
| Women | Men | Women | Men | |||
| <6.9h: 0.92 | 1.90 | <6.9h: 0.90 | 1.93 | |||
| (0.53–1.62) | (1.10–3.29) | (0.50–1 61) | (1.12–3.35) | |||
| 7–8.9h: 1.00 | 1.00 | 7–8.9h: 1.00 | 1.00 | |||
| 9–9.9h: 1.10 | 1.13 | 9–9.9h: 1.07 | 1.15 | |||
| (0.61–2.00) | (0.73–1.74) | (0.58–1.95) | (0.74–1.77) | |||
| >=10h: 0.42 | 1.94 | >=10h: 0.40 | 1.77 | |||
| (0.06–3.02) | (1.01–3.76) | (0.06–2.92) | (0.88–3.54) | |||
| Kripke et al.21 |
|
5 | All-Cause Mortality RR (ref 7–7.9h) |
|||
| Women | Men | |||||
| <4h: 1.48 | 2.80 | |||||
| 4–4.9h: 1.40 | 1.59 | |||||
| 5–5.9h: 1.20 | 1.38 | |||||
| 6–6.9h: 1.13 | 1.11 | |||||
| 7–7.9h: 1.00 | 1.00 | |||||
| 8–8.9h: 1.13 | 1.10 | |||||
| 9–9.9h: 1.27 | 1.29 | |||||
| >=10 h: 1.82 | 1.77 | |||||
| Similar trends for Mortality Associated with CHD, stroke, cancer, suicide. Similar trends across multiple age-groups | ||||||
| Kripke et al.5 |
|
32 | All-Cause Mortality RR (ref 7 hr) |
|||
| Women | Men | |||||
| 2.5–3.4h: 1.33 | 1.19 | |||||
| (1.08–1.64) | (0.96–1.47) | |||||
| 3.5–4.4h: 1.11 | 1.17 | |||||
| (1.01–1.22) | (1.06–1.28) | |||||
| 4.5–5.4h: 1.07 | 1.11 | |||||
| (1.01–1.13) | (1.05–1.18) | |||||
| 5.5–6.4h: 1.07 | 1.08 | |||||
| (1.03–1.11) | (1.04–1.11) | |||||
| 6.5–7.4h: 1.00 | 1.00 | |||||
| 7.5–8.4h: 1.13 | 1.12 | |||||
| (1.09–1.16) | (1.09–1.15) | |||||
| 8.5–9.4h: 1.23 | 1.34 | |||||
| (1.17–1.28) | (1.28–1.40) | |||||
| >=10 h: 1.41 | 1.34 | |||||
| (1.34–1.50) | (1.28–1.40) | |||||
| Mallon et al.24 |
|
17 | All-Cause Mortality RR (ref 6–8h) |
“Not Significant” Data Not Reported |
||
| Women | Men | Similar patterns for mortality associated with coronary artery disease, cancer, and all other causes. |
||||
| <6h: 1.0 | 1.1 | |||||
| (0.6–1.8) | (0.6–7.0) | |||||
| 6–8h: 1.0 | 1.0 | |||||
| >8h: 1.3 | 2.0 | |||||
| (0.6–2.6) | (1.2–3.2) | |||||
| Patel et al.15 |
|
11 | All-Cause Mortality RR (ref 7h) <5h: 1.41 (1.25–1.58) 6h: 1.07 (1.00–1.15) 7h: 1.00 8h: 1.18 (1.10–1.26) >=9h: 1.72 (1.55–1.91) |
All-Cause Mortality RR (ref 7h) <5h: 1.08 (0.96–1.22) 6h: 0.99 (0.92–1.06) 7h: 1.00 8h: 1.11 (1.03–1.19) >=9h: 1.40 (1.25–1.55) |
||
| ollak et al.16 |
|
10 | All-Cause Mortality Mortality Rate (per 100) |
Cox regression models not significant for Males or females. |
||
| Women | Men | Data not available for specific hrs of sleep. | ||||
| <=4h: 19 | 24 | |||||
| 5h: 7 | 25 | |||||
| 6h: 14 | 16 | |||||
| 7h: 8 | 16.5 | |||||
| 8h: 13 | 22 | |||||
| >=9h: 18 | 30 | |||||
| Qureshi et al.17 |
|
9 | All-Cause Mortality. RR (ref 6–8h) |
|||
| 6–8h: 1.0 >8h: 1.3 (1.1–1.5) | ||||||
| Risk of Stroke RR (ref 6–8 hr) 6–8h: 1.0 >8h: 1.9 (1.2–3.1) | ||||||
| Tamakoshi & Ohno8 |
|
14 | All-Cause Mortality RR (ref 7–7.9 hr) |
All-Cause Mortality RR (ref 7–7.9 hr) |
||
| Women | Men | Women | Men | |||
| <7h: 1.08 | 1.13 | <7h: 1.14 | 1.12 | |||
| (0.99–1.17) | (1.04–1.22) | (0.99–1.32) | (0.98–1.28) | |||
| 7–7.9h: 1.00 | 1.00 | 7–7.9h: 1.00 | 1.00 | |||
| 8–8.9h: 1.24 | 1.13 | 8–8.9h: 1.20 | 1.18 | |||
| (1.14–1.34) | (1.06–1.20) | (1.05–1.38) | (1.06–1.31) | |||
| >=9h: 1.64 | 1.52 | >=9h: 1.62 | 1.49 | |||
| (1.49–1.80) | (1.42–1.64) | (1.36–1.92) | (1.31–1.70) | |||
| Wingard et al.22 |
|
14 | All-Cause Mortality % Mortality (ref 7–8h) |
In multiple logistic analysis with all covariates, sleep had significant independent association with mortality. |
||
| Women | Men | |||||
| 7–8 h: 5.5% | 8.2% | |||||
| <=6 h or >=9: 8.8% | 13.6% | |||||
This table is adapted from the summary table previously published by Youngstedt and Kripke1.
Problems with epidemiological studies
While many studies have reported a link between increased mortality and long sleep, there are several important limitations to these findings. First, long sleep is sometimes defined as sleep over 8 hours, while others have used different cutoffs, such as 9 hours or a specified extreme end of the distribution of sampled sleep times. While this inconsistency reduces the generalizability of the conclusions across studies (e.g., are they all measuring “long sleep?”), the remarkable convergence of findings strengthens overall reliability of the long sleep - mortality link.
Second, since these studies are primarily epidemiological, they employ survey and self-report measures of sleep duration, which may better reflect time in bed rather than actual sleep time27. Additionally, subjective and objective measures of sleep duration are often discrepant, and both measures inherently contain error in their estimation. Together, this means it is not known whether increased mortality risk associated with long sleep directly involves EEG sleep time or time in bed. Nonetheless, studies that have attempted to measure time in bed separately from sleep time11,14 have found that mortality relationships were consistent across both measures. Additionally, rationales for the relationship between mortality and long sleep also apply to long time in bed, such that many of the reasons that long sleep may contribute to mortality risk apply to extended time in bed as well.
Third, these studies could not accurately describe how risks associated with long sleep vary across the lifespan. While age was used as a covariate, it is likely that the mechanisms by which sleep duration increases mortality risk have varying effects at different stages of life.
Finally, these large studies fail to adequately measure the extent to which those reporting long sleep do so because of a biological need for more sleep, rather than an extension of sleep. Thus, there may be some self-described long sleepers that experience negative effects of long sleep and others for whom less sleep would be associated with the negative consequences of sleep deprivation.
Possible causes of mortality in long sleep
While the numerous studies mentioned above contain some problems regarding limitations imposed by methodology, they do all converge on the common finding that long sleep is associated with mortality. However, these studies do not sufficiently propose or test mechanisms through which this relationship would manifest. Thus, a review of the possible ways in which long sleep could lead to increased mortality is necessary.
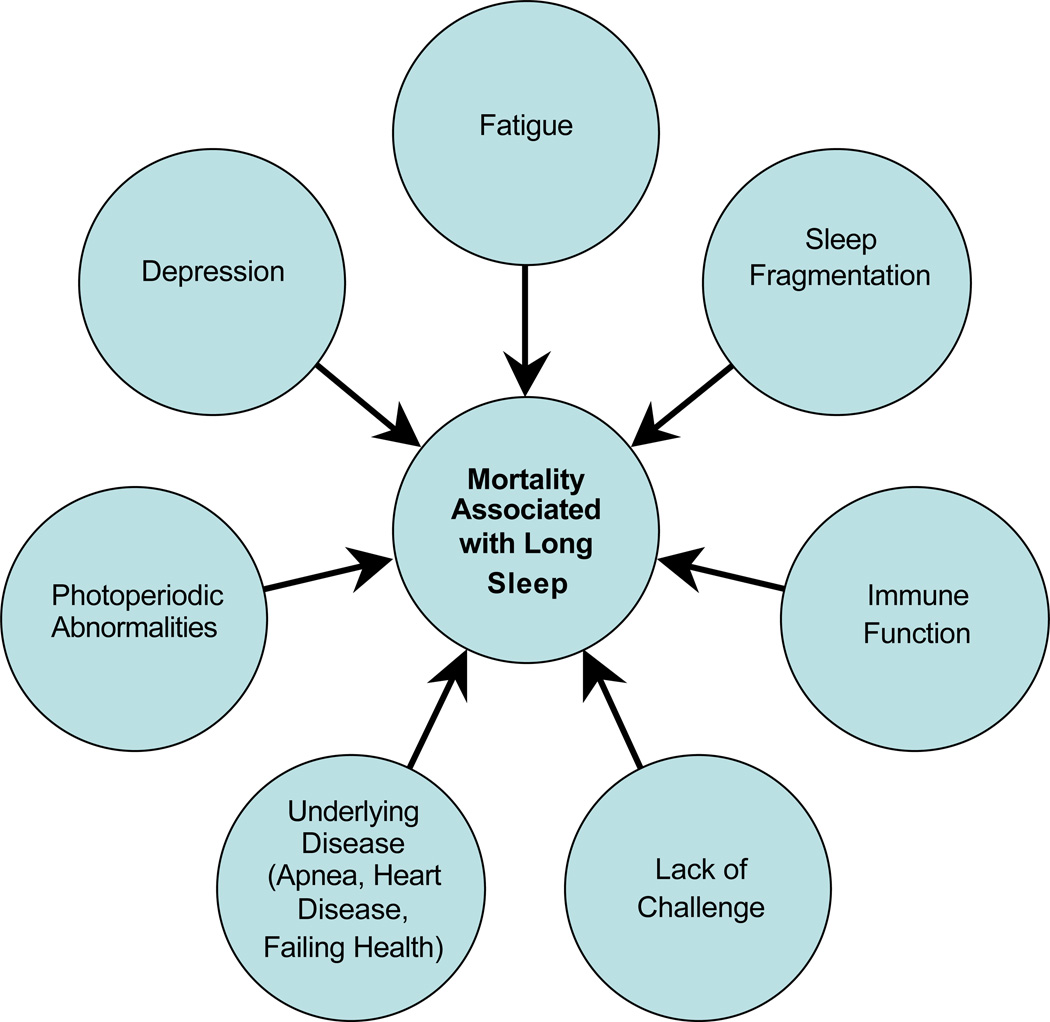
There are a number of possible explanations for the association between long sleep and increased mortality. Possible mechanisms for this relationship will be proposed and described, including (1) sleep fragmentation, (2) fatigue, (3) immune function (e.g., change to immune function), (4) photoperiodic abnormalities, (5) lack of challenge (e.g., lack of physiological challenge), (6) depression, or (7) an underlying disease process such as (a) sleep apnea, (b) heart disease, or (c) failing health. A graphical summary of these proposed mechanisms is shown in Figure 1.
Figure 1.
Hypothesized mechanisms of the relationship between long sleep and mortality.
Mortality associated with long sleep may be caused by a number of factors, which may be related to each other.
Excessive time in bed have been linked to increased sleep fragmentation, wake after sleep onset (WASO) and sleep latency1,26, each of which occur when the sleep period is punctuated by numerous intervals of wakefulness. Sleep fragmentation, in particular, has been associated with a number of negative health outcomes, including decreased energy and vitality and increased role limitations 28. Fragmented sleep may be caused by long time in bed or long sleep by extending the latter portion of sleep associated with more frequent awakenings29 . It may also be the case that long sleep (or time in bed) leads to reduced sleep efficiency through higher WASO or sleep latency, which may be associated with mortality, rather than fragmentation itself.
Second, long sleep has been associated with feelings of fatigue and lethargy30,31, as has induced sleep extension32 . These states may decrease resistance to stress and disease33, which, in turn, may lead to increased mortality. It should also be noted that fatigue and lethargy may cause long sleep.
Third, long sleep may influence the expression of cytokines (inter- and intra-cellular components of the immune system). Changes in cytokine expression associated with changes in sleep may influence mortality34–38.
Fourth, long times spent in a darkened environment may be related to a shortened photoperiod (the physiological day based on the light-dark cycle). Such photoperiodic changes and abnormalities have been associated with mortality in mammalian species39
Fifth, long sleep (or even long time in bed) may be associated with a lack of physiological challenge. A number of stressors, such as exercise, irradiation, heat and cold shock, and hypergravity, have been linked to longevity in many species, when compared to a relative absence of these stressors40. There are two possible ways in which long sleep may decrease longevity by decreasing possibly beneficial mild stressors. First, Mild sleep restriction may itself be one such stressor, associated with increased longevity; second, more time in bed provides fewer opportunities for the experiencing of other such stressors. However, it may be implausible that as little as one hour per day (8.5 hours vs. 7.5 hours) may have much of an effect on overall physiological challenge.
Sixth, there may be an underlying disease processes that mediates the relationship between long sleep and mortality. Although many risk factors were controlled in the statistical exploration of this relationship in the epidemiological studies reviewed above, it is possible that a high rate of undiagnosed illness may have contributed to both long sleep and mortality. There are at least four such diseases to consider. One is obstructive sleep apnea. Sleep apnea has been associated with increased risk of hypertension and carotid artery disease17. Several researchers have suggested that the relationship between sleep duration and mortality risk may be the result of patients with sleep apnea compensating for the large degree of fragmentation associated with the disorder by spending more time asleep or excessive amounts of time in bed41. Thus, it may be that mortality is related to variables associated with sleep apnea, rather than long sleep per se.
However, there is not sufficient evidence to suggest that patients with sleep apnea sleep any more or less than the average27 , though they may spend more time in bed. Additionally, many very reliable predictors of sleep apnea, including age, gender, body mass index and ethnicity, were controlled for in these epidemiological studies5,17. Moreover, the relationship between sleep duration and increased mortality risk has been evidenced while controlling for diseases associated with sleep apnea (e.g., cardiovascular disease), as well as with those that are not (e.g., cancer)5. Overall, then, it seems unlikely that a disease such as sleep apnea is the mechanism explaining the link between long sleep and mortality.
Another condition which may mediate the relationship between long sleep and increased mortality risk is depression. Depression can be associated with both long and short sleep, as well as over- or under-estimation of sleep time. Most of the previously mentioned epidemiological studies did not adequately measure mood disturbance. However, two of the large epidemiological studies that did measure mood disturbance showed that increased sleep duration was related to increased mortality over and above mood symptoms8,42. Moreover, sleep disturbance in depression is usually characterized as insomnia or lack of sleep rather than long sleep, and insomnia has not been consistently associated with increased mortality risk5.
Some researchers have proposed a relationship between coronary disease and sleep duration. Ayas and colleagues42 found that short and long sleep are associated with coronary events. A recent study found a U-shaped relationship between sleep duration and hypertension43. Glaser and Glaser44 suggest that mortality due to coronary events in long sleep may be due to blood pressure dipping too low over the course of the night, increased blood clotting or thrombosis. However, Mallon and colleagues 24 found that long and short sleep did not predict coronary artery disease mortality.
Finally, mortality risks of long sleep may be associated with general failing health. Long sleep is most prevalent in those over 60 years old5 and sleep is known to lengthen in the last weeks or months of life45. It may be that sleep duration lengthens gradually during the aging process and/or during periods of failing health. Under this possibility poor health would lead to long sleep, rather than long sleep leading to increased mortality.
To summarize, mortality associated with long sleep may be due to: (1) sleep fragmentation, (2) fatigue, (3) immune function (e.g., change to immune function), (4) photoperiodic abnormalities, (5) lack of challenge (e.g., lack of physiological challenge), (6) depression, or (7) an underlying disease process such as (a) sleep apnea, (b) heart disease, or (c) failing health. Additionally, it should be noted that these mechanisms are not mutually exclusive.
While some empirical support exists for these possibilities, relatively little research has attempted to elucidate the possible causal mechanisms underlying the relationship between long sleep and mortality. Also, relatively little is known about long sleepers, including factors that may influence the development and maintenance of patterns of long sleep, and the consequences of long sleep. These things may play roles in the observed mortality relationship, and a better understanding of the mechanisms and consequences of long sleep need to be understood in order to formulate and modify hypotheses regarding methods of action in the long sleep/ mortality relationship.
Before the mechanisms we propose may be responsible for the long sleep -mortality relationship can be directly tested, long sleepers need to be characterized, so that these hypotheses can be refined to more accurately reflect conditions actually associated with long sleep. While it may be plausible that all of these mechanisms relate long sleep and mortality, we first need to learn whether these mechanisms are associated with long sleep at all. To do this, we now examine the current literature to evaluate current support for these mechanisms and identify areas in which further characterization is needed.
DEFFERENCES BETWEEN LONG AND SHORT SLEEPERS
One way to understand long sleep is to examine differences between long and short sleepers. While differences between long and normal sleepers may be more relevant, most studies have examined the extremes of sleep duration relative to each other, rather than in relation to normal sleep. Despite limitations, these differences may highlight important characteristics of long sleepers suggesting mechanisms of the mortality relationship.
Scientific investigation of the correlates of extreme sleep duration has been conducted for over 80 years. Moore and colleagues46 found that shorter sleep was associated with muscular inefficiency, but Barry and Bousfield47 found that short sleep of 5.75 hours or less was associated with increased physical activity. Additionally, this study reported that ratings of “euphoria” were highest at reported sleep durations of 8 to 8.75 hours, though long sleepers of 9 hours or longer did not seem to report less “euphoria.” Over the subsequent decades, a number of studies have described differences between long and short sleepers.
Correlates of long versus short sleep
While there is relatively little known about problems associated with long sleep and how these may or may not be related to the mortality relationship, there have been several studies that have described some correlates of long sleep. While causal connections cannot be drawn from these studies, they can suggest possible future research directions by identifying conditions that are associated with long sleep. The paragraphs below will describe some demographic, diagnostic, behavioral and physiological correlates of long sleep.
Several epidemiological studies have examined correlates of sleep duration. A recent report has found numerous correlates of self-reported habitual long sleep from the Nurses Health Study II48. This study found that long sleepers (at least 9 hours per night) reported increased likelihood of a history of depressive symptoms, antidepressant use, benzodiazepine use, lack of physical activity, never married or divorced status, living alone, lower income, unemployed status, and lower social status. Lower socioeconomic status may be a primary driving factor in the long sleep-mortality relationship, and should be examined. Specifically, future studies could discern how socioeconomic status alters sleep duration.
Additionally, long sleep was associated with increased likelihood of the diagnosis of a number of medical conditions, including obesity, diabetes, hypothyroidism, seizure, head injury, multiple sclerosis, stroke, coronary disease, hypertension, lupus, rheumatoid arthritis, osteoarthritis, herniated disc, asthma, chronic obstructive pulmonary disease, cancer, and inflammatory bowel disease. Finally, long sleep was associated with restless legs syndrome, snoring and permanent night shift work. However, although all of these factors were associated with long sleep, none of them fully explained the mortality relationship with long sleep.
Depression was the factor that contributed most and may be most likely to confound the long sleep-mortality relationship48.
A population study from Finland49 found that long sleepers reported more feelings of being “non-energetic or tired” than mid-range sleepers, but no difference was found for short sleepers. A similar pattern was found for endorsements of feeling “exceptional tiredness.” Self-reports of “sleeping disorders or insomnia,” “difficulties in getting sleep without sleeping medicines,” “overexertion or exhaustion” and “being awake during the night” were reported more in short sleepers than long sleepers.
Another recent report50 suggests that short sleep (6–7 hours or <6 hours) was associated with lower reports of self-rated overall health than normal (7–8 hours) or long (8–10 or >10 hours) young adult sleepers. There were no differences reported between normal and long sleepers in this study. Interestingly, when depression was entered into statistical models, odds ratios were attenuated but otherwise did not change between sleep duration and health report. This may reflect ontogenetic factors in the relationship between sleep duration and health. A study by Pinheiro and colleagues51 suggests that long sleep (at least 8 hours) is associated with risk of developing breast cancer, relative to sleep less than 8 hours. Additionally, as sleep duration increases, risk for breast cancer seems to increase, and as sleep duration decreases, risk seems to slightly decrease.
Several studies have demonstrated that increased sleep duration and time in bed are associated with increased weight and daytime sleepiness and decreased mood, sleep quality, health and quality of well-being52,53. However, daytime sleepiness has been associated with sleep fragmentation rather than simply sleep duration, and since sleep fragmentation is directly related to time in bed, perhaps increased time in bed is itself harmful27.
Short sleep duration is associated with increased ghrelin and decreased leptin54, although long sleepers or a U-shaped relationship were not addressed. Ayas and colleagues42 found a U-shaped relationship between sleep duration and risk for diabetes, suggesting that long and short sleepers have approximately 1.5 times the risk as normal length (7–8 hours) sleepers. This finding was recently replicated, suggesting a 2.5-fold increase risk for diabetes in short sleepers and a 3-fold risk of diabetes in long sleepers55. Motohashi and colleagues56 found that there was no difference in blood glucose, blood cholesterol, HDL, cholesterol, and triglycerides in long versus short sleepers. Additionally, Hicks and colleagues57 found that long sleepers tend to eat larger meals and snacks less frequently than shorter sleepers, who tended to have a less regular meal pattern. These findings are in contrast to other recent evidence that partial sleep deprivation is associated with disrupted leptin and ghrelin as well58. Also, several recent studies suggest that short sleep, rather than long sleep, is associated with increased obesity59, as well as intake of fats 60. It is unclear which of these endocrine abnormalities are associated with sleep duration versus sleep disruption. Additionally, the fact that data suggest endocrine abnormalities seem to play a role in short sleep more than long sleep implies that the mechanisms for health effects on both ends of the spectrum may not be the same. Also, these changes may not reflect a continuous effect – rather, perhaps there are certain long and short sleep thresholds that increase risk.
Ohayon61 found that long sleep was associated with age of 65–74 years, not working, being underweight, lack of physical activity, disrupted sleep, use of sleeping medications, and anxiety disorder in an older sample. Short sleep was associated with age between 55–64 or 74–84 years, lack of physical activity, drinking six cups or more of coffee per day, taking sleeping medications, difficulty initiating sleep, disrupted sleep, early morning awakening, and anxiety disorder.
Thus, sleep duration has been shown to be related to a litany of variables, some of which may or may not be related to the mortality relationship. Most notably, long sleep may be associated with depression, medication use, lack of activity, lower socioeconomic status, medical problems, dietary problems, heart problems, breathing problems, and sleep disorders. These factors seem to support many of the proposed mechanisms, particularly sleep fragmentation, fatigue, immune function, sleep apnea, depression, and heart disease In addition to these correlates of long and short sleep, long sleep is related to many circadian, sleep-related and psychological factors.
Circadian characteristics of long versus short sleepers
Aschoff62 reported that perception of time and activity durations may be individual traits and may be different in long and short sleepers. There have been several other studies that describe relationships between circadian and photoperiodic variables and sleep duration.
Long sleepers demonstrate lower average daily temperature than controls63 and tend to initiate sleep much closer to the circadian body temperature peak than short sleepers64. It is interesting to note that this finding is similar to those in temporal isolation studies, where subjects tend to initiate sleep closer to the temperature peak65. However, long sleepers may initiate sleep at this point only because it coincides with an earlier bedtime, to accommodate longer sleep while adhering to a regular wake time8. Alternatively, it may be that long sleepers have a reduced ability to tolerate sleep pressure, which then leads to increased sleep, as suggested by Aeschbach and colleagues 66,67 .
Another physiological process that drives sleep is the regulation of the melatonin system. Melatonin is a hormone that is moderated by light transduction through the retina to the hypothalamus and signals the lack of light or duration of night in the environment – it is released in darkness and is inhibited by light. Endogenous melatonin functions as a sleep-promoting agent in diurnal animals such as humans; longer durations of melatonin excretion (via longer night) are related to increases in sleep, and shorter durations (associated with more light) with less sleep. Aeschbach and colleagues 68 reported that long sleepers have a longer duration of melatonin secretion at night relative to short sleepers. It may be the case that this produces longer sleep durations. Conversely, it may also be the case that more time in bed leads to increased melatonin secretion durations, leading to more sleep. There is experimental data that time in bed (or duration of the dark period) influences melatonin duration, but little experimental evidence for the converse, and melatonin agonists have only very minimal effects on sleep duration69. Thus, the increased duration of melatonin secretion in long sleepers may be a consequence, rather than cause, of extended time in bed.
Measures of “morningness” and “eveningness” are often utilized in circadian rhythms research to characterize people based on expressions of endogenous rhythms70. Several findings among long and short sleepers have demonstrated differences in this domain. Taillard and colleagues71 demonstrated that eveningness was associated with a greater need for sleep (which may be characteristic of long sleepers), as well as increased sleep debt. Vera-Villarroel and colleagues 72 showed that long sleepers demonstrated less morning activity than short sleepers, as well as more temperature sensitivity and less EMG activity in the morning than short sleepers.
These findings suggest that long sleepers may demonstrate circadian and photoperiodic differences, including increased homeostatic sleep pressure and melatonin duration, as well as different activity rhythms and perceptions of rhythmicity. These findings support the photoperiodic hypothesis of the long sleep-mortality relationship, although they do not directly assess photoperiodic and circadian variables influences on mortality risk.
Objective sleep in long versus short sleepers
Early studies of sleep differences in long and short sleepers reported that long sleepers demonstrated greater sleep latency and more WASO, REM, stage 1 and stage 2 sleep, and equivalent or less slow wave sleep than short sleepers29. Fukuda and colleagues29 also found that short sleepers had higher REM density in the 2nd and 3rd REM cycle. Aeschbach and colleagues66 found that following sleep deprivation, sleep latency and REM density went down in short sleepers, and slow wave sleep was affected to a greater extent in long sleepers.
These sleep differences are consistent with the idea that long sleep is not characteristically different from lengthened sleep, such that sleep characteristics typically associated with the end of the night tend to be more present in long sleep and sleep at the beginning of the night seems to be less affected. However, there may be abnormalities associated with slow wave sleep in long sleepers, such that they may experience less overall, despite more time asleep. Slow wave sleep reductions are also associated with aging and health problems associated with a number of the hypotheses regarding the long sleep-mortality link, including reduced immune function and conditions associated with decreased health73 . Also, long sleep may be associated with REM abnormalities. As REM abnormalities may be related to mood disturbance74, there may be a possible mood component in long sleep that is consistent with the depression hypothesis underlying the mortality relationship.
Studies of endocrine function during sleep have suggested that long sleep periods are associated with disturbed prolactin rhythms75 and that patients with growth hormone deficiencies show marked increases in total sleep time following treatment without increases in REM sleep76 . It is unclear how these findings relate to the larger picture of sleep differences in long sleep, but reinforce the idea that changes in sleep duration are related to endocrine function, as noted in the aforementioned increased diabetes risk.
Subjective sleep in long versus short sleepers
Two large studies have reported increased rates of self-reported insomnia in long sleepers, compared to average sleepers5,77 . Another study, analyzing data from a census-matched sample polled by the National Sleep Foundation, found that long sleepers report significantly more complaints than average sleepers31. Specifically, they reported increased rates of trouble falling asleep, awakenings during the night, early morning awakenings, nonrestorative sleep and daytime sleepiness. One possible explanation for these findings is that increased time in bed leads to fragmentation (described below), which may lead to these complaints.
Behavioral sleep practices in long versus short sleepers
Hicks and Youmans78 report that long sleepers are more likely to engage in sleep-promoting behaviors than short sleepers, reporting twice as many different sleep-promoting behaviors, and a trend toward increased frequency of behaviors. Long sleepers were more likely to use alcohol (perhaps to induce sleep) and short sleepers more likely to use food before bed to induce sleep. Alcohol intake close to bed time increases sleep fragmentation and daytime sleepiness after waking79 , potentially contributing to the increased reports of insomnia and poor sleep quality in long sleepers reviewed above. These findings, however, may be confounded with the age and social background of subject groups.
Overall, data on objective sleep, subjective sleep, and sleep behaviors suggest that long sleepers normally experience fragmented sleep, report more complaints about their sleep, and engage in more compensatory behaviors in an effort to increase sleep than do others. Long sleepers also show an exaggerated slow wave sleep rebound after sleep loss. Taken together, these findings support the photoperiodic findings by suggesting there may be homeostatic dysregulation in long sleepers, which may be indicative of depression, sleep fragmentation, sleep apnea, or other conditions that may underlie the mortality relationship.
Psychological characteristics of long versus short sleepers
Research literature on psychological characteristics of long sleepers has shown several interesting patterns, suggestive of impaired functioning and increased risk for negative health outcomes. As such, these data may also aid the development and evaluation of hypotheses regarding the mechanism underlying the link between long sleep and mortality.
Numerous studies have noted some psychological characteristics that may differentiate long and short sleepers. For example, Hartmann and colleagues 80 found that on the California Personality Inventory (CPI), long sleepers reported lower “social presence,” “sociability,” and “flexibility” than short sleepers. Taub81 found that long sleepers reported more “aggression and misfortune elements” in dreams. On the Minnesota Multiphasic Personality Inventory (MMPI), long sleepers have scored lower on scales measuring social desirability7, 80 and mania82 and higher on scales measuring social introversion7,80,82 and psychiatric disruption82.
Long sleepers may also demonstrate impaired coping abilities, which may lead to poor health outcomes. Long sleepers report less of an external locus of control than short sleepers83,84 . Hicks and colleagues85 found that following a particularly devastating earthquake in San Francisco, long and short sleepers differed in their responses on the Ways of Coping Questionnaire. Long sleepers reported lower “Confrontive,” “Self-controlling,” “Accepting responsibility,” and “Positive reappraisal” scores than short sleepers. Hicks and Picchioni86 found that after taking a long sleep, fewer positive coping strategies were reported, including “self-controlling,” “responsibility,” “problem solving,” and “reappraisal.” In a study of reported stressful events in long, short and variable length sleepers, Sexton-Radek87 found that long sleepers had more inconsistent responses to stress. When describing stressful events, long sleepers tended to emphasize performance quality, whereas short sleepers tended to emphasize objective performance and variable sleepers tended to emphasize interpersonal stresses.
Hartmann and colleagues7 also conducted clinical interviews with all of the long and short sleepers. Long sleepers reported more worries. They were “less definable,” but had variable opinions and tended to be “nonconformists and critical.” They were found to be “more uncomfortable in many ways” than short sleepers. They “complained” more, were “overly anxious” and inhibited and may even have been “mildly depressed.” They were unsure of themselves. They tended toward being creative and artistic. Sometimes they use sleep to escape from an unpleasant experience. They were “definitely worriers.”
Long sleepers reported having started work at an older age and for fewer hours per week than short sleepers80. More recently, Motohashi and colleagues56 found that short sleep was associated with increased overtime work.
Later studies demonstrated that short sleepers reported more anxiety88 than long sleepers and more hypomania symptoms89 than controls. In contrast, Jean-Louis and colleagues 27 found that increased sleep duration was not related to reported quality of well-being, though the range in the sample was only between 5–9 hours.
Taken together, these findings suggest that long sleepers are particularly susceptible to psychopathology, especially problems with mood and anxiety. Long sleepers might be better characterized as “worriers” and were typically less successful than short sleepers. These findings are very consistent with those recently reported by Patel and colleagues48. Regarding mortality, these findings suggest that long sleepers are predisposed to many stressors, which may be related to increased depression, heart disease, fatigue and lack of challenge.
STUDIES OF VARIABLE SLEEPERS
Variable sleepers are, by definition, people who fluctuate between short sleep, normal sleep, and long sleep, depending on various factors30. Understanding variable sleepers may provide insight into the function of sleep30 and may elucidate mechanisms by which people become long sleepers. Understanding how a person becomes a long sleeper may help clarify the long sleep - mortality connection.
Hartmann and Brewer90 reported that increased need for sleep was found when subjects reported a period of stress. However, Hicks and Garcia91 found that high stress leads to reduction in sleep time of about 1 standard deviation and low stress to an increase of about 1 standard deviation of sleep time. Nonetheless, findings from previously mentioned studies7,80,82,87 argue that lengthening sleep is related more to stress and stressful events than positive events. Sanford and colleagues92 note that an aversive event can shorten or lengthen sleep in mice for days, depending on the amount of conditioning and training the animal has received. While the neurological mechanisms of this response are currently not completely understood, some investigation has implicated that the noradrenergic locus coeruleus plays a role93.
Taken together, these results reiterate many of the findings associated with characterological data on long sleepers. Long sleep may be brought on by stress and stressful events. Variable sleepers may respond to stressors with increased sleep but do not maintain this pattern. It is currently unclear why some people develop this pattern for many years and some do not. These findings do, however, support the hypothesis that the relationship between long sleep and mortality may be driven by the factors that lead to long sleep in the first place, such as difficulty handling stress, which may be secondarily associated with depression, fatigue, or poor health.
CONTROLLED SLEEP EXTENSION
While there have been few studies of laboratory sleep extension, this literature may inform hypotheses regarding the long sleep and mortality relationship. These studies document the physiological and psychological effects of artificially lengthening otherwise normal sleep. Clarifying these responses may provide further evidence for mechanisms of the mortality relationship.
By spending additional time in bed, it is possible to increase sleep duration up to 10–12 hours94 for a few weeks only. A common finding, called the “Rip van Winkle Effect,” can be seen when adults sleep longer than usual – they often report a number of symptoms that can persist for hours, including feelings of fatigue, lethargy, irritability and sleepiness for up to 4.4 hours after finally waking95 . These feelings of sleepiness and fatigue may lead to the increased desire to sleep, creating a vicious cycle of increased sleep and sleepiness.
These results are supported by research96 which found that average-length sleepers who extend their sleep duration by 2–3 hours report sleepiness, decreased mood, slowed reaction time, lowered vigilance and problems with mathematical tasks. Some studies demonstrated decreases in objective sleepiness97 and increases in objective sleep98 following extended sleep, but these studies did not measure subjective experience of sleepiness, fatigue or mood impairment.
Sleep extension that increases time in bed will likely increase sleep fragmentation99 and this fragmentation is associated with a number of negative health outcomes and sleep complaints. If time in bed is extended to 24 hours, sleep becomes extremely fragmented, resembling that of nursing home patients who cannot stay awake or asleep for more than an hour at a time100.
LONG SLEEP IN CHILDREN AND ADOLESCENTS
One way in which long sleep risks may be pertinent to pediatric populations is the increasing incidence of sleep apnea in children, which may be related to increasing rates of overweight101 and is associated with performance deficits102.
Few studies have specifically identified risks associated with long sleep duration in children. Sampei and colleagues103 found that in a group of 5–6 year-olds, the quartile with the highest reported sleep duration (>=660 minutes) demonstrated the highest values of systolic blood pressure than the quartile with the lowest reported sleep duration (<=585 minutes). No relationship was found for diastolic blood pressure. A recent study by Gaina and colleagues104 found that short sleep duration (and increased sleep latency) was associated with evening-type preference in adolescents aged 12–15 years, though Giannotti and colleagues105 found that in students aged 14–19 years, eveningness was related to short sleep duration during the week, but long sleep duration on weekends, when sleep schedules may better approximate endogenous preference. These students demonstrated more napping during school days, daytime sleepiness, attention problems, and injuries. They also demonstrated poorer school achievement and more emotional upset than the other chronotype. These data illustrate that pediatric populations typically sleep longer than adults, and that sleep duration may be related to similar variables as adults, including health and functional impairment. However, it is unclear whether these relationships are valid for natural long sleepers, short sleepers or both.
CONCLUSION
While there are some reports of correlates and effects of long sleep in the scientific literature, there seems to be a relationship between long sleep and increased mortality risk, which may or may not be related to a number of factors. Six proposed mechanisms of this relationship include: (1) sleep fragmentation, (2) fatigue, (3) immune function, (4) photoperiodic abnormalities, (5) lack of physiological challenge, (6) depression, and (7) an underlying disease process, such as (a) sleep apnea, (b) heart disease, or (c) failing health.
The present literature suggests that long sleepers are characteristically different from short or normal sleepers in a number of domains; they present with demographic, circadian, sleep-related, psychological, and other differences. Taken together, these findings tend to support many of the proposed hypotheses. While most of the available studies did not examine long sleep in the context of mortality, there seems to be a significant overlap between long sleep and depression1, sleep fragmentation26,28–29 , and photoperiodic abnormalities1. Health issues (e.g., sleep apnea41 , heart disease42, and failing health5) and lack of challenge were also somewhat supported, though usually indirectly. Thus, much of the evidence supports these hypotheses to varying degrees and future studies should examine long sleep with respect to these domains, especially depression and sleep fragmentation (which itself may be indicative of sleep apnea or other conditions).
Studies of variable sleepers have elucidated some of the possible functions of long sleep and further research in this direction will better determine whether long sleep may be a consequence of stress or coping mechanisms. Sleep extension studies highlight some of the effects of artificially lengthening sleep.
What are the physiological characteristics of long sleepers?
Several recent studies have indicated that long sleepers have a characteristically different melatonin rhythm than short sleepers68. Other circadian physiological differences also seem to characterize long sleepers, such as temperature, timing and activity63–67. Future studies will further elucidate these findings and possibly extend them. For example, there may be CLOCK gene polymorphisms associated with long and short sleepers.
How can we describe the sleep of long sleepers?
Long sleepers seem to present with an extended sleep period that contains more REM, stage 1, and stage 2 sleep, which is to be expected. Long sleepers may have decreased slow wave sleep29. They also may experience more sleep fragmentation. More complex polysomnographic techniques may clarify and expand these findings.
What are the psychological characteristics of long sleepers?
Numerous studies have demonstrated that long sleepers experience more anxiety and social introversion and less psychological health than short sleepers7,80–82 . However, most of these studies were conducted over 30 years ago and have not been able to make use of much advancement in research and medicine since that time. Therefore, these studies need to be reevaluated and their findings need to be replicated.
How do the differences between long and short sleepers relate to the findings of increased mortality risk?
The circadian and photoperiodic findings implicate a photoperiodic mechanism in mortality. Increased incidence of psychological distress, depression, and anxiety, and decreased social interaction, coping skills and organization paint a picture of general poor psychological functioning, which is characteristic of many of the proposed mechanisms, most notably sleep fragmentation, fatigue, lack of challenge and depression. Taken together, many of the findings related to long sleep tend to agree with many of the proposed mechanisms of mortality associated with long sleep. However, many of these studies employed questionable methods. Additionally, most of these studies were purely cross-sectional, disallowing any conclusions of causality. Finally, many studies that would test some underlying mechanisms have not yet been conducted, including specific studies of immune functioning in long sleepers, psychological functioning in long sleepers, and genetic abnormalities associated with long sleep.
What are the clinical implications of these findings?
The findings inform sleep evaluation and treatment in a number of important ways. First and foremost, they establish that sleep evaluation should examine long sleep in addition to sleep insufficiency. Second, these findings have implications on the assessment of sleep quality. Long sleepers report and demonstrate poorer sleep quality than normal sleepers. However, sleep assessment instruments traditionally assign scores based on sleep insufficiency, as opposed to sleep inefficiency. Screening measures might need to include long sleep in addition to short sleep in their assessments. Third, mild sleep restriction for long sleepers may reduce the risks associated with long sleep. Such an intervention will reduce time in bed and total sleep time, which may reduce sleep fragmentation and normalize sleep. While a standardized procedure for such sleep restriction has not yet been developed, one possibility has been proposed by Youngstedt and Kripke1. In addition to these examples, the findings highlight the importance of measuring sleep duration (long and short) in patients complaining of sleep disorders, circadian rhythm problems, mood disturbance, anxiety, and other clinical conditions. Simply assessing lack of sleep or general sleep disturbance may be insufficient. Also, treatments for patients presenting with these conditions may include addressing long sleep.
When is long sleep a life-long trait and when can it be induced?
While some long sleepers report that their sleep pattern has existed for many years, studies of variable-length sleepers show that long sleep can also be induced30. Long sleep may be a form of coping with stress90, and further research into the mechanisms of varying sleep duration will clarify this. It is still currently unknown whether long sleep is generally a trait, what makes a person become a long sleeper when they were previously a short or normal sleeper, and how duration of long sleep pattern may be related to increased mortality risk.
Why is long sleep associated with increased mortality risk?
There are a number of ways in which long sleep may be related to shorter lifespan, such as depression, homeostatic, and photoperiodic disturbance. Also, long sleep may suggest an underlying health condition that may be related to increased mortality risk. Cross-sectional studies that adequately control for these factors need to be conducted and experimental studies need to be undertaken to elucidate causal relationships. Direct mechanism studies may be most appropriate in animal models were potential mechanisms can be more directly manipulated and their consequences more easily followed to fruition. In this manner, the hypotheses proposed here as most promising can be eliminated and/or refined. In undertaking this research, it should be noted that although long sleep is associated with increased mortality risk, these results are based on habitual sleep patterns and it is currently unknown whether reducing sleep time in long sleepers will positively or negatively impact mortality risk. This represents another set of studies that should be conducted.
PRACTICE POINTS.
Reported long sleep is associated with increased mortality risk. It is currently unclear whether mortality is associated with long sleep or long time in bed. Nonetheless, there are several testable mechanisms for this relationship that can apply to either marker.
Proposed mechanisms for mortality associated with long sleep include: (1) sleep fragmentation, (2) fatigue, (3) immune function, (4) photoperiodic abnormalities, (5) lack of challenge, (6) depression, and (7) an underlying disease process, such as (a) sleep apnea, ( b) heart disease, or (c) failing health. The mostly strongly supported mechanisms in the current literature include depression, photoperiodic abnormalities, and health risks.
Long sleepers demonstrate some physiological differences from short sleepers. Particularly, long sleepers seem to demonstrate a characteristically different melatonin rhythm, as well as differences in rhythms of temperature, timing and activity. Additionally, long sleepers demonstrate differences in electroencephalographic measurements of sleep.
Clinical sleep evaluations should examine long sleep in addition to short sleep. Assessment of sleep quality should be sensitive to the U-shaped relationship between sleep duration and sleep complaints. Screening measures might need to include long sleep in addition to short sleep in their assessments.
RESEARCH AGENDA.
Cross-sectional studies that adequately control for underlying health conditions, such as coronary disease, sleep apnea and depression, may further explain the roles of these factors in mortality.
Cross-sectional studies that sufficiently characterize “long-sleepers” will better ascertain to what extent “long sleep” describes time in bed and to what extent it describes sleep duration.
Experimental studies examining whether reducing sleep time in habitually long sleepers will positively or negatively impact mortality risk may provide a preventative measure to counteract the risks. The initial studies may be best conducted in animal models by: (a) shortening sleep in the longest sleeping members of a given species (to the species mean, for example), and/or (b) by shortening sleep in a long sleeping species to the length seen in the wild type species.
Experimental studies should further explore genetic and physiological differences among long, normal-length and short sleepers.
Experimental studies should examine relationships among the proposed mechanisms of mortality risk in long sleep, with particular emphasis on depression, immune functioning, homeostatic and photoperiodic characteristics, and medical history in long sleepers.
Clinical studies should examine the utility of adding long sleep to screening measures and indications of sleep disturbance.
Studies of the causes of long sleep (genetic and environmental) may further aid in the understanding of the mortality relationship.
Studies should examine the relationship between sleep duration and mortality across the lifespan, as risks may vary with age.
Mutant short and long sleepers in both rodents and flies (which may be preferred due to a shorter life span) should be examined to see if 1) there is a mortality difference, and 2) there are physiological or genetic markers associated with sleep duration and mortality. Subsequently, these additional markers should be explored for causal relationships with mortality.
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Youngstedt SD, Kripke DF. Long sleep and mortality: rationale for sleep restriction. Sleep Med Rev. 2004;8(3):159–174. doi: 10.1016/j.smrv.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 2.Bonnet MH, Arand DL. We are chronically sleep deprived. Sleep. 1995;18(10):908–911. doi: 10.1093/sleep/18.10.908. [DOI] [PubMed] [Google Scholar]
- 3.Kripke DF. Chronic hypnotic use: deadly risks, doubtful benefit. Sleep Med Rev. 2000;4(1):5–20. doi: 10.1053/smrv.1999.0076. [DOI] [PubMed] [Google Scholar]
- 4.Bliwise DL. Historical change in the report of daytime fatigue. Sleep. 1996;19(6):462–464. doi: 10.1093/sleep/19.6.462. [DOI] [PubMed] [Google Scholar]
- 5.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59(2):131–136. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 6.Hammond EC. Some preliminary findings on physical complaints from a prospective study of 1,064,004 men and women. Am J Public Health. 1964;54:11–24. doi: 10.2105/ajph.54.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hartmann E, Baekeland F, Zwilling GR. Psychological differences between long and short sleepers. Arch Gen Psychiatry. 1972;26(5):463–468. doi: 10.1001/archpsyc.1972.01750230073014. [DOI] [PubMed] [Google Scholar]
- 8.Tamakoshi A. Ohno Y Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study. Japan. Sleep. 2004;27(1):51–54. [PubMed] [Google Scholar]
- 9.Burazeri G, Gofin J, Kark JD. Over 8 hours of sleep --marker of increased mortality in Mediterranean population: follow-up population study. Croat Med J. 2003;44(2):193–198. [PubMed] [Google Scholar]
- 10.Chen D, Foley D. Prevalence of sleep disturbance and mortality in the U.S. population. Sleep Res. 1994;23:116. [Google Scholar]
- 11.Gale C, Martyn C. Larks and owls and health, wealth, and wisdom. Br Med J. 1998;317:1675–1677. doi: 10.1136/bmj.317.7174.1675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gottlieb DJ, Schulman DA, Nam BH, D’Agostino RA, Kannel WA. Sleep duration predicts mortality: the Framingham Study. Sleep. 2002;25:A108. [Google Scholar]
- 13.Huppert FA, Whittington JE. Symptoms of psychological distress predict 7-year mortality. Psychol Med. 1995;25:1073–1086. doi: 10.1017/s0033291700037569. [DOI] [PubMed] [Google Scholar]
- 14.Kojima M, Wakai K, Kawamura T, Tamakoshi A, Aoki R, Lin Y, Nakayama T, Horibe H, Aoki N, Ohno Y. Sleep patterns and total mortality: a 12-year follow-up study in Japan. J Epidemiol. 2000;10(2):87–93. doi: 10.2188/jea.10.87. [DOI] [PubMed] [Google Scholar]
- 15.Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, Stampfer MJ, Hu FB. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27(3):440–444. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- 16.Pollak CP, Perlick D, Linsner JP, Wenston J, Hsieh F. Sleep problems in the community elderly as predictors of death and nursing home placement. J Community Health. 1990;15:123–135. doi: 10.1007/BF01321316. [DOI] [PubMed] [Google Scholar]
- 17.Qureshi AI, Giles WH, Croft JB, Bliwise DL. Habitual sleep patterns and risk for stroke and coronary heart disease: a 10- year follow-up from NHANES I. Neurology. 1997;48:904–911. doi: 10.1212/wnl.48.4.904. [DOI] [PubMed] [Google Scholar]
- 18.Amagai Y, Ishikawa S, Gotoh T, Doi Y, Kayaba K, Nakamura Y, Kajii E. Sleep duration and mortality in Japan: the Jichi Medical School Cohort Study. J Epidemiol. 2004;14(4):124–128. doi: 10.2188/jea.14.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Breslow L, Enstrom JE. Persistence of health habits and their relationship to mortality. Prev Med. 1980l;9(4):469–483. doi: 10.1016/0091-7435(80)90042-0. [DOI] [PubMed] [Google Scholar]
- 20.Kaplan GA, Seeman TE, Cohen RD, Knudsen LP, Guralnik J. Mortality among the elderly in the Alameda County Study: behavioral and demographic risk factors. Am J Public Health. 1987 Mar;77(3):307–312. doi: 10.2105/ajph.77.3.307. Erratum in: Am J Public Health 1987;77(7):818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kripke DF, Simons RN, Garfinkel L, Hammond EC. Short and long sleep and sleeping pills. Is increased mortality associated? Arch Gen Psychiatry. 1979;36(1):103–116. doi: 10.1001/archpsyc.1979.01780010109014. [DOI] [PubMed] [Google Scholar]
- 22.Wingard DL, Berkman LF, Brand RJ. A multivariate analysis of health-related practices: a nine-year mortality follow -up of the Alameda County Study. Am J Epidemiol. 1982;116(5):765–775. doi: 10.1093/oxfordjournals.aje.a113466. [DOI] [PubMed] [Google Scholar]
- 23.Heslop P, Smith GD, Metcalfe C, Macleod J, Hart C. Sleep duration and mortality: The effect of short or long sleep duration on cardiovascular and all-cause mortality in working men and women. Sleep Med. 2002;3(4):305–314. doi: 10.1016/s1389-9457(02)00016-3. [DOI] [PubMed] [Google Scholar]
- 24.Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of a middle-aged Swedish population. J Intern Med. 2002;251(3):207–216. doi: 10.1046/j.1365-2796.2002.00941.x. [DOI] [PubMed] [Google Scholar]
- 25.Nilsson PM, Nilsson JA, Hedblad B, Berglund G. Sleep disturbance in association with elevated pulse rate for prediction of mortality--consequences of mental strain? J Intern Med. 2001;250(6):521–529. doi: 10.1046/j.1365-2796.2001.00913.x. [DOI] [PubMed] [Google Scholar]
- 26.Dew MA, Hoch CC, Buysse DJ, Monk TH, Begley AE, Houck PR, Hall M, Kupfer DJ, Reynolds CF., 3rd Healthy older adults' sleep predicts all -cause mortality at 4 to 19 years of follow-up. Psychosom Med. 2003;65(1):63–73. doi: 10.1097/01.psy.0000039756.23250.7c. [DOI] [PubMed] [Google Scholar]
- 27.Jean-Louis G, Kripke DF, Ancoli-Israel S. Sleep and quality of well -being. Sleep. 2000;23(8):1115–1121. [PubMed] [Google Scholar]
- 28.Bennett LS, Barbour C, Langford B, Stradling JR, Davies RJ. Health status in obstructive sleep apnea: relationship with sleep fragmentation and daytime sleepiness, and effects of continuous positive airway pressure treatment. Am J Respir Crit Care Med. 1999;159:1884–1890. doi: 10.1164/ajrccm.159.6.9808107. [DOI] [PubMed] [Google Scholar]
- 29.Fukuda K, Miyasita A, Inugami M. Differences in sleep-wake habits and EEG sleep variables between active morning and evening subjects. Sleep. 1987;10(4):330–342. doi: 10.1093/sleep/10.4.330. [DOI] [PubMed] [Google Scholar]
- 30.Hartmann E. The Functions of Sleep. New Haven: Yale; 1974. [Google Scholar]
- 31.Grandner MA, Kripke DF. Self-reported sleep complaints with long and short sleep: a nationally representative sample. Psychosom Med. 2004;66(2):239–241. doi: 10.1097/01.psy.0000107881.53228.4d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Taub JM, Berger RJ. Performance and mood following variations in the length and timing of sleep. Psychophysiology. 1973;10(6):559–570. doi: 10.1111/j.1469-8986.1973.tb00805.x. [DOI] [PubMed] [Google Scholar]
- 33.Dantzer R. Cytokine-induced sickness behavior: mechanisms and implications. Ann N Y Acad Sci. 2001;933:222–234. doi: 10.1111/j.1749-6632.2001.tb05827.x. [DOI] [PubMed] [Google Scholar]
- 34.Born J, Lange T, Hansen K, Molle M, Fehm HL. Effects of sleep and circadian rhythm on human circulating immune cells. J Immunol. 1997 May 1;158(9):4454–4464. [PubMed] [Google Scholar]
- 35.Irwin M, McClintick J, Costlow C, Fortner M, White J, Gillin JC. Partial night sleep deprivation reduces natural killer and cellular immune responses in humans. FASEB J. 1996;10(5):643–653. doi: 10.1096/fasebj.10.5.8621064. [DOI] [PubMed] [Google Scholar]
- 36.Irwin M. Neuroimmunology of disordered sleep in depression and alcoholism. Neuropsychopharmacology. 2001;25(5 Suppl):S45–S49. doi: 10.1016/S0893-133X(01)00338-4. [DOI] [PubMed] [Google Scholar]
- 37.Papanicolaou DA, Wilder RL, Manolagas SC, Chrousos GP. The pathophysiologic roles of interleukin-6 in human disease. Ann Intern Med. 1998;128(2):127–137. doi: 10.7326/0003-4819-128-2-199801150-00009. [DOI] [PubMed] [Google Scholar]
- 38.Rogers NL, Szuba MP, Staab JP, Evans DL, Dinges DF. Neuroimmunologic aspects of sleep and sleep loss. Semin Clin Neuropsychiatry. 2001;6(4):295–307. doi: 10.1053/scnp.2001.27907. [DOI] [PubMed] [Google Scholar]
- 39.Aujard F, Dkhissi-Benyahya O, Fournier I, Claustrat B, Schilling A, Cooper HM, Perret M. Artificially accelerated aging by shortened photoperiod alters early gene expression (Fos) in the suprachiasmatic nucleus and sulfatoxymelatonin excretion in a small primate, Microcebus murinus. Neuroscience. 2001;105(2):403–412. doi: 10.1016/s0306-4522(01)00202-0. [DOI] [PubMed] [Google Scholar]
- 40.Minois N. Longevity and aging: beneficial effects of exposure to mild stress. Biogerontology. 2000;1(1):15–29. doi: 10.1023/a:1010085823990. [DOI] [PubMed] [Google Scholar]
- 41.Bliwise DL, King AC, Harris RB. Habitual sleep durations and health in a 50–65 year old population. J Clin Epidemiol. 1994;47(1):35–41. doi: 10.1016/0895-4356(94)90031-0. [DOI] [PubMed] [Google Scholar]
- 42.Ayas NT, White DP, Manson JE, Stampfer MJ, Speizer FE, Malhotra A, Hu FB. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163(2):205–209. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 43.Gottlieb DJ, Redline S, Nieto FJ, Baldwin CM, Newman AB, Resnick HE, Punjabi NM. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. Sleep. 2006;29(8):1009–1014. doi: 10.1093/sleep/29.8.1009. [DOI] [PubMed] [Google Scholar]
- 44.Glaser JH, Glaser SK. To sleep, perchance to increase the risk of coronary events. Arch Intern Med. 2003;163(11):1374. doi: 10.1001/archinte.163.11.1374-c. [DOI] [PubMed] [Google Scholar]
- 45.Teno JM, Weitzen S, Fennell ML, Mor V. Dying trajectory in the last year of life: does cancer trajectory fit other diseases? J Palliative Med. 2001;4:457–464. doi: 10.1089/109662101753381593. [DOI] [PubMed] [Google Scholar]
- 46.Moore LM, Jenkins M, Barker L. Relation of number of hours of sleep to muscular efficiency. Am J Physiol. 1922;59:471. [Google Scholar]
- 47.Barry H, Bousfield WA. A quantitative determination of euphoria and its relation to sleep. J Abn Soc Psychol. 1935;119:385–389. [Google Scholar]
- 48.Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;29(7):881–889. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kronholm E, Harma M, Hublin C, Aro AR, Partonen T. Self-reported sleep duration in Finnish general population. J Sleep Res. 2006;15(3):276–290. doi: 10.1111/j.1365-2869.2006.00543.x. [DOI] [PubMed] [Google Scholar]
- 50.Steptoe A, Peacey V, Wardle J. Sleep duration and health in young adults. Arch Intern Med. 2006;166(16):1689–1692. doi: 10.1001/archinte.166.16.1689. [DOI] [PubMed] [Google Scholar]
- 51.Pinheiro SP, Schernhammer ES, Tworoger SS, Michels KB. A prospective study on habitual duration of sleep and incidence of breast cancer in a large cohort of women. Cancer Res. 2006;66(10):5521–5525. doi: 10.1158/0008-5472.CAN-05-4652. [DOI] [PubMed] [Google Scholar]
- 52.Pilcher JJ, Ginter DR, Sadowsky B. Sleep quality versus sleep quantity: relationships between sleep and measures of health, well-being and sleepiness in college students. J Psychosom Res. 1997;42(6):583–596. doi: 10.1016/s0022-3999(97)00004-4. [DOI] [PubMed] [Google Scholar]
- 53.Pilcher JJ, Schoeling SE, Prosansky CM. Self-report sleep habits as predictors of subjective sleepiness. Behav Med. 2000;25(4):161–168. doi: 10.1080/08964280009595745. [DOI] [PubMed] [Google Scholar]
- 54.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS Med. 2004;1(3):e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yaggi HK, Araujo AB, McKinlay JB. Sleep duration as a risk factor for the development of type 2 diabetes. Diabetes Care. 2006;29(3):657–661. doi: 10.2337/diacare.29.03.06.dc05-0879. [DOI] [PubMed] [Google Scholar]
- 56.Motohashi Y, Higuchi S, Ahara M, Kaneko Y. Sleep time and working conditions of office workers. Sleep Bio Rhyt hms. 2003;1(2):131–132. [Google Scholar]
- 57.Hicks RA, McTighe S, Juarez M. Sleep duration and eating behaviors of college students. Percept Mot Skills. 1986;62(1):25–26. doi: 10.2466/pms.1986.62.1.25. [DOI] [PubMed] [Google Scholar]
- 58.Spiegel K, Tasali E, Penev P, Van Cauter E. Brief communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. Ann Intern Med. 2004;141(11):846–850. doi: 10.7326/0003-4819-141-11-200412070-00008. [DOI] [PubMed] [Google Scholar]
- 59.Kohatsu ND, Tsai R, Young T, Vangilder R, Burmeister LF, Stromquist AM, Merchant JA. Sleep duration and body mass index in a rural population. Arch Intern Med. 2006;166(16):1701–1705. doi: 10.1001/archinte.166.16.1701. [DOI] [PubMed] [Google Scholar]
- 60.Grandner MA, Kripke DF, Langer RD. Correlations among dietary nutrient variables and subjective and objective sleep. Sleep. 2005;28(S2):A148–A149. [Google Scholar]
- 61.Ohayon MM. Interactions between sleep normative data and sociocultural characteristics in the elderly. J Psychosom Res. 2004;56(5):479–486. doi: 10.1016/j.psychores.2004.04.365. [DOI] [PubMed] [Google Scholar]
- 62.Aschoff J. Human perception of short and long time intervals: its correlation with body temperature and the duration of wake time. J Biol Rhythms. 1998;13(5):437–442. doi: 10.1177/074873098129000264. [DOI] [PubMed] [Google Scholar]
- 63.Taub JM. Behavioral and psychological correlates of a difference in chronic sleep duration. Biol Psychol. 1977;5(1):29–45. doi: 10.1016/0301-0511(77)90027-8. [DOI] [PubMed] [Google Scholar]
- 64.Benoit O, Foret J, Bouard G. The time course of slow wave sleep and REM sleep in habitual long and short sleepers: effect of prior wakefulness. Hum Neurobiol. 1983;2(2):91–96. [PubMed] [Google Scholar]
- 65.Czeisler CA, Zimmerman JC, Ronda JM, Moore-Ede MC, Weitzman ED. Timing of REM sleep is coupled to the circadian rhythm of body temperature in man. Sleep. 1980;2(3):329–346. [PubMed] [Google Scholar]
- 66.Aeschbach D, Cajochen C, Landolt H, Borbely AA. Homeostatic sleep regulation in habitual short sleepers and long sleepers. Am J Physiol. 1996;270(1 Pt 2):R41–R53. doi: 10.1152/ajpregu.1996.270.1.R41. [DOI] [PubMed] [Google Scholar]
- 67.Aeschbach D, Postolache TT, Sher L, Matthews JR, Jackson MA, Wehr TA. Evidence from the waking electroencephalogram that short sleepers live under higher homeostatic sleep pressure than long sleepers. Neuroscience. 2001;102(3):493–502. doi: 10.1016/s0306-4522(00)00518-2. [DOI] [PubMed] [Google Scholar]
- 68.Aeschbach D, Sher L, Postolache TT, Matthews JR, Jackson MA, Wehr TA. A longer biological night in long sleepers than in short sleepers. J Clin Endocrinol Metab. 2003;88(1):26–30. doi: 10.1210/jc.2002-020827. [DOI] [PubMed] [Google Scholar]
- 69.Roth T, Stubbs C, Walsh JK. Ramelteon (TAK-375), a selective MT1/MT2-receptor agonist, reduces latency to persistent sleep in a model of transient insomnia related to a novel sleep environment. Sleep. 2005;28(3):303–307. [PubMed] [Google Scholar]
- 70.Paine SJ, Gander PH, Travier N. The epidemiology of morningness/eveningness: influence of age, gender, ethnicity, and socioeconomic factors in adults (30–49 years) J Biol Rhythms. 2006;21(1):68–76. doi: 10.1177/0748730405283154. [DOI] [PubMed] [Google Scholar]
- 71.Taillard J, Philip P, Bioulac B. Morningness/eveningness and the need for sleep. J Sleep Res. 1999;8(4):291–295. doi: 10.1046/j.1365-2869.1999.00176.x. [DOI] [PubMed] [Google Scholar]
- 72.Vera-Villarroel PE, Sanchez AI, Rivera I, Buela-Casal G. Sleep pattern and daytime differences in the electromyographic activity and peripheral temperature. Int J Psychophysiol. 2001;41(2):181–186. doi: 10.1016/s0167-8760(01)00126-x. [DOI] [PubMed] [Google Scholar]
- 73.Opp MR. Sleep and psychoneuroimmunology. Neurol Clin. 2006;24(3):493–506. doi: 10.1016/j.ncl.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 74.Benca RM, Obermeyer WH, Thisted RA, Gillin JC. Sleep and psychiatric disorders: A meta-analysis. Archives of General Psychiatry. 1992;49:651–668. doi: 10.1001/archpsyc.1992.01820080059010. [DOI] [PubMed] [Google Scholar]
- 75.Beck U, Marquetand D. Effects of selective sleep deprivation on sleep-linked prolactin and growth hormone secretion. Arch Psychiatr Nervenkr. 1976;223(1):35–44. doi: 10.1007/BF00367451. [DOI] [PubMed] [Google Scholar]
- 76.Astrom C, Lindholm J. Growth hormone-deficient young adults have decreased deep sleep. Neuroendocrinology. 1990;51(1):82–84. doi: 10.1159/000125320. [DOI] [PubMed] [Google Scholar]
- 77.Kripke DF, Brunner R, Freeman R, et al. Sleep complaints of postmenopausal women. Clin J Women’s Health. 2001;1:2–252. doi: 10.1053/cjwh.2001.30491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Hicks RA, Youmans K. The sleep-promoting behaviors of habitual short-and longer-sleeping adults. Percept Mot Skills. 1989;69(1):145–146. doi: 10.2466/pms.1989.69.1.145. [DOI] [PubMed] [Google Scholar]
- 79.Roehrs T, Roth T. Sleep, sleepiness, sleep disorders and alcohol use and abuse. Sleep Med Rev. 2001;5(4):287–297. doi: 10.1053/smrv.2001.0162. [DOI] [PubMed] [Google Scholar]
- 80.Hartmann E, Baekeland F, Zwilling G, Hoy P. Sleep need: how much sleep and what kind? Am J Psychiatry. 1971;127(8):1001–1008. doi: 10.1176/ajp.127.8.1001. [DOI] [PubMed] [Google Scholar]
- 81.Taub JM. Dream recall and content in long and short sleepers. Percept Mot Skills. 1972;35(1):267–270. doi: 10.2466/pms.1972.35.1.267. [DOI] [PubMed] [Google Scholar]
- 82.Hartmann E. Sleep requirement: long sleepers, short sleepers, variable sleepers, and insomniacs. Psychosomatics. 1973;14(2):95–103. doi: 10.1016/S0033-3182(73)71362-1. [DOI] [PubMed] [Google Scholar]
- 83.Hicks RA, Pellegrini RJ. Locus of control in short and long sleepers. Percept Mot Skills. 1978;47(3 Pt 2):1337–1338. doi: 10.2466/pms.1978.47.3f.1337. [DOI] [PubMed] [Google Scholar]
- 84.Kumar A, Vaidya AK. Locus of control in short and long sleepers. Br J Psychiatry. 1986;148:739–740. doi: 10.1192/bjp.148.6.739. [DOI] [PubMed] [Google Scholar]
- 85.Hicks RA, Marical CM, Conti PA. Coping with a major stressor: differences between habitual short- and longer-sleepers. Percept Mot Skills. 1991;72(2):631–636. doi: 10.2466/pms.1991.72.2.631. [DOI] [PubMed] [Google Scholar]
- 86.Hicks RA, Picchioni D. Fluctuations in sleep duration are correlated with salience of stressful experience. Percept Mot Skills. 2003;96(3 Pt 2):1139–1140. doi: 10.2466/pms.2003.96.3c.1139. [DOI] [PubMed] [Google Scholar]
- 87.Sexton-Radek K. Stress triggers of long, short, and variable sleep patterns. Percept Mot Skills. 1998;87(1):225–226. doi: 10.2466/pms.1998.87.1.225. [DOI] [PubMed] [Google Scholar]
- 88.Kumar A, Vaidya AK. Anxiety as a personality dimension of short and long sleepers. J Clin Psychol. 1984;1940(1):197–198. doi: 10.1002/1097-4679(198401)40:1<197::aid-jclp2270400137>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- 89.Monk TH, Buysse DJ, Welsh DK, Kennedy KS, Rose LR. A sleep diary and questionnaire study of naturally short sleepers. J Sleep Res. 2001;10(3):173–179. doi: 10.1046/j.1365-2869.2001.00254.x. [DOI] [PubMed] [Google Scholar]
- 90.Hartmann E, Brewer V. When is more or less sleep required? A study of variable sleepers. Compr Psychiatry. 1976;17(2):275–284. doi: 10.1016/0010-440x(76)90001-8. [DOI] [PubMed] [Google Scholar]
- 91.Hicks RA, Garcia ER. Level of stress and sleep duration. Percept Mot Skills. 1987;64(1):44–46. doi: 10.2466/pms.1987.64.1.44. [DOI] [PubMed] [Google Scholar]
- 92.Sanford LD, Yang L, Tang X. Influence of contextual fear on sleep in mice: a strain comparison. Sleep. 2003;26(5):527–540. doi: 10.1093/sleep/26.5.527. [DOI] [PubMed] [Google Scholar]
- 93.Gonzalez MM, Debilly G, Valatx JL, Jouvet M. Sleep increase after immobilization stress: role of the noradrenergic locus coeruleus system in the rat. Neurosci Lett. 1995;202(1–2):5–8. doi: 10.1016/0304-3940(95)12209-5. [DOI] [PubMed] [Google Scholar]
- 94.Wehr TA. The durations of human melatonin secretion and sleep respond to changes in daylength (photoperiod) J Clin Endocrinol Metab. 1991;73(6):1276–1280. doi: 10.1210/jcem-73-6-1276. [DOI] [PubMed] [Google Scholar]
- 95.Globus GG. A syndrome associated with sleeping late. Psychosom Med. 1969;31(6):528–535. doi: 10.1097/00006842-196911000-00006. [DOI] [PubMed] [Google Scholar]
- 96.Taub JM, Globus GG, Phoebus E, Drury R. Extended sleep and performance. Nature. 1971;233(5315):142–143. doi: 10.1038/233142a0. [DOI] [PubMed] [Google Scholar]
- 97.Roehrs T, Shore E, Papineau K, Rosenthal L, Roth T. A two-week sleep extension in sleepy normals. Sleep. 1996;19(7):576–582. [PubMed] [Google Scholar]
- 98.Klerman E, Dijk DJ. Interi ndividual variation in sleep duration and its association with sleep debt in young adults. Sleep. 2005;28(10):1253–1259. doi: 10.1093/sleep/28.10.1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Levine B, Lumley M, Roehrs T, Zorick F, Roth T. The effects of acute sleep restriction and extension on sleep efficiency. Int J Neurosci. 1988;43:139–143. doi: 10.3109/00207458808986162. [DOI] [PubMed] [Google Scholar]
- 100.Ancoli-Israel S, Parker L, Sinaee R, Fell RL, Kripke DF. Sleep fragmentation in patients from a nursing home. J Gerontol. 1989;44(1):M18–M21. doi: 10.1093/geronj/44.1.m18. [DOI] [PubMed] [Google Scholar]
- 101.Ievers-Lanids CE, Redline S. Pediatric Sleep Apnea: Implications of the Epidemic of Childhood Overweight. Am J Respir Crit Care Med. doi: 10.1164/rccm.200606-790PP. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Blunden SL, Beebe DW. The contribution of intermittent hypoxia, sleep debt and sleep disruption to daytime performance deficits in children: consideration of respiratory and non-respiratory sleep disorders. Sleep Med Rev. 2006;10(2):109–118. doi: 10.1016/j.smrv.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 103.Sampei M, Dakeishi M, Wood DC, Murata K. Impact of total sleep duration on blood pressure in preschool children. Biomed Res. 2006;27(3):111–115. doi: 10.2220/biomedres.27.111. [DOI] [PubMed] [Google Scholar]
- 104.Gaina A, Sekine M, Kanayama H, Takashi Y, Hu L, Sengoku K, Kagamimori S. Morning-evening preference: sleep pattern spectrum and lifestyle habits among Japanese junior high school pupils. Chronobiol Int. 2006;23(3):607–621. doi: 10.1080/07420520600650646. [DOI] [PubMed] [Google Scholar]
- 105.Giannotti F, Cortesi F, Sebastiani T, Ottaviano S. Circadian preference, sleep and daytime behaviour in adolescence. J Sleep Res. 2002;11(3):191–199. doi: 10.1046/j.1365-2869.2002.00302.x. [DOI] [PubMed] [Google Scholar]