Abstract
Background
Exposure to stress is potentially important in the pathway to alcohol use and alcohol use disorders. Stressors occur at multiple time points across the life course, with varying degrees of chronicity and severity.
Method
We review evidence from epidemiologic studies on the relationship between four different stressors (fateful/catastrophic events, child maltreatment, common adult stressful life events in interpersonal, occupational, financial, and legal domains, and minority stress) and alcohol consumption and alcohol use disorders.
Results
Studies generally demonstrate an increase in alcohol consumption in response to exposure to terrorism or other disasters. Research has demonstrated little increase in incident alcohol use disorders, but individuals with a history of alcohol use disorders are more likely to report drinking to cope with the traumatic event. Childhood maltreatment is a consistent risk factor for early onset of drinking in adolescence and adult alcohol use disorders, and accumulating evidence suggests that specific polymorphisms may interact with child maltreatment to increase risk for alcohol consumption and disorder. Stressful life events such as divorce and job loss increase the risk of alcohol disorders, but epidemiologic consensus on the specificity of these associations across gender has not been reached. Finally, both perceptions of discrimination and objective indicators of discrimination are associated with alcohol use and alcohol use disorders among racial/ethnic and sexual minorities.
Conclusion
Taken together, these literatures demonstrate that exposure to stress is an important component in individual differences in risk for alcohol consumption and alcohol use disorders. However, many areas of this research remain to be studied, including greater attention to the role of various stressors in the course of alcohol use disorders and potential risk moderators when individuals are exposed to stressors.
Keywords: Alcohol, Stress
Exposure to stress in varying forms is an integral life experience that can provoke a variety of reactions. The last four decades have seen grseat growth in knowledge concerning the relationship between exposure to stressful life events and various types of psychopathology, including alcohol-related outcomes. Despite the accumulated research findings, however, many questions remain. To inform the development of effective prevention and treatments, investigators across disciplines, including epidemiologists, are involved in research to better understand the connection between stress and alcohol consumption, abuse, and dependence.
In psychiatric and substance abuse research, the term “stress” is often understood to indicate an experience denoting adversity (Dohrenwend 2000). Stress exposures consist of external stimuli that are threatening or harmful, that elicit fear, anxiety, anger, excitement, and/or sadness, and that are negative in impact and outcome (Sinha 2001;2008). As has been noted (Lazarus 1999; Levine 2005; McEwen 2007; Selye 1976; Sinha 2008), mild to moderate levels of stress can present challenges that are within the capabilities of an individual to overcome, producing a sense of mastery and accomplishment that eventually result in a positive outcome. However, adverse experiences that exceed the coping abilities of the individual increase the risk for psychopathology.
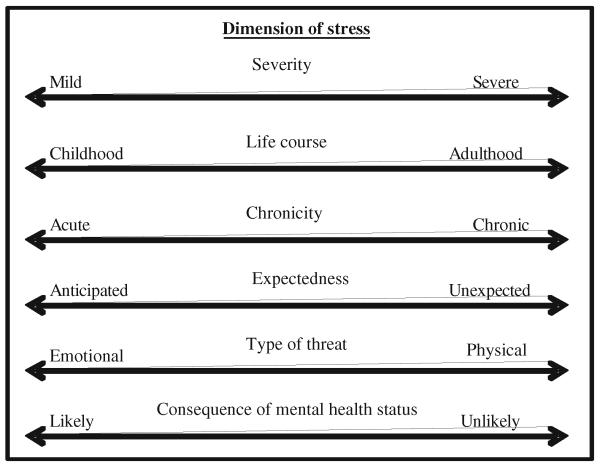
Just as individuals vary in their capabilities, stress exposures can be viewed as varying across several dimensions. Shown in Fig. 1 is an array of dimensions upon which stressful exposures can be conceptualized. One dimension is severity, which can range from the mild, e.g., the daily hassles of family and job among healthy individuals whose basic needs are met, to the severe, e.g., extreme adversity that threatens the life, physical integrity, health and home of oneself and one’s loved ones. Other dimensions, not necessarily orthogonal to each other, include whether the stressor occurred during childhood or maturity, the degree to which the stressor is acute or chronic, expected or unexpected, emotional or physical threat, and the difficulty of discerning whether the stressor was the cause or consequence of the health outcome under consideration.
Fig 1.
Dimensions of stressful experiences
When excess or pathological drinking is the health outcome of interest in epidemiologic research on stress, some aspects of the research context are useful to keep in mind. First, most research on stress and alcohol has been conducted in developed countries where alcohol is widely available and its consumption generally normative. In general population samples in these contexts, alcohol consumption is common (Keyes et al. 2008), as are alcohol use disorders (Hasin et al. 2007b), defined as maladaptive patterns of drinking associated with impaired control that affect major life domains such as health, interpersonal, and socio-occupational functioning. Second, unlike research on stress responses such as post-traumatic stress disorder or depression, research on stress and alcohol involves access to an exogenous substance. Thus, an individual must have access to alcohol and in most cases have the means to purchase alcohol in order for alcohol consumption to be an option as a stress response.
In this review, we consider the epidemiologic evidence for a relationship between stress and alcohol outcomes, including alcohol consumption, problem drinking, and alcohol use disorders as defined in DSM-IV. We focus on the epidemiologic evidence for a relationship between alcohol outcomes in response to four types of stressful experiences: (1) fateful/catastrophic events, (2) child maltreatment, (3) common adult stressful life events in interpersonal, occupational, financial, and legal domains, and (4) minority stress. These four types of stressors all have a considerable body of literature, and exemplify life stressors that vary across a number of the dimensions listed in Fig. 1. To be included in this review, studies must have included a defined measure of exposure to these stressors. As much as possible, we focus the review on studies with large, representative samples since these are most likely to produce clearly interpretable results. Recent reviews have elucidated the literature on biomarkers that indicate the mechanisms through which stress has an effect on substance use from animal and clinical human studies (Koob 2006; Sinha 2008); in this review, we focus on epidemiologic data for the overall effect of stress on alcohol use in non-treated human populations. We divide our review of each class of stressful experiences into three sections: first, we review the placement of each category of stressor along the dimensions described in Fig. 1; second, we describe methodological issues in terms of both measurement and study design in epidemiologic studies of each stressor; and third, we describe major epidemiologic findings regarding the relationship between each stressor and alcohol consumption as well as alcohol use disorders and highlight important directions for future research.
Part I. The relation between fateful/catastrophic events and alcohol use disorders
Considering the various correlated dimensions of stress in human populations described in Fig. 1, fateful/catastrophic events such as direct exposure to disaster and/or terrorism typically lies on the more extreme end of the severity continuum. These stressors are usually acute, unexpected, and exposure is very unlikely to result from an individual’s alcohol consumption. Fateful/catastrophic events can involve both physical threat to one’s life and emotional threat (e.g., knowing someone lost or killed in the fateful/catastrophic incident, fear of additional exposures), and are generally not limited to a particular point in the life course.
Methodological issues in the study of fateful/catastrophic events
Exposure to natural and man-made disasters including terrorism is unlikely to be caused by having an alcohol use disorder, a limitation in the study of other adult stressful exposures. Thus these exposures are often considered “fateful” (Dohrenwend 2000; Dohrenwend et al. 1978; Hasin et al. 2007a; Schiff et al. 2007), creating a quasiexperimental design. In the quasi-experimental design, individuals who are exposed to a disaster should be comparable to individuals who are not exposed on all other factors associated with alcohol consumption and alcohol use disorders. Such designs make causal inference concerning the relationship between exposure and outcome much stronger (Glymour 2006). However, interpretation may depend on the specific circumstances of the event. For example, studies of exposure to nightclub disasters (fires and terrorist attacks; Kennedy et al. 2005; Mahoney et al. 2005) involve individuals who are younger and more likely to consume alcohol than the general population. The study of such events may still provide important information, but the type of individuals involved and the appropriate control group must be considered carefully. Also, some exposures that could be viewed as fateful (e.g., traumatic experiences during combat) are non-random, given evidence that joining the military and volunteering for combat are partly heritable(Lyons et al. 1993) and may be related to traits that are also related to alcohol outcomes, such as risk-taking and sensation-seeking.
Substantive findings regarding the relationship between fateful/catastrophic events and alcohol
Studies of alcohol consumption in response to disaster
Both in the USA and internationally, many studies have addressed the relationship between different types of natural and man-made disaster and alcohol consumption. These have included studies of natural disasters such as exposure to flood (North et al. 2004), volcano (Adams and Adams 1984), earthquakes (Shimizu et al. 2000), and hurricanes (Cerda et al. 2011; Kohn et al. 2005). Studies have also addressed man-made disasters such as exposure to mass shootings (North et al. 1994; Smith et al. 1999), fire/exposure to grotesque death (Green et al. 1985; Reijneveld et al. 2003; Sims and Sims 1998), ferry disaster (Joseph et al. 1993), and nuclear accidents (Kasl et al. 1981). In studies whose timeframe is a year or less, these studies consistently indicate post-disaster increases in alcohol consumption (Joseph et al. 1993; Kasl et al. 1981; Kohn et al. 2005; Reijneveld et al. 2003; Sims and Sims 1998; Smith et al. 1999). Studies with multiple and/or longer follow-ups generally find attenuation of this relationship over time (Joseph et al. 1993).
A number of studies have also addressed alcohol consumption in response to exposure to terrorism. Substantial research on mental health generally and alcohol consumption specifically has been conducted after the terrorist attacks on the World Trade Center in New York and the Pentagon in Washington D.C. on September 11, 2001 (“9/11”), indicating that alcohol consumption generally increased in both New York City and elsewhere in the short term following the attacks. Increased alcohol use was found among the following groups: survivors of the attack on the Pentagon (Grieger et al. 2003); residents of Manhattan in the 1 and/or 6 months following the attack (Ho et al. 2002; Vlahov et al. 2004; Vlahov et al. 2002); residents in the tri-state area of Connecticut, New York, and New Jersey (Melnik et al. 2002); and adults from a nationally representative sample (Stein et al. 2004). Longer-term studies show increased alcohol consumption 1 and 2 years later among New Yorkers at greater exposure levels to the attack (Boscarino et al. 2006). Few studies examined alcohol and terrorism exposure outside the USA, but two studies of adolescents in different cities in Israel showed that geographic proximity to terrorist attacks was associated with greater quantity, frequency and binge drinking (Schiff et al. 2006, 2007). A recent meta-analysis of 27 studies assessing substance use in response to terrorism included studies whose follow-up times ranged from 1 week to more than 2 years (DiMaggio et al. 2009). This meta-analysis found a pooled effect indicating that the population level of alcohol consumption is increased following a terrorist attack (DiMaggio et al. 2009).
The studies noted above are limited by lack of ability to control for pre-disaster alcohol consumption or alcohol use disorders measured before the attack. Three studies that overcame this limitation documented an increase in alcohol consumption following exposure to disaster independent of alcohol consumption levels measured prior to the exposure (Cerda et al. 2011; Hasin et al. 2007a; Richman et al. 2004). For example, among community heavy drinkers in New Jersey who were assessed in detail at two times points before 9/11/01, participants within five miles of the World Trade Center at the time of the 9/11 attack had significantly higher levels of alcohol consumption in the subsequent 3 months than participants who were further away, even after controlling for pre-9/11 alcohol disorders (Hasin et al. 2007a). Work is underway to better understand cognitive factors associated with post-9/11 drinking in this sample (Beseler et al. 2011). Thus, the available evidence indicates that the population level of alcohol consumption increased following 9/11, at least over several months, with some evidence for longer-term increases in alcohol consumption among individuals with high exposure levels.
Studies of problem drinking in response to disaster
The research described above focuses on any alcohol consumption after disaster. Studies of alcohol use disorders and problem drinking following major disasters have been less consistent. Following the Oklahoma City bombings in 1995, North et al. reported no increase in incident alcohol use disorders, either in survivors of the attack (North et al. 1999) or rescue workers (North et al. 2002). Survivors of other disasters such as Hurricane Andrew (David et al. 1996), flooding (Green et al. 1992; North et al. 2004), jet crash (Smith et al. 1990), a combined sample of survivors from Oklahoma City terrorist bombings as well as the Nairobi bombing (North et al. 2005) also showed no evidence of incident alcohol use disorders. After 9/11, neither living near the attack site nor knowing someone lost or killed was associated with incident alcohol problems 6 months following the attack (Vlahov et al. 2006), and exposure to 9/11 was not associated with the trajectory of alcohol use and binge drinking in the 3 years following the attack (Cerda et al. 2008). In a recent pooled analysis of data from 10 different disasters including exposure to flooding, shootings, and plane crashes, North et al. again reported no evidence of increased risk for incident alcohol use disorders after these events (North et al. 2010). However, individuals with pre-existing alcohol disorders were more likely to report increased drinking after these events (North et al. 2010).
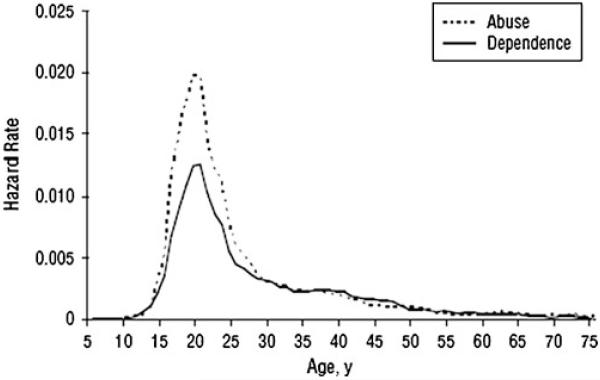
Several studies contradict the above evidence, however. Evidence from survivors of Hurricane Katrina indicates elevated rates of alcohol problems compared to national and local pre-disaster averages (Flory et al. 2009), and increases in binge drinking were found among those most exposed to the hurricane, controlling for pre-hurricane alcohol use (Cerda et al. 2011). Among New Yorkers interviewed 1 and 2 years after 9/11, greater exposure levels predicted binge drinking at 1 but not 2 years, and an increase in alcohol dependence at both time points (Boscarino et al. 2006). Further, 7 months after the Mount St. Helens volcano eruption, alcohol center referrals and liquor law violations had increased compared to the preeruption period (Adams and Adams 1984). Survivors of the Beverly Hills Supper Club fire appeared to have an increase in alcohol abuse more than 2 years after the fire (Green et al. 1985). Thus, the literature is inconsistent on the role of fateful traumatic events in the development of alcohol disorders. Note that studies of incident alcohol use disorders after major disasters were conducted in adult populations, wherein the risk for an incident alcohol use disorder is low (Hasin et al. 2007b). As shown in Fig. 2, the hazard rates for the age of onset of alcohol abuse and dependence in the general population (Hasin et al. 2007b) are highest in the late teens and early 20s, and negligible after age 30. Since early-onset drinking is strongly and consistently related to the risk for later alcohol use disorders (Grant and Dawson 1997), studies of incident alcohol use disorder risk following exposure to disaster in adolescent and young adult populations are necessary to comprehensively understand the relation between disaster and alcohol use disorders.
Fig 2.
Hazard rates for age of onset of DSM-IV alcohol abuse and dependence. Reprinted from Hasin et al. (2007b)
Taken together, there remain questions about the role of traumatic event exposure in alcohol consumption and the development of alcohol use disorders. Accumulating evidence suggests increases in alcohol consumption in the short term following exposure to trauma even among individuals with no history of alcohol use disorders, but there is less consistent evidence on the duration of this relationship at the population level. Few incident alcohol use disorders occur in response to traumatic events among adults. However, individuals with pre-existing or past alcohol use disorders may be more likely to experience relapse to problematic drinking or alcohol use disorders after trauma exposure. Such relapses may carry as much personal and societal burden as incident disorders. Thus, public health efforts following disasters should include assessment and proper referral of individuals at risk for post-disaster problematic drinking.
Part II. The relation between child maltreatment and alcohol use disorders
Childhood maltreatment includes many adverse exposures (sexual, emotional and physical abuse, emotional or physical neglect) during the first 18 years of life. Considering the various correlated dimensions of stress in human populations described in Fig. 1, childhood maltreatment experiences range from mild (e.g., occasionally saying hurtful things) to severe (e.g., chronic physical and/or sexual abuse). Further, these stressors can be acute but are often chronic throughout childhood, and are implausibly a consequence of alcohol consumption as they typically occur before drinking initiation. Childhood maltreatment can involve both physical threat (e.g., physical and sexual child abuse, physical neglect of needs) and emotional threat (e.g., emotional abuse and neglect). These experiences are common, and may account for a significant proportion of all adult psychopathology (Afifi et al. 2008; Green et al. 2010). Further, events frequently co-occur (Dong et al. 2004; Dube et al. 2002; Edwards et al. 2003; Finkelhor et al. 2007), such that exposure to one type of childhood maltreatment increases the risk of exposure to others.
Methodological issues in the study of child maltreatment
Concerning measurement, most studies use retrospective reporting of adverse childhood events among adults to determine exposure status as this is the most feasible means for data collection (Green et al. 2010; Hardt and Rutter 2004). However, several studies have used court and social service records as the exposure measurement (Kaufman et al. 2007; Thornberry et al. 2001; Widom et al. 1995,2007b). Child abuse self-reports, including childhood sexual abuse, are unstable over time (Fergusson et al. 2000; Johnson et al. 1999; Maughan and Rutter 1997; Widom 1996,1997; Widom et al. 1999). Reporting instability appears related to several factors, including the context, salience, and severity of the event(s), closeness to the perpetrator, time since the event(s) occurred, and social desirability in the context of the interview (Hardt and Rutter 2004; Widom 1996;1997). Available evidence from longitudinal data with multiple assessments of maltreatment and latent class analyses of report status (Fergusson et al. 2000) and comparison between court records and self-report (Widom 1996, 1997) indicate that few reports are false positives, indicating that the main result of unstable reporting is likely to be underestimation of the prevalence of adverse childhood events which could weaken but not bias apparent associations. Further, evidence from the Christchurch Health and Development study showed that underestimation is unrelated to psychiatric diagnosis at the time of the interview, and that relative risks for the association between childhood maltreatment and alcohol use disorders remained stable when maltreatment was assessed at multiple time points (Fergusson et al. 2000). Thus, the associations between maltreatment and alcohol use are unlikely to be fully explained by biased retrospective reporting.
Substantive findings regarding the relationship between child maltreatment and alcohol consumption and disorders
Epidemiologic studies addressing the role of adverse childhood events on alcohol consumption and alcohol use disorders have employed several types of designs, including cross-sectional studies of adults with retrospective assessment of adverse childhood events, prospective cohort studies, and twin and other genetically informed samples. Studies have generally shown that most forms of child maltreatment are related to higher risk of adolescent alcohol consumption (Bensley et al. 1999; Hussey et al. 2006; Sartor et al. 2007; Thornberry et al. 2001) and adult alcohol consumption and alcohol disorders (Anda et al. 2002; MacMillan et al. 2001; Molnar et al. 2001; Nelson et al. 2006). A review documented that childhood maltreatment and other childhood stressors were associated with earlier onset of adolescent alcohol consumption and with alcohol use disorders in adulthood (Enoch 2010). However, two issues may either confound or modify the apparent relationship between early maltreatment and adult alcohol use disorders: (1) family history or genetic vulnerability to alcohol problems, and (2) comorbid psychopathology.
Family history of alcoholism may confound the relationship between early maltreatment and adult alcohol use disorders because child maltreatment is more likely to occur among children of alcoholics (Gilbert et al. 2009), who may not only engage in harmful parenting practices (Kettinger et al. 2000; Stanger et al. 2004; Suchman et al. 2007,2008) but who may also pass along genes increasing risk of alcohol disorders to their offspring. While studies using animal model overcome this difficulty and suggest extended stress in early life leads to later self-administration of alcohol (Cruz et al. 2008; Miczek et al. 2008), some epidemiologic studies suggest that the relationship between maltreatment and alcohol disorders may be at least partially confounded by family history of alcohol problems. For example, a prospective cohort study of Midwest court-recorded cases of abuse and neglect compared to matched community controls found no remaining association between early abuse and adult DSM-III-R alcohol use disorders after controlling for family history of alcohol problems among men (Widom et al. 1995,2007b), although among women, physical neglect remained associated with alcohol use disorders. A confounding role of family history was also suggested by Sher et al. (1997) in a prospective convenience sample of college freshman. Finally, a population-based longitudinal study of adult female twins concordant for a positive history of sexual abuse indicated no residual association between childhood sexual abuse and alcohol disorders (Bulik et al. 2001).
However, several studies that controlled for family history of alcoholism indicate a persistent relationship between childhood adverse events and adult risk for alcohol use disorders, including parental divorce (Pilowsky et al. 2009; Thompson et al. 2008), and death of a parent or foster home placement (Pilowsky et al. 2009; Kendler et al. 1996). Further, one study documented strong and significantly increased odds of alcohol disorders based on retrospective assessment of childhood sexual abuse among same-sex twins in Australia (Nelson et al. 2002), even after controlling for family background variables including parental alcohol problems. Finally, recent data from a population-based study of twins in Virginia reported that participants who reported any maltreatment were 1.74 times as likely to experience an alcohol use disorder in adulthood; while controlling for family level risk factors substantially attenuated the observed association, a direct effect after control remained (Young-Wolff et al. 2011). Thus, the literature is inconsistent on whether family history of alcohol problems confounds the association of child maltreatment and adult alcohol use disorders, suggesting continued attention to this issue in further studies.
Information about possible modifying effects of genetic vulnerability comes from studies of specific genetic variants. The mapping of the human genome enables investigation of this possible source of variation through analysis of specific genetic polymorphisms. The finding that functional poly-morphisms in the monoamine oxidase A enzyme (Caspi et al. 2002) interact with childhood maltreatment to predict antisocial behavior in adulthood stimulated research on whether this effect generalizes to substance use disorders, but thus far, the findings did not replicate (Young et al. 2006). The serotonin transporter promoter variant, 5-HTTLPR, has been studied in interaction with stressful experiences in a wide variety of psychiatric outcomes in several studies after initial publication of such an interaction result for major depression (Caspi et al. 2003). For example, youth with court-documented maltreatment were at higher risk for early onset alcohol use if they had the heterozygous (s/l) genotype compared to the l/l genotype (Kaufman et al. 2007). In another youth study, the effect of the same heterozygous genotype on increased risk for substance use was attenuated in families providing involved-supportive parenting (Brody et al. 2009a). In an innovative step involving random assignment of the environment, the investigators then randomized at-risk families to an inter-vention designed to increase involved-supportive parenting or a control condition (Brody et al. 2009b). Among those with the heterozygous 5-HTTLPR genotype, children in treated families had less substance use at follow-up compared to children of the control families (Brody et al. 2009b). Taken together, these studies suggest that the risk for later alcohol outcomes is affected by an interaction of stressful early home environments and genetic vulnerability.
Psychiatric comorbidity may also confound the relationship between early maltreatment and alcohol disorders because maltreatment affects multiple psychiatric disorders (Green et al. 2010; Kendler et al. 2000; Kessler et al. 1997; Widom et al. 2007a); and alcohol use disorders are highly co-morbid with other forms of psychopathology (Hasin et al. 2007b). Data from the National Comorbidity Survey indicated that no adverse childhood experiences were associated with alcohol dependence in adulthood once comorbid psychopathology was controlled, although repeated molestation and a physically/verbally aggressive mother were associated with alcohol abuse (Kessler et al. 1997). The propensity to express psychopathology increases with the number of events experienced, and associations are strongest with risk for psychiatric disorders in early adulthood rather than with their persistence (McLaughlin et al. 2010a). Thus, careful examination of the effects of comorbidity is necessary in studies of early stressful exposures and adult outcomes.
These data suggest that the association between childhood maltreatment and adult alcohol use disorders is complex to measure, analyze, and interpret. While many studies document a strong relationship between maltreatment and alcohol use, those studies that control for family history of alcohol problems and/or co-morbid psychopathology find attenuation of the relationship. Genetic epidemiologic findings suggest that genetic vulnerability may interact with rather than confound the association between maltreatment and alcohol disorders; however, suggesting that further investigation of these pathways in genetically informed samples is crucial for advancing this literature.
Part III. The relation between interpersonal, occupational, financial, and legal stressful life events and alcohol use disorders
Stressors in adulthood related to interpersonal relationships, occupation, personal finance, and legal problems can have a profoundly negative impact on mental health (Greeley and Oei 1999). However, these stressful events could as easily be consequences or risk factors of alcohol disorders, creating ambiguity in interpreting associations between these stressors and alcohol outcomes. Compared to other stressors we discuss in this review and considering the dimensions described in Fig. 1, the events described in this section generally lie on the milder end of the severity continuum, though with considerable variability in severity. Further, these stressors are most often acute, although some may be chronic (e.g., unemployment during economic recessions). The events often involve emotional threat (e.g., divorce) but could involve physical threat as well (e.g., being the victim of a violent crime).
Methodological issues in the study of interpersonal, occupational, financial, and legal stressful life events
While the measurement of stressful life events in psychiatric epidemiologic research has been a source of debate for decades (Brown 1993; Dohrenwend 2000,2006; Wheatron 1994), the most commonly used method of measuring interpersonal, occupational, financial, and legal stressful life events is through subjective response in the form of a checklist or inventory. Typically, these questionnaires include 10 to 20 experiences thought to be stressful that are self-reported by the respondent (e.g., Cohen et al. 1983; Dohrenwend et al. 1978; Grant et al. 2004; Holmes and Rahe 1967; Paykel et al. 1971; Sarason et al. 1978). Shown in Box 1 is a list of common interpersonal, occupational, financial, and legal stressors that are often examined in epidemiologic studies, e.g., divorce, death of a relative, and job loss. Research participants indicate whether these experiences happened to them and in what time frame. Test-retest reliability studies of these scales indicate fair reliability (Klein and Rubovits 1987; Rahe et al. 1970; Ruan et al. 2008). As noted by Dohrenwend (2006), however, these scales have a number of problems, including “intracategory variability,” the lack of specific meaning within categories of stressful life events (Dohrenwend 2006). For example, losing a job is often included on stressful life event checklists, but the meaning of the lost job is different for one who experiences a plant shut down after 30 years in the same position compared to an artist or a musician accustomed to temporary work. Similarly, divorce can be devastating to one member of a couple and a relief to the other.
Box 1. Acute stressful life events often used in epidemiologic research of stress and alcohol.
Death or serious illness in a family member and/or close friend
Moved residence
Fired or laid off from job
Major financial crisis, bankruptcy, or problems paying bills
Trouble with boss or coworker
Separation, divorce, or breakup of a romantic relationship
Serious interpersonal problems with a friend, neighbor, or relative
Trouble with police, got arrested or sent to jail
Victim of a violent crime
Additionally, self-reported stressful life events may be subject to biased reporting, as negative events are more likely to be recalled and may be described as more salient when individuals are experiencing a psychiatric disorder (Brown 1989; Dohrenwend et al. 1984; Kihlstrom et al. 2000; Meyer 2003a; Schwarz 2007). Given the issues involved with self-reported stressful life events, some investigators have worked with methods to measure stressful events more objectively, or independently, of the participant’s perceptions or appraisals of the event as stressful by including assessments by independent raters (Dohrenwend 2000; Lazarus 1999; Meyer et al. 2008; Monroe 2008; Wethington et al. 1995). Despite the limitations of subjective self-report measures of stress, however, they capture how individuals respond to, cope with, and adapt to stressful experiences, which might be important for the development of psychiatric disorders (Clark et al. 1999; Williams et al. 2003). Thus, while imperfect, subjective self-reports of stress provide useful information and are thus commonly used in epidemiologic studies.
Further, daily interpersonal stress exposures such as problems at work, trouble with the police, or breakup of romantic relationships are likely to be influenced by having an alcohol disorder. While these exposures are likely to be stressful for anyone experiencing them, they can be as much a consequence of an alcohol use disorder as a cause. Stressful life events often co-occur, and individuals who experience multiple stressful life events may be different than individuals who do not experience such events on an underlying factor that also influences the risk for excess alcohol consumption and alcohol use disorders. For example, stressful experiences and alcohol use disorders are both heritable, and some have suggested a common genetic vulnerability to both of these experiences (Lyons et al. 1993; Sher et al. 2005). Thus, teasing apart the temporal and causal directions of relationships between these adult stressors and alcohol is a difficult task in general population epidemiologic samples. Despite these limitations, research into the effects of these exposures is important from a public health perspective as they are common in the general population.
Substantive findings regarding the relationship between interpersonal, occupational, financial, and legal stressful life events and alcohol
Surprisingly few large-scale epidemiologic studies have examined the association of interpersonal, occupational, financial, and legal stressful life events with alcohol use and disorder. Various studies in small to medium adult community samples have found that counts of perceived stressful life events are associated with alcohol consumption and problem alcohol use (not necessarily alcohol use disorders; Cole et al. 1990; King et al. 2003), though a population-based longitudinal study of older adults (mean age, 61) did not demonstrate long-term effects (i.e., 1 year or greater) of acute stressful life events on patterns of alcohol consumption (Skaff et al. 1999). A national prospective study of 3,006 women found increased risk of alcohol abuse after being an assault victim, and no evidence of reverse causation (that alcohol consumption alone contributed to the risk for assault) (Kilpatrick et al. 1997). Further, in a larger, longitudinal study of college students (N=295) in which reports of stressful events, alcohol, and drugs were reported daily for 2 years on the internet, students homozygous for the s allele of 5-HTTLPR were at substantially increased risk for heavy drinking and drug use if they experienced a high level of stressful life events (Covault et al. 2007). Thus, consistent with studies on gene by environment interaction in early maltreatment and alcohol outcomes, evidence suggests that these relationships may be modified by genetic factors, suggesting value in further studies of this type among varied samples.
Some epidemiologic studies suggest gender differences in the exposure to and effects of acute stressors. Women report more stressful life events than men (Kendler et al. 2001), and the stressful life events commonly reported by men and women differ (Kessler et al. 1985; Sieber 1974). Despite the greater number and different nature of stressful experiences in the lives of women, research has been inconsistent as to whether stressful experiences are more predictive of alcohol disorders in men or women. Smaller community-based samples have demonstrated that the relationship between stressful life events and alcohol consumption is stronger in women than men (Allan and Cooke 1985; King et al. 2003; Rospenda et al. 2008), though men are more likely to report drinking to cope with distress (Nolen-Hoeksema and Harrell 2002) and drinking to relieve tension (Armeli et al. 2000). However, two larger, more representative samples have shown the opposite relationship: stressful life events are more strongly associated with alcohol consumption and alcohol use disorders in men compared to women (Dawson et al. 2005; San José et al. 2000). Data from the National Epidemiologic Survey on Alcohol and Related Conditions found that the number of past-year stressors was associated with alcohol consumption and binge drinking in both men and women, but that the relationship was stronger for men; each additional stressor increased the odds of heavy drinking by 24% (odds ratio for each additional stressor equaled 1.24) in men and 13% (odds ratio for each additional stressor equaled 1.13) in women (Dawson et al. 2005). Further, events such as divorce are consistently associated with an increase in drinking among men, but inconsistently associated with drinking among women. For example, Wilsnack et al. (1991) demonstrated an inverse relationship between divorce and drinking in a nationally representative survey of women (Wilsnack et al. 1991). Finally, several general population studies have found an increase in incident alcohol use disorders following job loss, particularly among men (Catalano et al. 1993; Crawford et al. 1987; Lahelma et al. 1995). Given that this literature remains inconsistent, more data from large-scale studies with bearing on these relationships would be beneficial to advance this literature.
Part IV. The relation between minority stress and alcohol use disorders
Minority stress is defined as exposure to specific stressors that result from minority status, especially prejudice and discrimination events (Meyer 2003b; Williams et al. 2003). These events range from mild (e.g., daily hassles such as being followed in a store) to more severe (e.g., being a victim of a violent crime), and include both emotional (e.g., workplace harassment; Waldo 1999) and physical (e.g., hate crimes; Herek 2009) threats to self. Minority status cannot be attributed to having an alcohol disorder, making one aspect of interpretation straightforward in studies in this area. Although minority stress can involve acute events, it is most frequently viewed as a chronic exposure that occurs across the entire life course (Williams et al. 2003). Finally, as depicted in Fig. 1, stressors vary with respect to whether they are expected. Research has indicated that while many stressors that members of minority groups confront are unanticipated, one consequence of repeated exposure to discrimination is that individuals begin to expect rejection based on their stigmatized identity (Mendoza-Denton et al. 2002).
Methodological issues in the study of minority stress
Two salient methodological points are important in understanding the literature on minority stress and alcohol use. First, studies tend to assess discrimination due to a single aspect (e.g., race or sexual minority status or gender), but individuals have multiple domains of identity, all of which might be important in determining the amount of stress engendered by prejudice and/or discrimination (Meyer 2003b). For example, data from the National Epidemiologic Survey on Alcohol and Related Conditions indicated that among lesbians, gays, and bisexuals (LGBs), the risk of substance use disorders increased as a function of the number of domains in which discrimination was reported (McCabe et al. 2010). Thus, individuals who reported discrimination due to gender, race, and sexual orientation had a higher risk of substance use disorders compared to those who reported discrimination due to sexual orientation alone. Studies exploring the role of multiple identities in shaping the stress response and subsequent health outcomes, including alcohol use and abuse, are important to advance this literature.
Second, almost all studies described in this section use self-report of perceived discrimination experiences to measure exposure to discrimination. Although this research may capture how minority group members construe their experience of discrimination, these measures could be confounded with mental health status (Meyer 2003b), which may lead to biased associations between stress and alcohol use. Consequently, more recent research (discussed below) has attempted to utilize objective, ecologic measures of stress exposure that are outside the control of the individual, such as institutional discrimination (Hatzenbuehler et al. 2010).
Below, we briefly review the research for two specific minority groups: racial/ethnic minorities and sexual minorities (LGBs). While substantial research is available regarding alcohol use disorders among other minority groups (e.g., women, physically disabled, religious minorities), we focus on these two groups as they highlight some of the methodological issues and enduring paradoxes of this work. Although this section considers minority stress as one mechanism explaining alcohol use among racial/ethnic and sexual minority groups, we recognize that there are alternative pathways, such as social disadvantage (e.g., poverty level and cumulative disadvantage; Mulia et al. 2008) and social norms (e.g., Hatzenbuehler et al. 2008).
Racial/ethnic minorities
According to minority stress models, the stress resulting from prejudice and discrimination should lead to elevations in alcohol use among minority group members. Patterns of alcohol use among racial/ethnic minorities, however, fail to correspond to what would be predicted under a straightforward minority stress-psychopathology model. While Native Americans have higher rates of alcohol consumption and alcohol use disorders compared with non-Hispanic Whites (Hasin et al. 2007b), several large surveys indicate lower rates of alcohol consumption and alcohol use disorders among non-Hispanic Blacks, Asians, and Hispanics compared to Whites (Breslau et al. 2006; Hasin et al. 2007b; Kessler et al. 1994). These minority groups also have lower rates of other psychiatric disorders such as major depression, leading to what has been called the ‘minority paradox’ (Williams 2001) in mental health research: minority groups such as Blacks and Hispanics have lower rates of psychiatric and substance disorders despite greater exposure to institutional and interpersonal discrimination which have been shown to engender substantial stress via biological (Lewis et al. 2006) and psychological (Hatzenbuehler 2009) mechanisms. In contrast to findings from the between-group studies, within-group studies consistently show that perceived discrimination is associated with alcohol outcomes, including studies of Blacks (McLaughlin et al. 2010b; Richman et al. 1996; Taylor and Jackson 1990; Yen et al. 1999), Filipino-Americans (Gee et al. 2007), and Asian-American adolescents (Yoo et al. 2010).
Sexual minorities
In contrast to racial/ethnic minorities, LGB individuals have higher rates of substance use and substance use disorders than their heterosexual peers (Garofalo et al. 1998; Russell et al. 2002; Ziyadeh et al. 2007), including among adolescents (Eisenberg and Wechsler 2003; Hatzenbuehler et al. 2008) and adults (Burgard et al. 2005; Cochran et al. 2000; Drabble et al. 2005). Although research has tended to examine perceived discrimination as a risk factor for internalizing psychopathology such as depression and anxiety, recent studies have shown higher levels of alcohol use (Hatzenbuehler et al. 2011) and alcohol use disorders (McCabe et al. 2010) among LGBs who perceive that they have experienced higher levels of discrimination.
Because of the design of these studies, they are not able to rule out reverse causality (i.e., individuals with alcohol problems may perceive and report greater discrimination). In order to address some of these methodological limitations of subjective measures of discrimination, recent studies have developed novel measures for operationalizing objective stressors that LGB individuals confront, including institutional forms of discrimination (e.g., anti-marriage laws, employment discrimination policies). Given that these institutional stressors occur outside the control of LGB individuals, they are not confounded with mental health status and therefore provide a stronger test of the effect of discrimination on mental health than measures of subjective stress. Literature is emerging documenting the relationship between these objective stressors and LGB health, including alcohol use. For example, a recent study examined the impact of state-level ballot initiatives banning gay marriage on the prevalence of psychiatric and substance use disorders in LGB populations (Hatzenbuehler et al. 2010). Results indicated that LGB respondents living in states that passed such bans in 2004 had significantly greater increases in psychiatric and alcohol use disorders than LGB respondents in states that did not pass such bans (Hatzenbuehler et al. 2010). This research demonstrates the potential importance of incorporating more objectively defined indices of social stress into research on alcohol use among minority populations. Indeed, an examination of how and why such social stressors contribute to the development and maintenance of alcohol use disorders within LGB populations represents a crucial avenue for future inquiry.
In sum, despite the fact that both Blacks and LGBs experience multiple minority stressors across the life course, only LGB populations appear to be at increased risk for psychiatric morbidity, including alcohol disorders (Schwartz and Meyer 2010). Studies are needed that explore the underlying reasons that can explain the apparent inconsistencies in the minority stress-alcohol literature. LGBs and racial ethnic minorities differ in multiple respects that might have important consequences for alcohol use, including the availability of social support and develomental timing of when these minority identities become salient. Indeed, some researchers have hypothesized that African-American populations have adopted strong resilience and coping mechanisms to combat minority stress (Clark et al. 1999) that may buffer against the development of substance use, perhaps as a result of racial socialization early in development (Hughes et al. 2006). In support of this hypothesis, a daily diary study of LGB and African-American young adults found that on days in which minority stressors were reported, African-Americans were more likely to engage in some adaptive coping strategies (e. g., seeking out social support) than were LGB respondents (Hatzenbuehler et al. 2009). Another dimension on which these two groups differ is the concealability of the stigma. In contrast to racial/ethnic minority status, sexual minority status is considered more concealable. On the one hand, this concealability might be associated with less discrimination and resulting stress, as individuals can choose when and with whom to reveal a sexual minority status. On the other hand, those with concealed stigmas often experience greater stress than individuals with conspicuous stigmas (Pachankis 2007), perhaps because those with concealed stigmas have fewer opportunities for support from others who share their stigma (Frable et al. 1998). These and other potential explanations warrant further empirical testing.
Implications and prescriptions for future research
While the present review highlights many methodological challenges in conducting epidemiologic research on stress and alcohol, we also demonstrate remarkable consistency in the findings that major life stressors experienced by the general population are associated with increased risk of alcohol consumption and alcohol use disorders. Below we highlight the implications of these findings, and offer seven research areas in need of greater attention by the field of epidemiology.
First, as noted throughout this review, certain types of stressful life events are likely to be a cause as well as a consequence of alcohol consumption and alcohol use disorders. Below we describe several new methods aimed at resolving some of the temporality issues within existing study designs. Propensity analysis aims to mitigate the problem of reverse causation by carefully controlling confounding; these analyses have been applied to depression outcomes (Kendler and Gardner 2010), but have not yet been applied to alcohol outcomes. While propensity analysis deals with confounding issues, few studies have attempted to explore and model the interplay between stress and alcohol use disorders as iterative and dynamic processes. This type of analysis is difficult to conduct in traditional regression frameworks that do not allow for feedback loops and make assumptions about static processes. Dynamic systems models are an approach to modeling the dynamic interplay between stress and alcohol use. These are increasingly utilized by alcohol researchers to more accurately model dynamic processes other than stressful life events in human populations (Galea et al. 2010; Gruenewald and Johnson 2010; Gruenewald et al. 2010; Yu et al. 2009). No systems research has yet attempted to address the role of stress on alcohol consumption over time in the general population, but such research could aid in the etiologic investigation and specific estimation of effects of stressful life events on alcohol consumption, and also estimate the population-expected reduction in alcohol consumption and alcohol use disorders given the prevention of certain stressors. Such information can be useful for public health planning and resource allocation. None of these methods, however, can overcome the limitations of study design. Many of studies cited here are cross-sectionally collected samples with one-time measurement of stress and alcohol; temporality and reciprocality issues can only be resolved with prospective data and multiple time points of measurement.
Second, the literature addressing the interaction of genes and environment is still in early phases and studies are few. In this review, we note that allelic variation in risk genes modifies the relationship of childhood maltreatment or college-age daily stressors and alcohol consumption. Genetic data are increasingly collected in epidemiologic studies, so a greater variety of stressors and genetic variants can be tested in future studies to maximize our understanding of these relationships. In addition to examining biological factors (i.e., genetics) as effect modifiers, future research is also needed to identify biological factors as mediators linking stress to alcohol use and alcohol disorders. There is a growing literature showing that individuals exposed to highly stressful conditions have dysregulated physiological stress response systems (Chen et al. 2010; Evans and Kim 2007). In turn, HPA axis reactivity has been associated with multiple adverse health outcomes, including substance use (Daughters et al. 2009; Sinha 2008; Childs and De Wit 2009). These and other potential biological mechanisms warrant further investigation.
Third, checklists of stressful situations by respondents in epidemiologic surveys are a measurement approach that serves an important function due to their relative ease of administration and low cost. However, given the methodological issues outlined above, studies should utilize multiple measures of stressful life events whenever possible. For example, approaches designed by Brown et al. (Brown et al. 1995a,b) and used in epidemiologic research by Kendler et al. (2003) focus on more nuanced aspects of the stressful experience, categorizing each experience into non-mutually exclusive categories of loss, humiliation, entrapment, and danger. Research has shown differential relationships between each of these dimensions of a stressful experience and psychopathology, thus documentation of the effect of both the events themselves and the psychological dimensions of the events can be documented. Increasingly, researchers in epidemiology have been incorporating objective measures of stressful environments into research on substance use disorders. For example, the study described above using the objectively measured social context of LGBs shows how subjective, possibly biased aspects of stress reporting can be removed from the measure (Hatzenbuehler et al. 2010). Dohrenwend et al. (Dohrenwend 2006; Dohrenwend et al. 1993,1978) advocate the use of independent assessments of respondent reported stressful events; this approach is more timely and costly than respondent-driven checklists of stressful events, but when feasible provides well-validated assessment of stress. Researchers in other health areas have used a transdisciplinary approach to characterizing stress; for example, neighborhood stress has been captured by medical sociologists through observation and systematic recording of events and conditions of neighborhoods (Cohen et al. 2000; Sampson and Raudenbush 1999). Such an approach would be beneficial to add to subjective reports of stress to fully understand the relationships between objective and subjective forms of stress and alcohol.
Fourth, limited research has been conducted on the role of population-level economic recession on alcohol use and alcohol use disorders. A population-based study in Finland indicated that the relationship between job loss and alcohol consumption was greater during economic recessions than periods of economic growth (Luoto et al. 1998). Given the current worldwide economic downturn, the effects of economic stressors at the population-level on individual-level patterns of alcohol consumption and alcohol use disorders remain an important gap in the stress literature.
Fifth, meta-analyses of the effects of stressors on alcohol consumption are difficult to conduct given the wide variation in measurements of stress. However, an accumulation of studies has begun to facilitate this important type of review for exposure to terrorism (DiMaggio et al. 2009). Additional meta-analyses focused on specific types of stress or specific populations would be very useful contributions to summarize the accumulating epidemiologic data on stress and alcohol. Further, meta-analysis would allow for the estimation of pooled effect sizes for many of these exposures; given the large sample sizes reported here and the use of the odds ratio as the most common measure of association, it is possible that effects are statistically although not clinically significant. Studies examining the magnitude of these effects and the potential impact on public health of intervention are necessary.
Sixth, few large-scale epidemiologic studies have assessed the role of stressful life events on the course of alcohol use disorders after initial onset. Stress has primarily been examined as a risk factor for the adult incidence of alcohol disorders. Given that the age of onset sharply peaks in late adolescence and early adulthood (Fig. 2), those with a lifetime tendency to drink heavily or in a problematic manner, including after exposure to trauma, will mainly have already had their lifetime onset prior to adult trauma exposure. For these individuals, the risk for lifetime incidence is not what is clinically important, but rather, the potential for a relapse that might not otherwise have occurred. Clinical samples have documented that patients report stressful life events as a common trigger for relapse (Bottlender and Soyka 2005; Breese et al. 2005; Brown et al. 1990; Brown et al. 1995a,b; Vielva and Iraurgi 2001; Walter et al. 2006). Animal models have established that stress-related reinstatement of alcohol self-administration is possible (Gass and Olive 2007; Mason et al. 2009). However, few epidemiologic studies have addressed stressful events prospectively as a risk factor for exacerbation or relapse of alcohol use disorders in the general population. Given the potential costs of such outcomes (loss of jobs, relationships, and even suicide; Hallberg and Mattsson 1990), we suggest that this issue receive greater attention in studies of post-disaster drinking and other types of stress exposures.
Finally, limited data exist to evaluate the effect of stress engendered by discrimination on the course of alcohol consumption and alcohol use disorders among racial/ethnic minorities. A small study showed that perceived discrimination is associated with an earlier onset of alcohol use among American Indian adolescents (Whitbeck et al. 2001). No published studies have thus far evaluated whether individuals at higher levels of stress due to perceived discrimination are less likely to seek treatment or remit in their alcohol use disorder, and important area for future research.
In conclusion, the psychological and psychiatric effects of stress remain an important mechanism for individual differences in all areas of mental health. We have demonstrated here the substantial evidence for effects on alcohol consumption and alcohol use disorders of fateful/catastrophic events such as exposure to disaster and terrorism, childhood adversities such as maltreatment, interpersonal stressors such as divorce and job loss, and chronic minority stress. While these data demonstrate the importance of stress in the development of alcohol problems in human populations, substantial work remains to be done in these areas. Refined measures of stress exposures, careful assessment of confounding and reverse causation, an examination of alcohol disorder course, including relapse, and the potentiating of stress effects by genetic vulnerability remain important topic areas in need of more epidemiologic study. By exploring the epidemiology of stress in human populations, we can integrate and translate work in experimental human and animal models in order to demonstrate the real world effects of these common yet often devastating exposures.
Acknowledgements
This research was supported in part by grants from the National Institute on Alcoholism and Alcohol Abuse (K05 AA014223, Hasin; U01 AA018111; Hasin), a fellowship from the National Institute of Drug Abuse (F31-DA026689, Keyes), the Robert Wood Johnson Health and Society Scholars program (Hatzenbuehler), and New York State Psychiatric Institute (Hasin). We would like to thank Philip Bender for assistance in manuscript preparation.
Footnotes
The authors report no conflicts of interest.
Contributor Information
Katherine M. Keyes, Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, NY, USA; New York State Psychiatric Institute, Columbia University, 1051 Riverside Drive, Box 123, New York, NY 10032, USA
Mark L. Hatzenbuehler, Center for the Study of Social Inequalities in Health, Mailman School of Public Health, Columbia University, New York, NY, USA
Deborah S. Hasin, Department of Epidemiology, Mailman School of Public Health, Columbia University, New York, NY, USA; New York State Psychiatric Institute, Columbia University, 1051 Riverside Drive, Box 123, New York, NY 10032, USA; Department of Psychiatry, College of Physicians and Surgeons, Columbia University, New York, NY, USA
References
- Adams PR, Adams GR. Mount Saint Helens’s ashfall. Evidence for a disaster stress reaction. Am Psychol. 1984;39:252–260. doi: 10.1037//0003-066x.39.3.252. [DOI] [PubMed] [Google Scholar]
- Afifi TO, Enns MW, Cox BJ, Asmundson GJ, Stein MB, Sareen J. Population attributable fractions of psychiatric disorders and suicide ideation and attempts associated with adverse childhood experiences. Am J Public Health. 2008;98:946–952. doi: 10.2105/AJPH.2007.120253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allan CA, Cooke DJ. Stressful life events and alcohol misuse in women: a critical review. J Stud Alcohol. 1985;46:147–152. doi: 10.15288/jsa.1985.46.147. [DOI] [PubMed] [Google Scholar]
- Anda RF, Whitfield CL, Felitti VJ, Chapman D, Edwards VJ, Dube SR, Williamson DF. Adverse childhood experiences, alcoholic parents, and later risk of alcoholism and depression. Psychiatr Serv. 2002;53:1001–1009. doi: 10.1176/appi.ps.53.8.1001. [DOI] [PubMed] [Google Scholar]
- Armeli S, Carney MA, Tennen H, Affleck G, O’Neil TP. Stress and alcohol use: a daily process examination of the stressor-vulnerability model. J Pers Soc Psychol. 2000;78:979–994. doi: 10.1037//0022-3514.78.5.979. [DOI] [PubMed] [Google Scholar]
- Bensley LS, Spieker SJ, Van Eenwyk J, Schoder J. Self-reported abuse history and adolescent problem behaviors. II. Alcohol and drug use. J Adolesc Health. 1999;24:173–180. doi: 10.1016/s1054-139x(98)00112-8. [DOI] [PubMed] [Google Scholar]
- Beseler CL, Aharonovich E, Hasin D. The enduring influence of drinking motives on alcohol consumption after fateful trauma. Alcohol Clin Exp Res. 2011 doi: 10.1111/j.1530-0277.2010.01431.x. doi:10.1111/j.1530-0277.2010.01431.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino JA, Adams RE, Galea S. Alcohol use in New York after the terrorist attacks: a study of the effects of psychological trauma on drinking behavior. Addict Behav. 2006;31:606–621. doi: 10.1016/j.addbeh.2005.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bottlender M, Soyka M. Outpatient alcoholism treatment: predictors of outcome after 3 years. Drug Alcohol Depend. 2005;80:83–89. doi: 10.1016/j.drugalcdep.2005.03.011. [DOI] [PubMed] [Google Scholar]
- Breese GR, Chu K, Dayas CV, Funk D, Knapp DJ, Koob GF, Le DA, O’Dell LE, Overstreet DH, Roberts AJ, Sinha R, Valdez GR, Weiss F. Stress enhancement of craving during sobriety: a risk for relapse. Alcohol Clin Exp Res. 2005;29:185–195. doi: 10.1097/01.alc.0000153544.83656.3c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau J, Aguilar-Gaxiola S, Kendler KS, Su M, Williams D, Kessler RC. Specifying race-ethnic differences in risk for psychiatric disorder in a USA national sample. Psychol Med. 2006;36:57–68. doi: 10.1017/S0033291705006161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Beach SR, Philibert RA, Chen YF, Lei MK, Murry VM, Brown AC. Parenting moderates a genetic vulnerability factor in longitudinal increases in youths’ substance use. J Consult Clin Psychol. 2009a;77:1–11. doi: 10.1037/a0012996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brody GH, Beach SR, Philibert RA, Chen YF, Murry VM. Prevention effects moderate the association of 5-HTTLPR and youth risk behavior initiation: gene x environment hypotheses tested via a randomized prevention design. Child Dev. 2009b;80:645–661. doi: 10.1111/j.1467-8624.2009.01288.x. [DOI] [PubMed] [Google Scholar]
- Brown GW. Life events and measurement. In: Brown GW, Harris TO, editors. Life events and illness. Free Press; New York: 1989. pp. 3–45. [Google Scholar]
- Brown GW. Life events and affective disorder: replications and limitations. Psychosom Med. 1993;55:248–259. doi: 10.1097/00006842-199305000-00003. [DOI] [PubMed] [Google Scholar]
- Brown SA, Vik PW, McQuaid JR, Patterson TL, Irwin MR, Grant I. Severity of psychosocial stress and outcome of alcoholism treatment. J Abnorm Psychol. 1990;99:344–348. doi: 10.1037//0021-843x.99.4.344. [DOI] [PubMed] [Google Scholar]
- Brown GW, Harris TO, Hepworth C. Loss, humiliation and entrapment among women developing depression: a patient and non-patient comparison. Psychol Med. 1995a;25:7–21. doi: 10.1017/s003329170002804x. [DOI] [PubMed] [Google Scholar]
- Brown SA, Vik PW, Patterson TL, Grant I, Schuckit MA. Stress, vulnerability and adult alcohol relapse. J Stud Alcohol. 1995b;56:538–545. doi: 10.15288/jsa.1995.56.538. [DOI] [PubMed] [Google Scholar]
- Bulik CM, Prescott CA, Kendler KS. Features of childhood sexual abuse and the development of psychiatric and substance use disorders. Br J Psychiatry. 2001;179:444–449. doi: 10.1192/bjp.179.5.444. [DOI] [PubMed] [Google Scholar]
- Burgard SA, Cochran SD, Mays VM. Alcohol and tobacco use patterns among heterosexually and homosexually experienced California women. Drug Alcohol Depend. 2005;77:61–70. doi: 10.1016/j.drugalcdep.2004.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caspi A, McClay J, Moffitt TE, Mill J, Martin J, Craig IW, Taylor A, Poulton R. Role of genotype in the cycle of violence in maltreated children. Science. 2002;297:851–854. doi: 10.1126/science.1072290. [DOI] [PubMed] [Google Scholar]
- Caspi A, Sugden K, Moffitt TE, Taylor A, Craig IW, Harrington H, McClay J, Mill J, Martin J, Braithwaite A, Poulton R. Influence of life stress on depression: moderation by a polymor-phism in the 5-HTT gene. Science. 2003;301:386–389. doi: 10.1126/science.1083968. [DOI] [PubMed] [Google Scholar]
- Catalano R, Dooley D, Wilson G, Hough R. Job loss and alcohol abuse: a test using data from the epidemiologic catchment area project. J Health Soc Behav. 1993;34:215–225. [PubMed] [Google Scholar]
- Cerda M, Vlahov D, Tracy M, Galea S. Alcohol use trajectories among adults in an urban area after a disaster: evidence from a population-based cohort study. Addiction. 2008;103:1296–1307. doi: 10.1111/j.1360-0443.2008.02247.x. [DOI] [PubMed] [Google Scholar]
- Cerda M, Tracy M, Galea S. A prospective population based study of changes in alcohol use and binge drinking after a mass traumatic event. Drug Alcohol Depend. 2011 doi: 10.1016/j.drugalcdep.2010.09.011. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen E, Cohen S, Miller GE. How low socioeconomic status affects 2-year hormonal trajectories in children. Psychol Sci. 2010;21:31–37. doi: 10.1177/0956797609355566. [DOI] [PubMed] [Google Scholar]
- Childs E, De Wit H. Hormonal, cardiovascular, and subjective responses to acute stress in smokers. Psychopharmacology. 2009;203:1–12. doi: 10.1007/s00213-008-1359-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark R, Anderson NB, Clark VR, Williams DR. Racism as a stressor for African Americans. A biopsychosocial model. Am Psychol. 1999;54:805–816. doi: 10.1037//0003-066x.54.10.805. [DOI] [PubMed] [Google Scholar]
- Cochran SD, Keenan C, Schober C, Mays VM. Estimates of alcohol use and clinical treatment needs among homosexually active men and women in the U.S. population. J Consult Clin Psychol. 2000;68:1062–1071. doi: 10.1037//0022-006x.68.6.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- Cohen D, Spear S, Scribner R, Kissinger P, Mason K, Wildgen J. “Broken windows” and the risk of gonorrhea. Am J Public Health. 2000;90:230–236. doi: 10.2105/ajph.90.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole G, Tucker L, Friedman GM. Relationships among measures of alcohol drinking behavior, life-events and perceived stress. Psychol Rep. 1990;67:587–591. doi: 10.2466/pr0.1990.67.2.587. [DOI] [PubMed] [Google Scholar]
- Covault J, Tennen H, Armeli S, Conner TS, Herman AI, Cillessen AH, Kranzler HR. Interactive effects of the serotonin transporter 5-HTTLPR polymorphism and stressful life events on college student drinking and drug use. Biol Psychiatry. 2007;61:609–616. doi: 10.1016/j.biopsych.2006.05.018. [DOI] [PubMed] [Google Scholar]
- Crawford A, Plant MA, Kreitman N, Latcham RW. Unem-ployment and drinking behaviour: some data from a general population survey of alcohol use. Br J Addict. 1987;82:1007–1016. doi: 10.1111/j.1360-0443.1987.tb01561.x. [DOI] [PubMed] [Google Scholar]
- Cruz FC, Quadros IM, Planeta Cda S, Miczek KA. Maternal separation stress in male mice: long-term increases in alcohol intake. Psychopharmacology (Berl) 2008;201:459–468. doi: 10.1007/s00213-008-1307-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daughters SB, Richards JM, Gorka SM, Sinha R. HPA axis response to psychological stress and treatment retention in residential substance abuse treatment: a prospective study. Drug Alcohol Addiction. 2009;105:202–208. doi: 10.1016/j.drugalcdep.2009.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- David D, Mellman TA, Mendoza LM, Kulick-Bell R, Ironson G, Schneiderman N. Psychiatric morbidity following Hurricane Andrew. J Trauma Stress. 1996;9:607–612. doi: 10.1007/BF02103669. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Ruan WJ. The association between stress and drinking: modifying effects of gender and vulnerability. Alcohol Alcohol. 2005;40:453–460. doi: 10.1093/alcalc/agh176. [DOI] [PubMed] [Google Scholar]
- DiMaggio C, Galea S, Li G. Substance use and misuse in the aftermath of terrorism. A Bayesian meta-analysis. Addiction. 2009;104:894–904. doi: 10.1111/j.1360-0443.2009.02526.x. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP. The role of adversity and stress in psychopathology: some evidence and its implications for theory and research. J Health Soc Behav. 2000;41:1–19. [PubMed] [Google Scholar]
- Dohrenwend BP. Inventorying stressful life events as risk factors for psychopathology: toward resolution of the problem of intracategory variability. Psychol Bull. 2006;132:477–495. doi: 10.1037/0033-2909.132.3.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dohrenwend BS, Krasnoff L, Askenasy AR, Dohrenwend BP. Exemplification of a method for scaling life events: the Peri Life Events Scale. J Health Soc Behav. 1978;19:205–229. [PubMed] [Google Scholar]
- Dohrenwend BS, Dohrenwend BP, Dodson M, Shrout PE. Symptoms, hassles, social supports, and life events: problem of confounded measures. J Abnorm Psychol. 1984;93:222–230. doi: 10.1037//0021-843x.93.2.222. [DOI] [PubMed] [Google Scholar]
- Dohrenwend BP, Raphael K, Schwartz S, Steuve A, Skodol A. The structured event probe and narrative rating method for measuring stressful life events. In: Goldberger L, Breznits S, editors. Handbook of stress: theoritical and clinical aspects. Free Press; New York: 1993. pp. 174–199. [Google Scholar]
- Dong M, Anda RF, Felitti VJ, Dube SR, Williamson DF, Thompson TJ, Loo CM, Giles WH. The interrelatedness of multiple forms of childhood abuse, neglect, and household dysfunction. Child Abuse Negl. 2004;28:771–784. doi: 10.1016/j.chiabu.2004.01.008. [DOI] [PubMed] [Google Scholar]
- Drabble L, Midanik LT, Trocki K. Reports of alcohol consumption and alcohol-related problems among homosexual, bisexual and heterosexual respondents: results from the 2000 National Alcohol Survey. J Stud Alcohol. 2005;66:111–120. doi: 10.15288/jsa.2005.66.111. [DOI] [PubMed] [Google Scholar]
- Dube SR, Anda RF, Felitti VJ, Edwards VJ, Williamson DF. Exposure to abuse, neglect, and household dysfunction among adults who witnessed intimate partner violence as children: implications for health and social services. Violence Vict. 2002;17:3–17. doi: 10.1891/vivi.17.1.3.33635. [DOI] [PubMed] [Google Scholar]
- Edwards VJ, Holden GW, Felitti VJ, Anda RF. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: results from the adverse childhood experiences study. Am J Psychiatry. 2003;160:1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Eisenberg M, Wechsler H. Substance use behaviors among college students with same-sex and opposite-sex experience: results from a national study. Addict Behav. 2003;28:899–913. doi: 10.1016/s0306-4603(01)00286-6. [DOI] [PubMed] [Google Scholar]
- Enoch MA. The role of early life stress as a predictor for alcohol and drug dependence. Psychopharmacology (Berl) 2010 doi: 10.1007/s00213-010-1916-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW, Kim P. Childhood poverty and health: cumulative risk exposure and stress dysregulation. Psychol Sci. 2007;18:953–957. doi: 10.1111/j.1467-9280.2007.02008.x. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Woodward LJ. The stability of child abuse reports: a longitudinal study of the reporting behaviour of young adults. Psychol Med. 2000;30:529–544. doi: 10.1017/s0033291799002111. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod RK, Turner HA. Poly-victimization: a neglected component in child victimization. Child Abuse Negl. 2007;31:7–26. doi: 10.1016/j.chiabu.2006.06.008. [DOI] [PubMed] [Google Scholar]
- Flory K, Hankin BL, Kloos B, Cheely C, Turecki G. Alcohol and cigarette use and misuse among Hurricane Katrina survivors: psychosocial risk and protective factors. Subst Use Misuse. 2009;44:1711–1724. doi: 10.3109/10826080902962128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frable DE, Platt L, Hoey S. Concealable stigmas and positive self-perceptions: feeling better around similar others. J Pers Soc Psychol. 1998;74:909–922. doi: 10.1037//0022-3514.74.4.909. [DOI] [PubMed] [Google Scholar]
- Galea S, Riddle M, Kaplan GA. Causal thinking and complex system approaches in epidemiology. Int J Epidemiol. 2010;39:97–106. doi: 10.1093/ije/dyp296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garofalo R, Wolf RC, Kessel S, Palfrey SJ, DuRant RH. The association between health risk behaviors and sexual orientation among a school-based sample of adolescents. Pediatrics. 1998;101:895–902. doi: 10.1542/peds.101.5.895. [DOI] [PubMed] [Google Scholar]
- Gass JT, Olive MF. Reinstatement of ethanol-seeking behavior following intravenous self-administration in Wistar rats. Alcohol Clin Exp Res. 2007;31:1441–1445. doi: 10.1111/j.1530-0277.2007.00480.x. [DOI] [PubMed] [Google Scholar]
- Gee GC, Delva J, Takeuchi DT. Relationships between self-reported unfair treatment and prescription medication use, illicit drug use, and alcohol dependence among Filipino Americans. Am J Public Health. 2007;97:933–940. doi: 10.2105/AJPH.2005.075739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert R, Widom CS, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373:68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- Glymour M. Natural experiments and instrumental variable analysis in social epidemiology. In: Oakes J, Kaufman J, editors. Methods in social epidemiology. Jossey-Bass; New York: 2006. [Google Scholar]
- Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: resultsfrom the national longitudinal alcohol epidemiologic survey. J Subst Abuse. 1997;9:103–110. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- Grant KE, Compas BE, Thurm AE, McMahon SD, Gipson PY. Stressors and child and adolescent psychopathology: measure-ment issues and prospective effects. J Clin Child Adolesc Psychol. 2004;33:412–425. doi: 10.1207/s15374424jccp3302_23. [DOI] [PubMed] [Google Scholar]
- Greeley J, Oei T. Alcohol and tension reduction. In: Leonard KE, Blane HT, editors. Psychological theories of drinking and alcoholism. 2nd edn Guilford; New York: 1999. pp. 14–53. [Google Scholar]
- Green BL, Grace MC, Gleser GC. Identifying survivors at risk: long-term impairment following the Beverly Hills Supper Club fire. J Consult Clin Psychol. 1985;53:672–678. doi: 10.1037//0022-006x.53.5.672. [DOI] [PubMed] [Google Scholar]
- Green BL, Lindy JD, Grace MC, Leonard AC. Chronic posttraumatic stress disorder and diagnostic comorbidity in a disaster sample. J Nerv Ment Dis. 1992;180:760–766. doi: 10.1097/00005053-199212000-00004. [DOI] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: associations with first onset of DSM-IV disorders. Arch Gen Psychiatry. 2010;67:113–123. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grieger TA, Fullerton CS, Ursano RJ. Posttraumatic stress disorder, alcohol use, and perceived safety after the terrorist attack on the pentagon. Psychiatr Serv. 2003;54:1380–1382. doi: 10.1176/appi.ps.54.10.1380. [DOI] [PubMed] [Google Scholar]
- Gruenewald PJ, Johnson FW. Drinking, driving, and crashing: a traffic-flow model of alcohol-related motor vehicle accidents. J Stud Alcohol Drugs. 2010;71:237–248. doi: 10.15288/jsad.2010.71.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruenewald PJ, Johnson FW, Ponicki WR, Lascala EA. A dose-response perspective on college drinking and related problems. Addiction. 2010;105:257–269. doi: 10.1111/j.1360-0443.2009.02767.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallberg H, Mattsson B. Premature deaths among men in aSwedish municipality—civil status and primary health care utilization prior to death. Scand J Soc Med. 1990;18:213–219. doi: 10.1177/140349489001800310. [DOI] [PubMed] [Google Scholar]
- Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry. 2004;45:260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Keyes KM, Hatzenbuehler ML, Aharonovich EA, Alderson D. Alcohol consumption and posttraumatic stress after exposure to terrorism: effects of proximity, loss, and psychiatric history. Am. J Public Health. 2007a;97:2268–2275. doi: 10.2105/AJPH.2006.100057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the national epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2007b;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML. How does sexual minority stigma “get under the skin”? A psychological mediation framework. Psychol Bull. 2009;135:707–730. doi: 10.1037/a0016441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Corbin WR, Fromme K. Trajectories and determinants of alcohol use among LGB young adults and their heterosexual peers: results from a prospective study. Dev Psychol. 2008;44:81–90. doi: 10.1037/0012-1649.44.1.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Nolen-Hoeksema S, Dovidio J. How does stigma “get under the skin”?: the mediating role of emotion regulation. Psychol Sci. 2009;20:1282–1289. doi: 10.1111/j.1467-9280.2009.02441.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, McLaughlin KA, Keyes KM, Hasin DS. The impact of institutional discrimination on psychiatric disor-ders in lesbian, gay, and bisexual populations: a prospective study. Am J Public Health. 2010;100:452–459. doi: 10.2105/AJPH.2009.168815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Corbin WR, Fromme K. Discrimination and alcohol-related problems in emerging adults: A prospective examination of mediating effects. Drug Alcohol Depend. 2011 doi: 10.1016/j.drugalcdep.2010.11.002. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM. Hate crimes and stigma-related experiences among sexual minority adults in the United States: prevalence estimates from a national probability sample. J Interpers Violence. 2009;24:54–74. doi: 10.1177/0886260508316477. [DOI] [PubMed] [Google Scholar]
- Ho JE, Paultre F, Mosca L. Lifestyle changes in New Yorkers after September 11, 2001 (data from the Post-Disaster Heart Attack Prevention Program) Am J Cardiol. 2002;90:680–682. doi: 10.1016/s0002-9149(02)02587-0. [DOI] [PubMed] [Google Scholar]
- Holmes TH, Rahe RH. The social readjustment rating scale. JPsychosom Res. 1967;11:213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- Hughes D, Rodriguez J, Smith EP, Johnson DJ, Stevenson HC, Spicer P. Parents’ ethnic-racial socialization practices: a review of research and directions for future study. Dev Psychol. 2006;42:747–770. doi: 10.1037/0012-1649.42.5.747. [DOI] [PubMed] [Google Scholar]
- Hussey JM, Chang JJ, Kotch JB. Child maltreatment in the United States: prevalence, risk factors, and adolescent health consequences. Pediatrics. 2006;118:933–942. doi: 10.1542/peds.2005-2452. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Brown J, Smailes EM, Bernstein DP. Childhood maltreatment increases risk for personality disorders during early adulthood. Arch Gen Psychiatry. 1999;56:600–606. doi: 10.1001/archpsyc.56.7.600. [DOI] [PubMed] [Google Scholar]
- Joseph S, Yule W, Williams R, Hodgkinson P. Increased substance use in survivors of the Herald of free enterprise disaster. Br J Med Psychol. 1993;66(Pt 2):185–191. doi: 10.1111/j.2044-8341.1993.tb01740.x. [DOI] [PubMed] [Google Scholar]
- Kasl SV, Chisholm RF, Eskenazi B. The impact of the accident at the Three Mile Island on the behavior and well-being of nuclear workers; Part I: perceptions and evaluations, behavioral responses, and work-related attitudes and feelings. Am J Public Health. 1981;71:472–483. doi: 10.2105/ajph.71.5.472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman J, Yang BZ, Douglas-Palumberi H, Crouse-Artus M, Lipschitz D, Krystal JH, Gelernter J. Genetic and environmental predictors of early alcohol use. Biol Psychiatry. 2007;61:1228–1234. doi: 10.1016/j.biopsych.2006.06.039. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Gardner CO. Dependent stressful life events and prior depressive episodes in the prediction of major depression: the problem of causal inference in psychiatric epidemiology. Arch Gen Psychiatry. 2010;67:1120–1127. doi: 10.1001/archgenpsychiatry.2010.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Prescott CA, Kessler RC, Heath AC, Corey LA, Eaves LJ. Childhood parental loss and alcoholism in women: a causal analysis using a twin-family design. Psychol Med. 1996;26:79–95. doi: 10.1017/s0033291700033730. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Bulik CM, Silberg J, Hettema JM, Myers J, Prescott CA. Childhood sexual abuse and adult psychiatric and substance use disorders in women: an epidemiological and cotwin control analysis. Arch Gen Psychiatry. 2000;57:953–959. doi: 10.1001/archpsyc.57.10.953. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Thornton LM, Prescott CA. Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. Am J Psychiatry. 2001;158:587–593. doi: 10.1176/appi.ajp.158.4.587. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Hettema JM, Butera F, Gardner CO, Prescott CA. Life event dimensions of loss, humiliation, entrapment, and danger in the prediction of onsets of major depression and generalized anxiety. Arch Gen Psychiatry. 2003;60:789–796. doi: 10.1001/archpsyc.60.8.789. [DOI] [PubMed] [Google Scholar]
- Kennedy PJ, Haertsch PA, Maitz PK. The Bali burn disaster: implications and lessons learned. J Burn Care Rehabil. 2005;26:125–131. doi: 10.1097/01.bcr.0000155532.31639.0d. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Price RH, Wortman CB. Social factors in psychopathology: stress, social support, and coping processes. Annu Rev Psychol. 1985;36:531–572. doi: 10.1146/annurev.ps.36.020185.002531. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshleman S, Wittchen HU, Kendler KS. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States. Results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Davis CG, Kendler KS. Childhood adversity and adult psychiatric disorder in the US National Comorbidity Survey. Psychol Med. 1997;27:1101–1119. doi: 10.1017/s0033291797005588. [DOI] [PubMed] [Google Scholar]
- Kettinger LA, Nair P, Schuler ME. Exposure to environmental risk factors and parenting attitudes among substance-abusing women. Am J Drug Alcohol Abuse. 2000;26:1–11. doi: 10.1081/ada-100100586. [DOI] [PubMed] [Google Scholar]
- Keyes KM, Grant BF, Hasin DS. Evidence for a closing gender gap in alcohol use, abuse, and dependence in the United States population. Drug Alcohol Depend. 2008;93:21–29. doi: 10.1016/j.drugalcdep.2007.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kihlstrom JF, Eich E, Sandbrand D, Tobias BA. Emotion and memory: implications for self-report. In: Stone AA, Turkkan JS, Bachrach CA, Jobe JB, Kurtzman JS, Cain VS, editors. The science of self-report: implications for research and practice. Erlbaum; Mahwah: 2000. [Google Scholar]
- Kilpatrick DG, Acierno R, Resnick HS, Saunders BE, Best CL. A 2-year longitudinal analysis of the relationships between violent assault and substance use in women. J Consult Clin Psychol. 1997;65:834–847. doi: 10.1037//0022-006x.65.5.834. [DOI] [PubMed] [Google Scholar]
- King AC, Bernardy NC, Hauner K. Stressful events, personality, and mood disturbance: gender differences in alcoholics and problem drinkers. Addict Behav. 2003;28:171–187. doi: 10.1016/s0306-4603(01)00264-7. [DOI] [PubMed] [Google Scholar]
- Klein DN, Rubovits DR. The reliability of subjects’ reports on stressful life events inventories: a longitudinal study. J Behav Med. 1987;10:501–512. doi: 10.1007/BF00846147. [DOI] [PubMed] [Google Scholar]
- Kohn R, Levav I, Garcia ID, Machuca ME, Tamashiro R. Prevalence, risk factors and aging vulnerability for psychopathology following a natural disaster in a developing country. Int J Geriatr Psychiatry. 2005;20:835–841. doi: 10.1002/gps.1369. [DOI] [PubMed] [Google Scholar]
- Koob GF. The neurobiology of addiction: a neuroadaptational view relevant for diagnosis. Addiction. 2006;101(Suppl 1):23–30. doi: 10.1111/j.1360-0443.2006.01586.x. [DOI] [PubMed] [Google Scholar]
- Lahelma E, Kangas R, Manderbacka K. Drinking and unemployment: contrasting patterns among men and women. Drug Alcohol Depend. 1995;37:71–82. doi: 10.1016/0376-8716(94)01054-o. [DOI] [PubMed] [Google Scholar]
- Lazarus RS. Stress and emotion: a new synthesis. Springer; New York: 1999. [Google Scholar]
- Levine S. Developmental determinants of sensitivity and resistance to stress. Psychoneuroendocrinology. 2005;30:939–946. doi: 10.1016/j.psyneuen.2005.03.013. [DOI] [PubMed] [Google Scholar]
- Lewis TT, Everson-Rose SA, Powell LH, Matthews KA, Brown C, Karavolos K, Sutton-Tyrrell K, Jacobs E, Wesley D. Chronic exposure to everyday discrimination and coronary artery calcification in African-American women: the SWAN Heart Study. Psychosom Med. 2006;68:362–368. doi: 10.1097/01.psy.0000221360.94700.16. [DOI] [PubMed] [Google Scholar]
- Luoto R, Poikolainen K, Uutela A. Unemployment, sociodemographic background and consumption of alcohol before and during the economic recession of the 1990s in Finland. Int J Epidemiol. 1998;27:623–629. doi: 10.1093/ije/27.4.623. [DOI] [PubMed] [Google Scholar]
- Lyons MJ, Goldberg J, Eisen SA, True W, Tsuang MT, Meyer JM, Henderson WG. Do genes influence exposure to trauma? A twin study of combat. Am J Med Genet. 1993;48:22–27. doi: 10.1002/ajmg.1320480107. [DOI] [PubMed] [Google Scholar]
- MacMillan HL, Fleming JE, Streiner DL, Lin E, Boyle MH, Jamieson E, Duku EK, Walsh CA, Wong MY, Beardslee WR. Childhood abuse and lifetime psychopathology in a community sample. Am J Psychiatry. 2001;158:1878–1883. doi: 10.1176/appi.ajp.158.11.1878. [DOI] [PubMed] [Google Scholar]
- Mahoney EJ, Harrington DT, Biffl WL, Metzger J, Oka T, Cioffi WG. Lessons learned from a nightclub fire: institutional disaster preparedness. J Trauma. 2005;58:487–491. doi: 10.1097/01.ta.0000153939.17932.e7. [DOI] [PubMed] [Google Scholar]
- Mason BJ, Shaham Y, Weiss F, Le AD. Stress, alcohol craving, and relapse risk: mechanisms and viable treatment targets. Alcohol. 2009;43:541–543. doi: 10.1016/j.alcohol.2009.09.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maughan B, Rutter M. Retrospective reporting of childhood adversity: issues in assessing long-term recall. J Pers Disord. 1997;11:19–33. doi: 10.1521/pedi.1997.11.1.19. [DOI] [PubMed] [Google Scholar]
- McCabe SE, Bostwick WB, Hughes TL, West BT, Boyd CJ. The relationship between discrimination and substance use disorders among lesbian, gay, and bisexual adults in the United States. Am J Public Health. 2010;100:1946–1952. doi: 10.2105/AJPH.2009.163147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol Rev. 2007;87:873–904. doi: 10.1152/physrev.00041.2006. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication II: associations with persistence of DSM-IV disorders. Arch Gen Psychiatry. 2010a;67:124–132. doi: 10.1001/archgenpsychiatry.2009.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Keyes KM. Responses to discrimination and psychiatric disorders among Black, Hispanic, female, and lesbian, gay, and bisexual individuals. Am J Public Health. 2010b;100:1477–1484. doi: 10.2105/AJPH.2009.181586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Melnik TA, Baker CT, Adams ML, O’Dowd K, Mokdad AH, Brown DW, Murphy W, Giles WH, Bales VS. Psychological and emotional effects of the September 11 attacks on the World Trade Center—Connecticut, New Jersey, and New York, 2001. MMWR Morb Mortal Wkly Rep. 2002;51:784–786. [PubMed] [Google Scholar]
- Mendoza-Denton R, Downey G, Purdie VJ, Davis A, Pietrzak J. Sensitivity to status-based rejection: implications for African American students’ college experience. J Pers Soc Psychol. 2002;83:896–918. doi: 10.1037//0022-3514.83.4.896. [DOI] [PubMed] [Google Scholar]
- Meyer IH. Prejudice as stress: conceptual and measurement problems. Am J Public Health. 2003a;93:262–265. doi: 10.2105/ajph.93.2.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003b;129:674–697. doi: 10.1037/0033-2909.129.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH, Schwartz S, Frost DM. Social patterning of stress and coping: does disadvantaged social statuses confer more stress and fewer coping resources? Soc Sci Med. 2008;67:368–379. doi: 10.1016/j.socscimed.2008.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miczek KA, Yap JJ, Covington HE., 3rd Social stress, therapeutics and drug abuse: preclinical models of escalated and depressed intake. Pharmacol Ther. 2008;120:102–128. doi: 10.1016/j.pharmthera.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molnar BE, Buka SL, Kessler RC. Child sexual abuse and subsequent psychopathology: results from the National Comorbidity Survey. Am J Public Health. 2001;91:753–760. doi: 10.2105/ajph.91.5.753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe SM. Modern approaches to conceptualizing and measuring human life stress. Annu Rev Clin Psychol. 2008;4:33–52. doi: 10.1146/annurev.clinpsy.4.022007.141207. [DOI] [PubMed] [Google Scholar]
- Mulia N, Ye Y, Zemore SE, Greenfield TK. Social disadvantage, stress, and alcohol use among black, Hispanic, and white Americans: findings from the 2005 US National Alcohol Survey. J Stud Alcohol Drugs. 2008;69:824–833. doi: 10.15288/jsad.2008.69.824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson EC, Heath AC, Madden PA, Cooper ML, Dinwiddie SH, Bucholz KK, Glowinski A, McLaughlin T, Dunne MP, Statham DJ, Martin NG. Association between self-reported childhood sexual abuse and adverse psychosocial outcomes: results from a twin study. Arch Gen Psychiatry. 2002;59:139–145. doi: 10.1001/archpsyc.59.2.139. [DOI] [PubMed] [Google Scholar]
- Nelson EC, Heath AC, Lynskey MT, Bucholz KK, Madden PA, Statham DJ, Martin NG. Childhood sexual abuse and risks for licit and illicit drug-related outcomes: a twin study. Psychol Med. 2006;36:1473–1483. doi: 10.1017/S0033291706008397. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Harrell ZA. Rumination, depression, and alcohol use: tests of gender differences. J Cogn Psychother. 2002;16:391–403. [Google Scholar]
- North CS, Smith EM, Spitznagel EL. Posttraumatic stress disorder in survivors of a mass shooting. Am J Psychiatry. 1994;151:82–88. doi: 10.1176/ajp.151.1.82. [DOI] [PubMed] [Google Scholar]
- North CS, Nixon SJ, Shariat S, Mallonee S, McMillen JC, Spitznagel EL, Smith EM. Psychiatric disorders among survivors of the Oklahoma City bombing. JAMA. 1999;282:755–762. doi: 10.1001/jama.282.8.755. [DOI] [PubMed] [Google Scholar]
- North CS, Tivis L, McMillen JC, Pfefferbaum B, Spitznagel EL, Cox J, Nixon S, Bunch KP, Smith EM. Psychiatric disorders in rescue workers after the Oklahoma City bombing. Am J Psychiatry. 2002;159:857–859. doi: 10.1176/appi.ajp.159.5.857. [DOI] [PubMed] [Google Scholar]
- North CS, Kawasaki A, Spitznagel EL, Hong BA. The course of PTSD, major depression, substance abuse, and somatization after a natural disaster. J Nerv Ment Dis. 2004;192:823–829. doi: 10.1097/01.nmd.0000146911.52616.22. [DOI] [PubMed] [Google Scholar]
- North CS, Pfefferbaum B, Narayanan P, Thielman S, McCoy G, Dumont C, Kawasaki A, Ryosho N, Kim YS, Spitznagel EL. Comparison of post-disaster psychiatric disorders after terrorist bombings in Nairobi and Oklahoma City. Br J Psychiatry. 2005;186:487–493. doi: 10.1192/bjp.186.6.487. [DOI] [PubMed] [Google Scholar]
- North CS, Ringwalt CL, Downs D, Derzon J, Galvin D. Postdisaster course of alcohol use disorders in systematically studied survivors of 10 disasters. Arch Gen Psychiatry. 2010;68(2):173–180. doi: 10.1001/archgenpsychiatry.2010.131. [DOI] [PubMed] [Google Scholar]
- Pachankis JE. The psychological implications of concealing a stigma: a cognitive-affective-behavioral model. Psychol Bull. 2007;133:328–345. doi: 10.1037/0033-2909.133.2.328. [DOI] [PubMed] [Google Scholar]
- Paykel ES, Prusoff BA, Uhlenhuth EH. Scaling of life events. Arch Gen Psychiatry. 1971;25:340–347. doi: 10.1001/archpsyc.1971.01750160052010. [DOI] [PubMed] [Google Scholar]
- Pilowsky DJ, Keyes KM, Hasin DS. Adverse childhood events and lifetime alcohol dependence. Am J Public Health. 2009;99:258–263. doi: 10.2105/AJPH.2008.139006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahe RH, Mahan JL, Jr, Arthur RJ. Prediction of near-future health change from subjects’ preceding life changes. J Psychosom Res. 1970;14:401–406. doi: 10.1016/0022-3999(70)90008-5. [DOI] [PubMed] [Google Scholar]
- Reijneveld SA, Crone MR, Verhulst FC, Verloove-Vanhorick SP. The effect of a severe disaster on the mental health of adolescents: a controlled study. Lancet. 2003;362:691–696. doi: 10.1016/S0140-6736(03)14231-6. [DOI] [PubMed] [Google Scholar]
- Richman JA, Flaherty JA, Rospenda KM. Perceived workplace harassment experiences and problem drinking among physicians: broadening the stress/alienation paradigm. Addiction. 1996;91:391–403. [PubMed] [Google Scholar]
- Richman JA, Wislar JS, Flaherty JA, Fendrich M, Rospenda KM. Effects on alcohol use and anxiety of the September 11, 2001, attacks and chronic work stressors: a longitudinal cohort study. Am J Public Health. 2004;94:2010–2015. doi: 10.2105/ajph.94.11.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rospenda KM, Fujishiro K, Shannon CA, Richman JA. Workplace harassment, stress, and drinking behavior over time: gender differences in a national sample. Addict Behav. 2008;33:964–967. doi: 10.1016/j.addbeh.2008.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. The alcohol use disorder and associated disabilities interview schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell ST, Driscoll AK, Truong N. Adolescent same-sex romantic attractions and relationships: implications for substance use and abuse. Am J Public Health. 2002;92:198–202. doi: 10.2105/ajph.92.2.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampson R, Raudenbush S. Systematic social observation of public spaces: a new look at disorder in urban neighborhoods. Am J Sociol. 1999;105:603–651. [Google Scholar]
- San José B, Van Oers HAM, Van de Mheen HD, Garretsen HFL, Mackenbach JP. Stressors and alcohol consumption. Alcohol Alcohol. 2000;35:307–312. doi: 10.1093/alcalc/35.3.307. [DOI] [PubMed] [Google Scholar]
- Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: development of the life experiences survey. J Consult Clin Psychol. 1978;46:932–946. doi: 10.1037//0022-006x.46.5.932. [DOI] [PubMed] [Google Scholar]
- Sartor CE, Lynskey MT, Bucholz KK, McCutcheon VV, Nelson EC, Waldron M, Heath AC. Childhood sexual abuse and the course of alcohol dependence development: findings from a female twin sample. Drug Alcohol Depend. 2007;89:139–144. doi: 10.1016/j.drugalcdep.2006.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schiff M, Benbenishty R, McKay M, Devoe E, Liu X, Hasin D. Exposure to terrorism and Israeli youths’ psychological distress and alcohol use: an exploratory study. Am J Addict. 2006;15:220–226. doi: 10.1080/10550490600626200. [DOI] [PubMed] [Google Scholar]
- Schiff M, Zweig HH, Benbenishty R, Hasin DS. Exposure to terrorism and Israeli youths’ cigarette, alcohol, and cannabis use. Am J Public Health. 2007;97:1852–1858. doi: 10.2105/AJPH.2006.090514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwartz S, Meyer IH. Mental health disparities research: the impact of within and between group analyses on tests of social stress hypotheses. Soc Sci Med. 2010;70:1111–1118. doi: 10.1016/j.socscimed.2009.11.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarz N. Cognitive aspects of survey methodology. Appl Cogn Psych. 2007;21:277–287. [Google Scholar]
- Selye H. McGraw-Hill; McGraw-Hill: 1976. The stress of life. [Google Scholar]
- Sher KJ, Gershuny BS, Peterson L, Raskin G. The role of childhood stressors in the intergenerational transmission of alcohol use disorders. J Stud Alcohol. 1997;58(4):414–427. doi: 10.15288/jsa.1997.58.414. [DOI] [PubMed] [Google Scholar]
- Sher KJ, Grekin ER, Williams NA. The development of alcohol use disorders. Annu Rev Clin Psychol. 2005;1:493–523. doi: 10.1146/annurev.clinpsy.1.102803.144107. [DOI] [PubMed] [Google Scholar]
- Shimizu S, Aso K, Noda T, Ryukei S, Kochi Y, Yamamoto N. Natural disasters and alcohol consumption in a cultural context: the Great Hanshin Earthquake in Japan. Addiction. 2000;95:529–536. doi: 10.1046/j.1360-0443.2000.9545295.x. [DOI] [PubMed] [Google Scholar]
- Sieber SD. Toward a theory of role accumulation. Am SociolRev. 1974;39:567–578. [Google Scholar]
- Sims A, Sims D. The phenomenology of post-traumatic stress disorder. A symptomatic study of 70 victims of psychological trauma. Psychopathology. 1998;31:96–112. doi: 10.1159/000029029. [DOI] [PubMed] [Google Scholar]
- Sinha R. How does stress increase risk of drug abuse and relapse? Psychopharmacol Berl. 2001;158:343–359. doi: 10.1007/s002130100917. [DOI] [PubMed] [Google Scholar]
- Sinha R. Chronic stress, drug use, and vulnerability to addiction. Ann NY Acad Sci. 2008;1141:105–130. doi: 10.1196/annals.1441.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skaff MM, Finney JW, Moos RH. Gender differences in problem drinking and depression: different “vulnerabilities?”. Am J Community Psychol. 1999;27:25–54. doi: 10.1023/A:1022813727823. [DOI] [PubMed] [Google Scholar]
- Smith EM, North CS, McCool RE, Shea JM. Acute postdisaster psychiatric disorders: identification of persons at risk. Am J Psychiatry. 1990;147:202–206. doi: 10.1176/ajp.147.2.202. [DOI] [PubMed] [Google Scholar]
- Smith DW, Christiansen EH, Vincent R, Hann NE. Population effects of the bombing of Oklahoma City. J Okla State Med Assoc. 1999;92:193–198. [PubMed] [Google Scholar]
- Stanger C, Dumenci L, Kamon J, Burstein M. Parenting and children’s externalizing problems in substance-abusing families. J Clin Child Adolesc Psychol. 2004;33:590–600. doi: 10.1207/s15374424jccp3303_16. [DOI] [PubMed] [Google Scholar]
- Stein BD, Elliott MN, Jaycox LH, Collins RL, Berry SH, Klein DJ, Schuster MA. A national longitudinal study of the psychological consequences of the September 11, 2001 terrorist attacks: reactions, impairment, and help-seeking. Psychiatry. 2004;67:105–117. doi: 10.1521/psyc.67.2.105.35964. [DOI] [PubMed] [Google Scholar]
- Suchman NE, Rounsaville B, DeCoste C, Luthar S. Parental control, parental warmth, and psychosocial adjustment in a sample of substance-abusing mothers and their school-aged and adolescent children. J Subst Abuse Treat. 2007;32:1–10. doi: 10.1016/j.jsat.2006.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suchman N, McMahon T, Decoste C, Castiglioni N, Luthar S. Ego development, psychopathology, and parenting problems in substance-abusing mothers. Am J Orthopsychiatry. 2008;78:20–28. doi: 10.1037/0002-9432.78.1.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor J, Jackson B. Factors affecting alcohol consumption in black women. Part I. Int J Addict. 1990;25:1287–1300. doi: 10.3109/10826089009056222. [DOI] [PubMed] [Google Scholar]
- Thompson RG, Jr, Lizardi D, Keyes KM, Hasin DS. Childhood or adolescent parental divorce/separation, parental history of alcohol problems, and offspring lifetime alcohol dependence. Drug Alcohol Depend. 2008;98:264–269. doi: 10.1016/j.drugalcdep.2008.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thornberry TP, Ireland TO, Smith CA. The importance of timing: the varying impact of childhood and adolescent maltreatment on multiple problem outcomes. Dev Psychopathol. 2001;13:957–979. [PubMed] [Google Scholar]
- Vielva I, Iraurgi I. Cognitive and behavioural factors as predictors of abstinence following treatment for alcohol dependence. Addiction. 2001;96:297–303. doi: 10.1046/j.1360-0443.2001.96229713.x. [DOI] [PubMed] [Google Scholar]
- Vlahov D, Galea S, Resnick H, Ahern J, Boscarino JA, Bucuvalas M, Gold J, Kilpatrick D. Increased use of cigarettes, alcohol, and marijuana among Manhattan, New York, residents after the September 11th terrorist attacks. Am J Epidemiol. 2002;155:988–996. doi: 10.1093/aje/155.11.988. [DOI] [PubMed] [Google Scholar]
- Vlahov D, Galea S, Ahern J, Resnick H, Kilpatrick D. Sustained increased consumption of cigarettes, alcohol, and marijuana among Manhattan residents after september 11, 2001. Am J Public Health. 2004;94:253–254. doi: 10.2105/ajph.94.2.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlahov D, Galea S, Ahern J, Rudenstine S, Resnick H, Kilpatrick D, Crum RM. Alcohol drinking problems among New York City residents after the September 11 terrorist attacks. Subst Use Misuse. 2006;41:1295–1311. doi: 10.1080/10826080600754900. [DOI] [PubMed] [Google Scholar]
- Waldo CR. Working in a majority context: a structural model of heterosexism as minority stress in the workplace. J Couns Psychol. 1999;46:218–232. [Google Scholar]
- Walter M, Gerhard U, Duersteler-MacFarland KM, Weijers HG, Boening J, Wiesbeck GA. Social factors but not stress-coping stylespredict relapse in detoxified alcoholics. Neuropsychobiology. 2006;54:100–106. doi: 10.1159/000096991. [DOI] [PubMed] [Google Scholar]
- Wethington E, Brown GW, Kessler RC. Interview measurement of stressful life events. In: Cohen S, Kessler RC, Gordon LU, editors. Measuring stress: a guide for health and social scientists. Oxford University Press; New York: 1995. pp. 56–79. [Google Scholar]
- Wheatron B. Sampling the stress universe. In: Avison WR, Gotlib IH, editors. Stress and mental halth. Plenum; New York: 1994. pp. 77–114. [Google Scholar]
- Whitbeck LB, Hoyt DR, McMorris BJ, Chen X, Stubben JD. Perceived discrimination and early substance abuse among American Indian children. J Health Soc Behav. 2001;42:405–424. [PubMed] [Google Scholar]
- Widom CS. Accuracy of adult recollection of childhood victimization: Part I. Childhood physical abuse. Psychol Assess. 1996;8:412–421. [Google Scholar]
- Widom CS. Accuracy of adult recollection of childhood victimization: Part 2. Childhood sexual abuse. Psychol Assess. 1997;9:34–46. [Google Scholar]
- Widom CS, Ireland T, Glynn PJ. Alcohol abuse in abused and neglected children followed-up: are they at increased risk? J Stud Alcohol. 1995;56:207–217. doi: 10.15288/jsa.1995.56.207. [DOI] [PubMed] [Google Scholar]
- Widom CS, Weiler BL, Cottler LB. Childhood victimization and drug abuse: a comparison of prospective and retrospective findings. J Consult Clin Psychol. 1999;67:867–880. doi: 10.1037//0022-006x.67.6.867. [DOI] [PubMed] [Google Scholar]
- Widom CS, DuMont K, Czaja SJ. A prospective investigation of major depressive disorder and comorbidity in abused and neglected children grown up. Arch Gen Psychiatry. 2007a;64:49–56. doi: 10.1001/archpsyc.64.1.49. [DOI] [PubMed] [Google Scholar]
- Widom CS, White HR, Czaja SJ, Marmorstein NR. Long-term effects of child abuse and neglect on alcohol use and excessive drinking in middle adulthood. J Stud Alcohol Drugs. 2007b;68:317–326. doi: 10.15288/jsad.2007.68.317. [DOI] [PubMed] [Google Scholar]
- Williams DR. Racial variations in adult health status: patterns, paradoxes, and prospects. In: Smelser NJ, Wilson WJ, Mitchell F, editors. America becoming: racial trends and their consequences. National Academy Press; Washington, D.C: 2001. [Google Scholar]
- Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93:200–208. doi: 10.2105/ajph.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilsnack SC, Klassen AD, Schur BE, Wilsnack RW. Predicting onset and chronicity of women’s problem drinking: a five-year longitudinal analysis. Am J Public Health. 1991;81:305–318. doi: 10.2105/ajph.81.3.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen IH, Ragland DR, Greiner BA, Fisher JM. Racial discrimination and alcohol-related behavior in urban transit operators: findings from the San Francisco Muni Health and Safety Study. Public Health Rep. 1999;114:448–458. doi: 10.1093/phr/114.5.448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoo HC, Gee GC, Lowthrop CK, Robertson J. Self-reported racial discrimination and substance use among Asian Americans in Arizona. J Immigr Minor Health. 2010;12:683–690. doi: 10.1007/s10903-009-9306-z. [DOI] [PubMed] [Google Scholar]
- Young SE, Smolen A, Hewitt JK, Haberstick BC, Stallings MC, Corley RP, Crowley TJ. Interaction between MAO-A genotype and maltreatment in the risk for conduct disorder: failure to confirm in adolescent patients. Am J Psychiatry. 2006;163:1019–1025. doi: 10.1176/ajp.2006.163.6.1019. [DOI] [PubMed] [Google Scholar]
- Young-Wolff KC, Kendler KS, Ericson ML, Prescott CA. Accounting for the association between childhood maltreatment and alcohol-use disorders in males: a twin study. Psychol Med. 2011;41:59–70. doi: 10.1017/S0033291710000425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Q, Li B, Scribner RA. Hierarchical additive modeling of nonlinear association with spatial correlations—an application to relate alcohol outlet density and neighborhood assault rates. Stat Med. 2009;28:1896–1912. doi: 10.1002/sim.3600. [DOI] [PubMed] [Google Scholar]
- Ziyadeh NJ, Prokop LA, Fisher LB, Rosario M, Field AE, CamargoCA Jr, Austin SB. Sexual orientation, gender, and alcohol use in a cohort study of U.S. adolescent girls and boys. Drug Alcohol Depend. 2007;87:119–130. doi: 10.1016/j.drugalcdep.2006.08.004. [DOI] [PubMed] [Google Scholar]