Abstract
BACKGROUND:
Numerous medical conditions require timely medication administration in the emergency department (ED). Automated dispensing systems (ADSs) store premixed common doses at the point-of-care to minimize time to administration, but the use of such automation to improved time to medication administration has not been studied. Since vancomycin is a commonly used empiric antimicrobial, we sought to quantify the effect of using an ADS on time to drug delivery in patients presenting to the ED. The study aimed to determine the efficacy of utilizing an ADS to improve time to administration of vancomycin and determine any negative effects on dosing appropriateness.
METHODS:
The institional review board approved the retrospective quality improvement study took place in a single, urban academic tertiary care ED with an annual census of 80 000. Study subjects were all patients receiving vancomycin for the management of sepsis between March 1 to September 30, 2008 and the same time period in 2009. The primary outcome was the proportion of patients who received vancomycin within one hour of bed placement and the secondary outcome was dosing appropriateness.
RESULTS:
Sixty-three patients had weight and dosing information available (29 before and 34 after intervention) and were included in the study. Before intervention, no patient received vancomycin in less than 60 minutes, while after intervention 14.7% of the patients received it in less than 60 minutes (difference in proportions 14.7%, 95% CI 0.39%-30.0%, P=0.04). A similar proportion of the patients received correct dosing before and after intervention (44.8% vs. 41.2%, difference in proportions 3.7%, 95% CI -20.0%-26.7%, P=0.770).
CONCLUSION:
The use of an ADS may improve the timing of medication administration in patients presenting to the ED without affecting dosing appropriateness.
KEY WORDS: Automatic dispensing system, Pharmaceutical, Process improvement, Efficiency
INTRODUCTION
The administration of medications in a timely manner is critical in numerous patient populations that present to the emergency department (ED) for emergency conditions. Acute ischemic stroke, myocardial infarction and sepsis are disease processes commonly seen in the ED, which have evidence demonstrating that timely medication administration improves outcomes.[1-3] The Centers for Medicare and Medicaid have endorsed and tracked several measures for timely medication administration in U.S. hospital emergency departments, including medication for acute myocardial infarction and pneumonia.[4]
Sepsis is a disease process in which timely antimicrobial administration is a mainstay of management.[5] Timely antimicrobial administration is also a component of the resuscitation bundle for septic patients recommended by the Surviving Sepsis Campaign.[6,7] Although a conclusive link between timing, administration and mortality has not been definitively proven,[2,5,8,9] the Surviving Sepsis Campaign recommends empiric broad spectrum antimicrobials “as early as possible and within the first hour of recognition of septic shock and severe sepsis” for patients in an intensive care unit (ICU).[10] The current recommendation for EDs is to administer antibiotics within three hours of recognition.[10] While the timeframe for administration of antimicrobials is longer than that in the ICU, the ultimate goal is to administer broad spectrum antimicrobials rapidly.
Multiple process improvement projects have been undertaken to improve the compliance with the Surviving Sepsis Campaign guidelines through the use of treatment bundles.[11-15] No efforts have specifically targeted reducing the time to antimicrobial administration in septic patients presenting to the ED.
Medication administration in septic patients in the ED is a complex process. First, severe sepsis patients must be identified and placed in a bed in the ED. The health care team must initiate resuscitation measures, obtain adequate vascular access, identify a potential source of infection, and then order and administer broad spectrum antimicrobials. After the initial order for antimicrobials is written by the provider, medication orders must be input into the pharmacy computer system, occasionally mixed, labeled and taken to the care setting from a central pharmacy.
Automated dispensing systems (ADSs) provide alternative, rapid access medication storage, and the proportion of hospitals utilizing such systems has increased from 49% in 1999 to 83% in 2008.[16] ADSs are located within the ED and make emergent pharmaceuticals rapidly available at the site of care. Considering only 6.8% of hospitals have a pharmacist practicing in the ED and only 40.7% of ED medication orders are prospectively reviewed by a pharmacist, ADS represent a technology with an unknown benefit for medication administration times in the ED for critically ill patients.[16]
Our ED administration team decided to place a specific antimicrobial, vancomycin, in an ADS in the resuscitation bay to attempt to reduce the time to administration in septic patients. While vancomycin represented a single antimicrobial, its broad use in nearly every septic patient at this facility represented a unique opportunity to quantify the benefit of a single process change on a complex, multifactorial process such as medication administration. We hypothesized that using an ED-based ADS for dispensing vancomycin would increase the proportion of septic patients who are treated within 60 minutes of bed placement.
METHODS
Study design and setting
The study was a quasi-experimental study involving a retrospective review of medical records for patients seen at an urban, academic ED with an annual census over 80 000 visits. This study was approved by the local institutional review board.
Intervention
Vancomycin is available in the ADD-Vantage intravenous medication system (Hospira). This specially designed system consists of a vial of powdered intravenous medication that is provided in a threaded vial that mates with the top of a flexible diluent container. The ADD-Vantage design keeps the drug and diluent separate until the system is activated just prior to administration, allowing for a 30-day shelf-life.
The vancomycin ADD-Vantage bags were placed in one gram bags in the ADS (Pyxis Med Station version 3500, Cardinal Health) located in the ED. At the time of intervention, the ED staff were trained and educated on the availability of vancomycin in the ED.
Selection of participants
Patients were included in the pre-intervention group if they presented to the ED between March 1, 2008 and September 30, 2008 and those were included in the post-intervention group if they arrived during the same time period one year later. Eligible patients were identified by the ED’s Committee for Procedural Quality and Evidence Based Practice (CPQE) guidelines for sepsis[17] as being eligible for early goal directed therapy (EGDT), and had vancomycin ordered while in the ED.
CPQE reviewers regularly abstract charts of patients with the diagnosis of sepsis by ICD-9 code who presented to the ED. In order to be eligible for EGDT, patients must meet systemic inflammatory response syndrome (SIRS) criteria by having two of the following: heart rate greater than 90 beats per minute; respiratory rate above 20 breaths per minute or arterial pressure of carbon dioxide less than 32 mmHg; temperature greater than 38 degrees Celsius or less than 36 degrees Celsius; or white blood cell count less than 4000 cells/mm3 or greater than 12 000 cells/mm3 or the presence of greater than 10% immature neutrophils (bands). In addition to the SIRS criteria, eligibility for EGDT, as defined by the Surviving Sepsis Campaign, requires the patient to have a confirmed or suspected infectious source and have a lactate level greater than or equal to 4 mmol/deciliter or hypotension defined as a systolic blood pressure less than 90 mmHg despite a 20 mL/kg bolus of crystalloid fluid.[6] Patients eligible for EGDT had detailed chart reviews by a quality nurse to review the specific care they received in the ED.
Methods of measurement
Charts for patients determined to be eligible for EGDT by the quality nurse were additionally reviewed for this study by trained abstractors blinded to study hypothesis. A standardized case report form with an explicit data dictionary was created to facilitate data collection. Abstractors were trained and a pilot review was performed to provide abstractors with direct feedback on performance. All charts were then reviewed by two blinded abstractors. A 10% sample of data abstraction forms were randomly selected to check for accuracy. Discrepancies were adjudicated by a member of the investigative team. Time to administration of vancomcyin was defined as the time the patient was placed in a bed until administration of vancomycin by the treating nurse. If vancomycin was ordered but not administered in the ED or the ED length of stay was less than or equal to 60 minutes, we assumed that the administration time was greater than 180 minutes. Appropriate dosing was defined by hospital pharmacy as 15 mg/kg, rounded to the nearest 250 mg. Data were double entered into a custom database designed for this project (Microsoft Access, Microsoft Corporation, Redmond, WA) for analysis.
Data analysis
Patient characteristics are described using medians and ranges or frequencies and percents. Comparisons between before and after intervention groups used the chi-square test or Fisher’s exact test. The primary outcome for this study was the proportion of patients who received vancomycin within one hour of bed placement to administration and the secondary outcome was dosing appropriateness. Since our institution utilizes a paper-based system for order entry, clinician medication order times are frequently not available. Instead, we utilized bed placement time as a surrogate. The proportion was compared between before and after intervention. Analyses used SPSS version 18.0 (SPSS Inc, Chicago, IL) and Microsoft Excel (Microsoft Corporation, Redmond, WA).
RESULTS
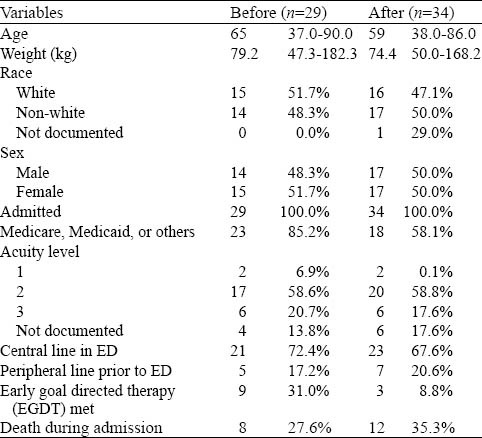
During the study, there were 96 patients eligible for EGDT, and two were excluded for incomplete data (Figure 1). Before intervention, 34/48 (70.8%) patients had vancomycin ordered, and after intervention 35/48 (72.9%) had vancomycin ordered. There were 63/94 patients eligible for EGDT who had vancomycin ordered and ED arrival time recorded (29 before intervention and 34 after intervention). The median age was 60 years (range 37-90 years). In the 63 patients 31 were Caucasians and 31 were male. Patient characteristics were similar before and after intervention (Table 1).
Figure 1.
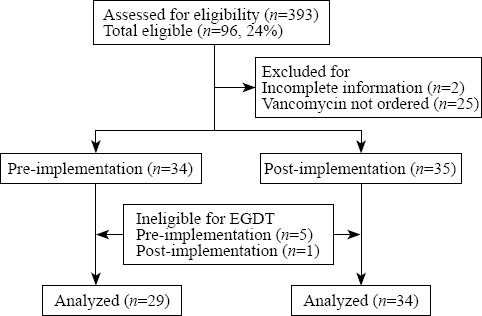
Represents the assessment of subjects for eligibility for the study. Of 393 screened subjects, 96 were eligible, 27 were excluded because they did not have complete information or vancomycin was not ordered. Six additional subjects were excluded because they were ineligible for EGDT. A total of 63 patients were analyzed. EGDT: early goal directed therapy.
Table 1.
Demographic data in median and range or frequency and percent (n=63)
Before intervention, 0/29 (0.0%) patients received vancomycin within 60 minutes from bed placement to drug administration. After intervention, 5/34 (14.7%) patients received vancomycin within 60 minutes from bed placement to drug administration (difference in proportions 14.7%, 95% CI 0.39%-30.0%, P=0.040) (Table 2).
Table 2.
Vancomycin dosing
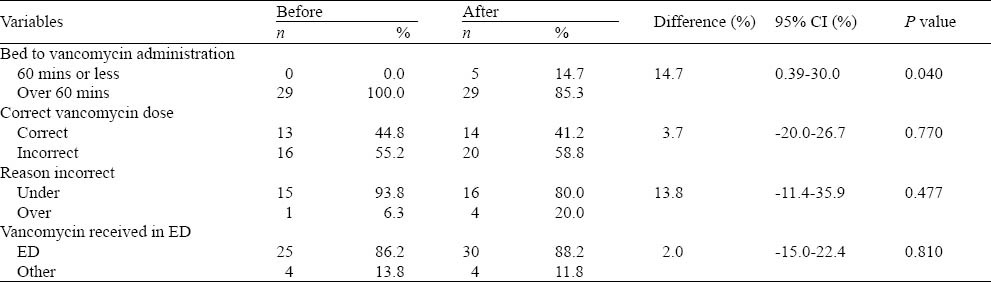
Dosing accuracy was not significantly affected by having it premixed and available in the ADS. Before intervention, 13/29 (44.8%) of patients received the correct dose of vancomycin and after intervention, 14/34 (41.2%) of patients received the correct dose of vancomycin (difference in proportions 3.7%, 95% CI -20.0%-26.7%, P=0.770). Patients with an incorrect dose were most often underdosed. Before intervention, 15/16 (93.8%) of incorrectly dosed patients were underdosed and after intervention 16/20 (80.0%) of incorrectly dosed patients were underdosed (difference in proportions 13.8%, 95% CI -11.4%-35.9%, P=0.477) (Table 2).
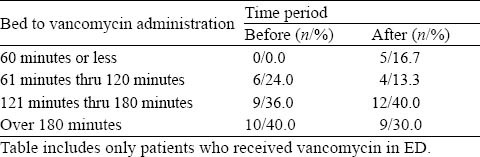
Before intervention, 25/29 (86.2%) of patients received vancomycin but still in the ED, and after intervention, 30/34 (88.2%) received vancomycin but still in the ED (difference in proportions 2.0%, 95% CI -15.0%-22.4%, P=0.810) (Table 2). Within the recommended three-hour timeframe for ED administration of antibiotics, 70% of patients received vancomycin after intervention compared with 60% of those who received vancomycin before intervention (Table 3).
Table 3.
Time intervals
DISCUSSION
Our results indicate that making vancomycin available in an ADS in the ED increased the proportion of septic patients receiving vancomycin within one hour as well as the recommended three-hour time frame. It is notable that the appropriateness of vancomycin dosing did not change as a result of the intervention, and patients were still more likely to be under-dosed when the incorrect dose was given. However, it might have been expected that given a pre-mixed dose, patients may be more likely to be given an inappropriate dose. Additionally, fewer patients received complete EGDT bundled care post-implementation. There are multifactorial reasons for nonadherence with the EGDT bundle and may be the result of the small patient sample.[18] Yet, despite this decrease, a significantly increased proportion of patients received vancomycin within one hour. A possible explanation for this discrepancy is that administration of antibiotics is one of the most frequently adhered to elements of the EGDT bundle.[19]
Whether using the more stringent one-hour goal or the ED recommendation for antimicrobial timing, both time constraints were improved with the ADS. While the absolute number and proportion of patients receiving vancomycin within one hour were small at 14.7%, which is due to the use of the more stringent timeframe; this difference was still seen at the three-hour timeframe. Despite the complex, multifactorial nature of medication administration, the use of the ADS for a single antimicrobial still showed a significant improvement. While the benefit of early antimicrobial administration in septic patients has not been conclusively proven, the results of this study have important implications for diseases in which medication timing and outcomes have a definitive association.
Beyond timing, dosing appropriateness did not change in this study. Considering the pharmacist was removed during this process change, the fact that dosing did not significantly change suggests that quality was not harmed by the use of the ADS. While dosing appropriateness was not a primary outcome of this study, this represents an important safety and effectiveness issue to be explored in future research. Just as this study explored a systematic approach to increasing timeliness of administration, future efforts should be directed at systematically increasing accuracy. While this study showed a benefit in a disease not seen on a daily basis, further studies should evaluate the introduction of multiple new medications, their use in a larger sample, and high volume medications on a daily basis in multiple disease processes.
LIMITATIONS
Despite the increase in the proportion of patients receiving vancomycin within an hour, the results of this study should be considered in light of several limitations. This study used an observational, retrospective methodology, which has the potential to result in selection bias because of the search for cases by ICD-9 codes and work-up bias. In addition, interpreting the data is limited by observations available in the chart. For example, if antibiotics are quickly available but cannot be administered owing to a limit in peripheral or central venous access, this would not be captured by our design. Similarly, multiple medications may be ordered because they are not always able to be administered simultaneously. Since the proportion of patients receiving vancomycin earlier was increased, one should consider that this intervention was directed at an isolated component of a much larger bundle of care for septic patients.
Additionally, times are subjected to recall bias and the times may be inaccurate or inconsistent. This study could be conducted prospectively with a larger sample size, thus improving the accuracy of times and limiting the biases associated with retrospective chart-based reviews.
In conclusion, the use of an automated dispensing system may reduce the times of medication administration in patients presenting to the ED.
Footnotes
Funding: This study was supported by a Resident Research Grant from the University of Cincinnati Department of Emergency Medicine, by a Research Fellowship Award from the Emergency Medicine Foundation and by an Institutional Clinical and Translational Science Award, NIH/NCRR Grant Number 5UL1RR026314-02.
Ethical approval: The paper was approved by the Ethical Committee of University of Cincinnati, Cincinnati, OH 45267, USA.
Conflicts of interest: The authors have no financial or other conflicts of interest regarding this article.
Contributors: All authors concepted, designed, prepared, edited, and reviewed the manuscript. Ward MJ and Lindsell CJ made the definition of intellectual content and clinical/experimental studies. Ward MJ, Boyd JS and Lindsell CJ did the literature search. Ward MJ, Smith CL, Walker SM, Hice JD, and Wright SW built the data acquisition. Ward MJ, Hart KW, and Lindsell CJ make the data/statistical analysis.
REFERENCES
- 1.Fonarow GC, Smith EE, Saver JL, Reeves MJ, Bhatt DL, Grau-Sepulveda MV, et al. Timeliness of tissue-type plasminogen activator therapy in acute ischemic stroke: patient characteristics, hospital factors, and outcomes associated with door-to-needle times within 60 minutes. Circulation. 2011;123:750–758. doi: 10.1161/CIRCULATIONAHA.110.974675. [DOI] [PubMed] [Google Scholar]
- 2.Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34:1589–1596. doi: 10.1097/01.CCM.0000217961.75225.E9. [DOI] [PubMed] [Google Scholar]
- 3.Lambert L, Brown K, Segal E, Brophy J, Rodes-Cabau J, Bogaty P. Association between timeliness of reperfusion therapy and clinical outcomes in ST-elevation myocardial infarction. JAMA. 2010;303:2148–55. doi: 10.1001/jama.2010.712. [DOI] [PubMed] [Google Scholar]
- 4.Services CfMaM. Overview of specifications of measures displayed on hospital compare [June 6, 2011] Available from: https://www.cms.gov/HospitalQualityInits/downloads/HospitalOverviewOfSpecs200512.pdf .
- 5.Gaieski DF, Mikkelsen ME, Band RA, Pines JM, Massone R, Furia FF, et al. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med. 2010;38:1045–1053. doi: 10.1097/CCM.0b013e3181cc4824. [DOI] [PubMed] [Google Scholar]
- 6.Dellinger RP, Levy MM, Carlet JM, Bion J, Parker MM, Jaeschke R, et al. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock: 2008. Crit Care Med. 2008;36:296–327. doi: 10.1097/01.CCM.0000298158.12101.41. [DOI] [PubMed] [Google Scholar]
- 7.Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 8.Morrell M, Fraser VJ, Kollef MH. Delaying the empiric treatment of candida bloodstream infection until positive blood culture results are obtained: a potential risk factor for hospital mortality. Antimicrob Agents Chemother. 2005;49:3640–3645. doi: 10.1128/AAC.49.9.3640-3645.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Puskarich MA, Trzeciak S, Shapiro NI, Arnold RC, Horton JM, Studnek JR, et al. Association between timing of antibiotic administration and mortality from septic shock in patients treated with a quantitative resuscitation protocol. Crit Care Med. 2011 May 12; doi: 10.1097/CCM.0b013e31821e87ab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Campaign SS. Timing to Antibiotics. 2010. [cited 2010 9/23]. Available from: http://www.survivingsepsis.org/Bundles/ Individual_Changes/Pages/improve_antibiotic_time.aspx.
- 11.De Miguel-Yanes JM, Munoz-Gonzalez J, Andueza-Lillo JA, Moyano-Villaseca B, Gonzalez-Ramallo VJ, Bustamante-Fermosel A. Implementation of a bundle of actions to improve adherence to the Surviving Sepsis Campaign guidelines at the ED. Am J Emerg Med. 2009;27:668–674. doi: 10.1016/j.ajem.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 12.Ferrer R, Artigas A, Levy MM, Blanco J, Gonzalez-Diaz G, Garnacho-Montero J, et al. Improvement in process of care and outcome after a multicenter severe sepsis educational program in Spain. JAMA. 2008;299:2294–303. doi: 10.1001/jama.299.19.2294. [DOI] [PubMed] [Google Scholar]
- 13.Gao F, Melody T, Daniels DF, Giles S, Fox S. The impact of compliance with 6-hour and 24-hour sepsis bundles on hospital mortality in patients with severe sepsis: a prospective observational study. Crit Care. 2005;9:R764–770. doi: 10.1186/cc3909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Levy MM, Dellinger RP, Townsend SR, Linde-Zwirble WT, Marshall JC, Bion J, et al. The Surviving Sepsis Campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med. 2010;38:367–374. doi: 10.1097/CCM.0b013e3181cb0cdc. [DOI] [PubMed] [Google Scholar]
- 15.Nguyen HB, Corbett SW, Steele R, Banta J, Clark RT, Hayes SR, et al. Implementation of a bundle of quality indicators for the early management of severe sepsis and septic shock is associated with decreased mortality. Crit Care Med. 2007;35:1105–1112. doi: 10.1097/01.CCM.0000259463.33848.3D. [DOI] [PubMed] [Google Scholar]
- 16.Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: dispensing and administration--2008. Am J Health Syst Pharm. 2009;66:926–946. doi: 10.2146/ajhp080715. [DOI] [PubMed] [Google Scholar]
- 17.Wright SW, Trott A, Lindsell CJ, Smith C, Gibler WB. Evidence-based emergency medicine. Creating a system to facilitate translation of evidence into standardized clinical practice: a preliminary report. (6 e1-8).Ann Emerg Med. 2008;51:80–86. doi: 10.1016/j.annemergmed.2007.04.009. [DOI] [PubMed] [Google Scholar]
- 18.Mikkelsen ME, Gaieski DF, Goyal M, Miltiades AN, Munson JC, Pines JM, et al. Factors associated with nonadherence to early goal-directed therapy in the ED. Chest. [Research Support, N.I.H., Extramural] 2010;138:551–558. doi: 10.1378/chest.09-2210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ward MJ DJ, Smith CL, Hart KW, Lindsell CJ, Gibler WB, Wright SW. Implementation of Early Goal-Directed Therapy: Which Components Are Not Performed? Ann Emerg Med. 2010;56:S58–59. [Google Scholar]


