SUMMARY
Objective
The purpose of this study is to report a case of full-arch rehabilitation on six endosseous implants loaded following the standard procedure.
Methods
An implant-prosthetic treatment was proposed to a 53-year-old woman with a total prosthesis in the upper jaw. Six implants on upper maxillary were placed keeping the upper complete denture during the osseointegration period. The implants were left submerged to allow the patient to wear removable prostheses and the prosthesis was rebase with Hydrocast to not compress the sites of healing during the osseointegration period.
The impression of implants was made with silicones for addition (VPS) with different viscosities after 8 weeks.
The final restoration was carried out taking into account the aesthetic and functional canons.
Conclusions
Correct diagnosis and accurate implant planning are key for success in implant rehabilitation.
Keywords: full-arch rehabilitation, VDO, implant supported prosthesis
Introduction
Implant-supported fixed restoration is a well-established treatment method for edentulous patients. Long-term clinical studies have shown that this type of restoration can be successful for many years (1–3). Historically, restoration of the edentulous dental arch was only possible through the use of conventional complete denture therapy and, in some cases, subperiosteal implant-retained prostheses (4, 5). While subperiosteal implants were associated with complications, such as mobility and questionable survival rates, 5–7 for years, the complete denture had been the gold standard for treatment of the edentulous dental arch.
Full-arch rehabilitation, a term used by many practitioners, has become a popular restorative option in dental settings. There have been many reports in literature on the use of full-arch, fixed (6, 7) and removable (8–12) implant-retained prostheses.
The purpose of this study is to report a case of full-arch rehabilitation on six endosseous implants loaded following the standard procedure.
Methods
A 53-year-old woman came to our attention with a total prosthesis in the upper jaw (Fig. 1). She showed no systemic pathology and was not a smoker. She was unhappy with the esthetics and the function of his prosthesis. After careful evaluation we decided to insert 6 implants on upper maxillary keeping the upper denture during the osseointegration period.
Figure 1.
Pre-operative case.
The patient was then informed about the possibility of applying an implant placement with eventual immediate loading. Such a surgical plan was to be considered under strict computer planning (Nobel Guide) but the patient decided for the standard surgical procedure.
The surgery was performed with the patient under local anesthesia with 4% mepivacaine and 1:100,000 adrenaline (Pierrel SpA, Rome, Italy) and sedation with a 1% propofol solution. Blood pressure, pulse, and oximetric monitoring were performed by the anesthetist.
A total of 6 implants were placed for maxillary rehabilitation. Nobel Biocare Replace implants were used. The implants size were (two) 3.5 × 10, (two) 4.3 × 13 and (two) 5 × 8 (Fig. 2).
Figure 2.
Six implants placed with healing abutment.
To place the implant the standard surgical procedure for Nobel Biocare Implants was followed. Implant stability was sufficient (35 N/cm measured with a torque spring) for all 6 implants.
The same upper denture was delivered and adapted to the patient the same day of implant surgery.
The implants were left submerged to allow the patient to wear removable prostheses. The pros-thesis was rebase with Hydrocast not to compress the sites of healing (Fig. 3). The sutures were 3-0 silk. Second-stage surgery was performed, and prosthetic rehabilitation was conducted. The prosthetic loading was realized at 8 weeks.
Figure 3.
The prosthesis rebased with Hydrocast.
At the preliminary appointment:
A conventional alginate impression is made and study models are cast;
A rigid custom tray is manufactured with a window cut through over the implant (see section of tray design for further detail).
At the next appointment:
The healing abutments are removed;
Appropriate impression copings are selected and fitted. These copings were splinted together intraorally to provide greater rigidity and possibly greater accuracy (Fig. 4);
The open tray is tried in; the impression copings should emerge level with the window. This permits easy removal of the impression copings, while ensuring that the copings are supported by sufficient impression material;
The window is sealed with wax;
An impression is taken in the open tray with a silicone impression material. The tips of the impression copings should be felt through the wax covering the window;
Once the impression has set, the impression copings are unscrewed through the window on the tray and the impression is removed from the mouth along with all the impression copings in place (Fig. 5);
The healing abutments are replaced.
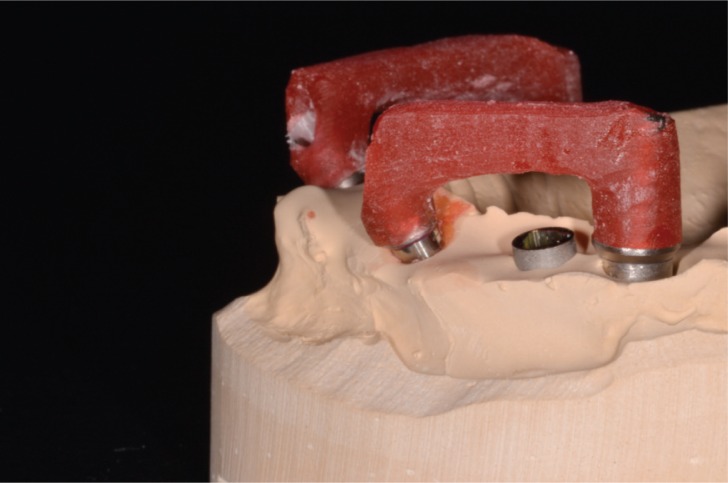
Figure 4.
Impression copings splinted together intraorally to provide greater rigidity and possibly greater accuracy.
Figure 5.
VPS Impression.
The impression of implants was made with silicones for addition (VPS) with different viscosities after merging all the impression transfer with Duralay red resin.
A recent systematic review on impression techniques showed that in situations where there are three or fewer implants, there was no difference between an open tray and closed tray approach. However, if there were four or more implants, impressions appeared more accurate with an open tray technique (13).
VDO of the patient remained unchanged. We used a compass for measuring two times the distance between the tip of the nose and the mandibular symphysis. The first time with the denture of the patient and the second time with a structure in resin mounted on four abutments previously screwed to the implants (Fig. 6).
Figure 6.
Structure in resin mounted on 4 abutments screwed to the implants.
The final restoration (Figs. 7, 8) realized in zirconia ceramic (14, 15) was carried out taking into account the aesthetic and functional canons of the most important:
centric contacts - even distribution occlusal contacts with small and centered over the implants;
eccentric contacts - anterior guidance only, distributed over multiple teeth;
angle of tooth contact - shallow as possible to minimize shear forces but still disclude posterior teeth;
jaw-to-jaw position - centric relation as defined by Dawson to be atto to control tooth contacts (16);
VDO - alter if necessary to create proper tooth form and guidance (17).
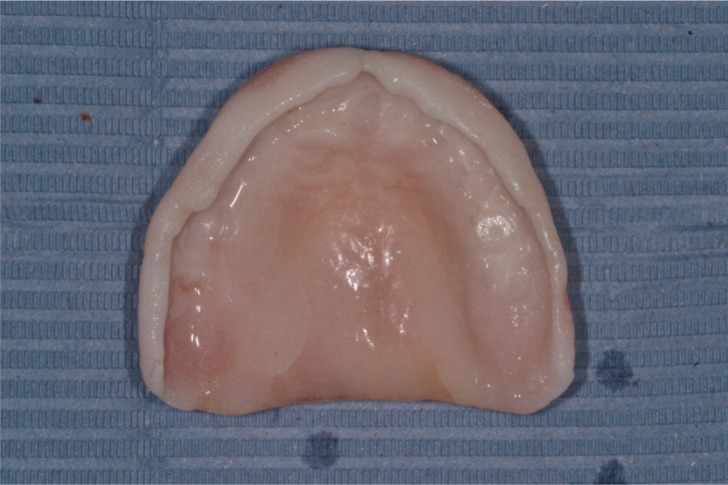
Figure 7.
Completed case 1.
Figure 8.
Completed case 2.
With these occlusal modifications, bite forces will be primarily compressive in nature to the prosthesis, the implants, and the bone. If the implants are providing any type of guidance, the stress is reduced by distributing the forces over multiple anterior teeth. By keeping the angle of tooth-contact shallow, vertical cantilevers, which are stress magnifiers, are reduced, thereby reducing stress to the implant system as well.
Conclusions
Correct diagnosis and accurate implant planning are key for success in implant rehabilitation.
Accurate impressions and meticulous attention to detail provide a foundation for successful implant prosthodontics. A comprehensive understanding of the range of prosthetic components is essential and often gained only by clinical experience.
References
- 1.Lindquist LW, Carlsson GE, Jemt T. A prospective 15-year follow-up study of mandibular fixed prostheses supported by osseointegrated implants: Clinical results and marginal bone loss. Clin Oral Implants Res. 1996;7:329. doi: 10.1034/j.1600-0501.1996.070405.x. [DOI] [PubMed] [Google Scholar]
- 2.Lemmerman KJ, Lemmerman NE. Osseointegrated dental implants in private practice: A long-term case series study. J Periodontol. 2005;76:310. doi: 10.1902/jop.2005.76.2.310. [DOI] [PubMed] [Google Scholar]
- 3.Peñarrocha-Diago MA, Maestre-Ferrín L. Immediate versus nonimmediate placement of implants for full-arch fixed restorations: a preliminary study. J Oral Maxillofac Surg. 2011 Jan;69(1):154–9. doi: 10.1016/j.joms.2010.07.083. [DOI] [PubMed] [Google Scholar]
- 4.Bodine RL. Prosthodontic essentials and an evaluation of the mandibular subperiosteal implant denture. J Amer Dent Assoc (1939) 1955;51(6):654–64. doi: 10.14219/jada.archive.1955.0260. [DOI] [PubMed] [Google Scholar]
- 5.Garefis PN. Full mouth reconstruction with dental implants. J Oral Implantol. 1979;8(4):563–73. [PubMed] [Google Scholar]
- 6.Kaptein ML, De Putter C, De Lange GL, Blijdorp PA. A clinical evaluation of 76 implant-supported super-structures in the composite grafted maxilla. J Oral Rehab. 1999;26(8):619–623. doi: 10.1046/j.1365-2842.1999.00444.x. [DOI] [PubMed] [Google Scholar]
- 7.Fischer K, Stenberg T. Three-year data from a randomized, controlled study of early loading of single-stage dental implants supporting maxillary full-arch prostheses. Int J Oral Maxillo Implants. 2006;21(2):245–52. [PubMed] [Google Scholar]
- 8.Kaptein ML, De Putter C, De Lange GL, Blijdorp PA. A clinical evaluation of 76 implant-supported super-structures in the composite grafted maxilla. J Oral Rehab. 1999;26(8):619–23. doi: 10.1046/j.1365-2842.1999.00444.x. [DOI] [PubMed] [Google Scholar]
- 9.Sullivan DY, Sherwood RL, Porter SS. Long-term performance of Osseotite implants: a 6-year clinical follow-up. Compend Contin Edu Dent. 2001;22(4):326–8. 30, 32–4. [PubMed] [Google Scholar]
- 10.Ferrigno N, Laureti M, Fanali S, Grippaudo G. Along-term follow-up study of non-submerged ITI implants in the treatment of totally edentulous jaws. Part I: Ten-year life table analysis of a prospective multicenter study with 1286 implants. Clinical Oral Implants Research. 2002;13(3):260–73. doi: 10.1034/j.1600-0501.2002.130305.x. [DOI] [PubMed] [Google Scholar]
- 11.el-Charkawi H. The use of precision attachments in a lower full-arch rehabilitation with osseointegrated implants - a clinical report. Egyptian Dent J. 1994;40(4):919–922. [PubMed] [Google Scholar]
- 12.Kramer A, Weber H, Benzing U. Implant and prosthetic treatment of the edentulous maxilla using a bar-supported prosthesis. Int J Oral & Maxillo Implants. 1992;7(2):251–5. [PubMed] [Google Scholar]
- 13.Lee H, So JS, Hochstedler JL, Ercoli C. The accuracy of implant impressions: a systematic review. J Prosthet Dent. 2008;100:285–291. doi: 10.1016/S0022-3913(08)60208-5. [DOI] [PubMed] [Google Scholar]
- 14.Gargari M, Gloria F, Cappello A, Ottria L.Strength of zirconia fixed partial dentures: review of the literature ORAL & Implantology III42010October–December15–24 [PMC free article] [PubMed] [Google Scholar]
- 15.Gargari M, Gloria F, Napoli E, Pujia AM. Zirconia: cementation of prosthetic restorations. Literature review. ORAL & Implantology. 2010 Oct-Dec;III(4) [PMC free article] [PubMed] [Google Scholar]
- 16.Dawson P. Evaluation, Diagnosis and Treatment of Occlusal Problems. 2nd ed. St. Louis: CV Mosby; 1989. pp. 28–55. [Google Scholar]
- 17.Gittelson Glenn L. Vertical Dimension of Occlusion in Implant Dentistry: Significance and Approach. Implant Dent. 2002;11:33–40. doi: 10.1097/00008505-200201000-00012. [DOI] [PubMed] [Google Scholar]