Abstract
Background: Esophagectomy is considered to be the main treatment for esophageal malignancies. Among the different methods, transhiatal approach can cause less damage to patients and is widely used; however, manipulation of esophagus result in heart rate and blood pressure variations. The aim of this study was to investigate changes in blood pressure and heart rhythm during transhiatal esophagectomy.
Methods: This prospective study was performed on 51 patients with esophageal cancer admitted for transhiatal esophagectomy. Anesthesia method was similar for all the patients. Blood pressure and heart rhythm were monitored in three stages; 30 min before, during, and up to 24 hours after mediastinal manipulation (blood pressure, every minute, and heart rhythm, continuously, were controlled during manipulation). Collected data were analyzed. Using SPSS statistical software
Results: Over the first 5 minutes, systolic blood pressure declined significantly compared with preoperation time (p=0.001). Diastolic pressure declared from to 2 to 5 minutes postoperatively (p=0.001). Before mediastinal manipulation, AF was observed in 3 and PVC in 5 patients; whereas, arrhythmia was not found in other 43 patients. During mediastinal manipulation, 1, 25 and 10 patients developed AF, bradycardia and PVC respectively, and 4 patients had bradycardia and PVC, simultaneously. Arrhythmia was not detected in 11 patients. Before manipulation, arrhythmia was seen in 15.7% of patients which increased to 78.4% during operation time (p=0.0001).
Conclusion: According to the findings of this study the development of hypotension and arrhytmia are common during mediastinal manipulation. These changes recover after surgical procedure without treatment. If the alterations remain after surgery, remedial actions will be required.
Key Words: Esophageal neoplasm, Transhiatal Esophagectomy, Blood pressure, Heart rate
Esophagectomy is the main treatment for esophageal malignancies, esophagogastric junction and some benign esophageal diseases (1). Among the different methods which have been explained for esophageal cancer, transhiatal approach causes less damage compare to thoractomy (2-4). Transhiatal approach was first explained by the German anatomist, Denk, in 1913 (1, 5). Afterwards, several reports have confirmed the safety of this approach for the treatment of benign and malignant esophageal diseases (1). However, this method may be associated with several difficulties during anesthesia. During the procedure, the stomach and the esophagus are released through the midline abdominal incision above the umbilicus (it is done by a blind manipulation through the posterior mediastinum); stomach is released and passed through the posterior mediastinum. Following esophagus resection, cervical esophagogastric anastomosis is possible (1). During manipulation the surgeon's hand causes unavoidable atrial pressure and heart rotation, leading to arterial hypotension and arrhythmia (2).
On the other hand, esophagus resection can contribute to vagus nerve stimulation, bradycardia and other types of arrhythmia and even rarely cardiac arrest (6). The surgeon's accidental touch of pericardium can also be involved in the creation of arrhythmia (7). The severity of hemodynamic disorders is proportional to the duration of mediastinal manipulation (7), and to reduce such abnormalities, coordination between the surgeon and anesthesiologist seems to be necessary (7-10). Although changes in blood pressure and arrhythmia during mediastinal manipulation are routinely seen, determining the type of arrhythmia and blood pressure levels has only been investigated in few studies for middle esophageal cancers. The aim of this study is to investigate changes in blood pressure and heart rhythm during transhiatal esophagectomy.
Methods
This prospective study was conducted on 51 patients with esophageal cancer referring to Beheshti Hospital of Babol for transhiatal esophagectomy. The patients with severe heart dysfunction, severe obstructive or constrictive pulmonary disease, electrolyte disorder, digitalin drugs or ACE inhibitors consumption were excluded from the study.Half an hour before surgery, during, and two hours after the operation, the patients' blood pressure, pulse oximetry, temperature and ECG were monitored. Urinary catheter and CV (central vein) line were used to control urinary output and central venous pressure respectively.
Controlling blood pressure, heart rhythm and ABG were performed in three steps; 30 min before, during, and up to 24 hours after mediastinal manipulation (blood pressure, every minute, and heart rhythm, continuously, were monitored during manipulation). Anesthesia method was same for all the patients. In pre-induction, midazolam (0.03 mg/kg) and morphine (0.1 mg/kg), for induction, thiopental (5 mg/kg) and atracurium (0.5 mg/kg); and to maintain anesthesia, isoflurane (1-1.5%), O2 (50%) and N2O (50%) were used. To collect data, checklists containing the following items was applied; age, sex, weight, smoking, serum albumin, potassium and sodium levels before surgery, blood pressure before, during (every minutes) and 24 hours after the operation, preoperative heart rate and ECG, FEV1 on spirometry, EF (ejection fraction) on echocardiography, intra-operative amount of IV fluid intake, tumor location, operation time (in minutes), duration of mediastinal manipulation, arrhythmia before, during, and up to 24 hours after mediastinal manipulation, type and duration of arrhythmia, PaO2 and PaCO2 and bicarbonate during esophagectomy, duration of hospital stay, post-operative complications and overall mortality within 30 days, existence and the amount of intra-operative bleeding, the need for blood transfusion and type of tumor pathology. Hypotension is defined as a 20% decrease in systolic blood pressure from the baseline. The data were collected, coded and after being logged in designed tables, were statistically analyzed by SPSS version. ANOVA, Post Hoc Test and repeated measurements were used when appropriate
Results
Among the 51 cases, 60.8% were males and 39.2% females. The mean age of the patients was 66±8.5 years (ranged 48- 82 years). The patients' mean weight was 62.94±11.06 kg (ranged 44-85 kg). Ten (19.9%) patients were smokers. Tumor location in 6 (11.8%) patients was in the proximal one-third of esophagus, in the 31 (60.8%) in the middle esophagus, and 8 (15.7%) patients lower esophagus and 6 (11.8%) in the cardia region. The mean duration of surgery was 160.1±31 minutes. The mean operation duration for cardia tumors was significantly more than middle (p=0.004) and distal (p=0.008) esophageal regions. The mean serum Na+ was 139.94±2.97 mEq/L, K+ 4.09±0.23 mEq /L and albumin 4.14±0.48 gr/dl. In all the patients, serum sodium, potassium and albumin levels were within normal ranges.
Before surgery, the mean systolic blood pressure was 140.78±14.95 mmHg (ranged 110-170 mmHg), diastolic blood pressure was 80.98±7.94 mmHg (ranged 60-90 mmHg) and heart rate was 82.73±6.78 (ranged 72 to 100). The mean calculated EF (ejection fraction) was 56.45%±5.52 (ranged 45 to 60%) and for FEV1 was 2.39±0.49 litter (ranged 1.3-3.3 litters).
Before surgery, 3 (5.9%) patients had AF, 4 (7.8%) PVC and other 44 (86.3%) patients had sinus rhythm. Before mediastinal manipulation, 3 (5.9%) patients showed AF, 5 (9.8%) PVC and other 43 (84.3%) had no sign of arrhythmia. The mean systolic blood pressure was 110.39±11.99 mmHg (ranged 90-160 mmHg) and diastolic blood pressure was 67.35±7.71 mmHg (ranged 60-85 mmHg).
The mean duration of mediastinal manipulation was 13.86±4.59 min (ranged 5 to 25 min). During manipulation, 1 (2%), 25 (49%) and 10 (19.6%) patients developed AF, bradycardia and PVC respectively, and 4 (7.8%) patients, bradycardia and PVC simultaneously. Arrhythmia was not observed in 11 (21.6%) patients.
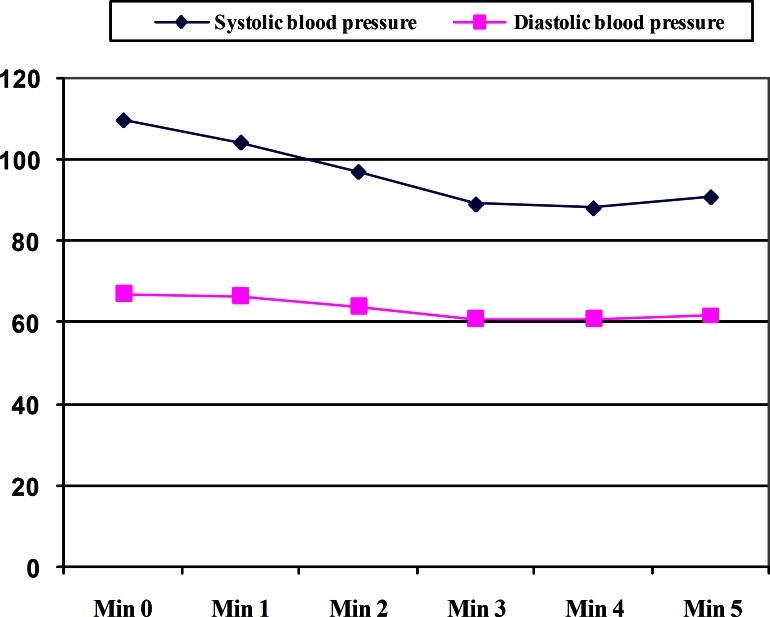
Table 1 shows comparison between arrhythmia during and before mediastinal manipulation. Prior to manipulation, arrhythmia was observed in 15.7% of patients while the percentage reached to 78.4 after the manipulation (p=0.0001). During mediastinal manipulation, the mean systolic blood pressure in the first, second, third, fourth and fifth minutes was 104.51±7.83 mmHg, 97.25±8.74 mmHg, 89.22±9.35 mmHg, 88.24±9.74 mmHg and 90.98±10.05 mmHg, respectively (p=0.000). Every 5 minutes, the systolic blood pressure was significantly lower than the level before manipulation (figure 1).
Table1.
Comparison between pre- and during manipulative arrhythmia
|
Without
arrhythmia |
AF | Bradycardia | PVC |
Bradycardia
and PVC |
|
|---|---|---|---|---|---|
| Pre- manipulation arrhythmia | 43 (84.3) | 3 (5.9) | 0 | 5 (9.8) | 0 |
| During manipulation arrhythmia | 11 (21.6) | 1 (2) | 25 (49) | 10 (19.6) | 4 (7.8) |
Figure1.
Alteration in systolic and diastolic blood pressure during the first 5 minutes of manipulation period
During the mediastinal manipulation, the mean diastolic blood pressure in the first minute was 66.67±6.83 mmHg, the second minute 64.12±6.06 mmHg, the third minute 60.98±5.75 mmHg, the fourth minute 60.98±5.01 mmHg and in the fifth minute 61.76±5.18 (p=0.0001). In minutes 2, 3, 4 and 5, diastolic blood pressure was also noticeably lower than before manipulation (figure 1).
Changes in systolic (p=0.420) and diastolic (p=0.115) blood pressure did not show meaningful difference between the two sexes. Also, blood pressure alterations were not age-related. Furthermore, the duration of mediastinal manipulation was not related to systolic and diastolic blood pressure. Changes in cardiac rhythm before and during mediastinal manipulation did not differ in the two sexes and tumor site and it was also unrelated to age and manipulation duration. The mean intra-operative HCO3 was 20.78±1.56 mmol (18 to 23), PaO2 251.39±26.19 mmHg (180 to 300) and PaCO2 28.98±1.27 mmHg (25 to 32).
The least amount of intra-operative bleeding was 100 cc, the highest level 500 cc and the mean was 270.59 ± 83.77ml. No patient required blood transfusion. After surgery, eight (15.7%) developed AF with an average of 160.00±120.00 minutes, one (2%) bradycardia over a one day period, nine (17.6%) tachycardia with an average of 218.89±153.13 minutes and 6 (11.8%) PVC (mean 170.00±130.84 min). Arrhythmia after surgery was seen in twenty seven (52.9%) (table 2).
Table 2.
Comparison between intra- and post-manipulative arrhythmia
|
Without
arrhythmia |
AF | Bradycardia and PVC | Bradycardia | Tachycardia | PVC | |
|---|---|---|---|---|---|---|
| Post-manipulation arrhythmia | 27 (51.9) | 8 (15.7) | 0 | 1 (2) | 9 (17.6) | 6 (11.8) |
| During manipulation Arrhythmia | 11( 21.6) | 1 (2) | 4 (7.8) | 25 (49) | 0 | 10 (19.6) |
There was no significant relation between post-operative and intra-operative arrhythmia (p<0.05). Following surgery, systolic and diastolic blood pressures were measured every 6 hours during a 24-hour period. In all patients, both systolic and diastolic blood pressures were back to the level before surgery.
The minimum, the maximum and the mean duration of hospital stay was 6, 10 and 7.18±1.05 days, respectively. In pathological studies, 44 (86.3%) were SCC and seven (13.7%) were adenocarcinoma. Samples after surgery, 37 patients (72.6%) did not have any major complications. One patient (1.9%) died postoperatively.
Discussion
In this study, every 5 minutes, the systolic blood pressure was significantly lower than the level before manipulation. In minutes 2, 3, 4 and 5, diastolic blood pressure was also noticeably lower than pre-manipulative level. In an only one study, similar to our study done by Malhotra et al. hypotension was examined during mediastinal manipulation, Hypotension and during 15 minutes mediastinal manipulation, hypotension occurred in 15 out of 20 cases. In their study, there was a linear relationship between hypotension period and duration of mediastinal manipulation. Similar to our study, all the patients' blood pressure returned to normal blood pressure following the surgeon's hand removal from the mediastinum. In the present study, before entering the mediastinum, 3 patients (5.9%) showed AF, 5 patients (9.8%) PVC and other 43 patients displayed (84.3%) no arrhythmia. During manipulation, 1 (2%), 25 (49%) and 10 (19.6%) patients developed AF, bradycardia and PVC respectively, and 4 (7.8%) patients, bradycardia and PVC simultaneously. Arrhythmia was not observed in 11 (21.6%) patients. Before manipulation, arrhythmia was found in 15.7% of patients while the percentage reached to 78.4 after manipulation (p=0.000). Malhotra et al. reported arrhythmia in two patients (out of 20) before and 13 patients during the manipulation (p<0.01). Arrhythmia was transient and unrelated to duration or degree of blood pressure. Post-operative arrhythmia was detected in two patients (11).
In a study done by Kuppusamy et al. intra-operative arrhythmia was observed in 11 patients (12). Patti et al. reported atrial arrhythmia in 14 patients (out of 44) and all cases were treated well.
During transhiatal esophagectomy, the surgeon's hand, separating esophagus from mediastinal surrounding tissues (a blind manipulation), pressures atrium inevitably, leading to hypotension and arrhythmia (2). The separation per se can be followed by a significant stimulation of vagus nerve and eventuate in bradyarrythmia and even rarely cardiac arrest (6). The surgeon’s accidental touch of pericardium can also be involved in creating arrhythmia. Only by careful monitoring of arterial blood pressure, an anesthesiologist is able to judge an acceptable duration for insult or recommend the surgeon to stop. Heart refill is usually fast and causes rapid reconstruction of arterial pressure; however, prolonged and severe hypotension can often result in severely impaired heart function, such as impaired coronary blood flow (11).
The patients with cardiac and pulmonary diseases were excluded from the study, because the present investigation was designed to determine the exclusive effect of mediastinum manipulation.
Since hypotension and arrhythmia may be dangerous for the patients with heart disease, the effect of mediastinal manipulation would be considerable in these cases.
In the study done by Patti et al. on 44 patients, which was conducted with a similar purpose and to determine the effect of transhiatal esophagectomy on cardiac and pulmonary function, the mean duration of hypotension was more in patients with heart disease (2).
Furthermore, HCO3, PaO2, PaCO2 and electrolytes were measured in our study. Since there was not any sign of hypoxia, hypercapnia and electrolyte disturbances in patients, these factors have not been mentioned as the causes of arrhythmia. Mediastinal manipulation was done by one surgeon in all patients in order to reduce the related errors to a minimum.
Taken together, according to the findings of the present study, the severity of arrhythmia and hypotension during mediastinal manipulation is considerable; however, these changes are usually transient and improve after manipulation. Therefore, if these alterations remain after surgery, therapeutic interventions will be required.
Acknowledgments
We would like to thank the staff of the Clinical Research Development Center of Shahid Beheshti Hospital for their help and also to all the patients for their cooperation.
Funding: This project was fully sponsored by the Research Center of Babol University of Medical Sciences with grant number of (30/3078 Date 2009/04/14).
Conflict of Interest: We have no conflict of interest in this article.
Authors' Contribution: NN and PA designed the study and wrote the paper. ASS and AYS analyzed data and literature review. All authors read and approved the final manuscript.
References
- 1.Orringer MB. Transhiatal esophagectomy. In: Patterson GA, Pearson FG, Cooper JD, et al., editors. Pearson's thoracic & esophageal surgery. 3rd ed. Philadelphia: Churchill Livingstone; 2008. pp. 563–83. [Google Scholar]
- 2.Black AMS, Prys-Roberts C. Anesthesia for gastrointestinal surgery. In: Prys-Roberts C, Brown JrBR, editors. Oxford International practice of anesthesia. 1st ed. Oxford, UK: Butter Worth-Heinemann; 1996. pp. 1–15. [Google Scholar]
- 3.Law SY, Fok M, Wei WI, et al. Thoracoscopic esophageal mobilization for pharyngolaryngoesophagectomy. Ann Thorac Surg. 2000;70:418–22. doi: 10.1016/s0003-4975(00)01402-8. [DOI] [PubMed] [Google Scholar]
- 4.Sia AT. A preliminary report on anesthesia for thoracoscopic oesophagectomy. Med J Malaysia. 1997;52:433–7. [PubMed] [Google Scholar]
- 5.Denk W. Zur Radikaloperation des Oesophaguskarfzinoms. Z Chir. 1913;40:1065–8. [Google Scholar]
- 6.Amar D, Burt ME, Bains MS, Leung DH. Symptomatic tachydysrhythmias after esophagectomyincidence and outcome measures. Ann Thorac Surg. 1996;61:1506–9. doi: 10.1016/0003-4975(96)00111-7. [DOI] [PubMed] [Google Scholar]
- 7.Patti MG, Wiener-Kronish JP, Way LW, Pellegrini CA. Impact of transhiatal esophagectomy on cardiac and respiratory function. Am J Surg. 1991;162:563–6. doi: 10.1016/0002-9610(91)90109-q. [DOI] [PubMed] [Google Scholar]
- 8.Orringer MB. Transhiatal esophagectomy without thoracotomy. In: Zuidema GD, Yes CJ, editors. Surgery of the alimentary tract. 5th ed. Philadelphia, PA: WB Saunders; 2002. pp. 407–42. [Google Scholar]
- 9.Yakoubian K, Bougeois B, Marty J, Marmuse JP, Desmonts JM. Cardiovascular responses to manual dissection associated with transhiatal esophageal resection. J Cardiothorac Anesth. 1990;4:458–61. doi: 10.1016/0888-6296(90)90291-m. [DOI] [PubMed] [Google Scholar]
- 10.Katariya K, Harvey JC, Pina E, Beattie EJ. Complications of transhiatal esophagectomy. J Surg Oncol. 1994;57:157–63. doi: 10.1002/jso.2930570305. [DOI] [PubMed] [Google Scholar]
- 11.Malhotra SK, Kaur RP, Gupta NM, et al. Incidence and types of arrhythmias after mediastinal manipulation during transhiatal esophagectomy. Ann Thorac Surg. 2006;82:298–302. doi: 10.1016/j.athoracsur.2006.02.041. [DOI] [PubMed] [Google Scholar]
- 12.Kuppusamy MK, Chance FD, Helman JD, et al. Assessment of intra-operative haemodynamic changes associated with transhiatal and transthoracic oesophagectomy. Eur J Cardiothorac Surg. 2010;38:665–8. doi: 10.1016/j.ejcts.2010.05.002. [DOI] [PubMed] [Google Scholar]