Abstract
Video-assisted thoracic surgery (VATS) is a minimally invasive technique that has many advantages in postoperative pain and recovery time. Because of its advantages, VATS is one of the surgical techniques widely used in patients with lung cancer. Most surgeons perform VATS for lung cancer with three or more incisions. As the technique of VATS has evolved, single-port VATS for lung cancer has been attempted and its advantages have been reported. We describe our experiences of VATS for lung cancer with a single incision in this report.
Keywords: Video-Assisted thoracic surgery, Lung neoplasms, Lobectomy
CASE REPORT
Three cases of single-port VATS were performed for lung cancer in Haeundae Paik Hospital. The characteristics of the patients and surgical procedures are described in Table 1. Preoperatively, needle biopsy was performed in all of the patients, and lung cancer was confirmed by microscopic examination.
Table 1.
Summaries of characteristics of patients and operative procedures
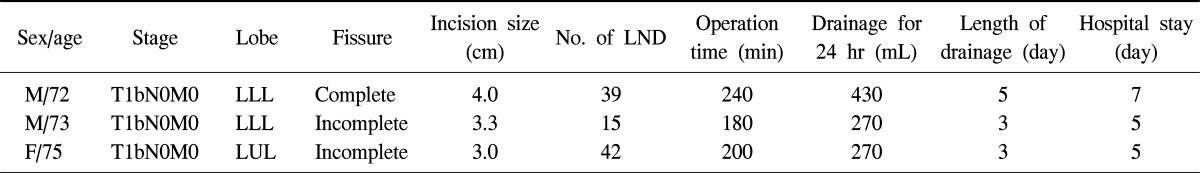
LND, lymph nodes dissection; LLL, left upper lobe; LUL, left lower lobe.
Under general anesthesia, the patient was placed in a lateral decubitus position and one lung ventilation was performed. A 3- to 4-cm incision was made in the 6th intercostal space on the anterior axillary line. The soft tissue and intercostal muscles were retracted with an X-small Alexis (Applied Medical, Rancho Santa Margarita, CA, USA) wound retractor for securing the intercostal space (Fig. 1). A 5-mm, 30° thoracoscope (Karl Storz endoscope; Karl Storz, Tuttlingen, Germany) was used in all of the patients. There was no pleural adhesion in any of the patients. Complete fissure was found in one case and incomplete fissure in two cases. Optimal surgical vision was achieved with pulmonary traction using endoscopic ring forceps. The pulmonary vessels and bronchus were dissected with a 5-mm endoscopic grasper, spatula-shaped electrocautery, and 5-mm endoscopic harmonic scalpel (Harmonic Ace; Ethicon Endo-Surgery, Cincinnati, OH, USA). First, the pulmonary veins were divided, and then branches of the pulmonary artery and bronchus were divided. The pulmonary veins and bronchus were divided with endoscopic flexible linear staplers (Ethicon Echelon Flex; Ethicon Endo-Surgery) in all cases. The branches of pulmonary artery were also divided with endoscopic linear staplers in two left lower lobe cases. In a left upper lobe case, the segmental arteries were divided at the level of the proximal portion with endoscopic scissors after clipping with hemoclips (Hem-o-lok; Teleflex Medical Co., Westmeath, Ireland) because optimal angulation could not be achieved for stapling with endoscopic linear staplers. In the patients with incomplete fissure, the fissure was divided with an endoscopic linear stapler and harmonic scalpel. After lobectomy, the resected lobe was removed using a protective bag in all cases. Routine systematic mediastinal and hilar lymph node dissection was performed with a harmonic scalpel in all cases. The lymph nodes, including perinodal tissue, were removed. In all of the cases, the lower paratracheal (no. 4), subaortic (no. 5), paraaortic (no. 6), subcarinal (no. 7), lower paraesophageal (no. 8), inferior pulmonary ligament (no. 9), hilar (no. 10), interlobar (no. 11), and lobar (no. 12) nodes were removed. At the end of the procedure, a 24-French chest tube was placed in the posterior part of the single incision (Fig. 2).
Fig. 1.
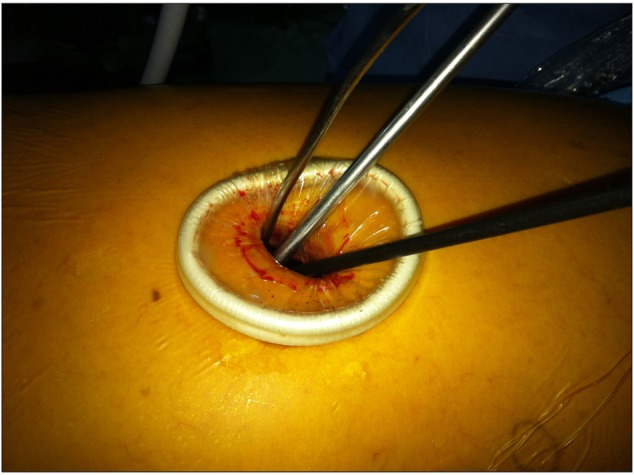
Surgical incision.
Fig. 2.

Postoperative surgical wound.
The mean operation time was 206.7±30.6 minutes. The mean duration of the chest tube drainage was 3.7±1.2 days and mean amount of chest tube drainage for the initial 24 hours was 323±92.4 mL. The mean length of the hospital stay was 5.7±1.2 days.
DISCUSSION
VATS is a minimally invasive technique that has advantages with regard to postoperative pain and respiratory function when compared with conventional thoracotomy [1]. As the technique of VATS evolved, minimally invasive major pulmonary resection, such as lobectomy and pneumonectomy, became possible. VATS lobectomy was initially reported in 1993 [2,3].
Generally, most surgeons have performed VATS pulmonary resection with three or more incisions [1,4]. Recently, single-port VATS has been attempted and its advantages have been reported. Some authors have reported that one of advantages of single-port VATS was less postoperative pain because only one intercostal space was involved [1,5]. Salati et al. [6] reported that there was less postoperative pain and fewer cases of paresthesia in patients who underwent single-port VATS than who underwent the traditional three-port VATS. However, most cases of single-port VATS have been limited to diagnostic purposes or minor pulmonary resection. Gonzalez et al. [1] first reported the outcomes of single-port VATS lobectomy in 2010. They performed a VATS lobectomy for lung cancer through only one incision. The size of the incision was about 4 cm. The resected lobe was removed through this incision, and a single chest tube was placed in the posterior part of the incision. They reported that there was no difference in postoperative results or operation time between single-port VATS lobectomy and three-port VATS lobectomy. They also reported that a systematic lymph node dissection was possible [1,7].
In Haeundae Paik Hospital, three single-port VATS lobectomies for lung cancer have been performed. Systematic lymph node dissection was possible to perform similarly to three-port VATS lobectomy. The mean operation time was 206.7 minutes. Compared with the mean operation time of the three-port VATS lobectomy for lung cancer in Haeundae Paik Hospital (190.0 minutes), there was no significant difference. However, there was no statistical significance because the number of patients who underwent single-port VATS lobectomy was very small. With the accumulation of experience, it should be possible to shorten the operation time.
Some authors have reported that VATS left upper lobectomy is the most difficult and challenging major pulmonary resection because of the branching pattern of the pulmonary artery [8]. Gonzalez-Rivas et al. [7] reported that single-port VATS left upper lobectomy was the most difficult. They recommended using hemoclips to divide the pulmonary vessels. In our left upper lobectomy case, optimal angulation for stapling the vessels could not be achieved. We were able to perform the left upper lobectomy using hemoclips.
When we performed the single-port lobectomies, the most difficult aspect of the procedure was optimal lung exposure and stapling the pulmonary vessels. Using a 30° thoracoscope, flexible stapler, and hemoclips would be helpful in solving these problems.
We prefer to make a single port in the 6th intercostal space on the anterior axillary line. If the single port is made above the 6th intercostal space, investigating the lower lobe might be difficult. If the single port is made below the 6th intercostal space, endoscopic instruments might not be able to reach the pulmonary apex. Therefore, manipulation of the pulmonary apex might be difficult. The intercostal space on the anterior axillary line is wider than the space on the mid- or posterior axillary line, which could make the surgical procedure easier. In our cases, there was less postoperative pain in the patients with a single-port on the anterior axillary line than in the patients with a port on the mid- or posterior axillary line. Through more experience, determination of the appropriate location for the single incision for each lobe will be important.
In conclusion, we successfully used single-port VATS to treat lung cancer in three patients. Nevertheless, to evaluate the feasibility and advantages of single-port VATS lobectomy for lung cancer, more experience, including right side lobectomies, will be required in well selected patients.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Gonzalez D, Paradela M, Garcia J, Dela Torre M. Single-port video-assisted thoracoscopic lobectomy. Interact Cardiovasc Thorac Surg. 2011;12:514–515. doi: 10.1510/icvts.2010.256222. [DOI] [PubMed] [Google Scholar]
- 2.Roviaro G, Varoli F, Rebuffat C, et al. Major pulmonary resections: pneumonectomies and lobectomies. Ann Thorac Surg. 1993;56:779–783. doi: 10.1016/0003-4975(93)90979-r. [DOI] [PubMed] [Google Scholar]
- 3.Kirby TJ, Mack MJ, Landreneau RJ, Rice TW. Initial experience with video-assisted thoracoscopic lobectomy. Ann Thorac Surg. 1993;56:1248–1252. doi: 10.1016/0003-4975(93)90661-z. [DOI] [PubMed] [Google Scholar]
- 4.Shigemura N, Akashi A, Nakagiri T, Ohta M, Matsuda H. Complete versus assisted thoracoscopic approach: a prospective randomized trial comparing a variety of video-assisted thoracoscopic lobectomy techniques. Surg Endosc. 2004;18:1492–1497. doi: 10.1007/s00464-003-8252-4. [DOI] [PubMed] [Google Scholar]
- 5.Rocco G, Martin-Ucar A, Passera E. Uniportal VATS wedge pulmonary resections. Ann Thorac Surg. 2004;77:726–728. doi: 10.1016/S0003-4975(03)01219-0. [DOI] [PubMed] [Google Scholar]
- 6.Salati M, Brunelli A, Rocco G. Uniportal video-assisted thoracic surgery for diagnosis and treatment of intrathoracic conditions. Thorac Surg Clin. 2008;18:305–310. vii. doi: 10.1016/j.thorsurg.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez-Rivas D, de la Torre M, Fernandez R, Mosquera VX. Single-port video-assisted thoracoscopic left upper lobectomy. Interact Cardiovasc Thorac Surg. 2011;13:539–541. doi: 10.1510/icvts.2011.274746. [DOI] [PubMed] [Google Scholar]
- 8.Sawada S, Komori E, Yamashita M. Evaluation of video-assisted thoracoscopic surgery lobectomy requiring emergency conversion to thoracotomy. Eur J Cardiothorac Surg. 2009;36:487–490. doi: 10.1016/j.ejcts.2009.04.004. [DOI] [PubMed] [Google Scholar]


