Abstract
Thoracoscopic needle aspiration is a good alternative for a centrally-located solitary pulmonary nodule (SPN) suspected of being lung cancer without severe pleural adhesion. The authors report the technique of thoracoscopic needle aspiration biopsy in a SPN just in the medial aspect of the truncus anterior pulmonary artery and the right upper lobe bronchus.
Keywords: Biopsy, needle; Lung neoplasms; Solitary pulmonary nodule; Thoracoscopy
INTRODUCTION
Thoracoscopic needle aspiration biopsy has the greatest utility for the diagnosis of peripheral solitary pulmonary nodules (SPNs) that are suspected of being lung cancer. However, for centrally-located SPNs adjacent to major vessels, open thoracotomy is usually performed to obtain pathologic specimens. The authors report the technique of thoracoscopic needle aspiration biopsy for a centrally-located SPN.
TECHNIQUE
Chest computed tomography (CT) scans showed an SPN 2.5 cm in size in just the medial aspect of the truncus anterior pulmonary artery and right upper lobe bronchus with no evidence of lymph node enlargement in the mediastinum (Fig. 1). A double-lumen endotracheal tube was inserted under general anesthesia, and the patient was placed in the right lateral position. A 5-mm thoracoscopic port was made at the 6th intercostal space on the mid-axillary line and two 5-mm ports for thoracoscopic forceps and the aspiration needle were made at the 5th intercostal space on the anterior and posterior axillary lines. After a nodule was localized by palpation with the thoracoscopic forceps, a tumor biopsy specimen was obtained using a 5-mm endobiopsy aspiration cannula (Wisap, Munchen, Germany) (Fig. 2).
Fig. 1.
Chest computed tomography scans showing a 2.5-cm nodule (arrow) in just the medial aspect of the truncus anterior pulmonary artery and the right upper lobe with no evidence of lymph node enlargement in the mediastinum.
Fig. 2.
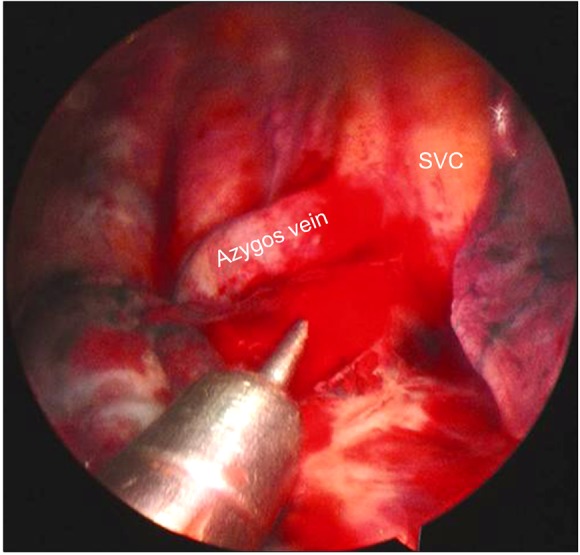
A 5-mm endobiopsy aspiration needle was introduced into the mass. SVC, superior vena cava.
The specimen was Giemsa-stained and examined cytologically, and within 30 minutes the pathologic report revealed adenocarcinoma. His clinical stage was T3N0M0 (stage IIb). Right upper lobectomy with mediastinal lymph node dissection was performed through video-assisted thoracoscopic surgery on the spot.
In this case, the patient complained of intermittent blood tinged-sputum of 2 weeks duration, but bronchoscopy failed to reveal the lesion and percutaneous needle aspiration could not be done due to its location. The pathologic diagnosis was T3N2M0 (stage IIIa). The patient was discharged uneventfully on the eighth postoperative day. During 3 months of follow-up he was administered three cycles of adjuvant chemotherapy.
DISCUSSION
The diagnosis of SPN is one of the most common problems encountered by physicians treating diseases of the chest. Low-suspicion lesions are frequently followed up by serial radiographs. However, SPNs with shapes resembling carcinoma and arising in patients with a smoking history are highly likely to be lung cancer and require an urgent definitive diagnosis. Larger central lesions lend themselves to bronchoscopic sampling, whereas smaller, peripheral lesions are commonly approached by percutaneous fine-needle aspiration under radiographic guidance [1].
Percutaneous needle aspiration has a relatively low sensitivity versus thoracoscopic lung biopsy and it is not helpful at avoiding open lung biopsy because a negative result does not guarantee benignity [2,3]. Thoracoscopic needle aspiration is a procedure intermediate between thoracoscopic lung biopsy and percutaneous needle biopsy. It can save surgical time, reduce costs, yields more information to pathologist compared with thoracoscopic lung biopsy [4]. These advantages have encouraged the use of thoracoscopic needle aspiration for the rapid diagnosis of indeterminate peripheral SPNs.
In cases of a centrally-located SPN with a pathology not revealed by bronchoscopy and located too close to major vessels or structures to obtain a specimen by percutaneous needle aspiration or thoracoscopic or open lung biopsy, needle aspiration through exploratory thoracotomy provides a means of confirming pathology. Thoracoscopic needle aspiration biopsy allowed us to acquire enough tissue for frozen biopsy during the operation because it uses a large bore needle. Therefore, immediate diagnosis and further procedures are possible without waiting for days for permanent pathology. In addition, there is less risk of postoperative air leakage and bleeding, unlike thoracoscopic incisional biopsy. Having achieved an advanced level of thoracoscopic surgical skill, a surgeon can directly palpate and control lesions with thoracoscopic instruments and can easily perform multiple aspirations of suspect nodules under clear vision. With a non-palpable SPN, anatomic localization of the SPN can be corroborated by careful preoperative CT imaging, and intraoperative instrumental palpation enables further localization. Even if the aspiration needle punctures the wrong place such as a pulmonary artery, bleeding is easy to control by compression. Therefore, thoracoscopic needle aspiration biopsy can be used in selective cases of non-palpable SPN.
In conclusion, the authors successfully attempted thoracoscopic needle aspiration for a central lesion. Compared with exploratory thoracotomy, this procedure facilitates neoadjuvant chemotherapy, saves surgical time, and reduces the length of stay and postoperative pain. In the absence of severe pleural adhesion, thoracoscopic needle aspiration is a good alternative for centrally-located SPNs suspected of being lung cancer.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Bousamra M, 2nd, Clowry L., Jr Thoracoscopic fine-needle aspiration of solitary pulmonary nodules. Ann Thorac Surg. 1997;64:1191–1193. doi: 10.1016/s0003-4975(97)00813-8. [DOI] [PubMed] [Google Scholar]
- 2.Haramati LB. CT-guided automated needle biopsy of the chest. AJR Am J Roentgenol. 1995;165:53–55. doi: 10.2214/ajr.165.1.7785631. [DOI] [PubMed] [Google Scholar]
- 3.Levine MS, Weiss JM, Harrell JH, Cameron TJ, Moser KM. Transthoracic needle aspiration biopsy following negative fiberoptic bronchoscopy in solitary pulmonary nodules. Chest. 1988;93:1152–1155. doi: 10.1378/chest.93.6.1152. [DOI] [PubMed] [Google Scholar]
- 4.Nakajima J, Furuse A, Kohno T, Ohtsuka T, Matsumoto J, Oka T. Transthoracoscopic needle biopsy for indeterminate lung nodules. Surg Endosc. 1999;13:386–389. doi: 10.1007/s004649900995. [DOI] [PubMed] [Google Scholar]



