Abstract
Background
Recent epidemiologic studies have shown that environmental contaminants such as air pollution and tobacco smoke play an important role in the pathophysiology of atopic dermatitis (AD).
Objective
The aim of this study was to evaluate the relationship between the severity of AD and indoor air pollution.
Methods
The study population consisted of 425 children from 9 kindergartens, Korea. The authors surveyed the prevalence of AD and evaluated disease severity by the eczema area and severity index (EASI) score and investigator's global assessment (IGA). After measuring indoor air pollution, a program to improve indoor air quality was conducted in 9 kindergartens. Seven months later, the prevalence and disease severity were evaluated.
Results
The initial prevalence of AD was 8% and the mean EASI score was 2.37. The levels of particulate material 10 (PM10) and carbon dioxide (CO2) were higher in some kindergartens compared to the normal values. Subsequent to the completion of the indoor air quality improvement program, the mean PM10 level was significantly decreased from 182.7 to 73.4 µg/m3. After the completion of the program, the prevalence of AD and the mean EASI were decreased, and the changes were both statistically significant. The mean number of hospital visits decreased from 1.3 per month during the first survey to 0.7 per month during the second survey, which was statistically significant.
Conclusion
Indoor air pollution could be related to AD. The reduction of PM10 through improving indoor air quality should be considered in kindergartens and schools in order to prevent and relieve AD in children.
Keywords: Atopic dermatitis, Improvement, Indoor air pollutants, Severity
INTRODUCTION
Atopic dermatitis (AD) is a chronic, itching and eczematous skin disease, which particularly affects subjects in early or late childhood. The prevalence of AD has been reported to be between 5% and 10% in the general population, and it has been increasing continuously worldwide in the recent decades1. This increase suggests that the pathogenesis of AD may be attributed to both genetic predisposition and environmental factors. There is much disagreement between the results of several epidemiological surveys, which studied the relationships between AD and environmental factors. Some studies portrayed that more industrialization and urbanization augments the prevalence of AD, whereas others presented no such relationship2-5.
There have been several epidemiological studies on the relationship between AD and air pollution. However, there is little clinical evidence in the literature. A few studies reported the relationship between AD and the environment. Wen et al.6 showed that fungus on walls, house renovation and house painting are significantly associated with AD. Arnedo-Pena et al.7 reported that the annual average concentration of carbon monoxide (CO) is also associated with the prevalence of AD.
This study is designed to evaluate the effect of indoor air quality on the severity of AD. We surveyed the prevalence and severity of AD in 9 kindergartens in Guro-gu, Seoul in collaboration with the Guro-gu public health center. After improving the indoor air quality through frequent cleaning and vacuuming, we evaluated the changes in clinical signs and symptoms among children with AD.
MATERIALS AND METHODS
Subjects
Of the 301 kindergartens in Guro-gu, Seoul, 9 were randomly selected for on-site surveys, which included physical examinations by a dermatologist. A total of 425 children (males, 210; females, 215) aged from 1 to 5 years were enrolled in the study. AD patients were diagnosed by a single dermatologist during the study. Exclusion criteria included any skin disorders other than AD in the area to be treated as well as children with any other systemic diseases. We received voluntary informed consent form the patients' parents.
Methods
1) Program for improving indoor air quality
Indoor air quality measurements included indoor temperature, humidity, particulate materials (PM10), CO, carbon dioxide (CO2) and formaldehyde (HCHO) in accordance with the official test standard of indoor air quality (Notification no. 2008-73 of the Ministry of Environment), gauged by a simplified measuring instrument (Model: LD-3B; Sibata Scientific Technology Ltd., Tokyo, Japan). Each kindergarten conducted general cleaning every week during the first survey and changed the frequency of general cleaning to every 2 or 3 days during the second survey. To improve indoor air quality, several daily practices were instituted: (1) elimination of fine dust, cobweb and mold spores on the walls, ceilings, bookshelves, floors and bedding; (2) steam sterilization of chairs, desks and other furniture in the hall and the gymnasium; and (3) removal of floating matters and mites in the bedding by steam cleaning.
2) Evaluation of atopic dermatitis
AD was diagnosed based on the Korean diagnostic guideline for AD8 and the patients were evaluated by a single dermatologist during the study. The objective skin manifestations of AD patients were checked for the point prevalence at the time of examination. The extent of skin lesions was estimated based on the Nine's rule and the severity of AD was evaluated by the eczema area and severity index (EASI) score and investigator's global assessment (IGA) measurement (a static 6-point measure of disease severity based on an overall assessment of skin lesions: 0=clear, no inflammatory signs of AD; 1=almost clear, just perceptible erythema and just perceptible population/infiltration; 2=mild disease, mild erythema and population/infiltration; 3=moderate disease, moderate erythema and moderate population/infiltration; 4=severe disease, severe erythema and severe population/infiltration; and 5=very severe disease, severe erythema and severe population/infiltration with oozing/crusting)9. Their parents were asked on the phone as to whether they regarded their children as AD patients or not. The evaluation and improvement of indoor air quality in kindergartens were attempted in collaboration with the Guro-gu public health center.
The first survey was conducted in order to collect data on the prevalence, severity and hospital visits of AD among children in kindergartens of Guro-gu, Seoul, between March and April of 2009. The second survey was conducted between November and December of 2009 in order to assess changes after the completion of the program for improving indoor air quality. The mean number of hospital visits per month in AD patients was calculated for each survey.
Statistical analysis
The paired t test was applied in order to compare the EASI score, decrease in the number of hospital visits and PM10/CO2 level between the first and second surveys. A p-value of <0.05 was considered as being statistically significant.
RESULTS
Program for improving indoor air quality
Table 1 presents the baseline value of indoor air quality. The baseline value of PM10 is usually under 150 µg/m3, particularly under 100 µg/m3 in medical institutes and child, elderly and postpartum care centers; hence, the authors considered that an optimal value of PM10 in kindergartens should be under 100 µg/m3.
Table 1.
Baseline values of indoor air in nine kindergartens
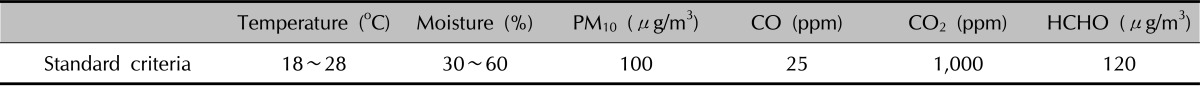
HCHO: formaldehyde.
Table 2 conveys the changes in PM10 and CO2 levels during the first and second surveys. CO and HCHO were not detected in any kindergarten. In the first survey, all of the 9 kindergartens showed a higher PM10 level than the baseline value, and 3 kindergartens showed a higher CO2 level than the baseline value. In the second survey after the program, the PM10 level dropped under the baseline value in 7 of the 9 kindergartens. Three kindergartens still showed a higher CO2 level. Five kindergartens satisfied the environmental standards for both PM10 and CO2 levels. The mean PM10 level decreased from 182.7±23.68 to 73.4±22.05 µg/m3 with statistical significance, while the mean CO2 level did not change significantly (from 934±384.4 to 1,040±540.4 ppm). The detection sites included 2 classrooms, 4 study rooms and 3 corridors. All sites showed improvement in the PM10 level after the program; yet, in 3 study rooms, the CO2 level increased.
Table 2.
Measurement results of indoor air in nine kindergartens
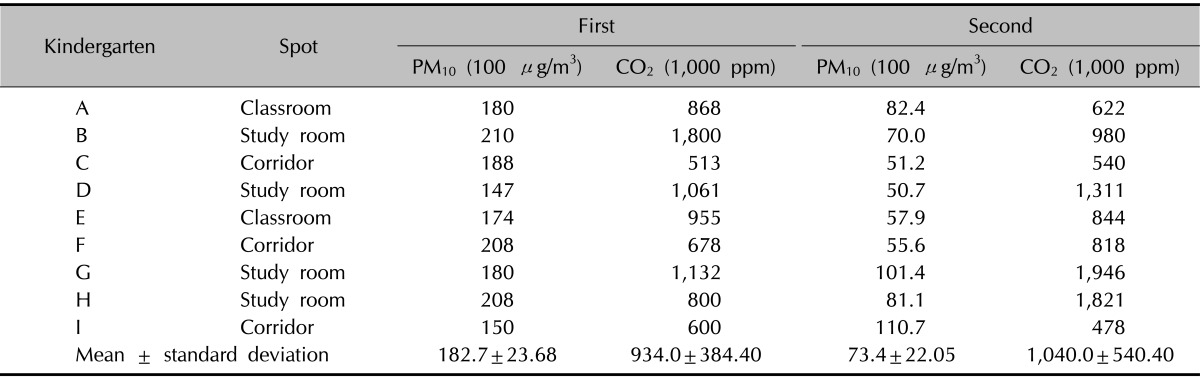
During the first survey, excessive particulate material 10 (PM10) level and CO2 were detected in 9 and 3 of the 9 kindergartens, respectively. During the second survey, the PM10 level was significantly decreased in all kindergartens, and 7 of the 9 kindergartens was decreased below the baseline value. The average changes in CO2 levels were variable slightly increased. The CO2 level increased in the study room with poor ventilation.
Prevalence of AD
During the first survey, 123 children (28.9%, 63 boys and 60 girls) were reported as AD patients by their parents via telephone interviews. However, 34 (8%, 20 boys and 14 girls) of the 425 children were diagnosed with AD by medical examination. The parents of 8 children (23.5%; 5 boys and 3 girls) of the 34 AD patients reported that their children had no AD. The prevalence of AD in each kindergarten varied from 3% to 15% (Table 3); however, there were no statistically significant differences between the 9 kindergartens (p>0.05). However, between the first and second surveys, 15 children moved to other kindergartens or dropped out before the second survey, leaving the study with 410 children. During the second survey, 3 children were newly diagnosed with AD, and 6 of 34 AD patients in the first survey moved to other kindergartens; thus, 31 (7.6%, 19 boys and 12 girls) of the total 410 children were classified as having AD.
Table 3.
Prevalence of atopic dermatitis in 9 kindergartens during first survey
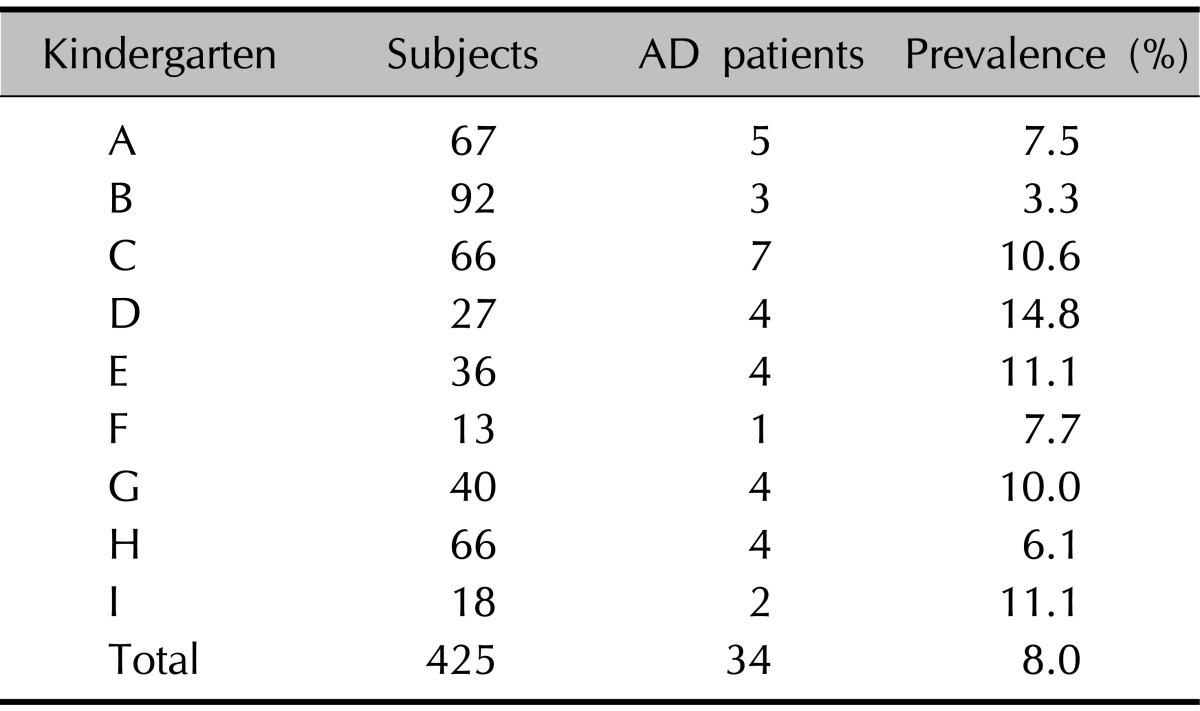
34 of the 425 patients were diagnosed with atopic dermatitis (AD). The average prevalence was 8% and varied from 3% to 15% in each kindergarten.
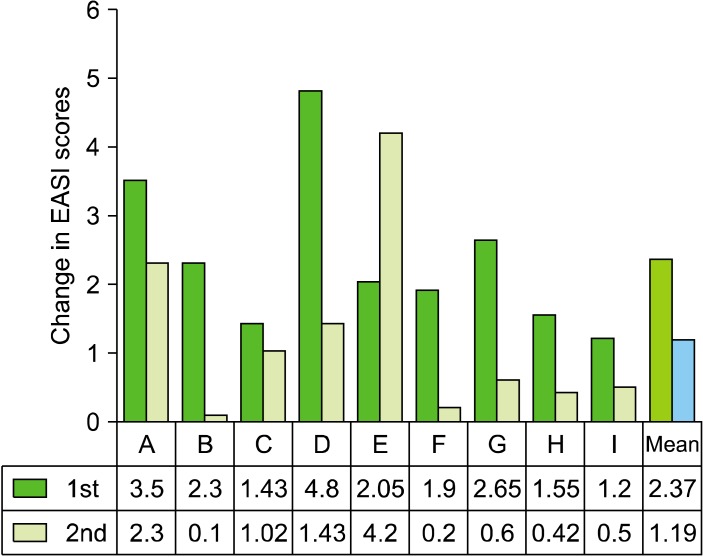
The mean EASI score decreased from 2.37±1.08 in the first survey to 1.19±1.25 in the second survey (Fig. 1), and the difference was statistically significant (p<0.05).
Fig. 1.
The comparison of atopic dermatitis improvement and the EASI score between the first and second surveys at 9 different kindergartens (A to I). The mean EASI score decreased from 2.37 in the first survey to 1.19 in the second survey (p<0.05). All kindergartens except 1 showed a decrease in the EASI score during the second survey. EASI: eczema area and severity index.
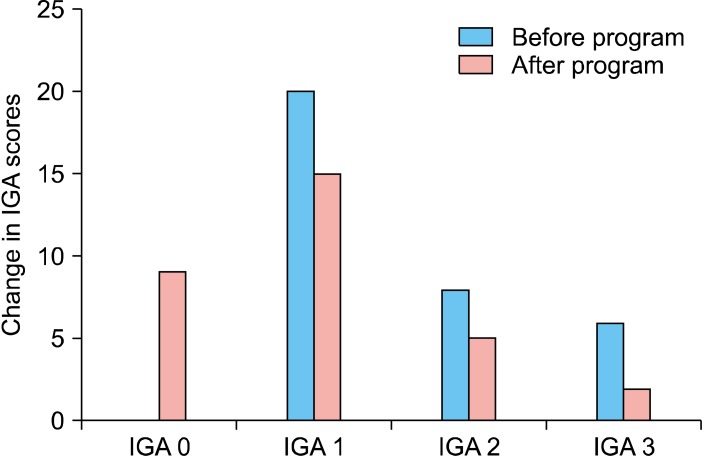
The IGA score showed much improvement after the completion of the program. The IGA scores in the first survey were as follows: IGA 1 (almost clear) in 20 children, IGA 2 (mild) in 8 children and IGA 3 (moderate) in 6 children. In the second survey, the score was changed as follows: IGA 0 (clear) in 9 children, IGA 1 (almost clear) in 15 children, IGA 2 (mild) in 5 children and IGA 3 (moderate) in 2 children (Fig. 2).
Fig. 2.
Atopic dermatitis patients were evaluated and grouped according to the IGA score as follows: 20 patients in IGA 1 (almost clear), 8 patients in IGA 2 (mild) and 6 patients in IGA 3 (moderate). After performance of the program, 9 patients were in IGA 0 (clear), 15 patients in IGA 1, 5 patients in IGA 2 and 5 patients in IGA3. IGA: investigator's global assessment.
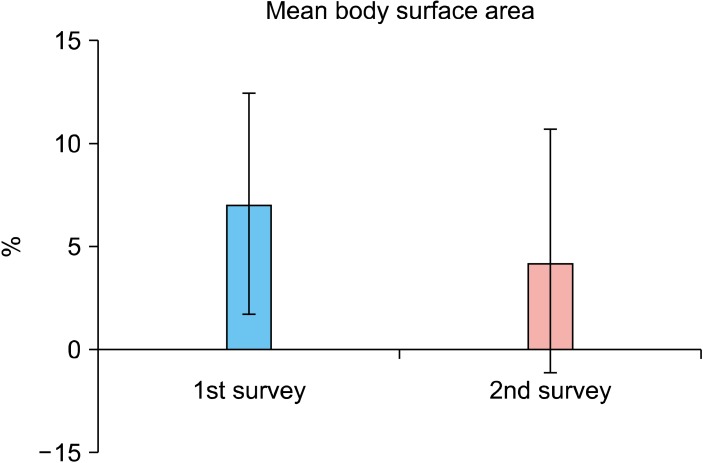
The mean extent of the skin lesion decreased from 7.06% in the first survey to 4.22% in the second survey with statistical significance (p<0.05) (Fig. 3).
Fig. 3.
The mean extent of the skin lesion decreased from 7.06% in the first survey to 4.22% in the second survey (p<0.05).
The mean number of hospital visits of 15 AD patients decreased from 1.3 per month in the first survey to 0.7 per month in the second survey, and the difference was statistically significant (p<0.05). During this period, none of the patients required additional hospital visits.
DISCUSSION
The prevalence of allergic diseases including AD, asthma and allergic rhinitis has increased, keeping pace with industrial development due to multifactorial causes. Environmental pollution has been considered as an exacerbating factor of AD; however, only a few studies have supported this assumption.
Interior decoration materials and building materials used in Western-style buildings for durability and insulation are known to cause indoor air pollution. As most buildings in Korea are Western-style, the detection of these materials is essential. In Korea, the indices for indoor air pollution include CO, CO2, HCHO, nitrogen dioxide, ozone, fine dust (PM10), volatile organic compounds, radon, asbestos and total bioaerosol10. In this study, CO, CO2, HCHO and PM10 were analyzed to assess indoor air quality in 9 kindergartens. Although CO and HCHO were within the normal range in all kindergartens, the CO2 level was higher than the normal value in 3 kindergartens, and the PM10 level was higher in 8 kindergartens. After the completion of the program for improving air quality, the PM10 level dramatically decreased and the PM10 level above the baseline value was detected only in 2 kindergartens. However, the CO2 level demonstrated variable changes.
There have been only a few studies on the relationship between AD and indoor air pollution, although many studies on the relationship between asthma and indoor air pollution have been found in the literature. Moon et al.11 have demonstrated that the aldehyde level is not significantly different between houses of AD patients and control subjects. Hagerhed-Engman et al.12 have indicated that there is a close relationship between indoor molds and AD. However, their result is questionable because the magnitude of molds was assessed using subjective odor, not an objective method. In our study, the EASI score decreased from 2.37 to 1.19 and the IGA score was improved, suggesting that indoor air quality improvement relieved symptoms of AD. After the completion of the program for improving indoor air quality, the frequency of hospital visits was the same as before in 10 of the 34 AD patients and lower than before in 15 AD patients. Nine AD patients did not take any medical services before and after the program. The mean number of hospital visits decreased from 1.3 to 0.7 per month in 15 AD patients with statistical significance. The mean value of EASI scores was low, which did not suggest an improvement of AD. The decrease of hospital visits could reflect the improvement of AD better rather than the EASI score.
PM means a mixture of solid particles and liquid droplets suspended in air. The definition of PM10 is fine dust less than 10 µm in diameter, which is not filtered by oral and nasal mucous membranes and infiltrates deeply into the respiratory organs. PM10 hinders lung function by sticking to the bronchus and pulmonary alveoli13. PM10 includes harmful materials, such as sulphate, nitrate, acid and all sorts of heavy metal. It shows a very slow sedimentation rate; thus, it stays for a relatively long time in the air. Numerous studies on the toxic properties of PM in the human body have been carried out in the air pollution field14. Some previous studies have shown that PM in air pollution influences the aggravation of asthma attacks and chronic respiratory diseases15,16. It has been reported that PM increases tumor necrosis factor-α and interleulin (IL)-1β in pulmonary alveoli mRNA of IL-1α, IL-1β, IL-8 and granulocyte macrophage colony stimulating factor17,18. Increased amounts of proinflammatory cytokines contribute to the deterioration of chronic respiratory diseases as well as several skin diseases such as AD.
Due to the fact that fine dust between 10 to 30µm carries dust mites19, it can exacerbate the symptoms of AD. It has been documented that a high prevalence of AD is related to the environment with abundant fine dust20,21. In our study, symptoms of AD were improved by reducing the amount of PM10.
CO2 is a colorless and odorless gas. It is harmless in low density. High-density CO2 in limited restricted indoor space indicates insufficient ventilation due to congested indoor harmful substances, namely, of the decreasing air quality. It is used as a representative index of indoor air quality22. Modern-style, highly sealed buildings without supplementary equipment for ventilation cannot provide fresh air; hence, the environmental quality of such living spaces is low, especially in long-term dwellings. CO2 concentrations between 1,000 to 2,000 ppm can cause headache, hypertension, vomiting and fatigue in healthy adults and more severe symptoms in the elderly people and children. In our study, the indoor CO2 level was higher than the baseline value. Subsequent to the completion of the program for improving air quality, the results varied from kindergarten to kindergarten. This may be due to different detection sites, such as classrooms, corridors and study rooms. Most study rooms indicated a higher CO2 concentration than the baseline value due to a relatively large number of students in narrow space. Further, the program contents did not include ventilation by opening the windows and entrance doors in order to decrease the CO2 concentration. The program for improving indoor air quality were conducted in 3 different methods; (1) removal of fine dust, spider web and mold spores in the wall and ceiling; (2) sterilization of desks, chairs and other teaching materials through steam heating after the removal of dust; and (3) reduction of fine dust, molds and dust mites through elimination of dust mites and floating matter as well as by steam cleaning the bedding. The program was designed to decrease amounts of fine dust and CO2. After conducting the program, the PM10 level decreased in all 9 kindergartens, while the CO2 level showed variable results. This result may be attributed to different detection time, for example, school hours or between-classesbreaks, or before or after ventilation.
The prevalence of AD in 9 kindergartens located in Guro-gu, Seoul was 8%. The mean EASI score was 2.37 and the mean body surface area was 7.06%. After the completion of the program, the prevalence dropped to 7.6%, the mean EASI score decreased to 1.19, and the mean body surface area decreased to 4.22%. The IGA score also improved. The mean number of hospital visits also decreased from 1.3 to 0.7 per month in 15 patients. In conclusion, the results of this study suggest that the program for improving indoor air quality could improve the clinical symptoms and signs of AD as well as decrease the PM10 level. Further studies on the relationship between AD and PM10 level are needed in order to confirm our results.
ACKNOWLEDGMENT
This research was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (No. 2011-0013003 and No. 2011-0004436) and by a grant from Amore Pacific Co. Ltd, 2011.
References
- 1.Kay J, Gawkrodger DJ, Mortimer MJ, Jaron AG. The prevalence of childhood atopic eczema in a general population. J Am Acad Dermatol. 1994;30:35–39. doi: 10.1016/s0190-9622(94)70004-4. [DOI] [PubMed] [Google Scholar]
- 2.Aberg N, Engström I, Lindberg U. Allergic diseases in Swedish school children. Acta Paediatr Scand. 1989;78:246–252. doi: 10.1111/j.1651-2227.1989.tb11064.x. [DOI] [PubMed] [Google Scholar]
- 3.Kilpeläinen M, Terho EO, Helenius H, Koskenvuo M. Farm environment in childhood prevents the development of allergies. Clin Exp Allergy. 2000;30:201–208. doi: 10.1046/j.1365-2222.2000.00800.x. [DOI] [PubMed] [Google Scholar]
- 4.McNally NJ, Williams HC, Phillips DR, Strachan DP. Is there a geographical variation in eczema prevalence in the UK? Evidence from the 1958 British Birth Cohort Study. Br J Dermatol. 2000;142:712–720. doi: 10.1046/j.1365-2133.2000.03416.x. [DOI] [PubMed] [Google Scholar]
- 5.Riedler J, Eder W, Oberfeld G, Schreuer M. Austrian children living on a farm have less hay fever, asthma and allergic sensitization. Clin Exp Allergy. 2000;30:194–200. doi: 10.1046/j.1365-2222.2000.00799.x. [DOI] [PubMed] [Google Scholar]
- 6.Wen HJ, Chen PC, Chiang TL, Lin SJ, Chuang YL, Guo YL. Predicting risk for early infantile atopic dermatitis by hereditary and environmental factors. Br J Dermatol. 2009;161:1166–1172. doi: 10.1111/j.1365-2133.2009.09412.x. [DOI] [PubMed] [Google Scholar]
- 7.Arnedo-Pena A, García-Marcos L, Carvajal Urueña I, Busquets Monge R, Morales Suárez-Varela M, Miner Canflanca I, et al. Air pollution and recent symptoms of asthma, allergic rhinitis, and atopic eczema in schoolchildren aged between 6 and 7 years. Arch Bronconeumol. 2009;45:224–229. doi: 10.1016/j.arbres.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 8.Park YL, Kim HD, Kim KH, Kim MN, Kim JW, Ro YS, et al. A study on the diagnostic criteria of Korean atopic dermatitis. Korean J Dermatol. 2006;44:659–663. [Google Scholar]
- 9.Gelmetti C, Colonna C. The value of SCORAD and beyond. Towards a standardized evaluation of severity? Allergy. 2004;59(Suppl 78):61–65. doi: 10.1111/j.1398-9995.2004.00651.x. [DOI] [PubMed] [Google Scholar]
- 10.Kim JH, Lee KM, Koh SB, Kim SH, Choi EH. Effect of polyurushiol paint on indoor air quality and atopic dermatitis. Korean J Dermatol. 2010;48:198–205. [Google Scholar]
- 11.Moon KW, Byeon SH, Choi DW, Lee EI, Oh EH, Kim YW. Risk assessment of aldehydes in some residential indoor air included atopy patient's homes. Korean J Environ Toxicol. 2006;32:19–26. [Google Scholar]
- 12.Hägerhed-Engman L, Sigsgaard T, Samuelson I, Sundell J, Janson S, Bornehag CG. Low home ventilation rate in combination with moldy odor from the building structure increase the risk for allergic symptoms in children. Indoor Air. 2009;19:184–192. doi: 10.1111/j.1600-0668.2008.00573.x. [DOI] [PubMed] [Google Scholar]
- 13.Dockery DW, Pope CA, 3rd, Xu X, Spengler JD, Ware JH, Fay ME, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med. 1993;329:1753–1759. doi: 10.1056/NEJM199312093292401. [DOI] [PubMed] [Google Scholar]
- 14.Logan WP. Mortality in the London fog incident, 1952. Lancet. 1953;1:336–338. doi: 10.1016/s0140-6736(53)91012-5. [DOI] [PubMed] [Google Scholar]
- 15.Dockery DW, Pope CA., 3rd Acute respiratory effects of particulate air pollution. Annu Rev Public Health. 1994;15:107–132. doi: 10.1146/annurev.pu.15.050194.000543. [DOI] [PubMed] [Google Scholar]
- 16.Schwartz J, Slater D, Larson TV, Pierson WE, Koenig JQ. Particulate air pollution and hospital emergency room visits for asthma in Seattle. Am Rev Respir Dis. 1993;147:826–831. doi: 10.1164/ajrccm/147.4.826. [DOI] [PubMed] [Google Scholar]
- 17.Kim JH, Jeon HK, Kim MK, Kyung SY, An CH, Lee SP, et al. Particulate matter from Asian dust storms induces the expression of proinflammatory cytokine in A549 epithelial cells. Tuberc Respir Dis. 2006;60:663–672. [Google Scholar]
- 18.Li TZ, Lee SJ, Park SJ, Chang BJ, Lee JH, Kim KS, et al. The effects of air-borne particulate matters on the alveolar macrophages for the TNF-α and IL-1β secretion. Tuberc Respir Dis. 2006;60:554–563. [Google Scholar]
- 19.Sharma HP, Hansel NN, Matsui E, Diette GB, Eggleston P, Breysse P. Indoor environmental influences on children's asthma. Pediatr Clin North Am. 2007;54:103–120. doi: 10.1016/j.pcl.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 20.Annesi-Maesano I, Moreau D, Caillaud D, Lavaud F, Le Moullec Y, Taytard A, et al. Residential proximity fine particles related to allergic sensitisation and asthma in primary school children. Respir Med. 2007;101:1721–1729. doi: 10.1016/j.rmed.2007.02.022. [DOI] [PubMed] [Google Scholar]
- 21.Salvi S. Health effects of ambient air pollution in children. Paediatr Respir Rev. 2007;8:275–280. doi: 10.1016/j.prrv.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 22.Persily AK. Relationship between indoor air quality and carbon dioxide; Proceeding of the Indoor Air Quality and Climate, 7th International Conference; 1996 Jul 21-26; Nagoya, Japan. 1996. [Google Scholar]