Dear Editor:
The critical role of T helper (Th) 17 cells has recently been reported in a variety of inflammatory skin diseases (psoriasis, atopic eczema, contact dermatitis)1,2. Interestingly, the number of Th17 cells is higher in acute atopic dermatitis (AD) lesions than in chronic ones in a severity-dependent manner3. Other studies have shown conflicting results on the correlation between levels of circulating Th17 cells and severity of AD3,4. Thus, the pathogenic role of Th17 cells in AD is not completely understood. The usefulness of ustekinumab in AD has only been described in one previous case report5. This finding also supports the implication of Th17 cells in AD. We report a case of severe refractory AD in an adolescent patient successfully treated with ustekinumab.
A 16-year-old woman was presented with over a 13-year history of severe AD. She also had persistent rhinitis and childhood asthma. During follow-up, the patient underwent several oral corticoid regimens with clear improvement and later relapses. She had undergone other therapies, such as topical agents (emollients, tacrolimus, pimecrolimus, corticosteroids), phototherapy (psoralen ultraviolet A [PUVA], narrow band ultraviolet B) and systemic agents (cyclosporine, azathioprine) with minimal response.
The patient came to our clinic in January 2011 for a flare-up of AD. The physical examination revealed eczematous scaly plaques over 80% of her total body surface, with an objective SCORing atopic dermatitis (SCORAD) of 23 (Fig. 1). The histopathologic study of two lesions showed a superficial perivascular lymphohistiocytic infiltrate. The overlying epidermis revealed irregular acanthosis and mild hyperkeratosis with moderate spongiosis (Fig. 2).
Fig. 1.
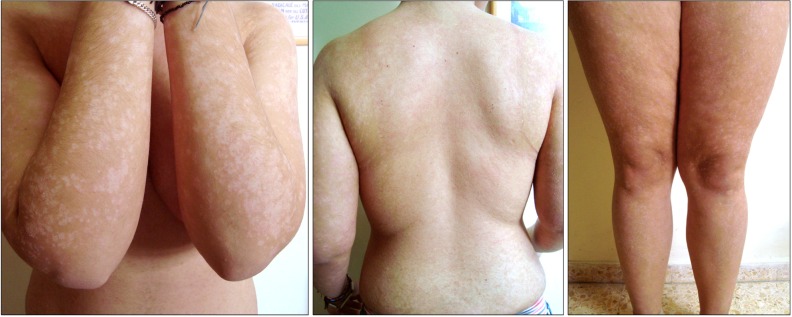
Patient lesions in January 2011, erythematous scaly plaques over 80% of her total body surface (SCORing atopic dermatitis [SCORAD]: 23).
Fig. 2.
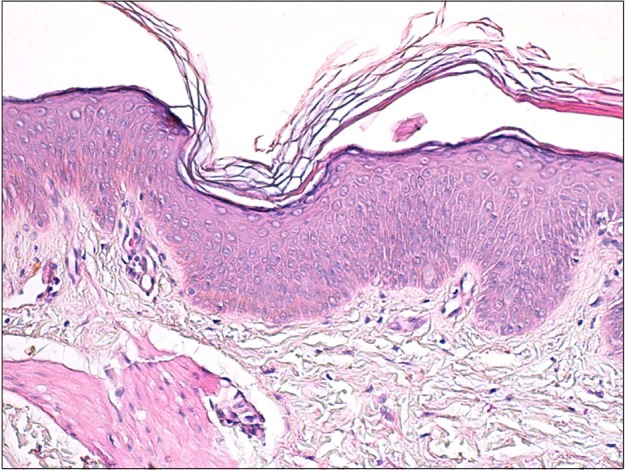
Histopathologic findings of skin biopsy specimen from eczematous lesion before treatment, revealing features of subacute eczema with irregular acanthosis of epidermis, moderate spongiosis, and mixed cellular infiltrate of lymphocytes and histiocytes (H&E, ×100).
Prick tests showed sensitization to Dermatophagoides pteronyssinus and D. farinae. The laboratory workup demonstrated a total serum immunoglobulin E (IgE) of 752 kU/L. IgE-specific antibodies against Dermatophagoides were above 100 kU/L. In March 2011, the patient began treatment with ustekinumab administered in a single dose of 45 mg. She did not receive any adjuvant or symptomatic treatment.
One month later, the patient reported a substantial clinical improvement in her condition, particularly in the pruritus. A second 45 mg dose was administered at that point, according to the recommended dosage in psoriasis (at weeks 0 and 4, followed by every 12 weeks). In July 2011, the lesions had cleared (Fig. 3) and pruritus was absent (SCORAD: 0). In April 2011, the patient had completed month 14 of treatment. She remained asymptomatic without any skin lesions.
Fig. 3.

Absence of lesions in July 2011 (SCORing atopic dermatitis [SCORAD]: 0), 4 months after starting ustekinumab.
The management of severe AD is often difficult and requires successive regimens of oral corticosteroids that may cause important side effects in an adolescent patient. Ustekinumab is a human monoclonal antibody approved for the treatment of moderate to severe plaque psoriasis. It is directed against interleukin 12 and interleukin 23, which are naturally occurring proteins that regulate the immune system. AD and psoriasis are two conditions with profound clinical and pathogenic differences. However, several findings suggest the participation of Th17 cells in the development of AD. The binding between ustekinumab and interleukins 12/23 might prevent the upregulation of Th17 cells in AD3,4. Against this background, we decided to use the ustekinumab, in an off-label manner, to treat an AD patient who had not reached improvement with other systemic treatments. Our patient showed a total control of her disease without any side effect related to ustekinumab.
Although controlled clinical trials will be required to establish the effectiveness of ustekinumab in AD, we suggest that ustekinumab might be a useful and safe treatment of refractory AD in young patients.
References
- 1.Hu Y, Shen F, Crellin NK, Ouyang W. The IL-17 pathway as a major therapeutic target in autoimmune diseases. Ann N Y Acad Sci. 2011;1217:60–76. doi: 10.1111/j.1749-6632.2010.05825.x. [DOI] [PubMed] [Google Scholar]
- 2.Di Cesare A, Di Meglio P, Nestle FO. The IL-23/Th17 axis in the immunopathogenesis of psoriasis. J Invest Dermatol. 2009;129:1339–1350. doi: 10.1038/jid.2009.59. [DOI] [PubMed] [Google Scholar]
- 3.Koga C, Kabashima K, Shiraishi N, Kobayashi M, Tokura Y. Possible pathogenic role of Th17 cells for atopic dermatitis. J Invest Dermatol. 2008;128:2625–2630. doi: 10.1038/jid.2008.111. [DOI] [PubMed] [Google Scholar]
- 4.Hayashida S, Uchi H, Moroi Y, Furue M. Decrease in circulating Th17 cells correlates with increased levels of CCL17, IgE and eosinophils in atopic dermatitis. J Dermatol Sci. 2011;61:180–186. doi: 10.1016/j.jdermsci.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 5.Puya R, Alvarez-López M, Velez A, Casas Asuncion E, Moreno JC. Treatment of severe refractory adult atopic dermatitis with ustekinumab. Int J Dermatol. 2012;51:115–116. doi: 10.1111/j.1365-4632.2011.05195.x. [DOI] [PubMed] [Google Scholar]


