Abstract
Background
This study evaluated the effects on healthcare access inequities of an intervention exempting children under 5 years from user fees in Burkina Faso.
Methods
The design consisted of two complementary studies. The first was an interrupted time series (56 months before and 12 months after) study of daily curative consultations according to distance (<5, 5–9 and ≥10 km) in a stratified random sample of 18 health centres: 12 with the intervention and 6 without. The second was a household panel survey (n=1214) assessing the evolution of health-seeking behaviours. Multilevel regression was used throughout.
Results
Attendance doubled under the intervention, after adjusting for Centres de Santé et de Promotion Sociale size, districts, secular trend and seasonal variation. Utilisation increased for all distance ranges and in all of the 12 health centres of the intervention area. The exemption benefited all children (rate ratios (RR)=1.52 (1.23 to 1.88)), whether their health needs were high (RR=1.69 (1.22 to 2.32)) or not (RR=1.46 (1.10 to 1.93)) and whether the children lived near (RR=1.42 (1.09 to 1.85)) or far from a health centre (RR=1.79 (1.31 to 2.43)). The exemption benefited the children of poor families when health need was high and services near (RR=5.23; (1.30 to 20.99)). The amount saved for a child's treatment by the exemption was on average and median 2500 F CFA (≈US$5).
Conclusions
Exempting children under five from user fees is effective and helps reduce inequities of access. It benefits vulnerable populations, although their service utilisation remains constrained by limitations in geographic accessibility of services.
Background
Since the early 2000s, many African countries have undertaken major reforms of their healthcare funding policies to improve equity of access to healthcare for children under five. The generalisation of user fees had until then heavily constrained access to the healthcare system.1 This prompted the African Union, in 2010, to call for the abolition of healthcare user fees for children under five. A simulation involving 20 African countries estimated that the lives of more than 200 000 children under five could be saved by these measures.2 Evaluations of these initiatives have shown that they are effective in improving children's access to care, but almost no studies have examined their distributive effects.1 3 The distribution of outcomes of health policies in Africa is, in fact, rarely analysed.4 For obvious pragmatic reasons, these policies are always universal, in that the fees abolition applies to all children attending public-health centres, regardless of their parents' income. Yet data from the 1990s suggest that the well-off derived greater benefit than the poor from public resources invested in curative consultations in certain African countries.5 This appears still to be the case in Ghana and South Africa, where such exemption policies have been in place for several years,6 although it was probably true even before these policies were implemented. On the other hand, in Uganda, a study showed that the worst-off benefited more than did others from the user fees abolition policy.7 Some observers wondered about the distribution of the benefits of these new policies and to what extent they were monopolised by the less poor. However, there is still insufficient evidence to support the hypothesis that exemption policies have been more advantageous for less vulnerable groups. There are numerous methodological issues associated with such evaluations, and a recent Cochrane systematic review concluded that “for equity and health expenditure outcomes at household level…we found no evidence.”1 The objective of this article is to evaluate the effectiveness and distributive effects of an intervention in Burkina Faso exempting children under five from healthcare fees.
Context and intervention
The organisation of primary healthcare services in Burkina Faso follows a pyramidal model. First-line service is composed of primary healthcare centres (CSPS, Centres de Santé et de Promotion Sociale), each being managed by a village health committee. Previous studies have shown that paying for healthcare has negative impacts on children's access to services.8 Inequities in access remain substantial. For example, in 2003, 54% of children with fever in well-off families were treated in public health centres, while this proportion was only 22% for children in poor families.9 A recent simulation suggested that child mortality might be reduced by up to 20% if the proportion of children treated in health centres for malaria, respiratory infections and diarrhoea were increased.10 The results of the most recent Demographic and Health Survey showed that in 2010 only half of the children with one of these three conditions were treated in health centres.11 Likewise, the risk of death doubled if a child lived more than 6 h walk from a health centre.12
The fee exemption experiment was carried out in the Sahel health region in the North-East. This is one of the country's most disadvantaged regions, where the rate of severe anaemia in children (20%) is the highest, while vaccination coverage (65% for all vaccinations) and health-centre utilisation are lowest (only 32% of children with fever use healthcare services).11 In this region, there is no supply of private healthcare. The only other options for patients are traditional healers and self-medication, both of which involve costs. Before the experiment, patients visiting a health centre had to pay for the consultation ($0.20), for drugs (varying costs depending on the prescription) and for care under observation ($0.60/day) if they were hospitalised in the CSPS. Faced with this difficult situation for children, in September 2008 two of the region's four health districts (Dori and Sebba) exempted them from point-of-service user fees. Thus, in Dori and Sebba, children under five no longer had to pay for curative care provided by State-employed nurses in a CSPS. CSPSs were reimbursed by a non-governmental organisational for expenses incurred to provide free care to children. The intervention did not change the drug supply chain; the CSPSs continued to obtain their drugs from the national procurement centre. The intervention was not limited to removing user fees, but also included activities related to social mobilisation, health education, improvement of service quality (training, supervision) and financial monitoring. The intervention's objectives were to encourage mothers to bring their children for care earlier when symptoms appeared and to increase CSPS utilisation by all sick children, including the poorest and those living furthest away. In another study, we showed that the quality of medical prescriptions had been maintained after the removal of user fees.13
Methods
Design
The study included two complementary components. The first was an interrupted time series (ITS) analysis performed on a stratified random sample of CSPSs drawn from one intervention district (12 in Dori) and a neighbouring non-intervention district (six in Djibo). The health centre areas were stratified according to their belonging or not to the so-called ‘pastoral zone’,14 where cattle raising is relatively more important and from where many families or family members seasonally move southward with their cattle. Only CSPSs that had been operating for at least 1 year before the intervention were included. The observation window covered a 56-month preintervention period (January 2004–August 2008) and a 12-month period of intervention (September 2008–August 2009). The second component was a panel survey of 1214 households in one of the two districts exposed to the intervention (Dori). Each household was visited in 2008 for the preintervention round 1 month before the intervention's inception, and again 12 months later.
Outcome measures
For the ITS component, the outcome was changed in CSPS attendance by children living at different distances from the CSPS. For the household survey, one indicator was the extent to which parents had opted to bring their child to the CSPS in cases of illness during the previous 4 weeks, in different categories of income and distance from the CSPS. Another indicator was the amount paid for services received from the CSPS. Our hypothesis was that lifting the financial barrier should increase the utilisation of CSPSs and reduce the burden of costs associated with an episode of care.
Data sources, sampling
The data used for the ITS were collected from the CSPSs' administrative records. The data were extracted directly from registry books, where a line is recorded during each patient contact (age, sex, location of residence, time of arrival, symptoms, treatment). We were able to retrieve 78% of the records—a high proportion, given the context. Data quality was automatically controlled during data entry by page-wise grand totals and subtotals for distance and age strata, with which the stratum frequencies that were subsequently entered had to be consistent. Units of observation were curative consultations by children under five. For each visit recorded in the centres' consultation registers within the observation period, we extracted information on the child's age and the distance between the child's village of residence and the CSPS (<5, 5–9 and ≥10 km). In total, 112 724 observations were recorded.
The panel household survey was based on a two-stage sample design following the WHO's Expanded Program on Immunization (EPI) Cluster Survey Design.15 First, 48 clusters of households were randomly selected using the study area's 304 national census enumeration areas (EAs) as the primary sampling unit, with the clusters proportional to EA size. For the second-stage selection of households within EAs, we adapted the improved EPI sampling scheme.15 We selected 30 households randomly per cluster.
The two rounds were conducted at the same period of the year (July–August) to limit seasonal variations in morbidity and in households' financial liquidity. Caretakers of children (generally mothers) were asked whether a child in the household had an episode of illness within the preceding 30 days. For each child who had been ill, a detailed questionnaire was used to record key events of the episode, symptoms, severity, sources of healthcare used and total episode-related expenses at the CSPS. Table 1 presents the number of children surveyed and the number of episodes of illness recorded in 2008 and 2009. Household socioeconomic status was measured by the household's annualised per capita consumption expenditures. Households were then divided into income quartiles in each of the three distance ranges. Quartiles 2 and 3 were collapsed for the analysis.
Table 1.
Household panel survey in Dori Burkina Faso
| Year | 2008 | 2009 |
|---|---|---|
| Children | ||
| Seen per year | 1214 | 1098 |
| Seen both years | 1069 | |
| Household characteristics | ||
| Per capita annual income (CFA Francs) | ||
| Median (25th; 75th centiles) | 174,115 (110,380;299,750) | |
| Proportion living in rural areas (%) | 88 | |
| Distance to the closest health centre (%) | ||
| d<5 km | 30.1 | |
| 5 km≤d<10 km | 24.5 | |
| d≥10 km | 45.2 | |
| Schooling of head (none) | 94.8 | |
| Children reported ill (recall=30 days) | 327 (22.4%) | 224 (17.1%) |
| Proportion of ill children with severe episode (%) | 29.4 | 26.8 |
| Utilisation of a health centre during the episode (%) | ||
| All episodes | 36.1 | 54.9 |
| Severe episodes only | 41.7 | 70.0 |
Description of the children sample.
Analyses
Multilevel Poisson models were used to analyse the two datasets, using sitewise random intercepts and slopes, and estimating the intervention effects as rate ratios (RR). The Poisson model is statistically required to deal with the ITS data, which are counts;16 conceptually, it better reflects the multiplicative nature of the expected effect driven by modified user behaviour (thus depending more on the size of the catchment area population than on the capacity of the individual health facility). For the household data whose outcome are binary, we preferred a Poisson model over a logistic one because it produces relative risks (RR) rather than ORs.15 A logarithmic link function and robust variance estimators were applied throughout. The time series analyses were controlled for secular trend, seasonal variation and (via an offset) population growth. Residual differences between the two districts were controlled by a district indicator and health centre random intercepts and slopes in the regression model, which at the same time controlled for the serial autocorrelation.17 The analysis of the household survey data controlled for age, village and district of residence and used first-order, second-order and third-order interaction terms to study the intervention's increases separately by household socioeconomic status, distance from the nearest health centre and severity of the episode of illness. All analyses were carried out with Stata software.
Results
Frequency of health-centre attendance
Figure 1 shows the evolution in the number of daily visits of children under five in primary healthcare facilities in the intervention and comparison districts. From the first month of the intervention's implementation (September 2008), there was an immediate and ample rise in utilisation in the intervention district (Dori), while in Djibo, where children continued to pay for services, the level of utilisation was unchanged. This finding was observed for all types of users, whether they lived near or far from the CSPSs. Attendance at health centres varied with season. The statistical models confirmed this result. Attendance doubled under the intervention, after adjusting for CSPS size, districts, secular trend and seasonal variation (table 2). The increases were nearly comparable for the three distance groups. The largest increase was observed among users living within 5–9 km from the health centre; this group had constituted the smallest proportion of users at the outset (around one consultation per day per centre). The average increase attributable to the intervention was almost 2000 visits/year/centre, or +110%. It should be noted that these values are averages, since we are dealing with parameters corresponding to the models' fixed effects. Close examination of the random part of the final model revealed that the impact of the intervention varied significantly from one centre to another (the complete results of the regression can be consulted in web appendix 1). The centres' responses were thus significantly heterogeneous, even after taking into account the size of their target populations, their individual secular trends and the districts in which they are located. Despite these variations, utilisation increased for all distance ranges and in all of the 12 health centres of the intervention area, without exception.
Figure 1.
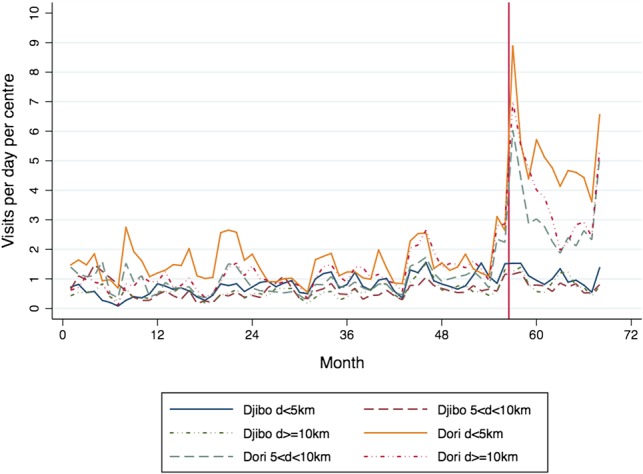
Number of daily visits of children under five in CSPS.
Table 2.
Effects of the intervention on health centre utilisation (source: administrative records of CSPSs)
| Users’ place of residence (1) | Users/year/centre, preintervention period (2) | Effects of the intervention (3) | ||
|---|---|---|---|---|
| Rate ratio estimate and (95% CI) (4) | Average increase (additional users per year and % increase) (4) | |||
| d<5 km | 649.5 | 2.21 (1.74 to 2.79) | 782.7 | 121 |
| 5 km≤d<10 km | 478.4 | 2.43 (1.92 to 3.09) | 686.0 | 143 |
| d≥10 km | 655.0 | 1.77 (1.39 to 2.24) | 501.1 | 77 |
| All | 1782.9 | 2.09 (1.67 to 2.63) | 1948.1 | 109 |
(1) Distance from home to the health centre.
(2) Average number of users per centre in the 12 months preceding the intervention.
(3) RRs and marginal increases estimated by multilevel Poisson regression.
(4) All RRs and marginal increases are significant at a threshold of p<0.001.
Propensity to use a health centre when a child is sick
The estimates from the analysis of the use of health centres by children in the household panel were congruent with the results above and in the same range. Overall, the exemption benefited the target population (RR=1.52; (1.23 to 1.88)), whether the health need was great or small, and whether the children lived near or far from the CSPS (table 3). We found no significant difference when we compared the effects of the intervention on children living near a CSPS with those on children living more than 5 km away, nor when we compared the children whose parents felt their lives were in danger with children whose health status was considered less serious.
Table 3.
Effects of the intervention on health centre utilisation by illness severity, health centre distance and household income (source: panel survey)
| Condition | Rate ratio* (95% CI) | Ratio (1)/(2) (95% CI) | |
|---|---|---|---|
| Severity† | Severe (1) | 1.69 (1.22 to 2.32) | 1.16 |
| Not severe (2) | 1.46 (1.10 to 1.93) | (0.75 to 1.79) | |
| Place of residence | d<5 km (1) | 1.42 (1.09 to 1.85) | 0.79 |
| d≥5 km (2) | 1.79 (1.31 to 2.43) | (0.53 to 1.19) | |
| Income quartile | First quartile, poorest (1) | 1.13 (0.73 to 1.74) | 0.65 |
| Other quartiles (2) | 1.73 (1.43 to 2.09) | (0.43 to 0.99) | |
| All | 1.52 (1.23 to 1.88) |
*Rate ratios estimated by multilevel Poisson regression.
†As reported by the caregiver; the question was: do you think your child's life was in danger?
The benefits were statistically significant for children living in families that were not in the first income quartile (Q1). However, the situation appeared more complex when we examined the effects on children in Q1 households. The analyses showed that the intervention effects for poor children varied with illness severity and geographic accessibility of services. Significant benefits for children of poor families were only found when the health need was serious and the services nearby (table 4). It was these children who derived the greatest benefit (RR=5.23; (1.30 to 20.99)). The benefit was less, and non-significant, for children whose health status was considered serious but who lived more than 5 km from a health centre (RR=1.28 (0.90 to 1.82)). No benefit was observed among children whose health needs were judged to be less serious, regardless of the effort required to reach a health centre. The complete results of the regression may be consulted in web appendix 2.
Table 4.
Effects of the intervention on health centre utilisation across income groups, according to place of residence and severity of illness (source: panel survey)
| Severity | Place of residence | Income group | Ratio (1)/(2) Est. and (95%CI) |
|
|---|---|---|---|---|
| First income quartile (1) Rate ratio* and (95% CI) |
Other income groups (2) Rate ratio* and (95%CI) |
|||
| Severe | d<5 km | 5.23 (1.30 to 20.99) | 2.23 (1.29 to 3.86) | 2.35 (0.44 to 12.45) |
| d≥5 km | 1.28 (0.90 to 1.82) | 1.56 (0.87 to 2.79) | 0.82 (0.40 to 1.66) | |
| Not severe | d<5 km | 0.87 (0.39 to 1.95) | 1.90 (1.23 to 2.92) | 0.46 (0.20 to 1.04) |
| d≥5 km | 1.15 (0.54 to 2.47) | 1.65 (1.20 to 2.27) | 0.70 (0.34 to 1.42) | |
*Rate ratios estimated by multilevel Poisson regression.
Effects on the cost of an episode of care at the health centre
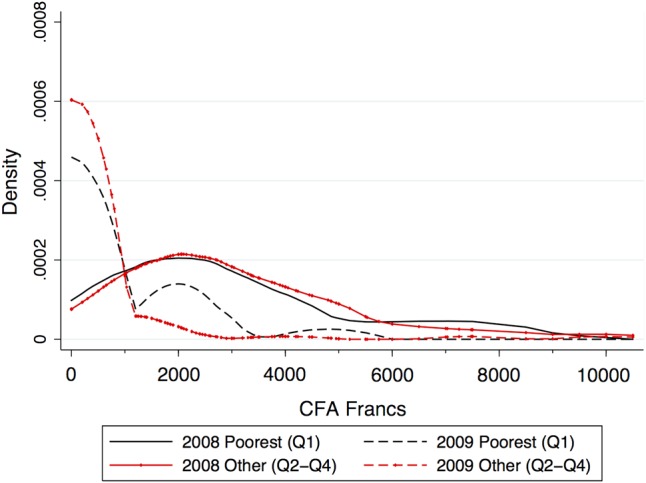
The exemption reduced the expenses incurred for children's treatment at the CSPS (table 5). The amount saved for a child's treatment was on average 2500 F CFA, or around US$5 (same value for the median benefit). This is a substantial benefit when considered in light of rural households' meagre capacity to pay in that country (where 46% live on less than 275 F CFA/day18); the majority of these householders are farmers or herdsmen for whom, in the rainy season, it is extremely difficult to raise cash on short notice to cover their families' needs. All the groups we considered benefited from the exemption (table 5). The distribution of expenses narrowed considerably, and 85% of the care episodes were entirely free of charge. Figures 2–4 present the Kernel density estimates of the probability density function. Horizontal disparities (inequalities within each group) were demonstrably substantially reduced after the intervention. In 2008, health expenditure distributions were comparable between poor and non-poor children, whether their episodes of illness were severe or not, and regardless of whether they lived near or far from a health centre. These distributions narrowed considerably in 2009. They evolved comparably in terms of severity of illness episode (figure 2); the changes were also comparable for poor and non-poor children (figure 3). Figure 4 shows that the reduction of more than 90% in children's health expenditures actually reflects considerable narrowing in the distribution of their expenditures. The form of the 2009 distributions confirms that these children were the primary beneficiaries of removing user fees. The narrowing is less marked, but still significant, in children for whom medical expenditures at health centres represented only a fraction of their total expenditure, and thus particularly children living more than 5 km from a centre.
Table 5.
Effect of the intervention on cost of care* at the health centre (source: panel survey)
| Condition | Mean (SD) | Mean saving | Median | |||
|---|---|---|---|---|---|---|
| 2008 | 2009 | 2008 | 2009 | |||
| Severe | 2650 (2039) | 309 (854) | −2341 | −88% | 2125 | 0 |
| Not severe | 3027 (2217) | 468 (1532) | −2559 | −85% | 2600 | 0 |
| D<5 km | 3080 (2239) | 221 (638) | −2859 | −93% | 2550 | 0 |
| D≥5 km | 2508 (1939) | 791 (2087) | −1717 | −68% | 2250 | 0 |
| Q1 | 2898 (2237) | 670 (1230) | −2228 | −77% | 2450 | 0 |
| Other | 2957 (2167) | 348 (1365) | −2609 | −88% | 2500 | 0 |
| All | 2893 (2154) | 414 (1340) | −2479 | −86% | 2450 | 0 |
*Includes fees, medications, and other treatments charged during the episode of care.
Figure 2.

Health expenditure distributions according to illness severity.
Figure 3.
Health expenditure distributions according to income groups.
Figure 4.
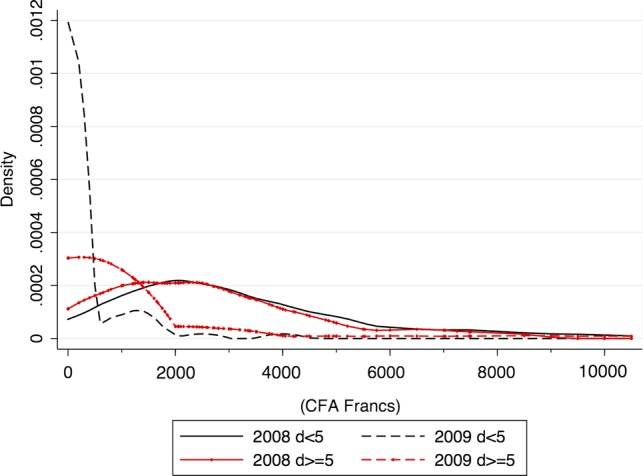
Health expenditure distributions according to place of residence
discussion
Removing user fees responds to healthcare demand
According to the national health information system, in 2011 the attendance levels at health centres in these two districts reached an unprecedented level of 2.3 first curative consultations per year per child under five in Dori and 2.7 in Sebba.19 This is an extraordinarily high rate not only for that country, but for almost all of West Africa. Only in the Kangaba district in Mali, where a similar intervention exempted children from user fees, were comparable levels of utilisation and progression documented in the postintervention period.20 At the country level in Burkina Faso, the number of new curative consultations for children under five was only 1.4 in 2011,19 which testifies to this intervention's success in meeting a need. It should be recalled that after 5 years of user fees implemented in the wake of the Bamako Initiative (1989–1993), the utilisation rate for all ages combined was 0.31 first curative visits per capita per year in Benin and 0.28 in Guinea.21 This rate was still 0.3 in Benin and Guinea in 2010. What is even more impressive in this intervention is that, just 1 year after the removal of user fees (2009), around 82% of children, who had an episode of illness, were able to consult a health professional for care. This is in sharp contrast with the proportion of 50% in the rest of the country in 2010, where children have to pay.11 In Rwanda, in 2008, this proportion was 33% while user fees (copayments) were still in effect, even though 85% of the population was covered by health insurance.22 This very high proportion of use of healthcare services in a context of user fees exemption was also confirmed by a household survey in Sierra Leone, where 3 months after the removal of user fees, 85% of sick children consulted a health professional.23 Likewise in Niger, 70% of children with diarrhoea consulted a health professional in 2009, compared with 17% in 2006, before the exemption.24 This strategy's impact on reducing child mortality, combined with other child survival interventions, has helped save the lives of 59 000 children.25
Removing user fees contributes to more equity in access
While decisionmakers in Burkina Faso have not yet resolved to exempt children from healthcare fees, the results of this intervention suggest that removing user fees improves equity of healthcare access. Not only did this study confirm that exempting children from user fees led to increased service utilisation in general, as was seen in neighbouring Niger and Mali,26 27 but it also corroborated some less-known results, particularly in Uganda, on the progressive character of such a policy option.28–30 Contrary to the inverse equity hypothesis31 or to the situation with respect to public services utilisation in the 1990s, when patients were required to pay user fees in some African countries,5 the intervention benefited the poorest and those who were sicker as much as it did the others, as long as utilisation was not overly constrained by distance to the CSPS. The fact that the most seriously ill children benefited from user fees exemptions bodes well for the struggle against infant mortality, as was shown in a recent study in Niger.25 This leads us to consider this intervention as being pro-poor, which is quite encouraging for improving the health of children, as suggested by studies elsewhere where user fees exemptions were implemented.20 24
But removing user fees is not enough
A survey conducted in parallel concerning this intervention suggests that this progress was achieved without affecting the quality of prescriptions in primary healthcare facilities.13 However, as demonstrated by other studies in Burkina Faso,12 32 lowering the geographic barrier so that sick children living furthest from health centres, who have the same needs as others, can enjoy the same access to care remains a key challenge. The country has built many CSPSs in recent years, bringing health centres closer to the population. These efforts should obviously be continued. For this, health authorities may need to promote the strengthening of transportation systems and experiment with innovative approaches, such as distributing vouchers to facilitate access for the poor in rural areas.
Strengths and limitations of the study
In evaluating this natural experiment, it is not possible to attribute the rise in service utilisation and the reduction in costs unequivocally and exclusively to user fees abolition. Other components of the intervention (eg, supervision and training) may have improved the public's perception of the quality of the service offer. However, another study showed that the quality of medical prescriptions was maintained.13 Thus, given the alignment between the empirical data from this evaluation and the effects demonstrated in other countries,1 20 24 27 we believe the majority of changes observed can be explained by the removal of the financial barrier.
To reinforce the strength of the evidence and the study's internal validity, we used a pattern matching design based on two complementary quantitative methods. Pattern matching designs aim at producing “multiple probes of a causal hypothesis that inform different threats to internal validity without all sharing the same threat.”33 Thus, even if the two-wave household survey could not control for secular trend, the immediate effect found in the time series analysis of the register data largely dominated any trend effect. The magnitudes of the RRs estimates from the two analyses were also comparable (in the region of two on average for fixed effects), and the major part of the effect found in the household survey can reasonably be attributed to the intervention, especially since there is no competing explanation, such as the implementation in 2009 of other interventions that would have encouraged service utilisation.
A first limitation of the study is the length of the postintervention observation window. Extending the points of observation would have allowed us to show the medium-term effects of the intervention and the extent to which the effects were sustained. However, data from the Ministry of Health's health information systems show that the activity continued to progress and, in fact, intensified over the two following years.19 A second limitation lies in the constraints imposed by the size of the sample of sick children, which limits group comparisons and the study of second-order and third-order interactions. We believe, for example, that the inability to identify significant differences in the effects observed in poor children compared with others when taking into consideration severity of illness is probably due to insufficient statistical power. The results of our study nevertheless clearly show that any analysis of the effects of the intervention cannot be limited to looking at the aggregated effects for children, but rather, requires a more discriminating approach that takes into account the combined modifying effects of need, quality of care, ability to pay and geographic access. Unfortunately, our data did not allow us to study, for example, the effects of the intervention in terms of the types of illnesses presented by the children.
Conclusion
Burkina Faso is among the countries with the poorest health indicators. Health needs are largely unfulfilled by the health system, particularly because users are required to pay for care at the point of service. This study shows that point-of-service user fees exemptions enabled more children, and especially those who were more vulnerable because of poverty, sickness or distance from a health centre, to access care and save money. The results provide arguments for scaling up the user fees exemptions nationally, while maintaining quality of care and tackling the geographic barrier.
What is already known on this subject.
User fees reinforce inequities of access to healthcare.
Removing user fees increases utilisation of health care facilities although it is not known whether this strategy benefits everyone or favours the better-off.
What this study adds.
Exemption from user fees had an immediate, substantial effect of increasing access to care and reducing expenses.
The benefits of the exemption were not monopolised by the better-off families.
The exemption was effective but did not overcome barriers caused by distance.
Supplementary Material
Supplementary Material
Acknowledgments
The authors thank the health authorities of Burkina Faso who initiated these interventions and studies, the health workers in the health centres, the community leaders and beneficiaries in the areas studied, as well as the managers and agents of the intervention studied (HELP). A special thanks to AFRICSanté (Issiaka Sombié and Moussa Bougma) for assistance with the household survey data collection and entry. The authors would like to thank Donna Riley for translation and editing support.
Footnotes
Contributors: RH and VR prepared and supervised the field surveys. RH supervised data entry and data management processes and conducted the primary analyses. SH did the analyses and prepared tables and figures. All authors contributed to the interpretation of the results. VR and SH wrote the first draft. All authors read, improved and approved the final manuscript.
Funding: This research was funded by the Humanitarian Aid Service (ECHO) of the European Commission and the Fonds de Recherche en Santé du Québec (FRSQ). Valéry Ridde is a New Investigator of the Canadian Institutes of Health Research (CIHR). The funders and the NGO had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Competing interests: None.
Ethics approval: The research was accepted by the Ministry of Health and the ethics committees in Burkina Faso and Canada (CRCHUM).
Provenance and peer review: Not commissioned; externally peer reviewed.
references
- 1.Lagarde M, Palmer N. The impact of user fees on access to health services in low- and middle-income countries. Cochrane Database Syst Rev 2011;(4):CD009094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.James C, Morris SS, Keith R, et al. Impact on child mortality of removing user fees: simulation model. BMJ 2005;331:747–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meessen B, Hercot D, Noirhomme M, et al. Removing user fees in the health sector: a review of policy processes in six sub-Saharan African countries. Health Policy Plan (Suppl 2) 2011;26:ii16–29 [DOI] [PubMed] [Google Scholar]
- 4.McIntyre D, Ataguba JE. How to do (or not to do) … a benefit incidence analysis. Health Policy Plan 2010;26:174–82 [DOI] [PubMed] [Google Scholar]
- 5.Castro-Leal F, Dayton J, Demery L, et al. Public spending on health care in Africa: do the poor benefit? Bull World Health Organ 2000;78:66–74 [PMC free article] [PubMed] [Google Scholar]
- 6.Mills A, Ataguba JE, Akazili J, et al. Equity in financing and use of health care in Ghana, South Africa, and Tanzania: implications for paths to universal coverage. Lancet 2012;380:126–33 [DOI] [PubMed] [Google Scholar]
- 7.Deininger K, Mpuga P. Economic and welfare impact of the abolition of health user fees: evidence from Uganda. J Afr Econ 2004;14:55–91 [Google Scholar]
- 8.Ridde V. Fees-for-services, cost recovery, and equity in a district of Burkina Faso operating the Bamako Initiative. Bull World Health Organ 2003;81:532–8 [PMC free article] [PubMed] [Google Scholar]
- 9.Gwatkin DR, Rutstein S, Johnson K, et al. Socio-economic differences in health, nutrition, and population. Burkina Faso. Washington: The World Bank-HNP, 2007:149. [PubMed] [Google Scholar]
- 10.Bryce J, Friberg IK, Kraushaar D, et al. LiST as a catalyst in program planning: experiences from Burkina Faso, Ghana and Malawi. Int J Epidemiol 2010; 39(Suppl 1):i40–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.INSD, Measure DHS, ICF Macro Enquête démographique et de santé et à indicateurs multiples (EDSBF-MICS IV), Rapport préliminaire, Burkina Faso, 2010. Ouagadougou: INSD, 2011:40 [Google Scholar]
- 12.Schoeps A, Gabrysch S, Niamba L, et al. The effect of distance to health-care facilities on childhood mortality in rural Burkina Faso. Am J Epidemiol 2011;173:492–8 [DOI] [PubMed] [Google Scholar]
- 13.Atchessi N, Ridde V, Haddad S. Combining user fees exemption with training and supervision helps to maintain the quality of drug prescriptions in Burkina Faso. Health Policy Plan 2012;In press [DOI] [PubMed] [Google Scholar]
- 14.Wane A. Economie du pastoralisme: une analyse bibliographique. Afrique de l'Ouest. Dakar: URP Pastoralisme—PPZS (Pôle Pastoral Zones Sèches), 2006. http://data.iucn.org/wisp/fr/documents_french/west_africa_reports_french.pdf (accédé le 23 janv 2013). [Google Scholar]
- 15.Bennett S, Radalowicz A, Vella V, et al. A computer simulation of household sampling schemes for health surveys in developing countries. Int J Epidemiol 1994;23:1282–91 [DOI] [PubMed] [Google Scholar]
- 16.Snijders T, Bosker R. Multilevel analysis. An introduction to basic and advanced multilevel modeling. 2nd edn London: Sage Publications, 2012 [Google Scholar]
- 17.Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. Hoboken, NJ: Wiley, 2004 [Google Scholar]
- 18.INSD Annuaire statistique. Édition 2008. Burkina Faso. Ouagadougou: INSD, 2009 [Google Scholar]
- 19.ministère de la santé Annuaire statistique 2011. Burkina Faso. Ouagadougou: Ministère de la Santé. DGISS, 2012:196 [Google Scholar]
- 20.Ponsar F, Van Herp M, Zachariah R, et al. Abolishing user fees for children and pregnant women trebled uptake of malaria related interventions in Kangaba, Mali. Health Policy Plan 2011;26:ii72–83 [DOI] [PubMed] [Google Scholar]
- 21.Soucat A, Gandaho T, Levy-Bruhl D, et al. Health seeking behaviour and household health expenditures in Benin and Guinea: the equity implications of the Bamako Initiative. Int J Health Plann Manage 1997;12:S137–63 [DOI] [PubMed] [Google Scholar]
- 22.Lu C, Chin B, Lewandowski J, et al. Towards Universal health coverage: an evaluation of Rwanda Mutuelles in its first eight years. PLoS ONE 2012;7:e39282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Statistics Sierra Leone, Ministry of Health and Sanitation Sierra Leone Multiple Indicator Survey 2010. Freetown, Sierra Leone: Statistics Sierra Leone, Ministry of Health and Sanitation, 2012 [Google Scholar]
- 24.Page AL, Hustache S, Luquero FJ, et al. Health care seeking behavior for diarrhea in children under 5 in rural Niger: results of a cross-sectional survey. BMC Public Health 2011;11:389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amouzou A, Habi O, Bensaïd K, et al. Reduction in child mortality in Niger: a Countdown to 2015 country case study. Lancet 2012. Published Online First: 20 September 2012. http://dx.doi.org/10.1016/S0140-6736(12)61376-2 [DOI] [PubMed] [Google Scholar]
- 26.Barroy H, Carasso BS. Assessing the Effects of Removing User Fees in Zambia and Niger. J Health Serv Res Policy 2012;17:30–6 [DOI] [PubMed] [Google Scholar]
- 27.Heinmüller R, Dembélé YA, Jouquet G, et al. Free healthcare provision with an NGO or by the Malian government—impact on health center attendance by children under five. Field ACTions Sci Rep 2012. Connection on 07 December 2012. http://factsreports.revues.org/1731 [Google Scholar]
- 28.Nabyonga J, Desmet M, Karamagi H, et al. Abolition of cost sharing is pro poor: evidence from Uganda. Health Policy Plan 2005;20:101–8 [DOI] [PubMed] [Google Scholar]
- 29.Deininger K, Mpuga P. Economic and welfare impact of the abolition of health user fees: evidence from Uganda. J Afr Econ 2005;14:55–91 [Google Scholar]
- 30.Xu K, Evans DD, Kadama P, et al. Understanding the impact of eliminating user fees: utilization and catastrophic health expenditures in Uganda. Soc Sci Med 2006;62:866–76 [DOI] [PubMed] [Google Scholar]
- 31.Victora CG, Vaughan JP, Barros FC, et al. Explaining trends in inequities: evidence from Brazilian child health studies. Lancet 2000;356:1093–8 [DOI] [PubMed] [Google Scholar]
- 32.De Allegri M, Ridde V, Louis VR, et al. Determinants of utilisation of maternal care services after the reduction of user fees: a case study from rural Burkina Faso. Health Policy 2010;99:210–18 [DOI] [PubMed] [Google Scholar]
- 33.Shadish WR, Cook TD. The renaissance of field experimentation in evaluating interventions. Annu Rev Psychol 2009;60:607–29 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


