Abstract
Objective
Treatment for alcohol use disorder (AUD) is far less effective for those with a co-occurring anxiety disorder. Surprisingly, adding an independent anxiety treatment to AUD treatment does not substantially improve the poor alcohol outcomes of these patients. This may reflect the lack of attention from independent treatments to the dynamic interaction of anxiety symptoms with alcohol use and drinking motivation. On the basis of this view, we assembled a cognitive behavioral therapy (CBT) program designed to both reduce anxiety symptoms and weaken the links between the experience of anxiety and the motivation to drink.
Method
344 patients undergoing residential AUD treatment with current social phobia, generalized anxiety disorder, or panic disorder were randomly assigned to receive either the CBT or an active comparison treatment, Progressive Muscle Relaxation Training (PMRT). Assessments took place immediately following treatment and 4 months later (n = 247).
Results
As predicted, the CBT group demonstrated significantly better alcohol outcomes 4 months following treatment than did the PMRT group. Although both groups experienced a substantial degree of anxiety reduction following treatment, there were no significant group differences immediately after treatment and only a slight advantage for the CBT group 4 months after treatment.
Conclusions
These findings suggest that specific interventions aimed at weakening the association between the experience of anxiety and drinking motivation play an important role in improving the alcohol outcomes of these difficult-to-treat patients beyond that of anxiety reduction alone.
Keywords: anxiety disorder, alcohol use disorder, cognitive behavioral therapy, comorbidity
Individuals with an anxiety disorder are 2–4 times more likely to be dependent on alcohol than are others in the general U.S. community (Grant et al., 2004; Kessler et al., 1997; Regier et al., 1990), and up to half of all individuals being treated for alcohol dependence also have an anxiety disorder (e.g., Kushner, Sher, & Beitman, 1990). The strong correlation between anxiety disorder and alcohol dependence suggests that important etiologic and/or maintaining processes link these conditions. Consistent with this possibility, studies show that clinically elevated anxiety at the outset of alcohol treatment predicts a poor treatment response (Driessen et al., 2001; Kushner et al., 2005). A straightforward hypothesis extrapolated from these data is that effectively treating co-occurring anxiety disorders would improve alcohol use disorder (AUD) treatment outcomes. However, empirical tests of this intuitively appealing clinical hypothesis have been disappointing.
For example, Bowen, D’Arcy, Keegan, and Senthilselvan (2000) found that 12 hr of standard cognitive behavioral therapy (CBT) for co-occurring panic disorder, a treatment known to be effective in psychiatric patients, produced no better alcohol outcomes than did AUD treatment without CBT. Similarly, Schadé et al. (2004) found that adding CBT for co-occurring phobia (social or agoraphobia) to a standard relapse prevention program improved anxiety but did not improve alcohol outcomes compared with the relapse prevention program alone. Randall, Thomas, and Thevos (2001) found that adding a CBT treatment for social anxiety disorder to a standard AUD treatment program actually resulted in slightly worse alcohol outcomes than the standard alcohol treatment alone. Randall and colleagues (i.e., Book, Thomas, Randall, & Randall, 2008; Thomas, Randall, Book, & Randall, 2008) also reported that treatment of social phobia with paroxetine was successful (relative to placebo) in reducing social anxiety but left the level of hazardous alcohol use in their study sample unchanged after 6 weeks. Although these individual studies have not detected effects for anxiety treatment in terms of alcohol outcomes, a recent meta-analysis did identify a small (d = .22) but significant effect for anxiety treatment relative to control in improving alcohol outcomes when combining the results from all available randomized controlled trials (Hobbs, Kushner, Lee, Reardon, & Maurer, 2011). These modest results suggest that processes beyond simple anxiety reduction should be identified and targeted if the AUD treatment outcomes of patients with co-occurring anxiety disorders are to be improved substantially.
Kushner, Abrams, and Borchardt (2000) described a “vicious cycle” model in which interacting biopsychosocial factors can link anxiety symptoms with alcohol use in a positive-feedback system that exacerbates both conditions. This view implies that directly modifying processes linking anxiety symptoms with alcohol use and craving in these cases could add therapeutic value beyond anxiety reduction alone. Consistent with this view, studies show that alcohol outcome expectancies modulate the extent to which anxiety symptoms correlate with alcohol use (e.g., Kushner, Abrams, Thuras, & Hanson, 2000b; Kushner, Sher, Wood, & Wood, 1994), and other studies show that such expectancies can be directly modified with a corresponding effect on level of alcohol use (e.g., Beck, Wright, Newman, & Liese, 1993; Darkes & Goldman, 1998). Additionally, whereas conditioned cues have long been considered important in promoting alcohol use and craving (e.g., Poulos, Hinson, & Siegel, 1981), more recent studies have shown that anxiety and other negative affect can serve as conditioned cues for alcohol craving and relapse and that the strength of these associations can be lessened through extinction training (e.g., Cooney, Litt, Morse, Bauer, & Gaupp, 1997; Litt, Cooney, Kadden, & Gaupp, 1990; Sinha, 2009).
On the basis of these ideas, Kushner and colleagues (2006) developed and tested a prototype of a hybrid CBT treatment that integrated standard CBT-based panic disorder treatment techniques (e.g., Barlow, Craske, Cerny, & Klosko, 1989) with parallel content aimed at disrupting psychological processes linking anxiety feelings to alcohol use (e.g., Kushner, Abrams, & Borchardt, 2000). Using a quasi-experimental design, Kushner and colleagues (2006, 2009) demonstrated that standard AUD treatment augmented by the hybrid CBT resulted in better 4-month alcohol outcomes than did the AUD treatment alone. However, several potentially important limitations noted in that work included (a) many interested patients who reported drinking to manage social or generalized anxiety symptoms could not participate in the study because they did not have panic disorder; (b) many patients who did participate in the study also experienced significant social and/or generalized anxiety symptoms that, unlike panic disorder symptoms, were not specifically addressed in the prototype hybrid CBT; and (c) use of a nonrandomized quasi-experimental design with AUD treatment as usual as the control group precluded the drawing of strong conclusions regarding the specific treatment effects of the hybrid CBT.
The prototype hybrid CBT tested by Kushner and colleagues (2006, 2009) focused on AUD treatment patients with co-occurring panic disorder. However, the scientific literature on which the vicious cycle model was based (cf. Kushner, Abrams, & Borchardt, 2000) did not specify important differences between various domains of internalizing psychopathology in terms of their association with AUD. Consistent with this, Menary, Kushner, Maurer, and Thuras (2011) showed that the increased risk for AUD associated with drinking to manage anxiety was not restricted to any single anxiety disorder subtype. Similarly, Kushner, Wall, et al. (2012) showed that the variance shared by common anxiety (and depression) disorders relate more strongly to AUD risk than does variance that is unique to a single anxiety disorder. Underlying these scientific findings is the high intercorrelation among various internalizing disorders in those with AUDs (e.g., Andrews, Slade, & Issakidis, 2002; Boyd et al., 1984; T. A. Brown, Campbell, Lehman, Grisham, & Mancill, 2001; Kushner et al., 2005; Kushner, Krueger, Frye, & Peterson, 2008; Magee, Eaton, Wittchen, McGonagle, & Kessler, 1996). On the basis of the empirical and theoretical indications that the core processes linking anxiety and AUD transcend specific anxiety diagnoses, along with the practical implications of highly intercorrelated internalizing disorders (above), we concluded that the panic-centric hybrid CBT prototype of Kushner et al. (2006) could and should be expanded to include patients with other common internalizing disorders.
In the present study, individuals undergoing a standard community-based AUD treatment with either panic, social, or generalized anxiety disorder were randomized to also receive either the expanded hybrid CBT or an active comparison control treatment, Progressive Muscle Relaxation Training (PMRT; Bernstein & Borkovec, 1973; Jacobson, 1938). PMRT is a widely disseminated program for managing a broad spectrum of anxiety and stress problems that can be easily administered by nonspecialists (e.g., Conrad & Roth, 2007; Jorm et al., 2004; Manzoni, Pagnini, Castelnuovo, & Molinari, 2008; Siev & Chambless, 2007). Features of PMRT that made it attractive as a comparison to the CBT include (a) credibility as a treatment for anxiety in this population, (b) a transdiagnostic focus that could be reasonably applied to any of the qualifying anxiety disorders, (c) a time frame and intensity level that could easily be made to match those of the hybrid CBT, and (d) a focus on anxiety/stress management without any reference to the association of stress or anxiety to alcohol use. This latter feature, in particular, helps to experimentally isolate treatment elements aimed at anxiety reduction (both the CBT and PMRT programs) from those aimed at decoupling anxiety experiences from alcohol use and craving (the CBT program only).
The primary aim of this study was to test whether the hybrid CBT, relative to PMRT, improves 4-month alcohol outcomes in AUD treatment patients with any of several common co-occurring anxiety disorders. A secondary aim of this work was to explore whether anxiety outcomes at the posttreatment assessment mediate or moderate group effects on alcohol outcomes at the 4-month assessment. Note that mediation analyses use anxiety outcomes from the posttreatment assessment (just prior to discharge from the residential AUD program) and alcohol outcomes from the 4-month assessment in order to (a) establish the temporal priority of the putative mediator relative to the outcome and (b) avoid the potential for the confounding of anxiety outcomes with alcohol relapse. (Here, it was presumed that participants could not have relapsed to drinking by the posttreatment assessment because they had not yet been discharged from the closely monitored residential program.) Finally, we evaluated whether differences on clinical variables related to either anxiety (e.g., the particular qualifying anxiety diagnosis) or alcohol (e.g., severity of use prior to treatment) moderated the association between treatment group and alcohol outcomes.
Method
Participants
Inclusion/exclusion criteria
All participants were drawn from an adult (age ≥ 18) community-based residential AUD treatment program located in a medium-sized metropolitan area in the midwestern United States. Inclusion required current (past 30 days) alcohol dependence and at least one of the following anxiety disorders: panic disorder, social anxiety disorder, or generalized anxiety disorder. Individuals were excluded from participation if they had a history of bipolar disorder or schizophrenia, as well as if they had conditions deemed likely to interfere with their capacity to fully participate in the study such as cognitive impairment or serious ongoing suicidality. Patients were also excluded if they were unable to read and understand English. Patients were not excluded if they had major depression, posttraumatic stress disorder, or drug dependence; however, we only included those seeking treatment primarily for alcohol- (vs. other drug-) related problems. This study was approved by the University of Minnesota’s Institutional Review Board. Each participant provided their informed consent to be in the study.
Recruitment
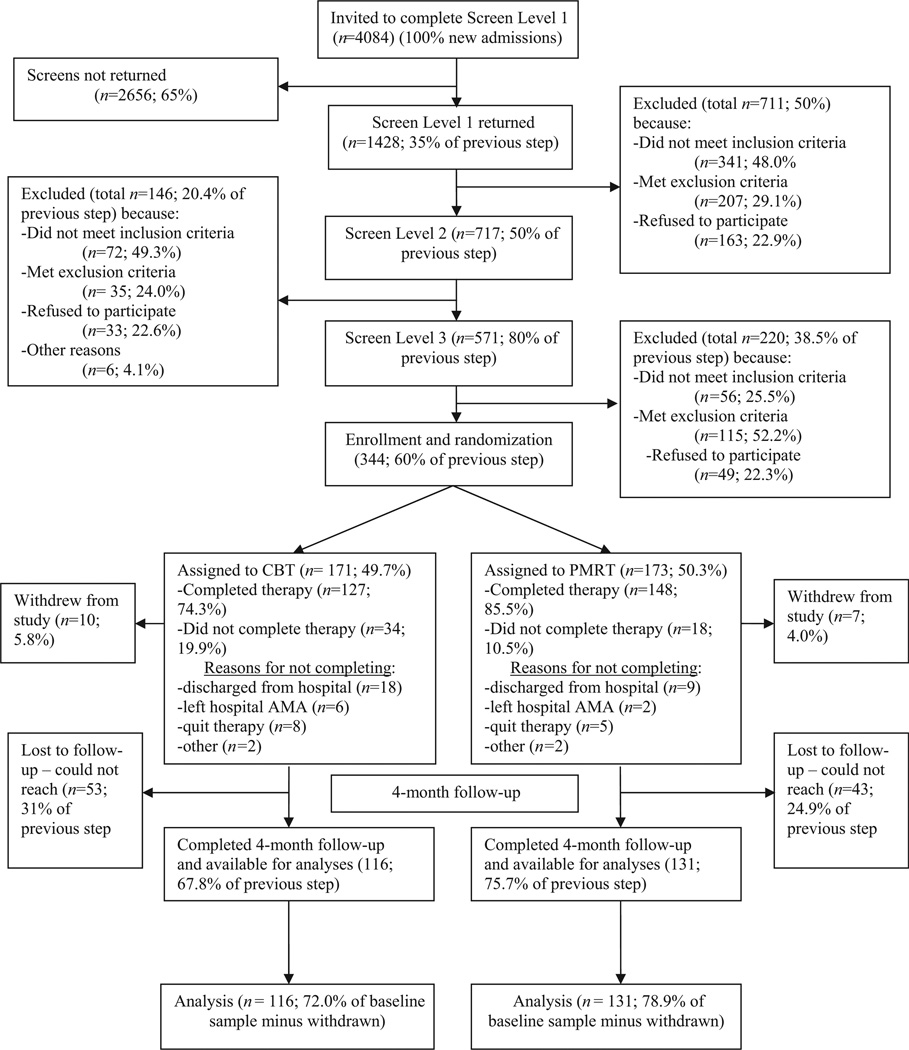
Figure 1 shows the flow of individuals through the various stages of recruitment and the study itself. Participant recruitment occurred over a 4-year period and took place in a 61-bed adult 21-day residential chemical dependency treatment center. Screening for qualified participants involved three levels of assessment that took place within a patient’s first week in the AUD treatment program. The Level 1 and Level 2 screening steps emphasized identifying all individuals who might be qualified and interested in participating (i.e., minimizing false negatives), whereas the Level 3 screening step emphasized the exclusion of individuals who were not qualified to participate (i.e., minimizing false positives). In the Level 1 screening step (see Figure 1, top box), we offered a brief screening questionnaire to 100% of patients entering the AUD treatment over the period of recruitment. Here, patients were asked to indicate the primary substance of abuse for which they were seeking treatment and whether they had experienced any disturbing “anxiety attacks,” excessive worry, or anxiety/discomfort in (or anxiety-related avoidance of) social situations in the past 30 days. Individuals who endorsed alcohol as the primary substance for which they were receiving treatment, as well as symptoms related to at least one of the anxiety domains of interest, were invited to attend a brief semistructured interview (Screen Level 2 shown in Figure 1). In this step, potential participants were asked by a trained research assistant to elaborate on the endorsements they made in response to the earlier screen questions. The clinical team (including at least one staff psychologist) then evaluated the interview responses related to inclusion/exclusion criteria to determine whether further screening was warranted (i.e., Screen Level 3), including a formal diagnostic interview (described below).
Figure 1.
Recruitment flowchart. CBT = cognitive behavioral therapy; AMA = against medical advice; PMRT = Progressive Muscle Relaxation Training.
Study therapy completion rates
As shown in Figure 1, there was a difference in the rate of study therapy completion between the groups: 74.3% in the CBT group versus 85.5% in the PMRT group. This group effect was statistically significant (χ2 = 6.67, p = .01). In spite of this difference, the proportion that dropped out for the various reasons listed in Figure 1 is reasonably comparable between the two groups. For example, 18 (53%) of the CBT noncompleters did not complete the therapy because of early discharge from the AUD program versus nine (50.0%) of the PMRT noncompleters. This is the single largest reason for subject loss in either group and was presumably unrelated to which group an individual had been randomized. Nonetheless, it was unexpected and potentially relevant that the number of those who dropped out for any reason was greater in the CBT group.
Study participation/adherence rates
Completion of assigned practice/homework was high (>80%) in both groups, although participants in the CBT group did complete their assignments more often than did individuals in the PMRT group (91% vs. 81%), F(1, 214) = 7.23, p = .008. Also, therapists indicated on a 10-point scale that those in the CBT group were more enthusiastic about therapy and comprehended the therapy better than those in the PMRT group (“enthusiasm”: CBT M = 9.0, SD = 0.95 vs. PMRT M = 7.5, SD = 1.42), F(1, 325) = 116.2, p < .001 (“comprehension”: CBT M = 9.2, SD = 0.87 vs. PMRT M = 8.2, SD = 1.13); F(1, 325) = 86.63, p < .001. Using a 4-point scale, therapists also rated individuals in the CBT group as more cooperative/eager than individuals in the PMRT group (CBT M = 3.5, SD = 0.43 vs. PMRT M = 3.25, SD = 0.43), F(1, 325) = 26.29, p < .001. Finally, therapists completed postsession checklists to monitor the degree to which all materials were presented after each session. These data showed that all material was presented in 99% of CBT sessions and 98% of PMRT sessions.
Follow-up retention
Efforts to contact participants included multiple modalities (e.g., phone, e-mail, letters) and the use of informants where authorized. However, due in part to the fact that many participants were undomiciled (“homeless”) at some point over the course of the study, we had difficulty locating some individuals for the follow-up. In fact, participant loss at follow-up in nearly all cases was due to our inability to locate participants rather than their refusal to participate once located. As shown in Figure 1, we retained 72% of the CBT group and 79% of the PMRT group at the 4-month follow-up. This group difference was not statistically significant.
The final sample
The final sample with complete follow-up data included 247 individuals (75.5% of those captured at the baseline), 146 men and 101 women, ranging in age from 18 to 68 years, with a mean age of 39.8 years (SD = 10.5 years).
Assessment Time Frames
The baseline assessment occurred at the point of enrollment-randomization, just prior to initiation of the study treatment and about 1 week after the participant had started the AUD treatment program or, if relevant, after medically supervised detoxification. The posttreatment assessment occurred in the brief period (usually 1–2 days) between the completion of the 6-day study treatment and discharge from the AUD residential program. (As noted earlier, this approach was meant to ensure that participants had not relapsed prior to the posttreatment assessment.) The 4-month follow-up assessment occurred approximately 120 days following completion of the study treatment. Study staff began attempts to contact participants to schedule the in-person 4-month follow-up assessment approximately 90 days after the participant completed the study therapy. Appointments were scheduled within a window that began at this contact point and extended for the next 30 days.
Symptom and Diagnostic Assessments
Alcohol and anxiety diagnoses for the purpose of inclusion
We established the presence of relevant psychiatric diagnoses at baseline for inclusion purposes using the Structured Clinical Interview for DSM-IV (SCID; First, Spitzer, Gibbon, & Williams, 1989). The SCID has demonstrated good reliability in multiple studies, with Ks > 0.70 for most psychiatric diagnoses (Segal, Hersen, & Van Hasselt, 1994; Summerfeldt & Antony, 2004). Diagnostic modules included panic disorder (with or without agoraphobia; PD), social anxiety disorder (SAD), generalized anxiety disorder (GAD), major depressive disorder, posttraumatic stress disorder, and alcohol dependence. The SCID was also slightly modified on the basis of the approach outlined by Andrews et al. (2002) to establish a “principal” anxiety disorder (PD, SAD, or GAD) for those participants with more than one of the inclusionary anxiety disorders. In these cases, the participant was asked to nominate a principal anxiety disorder from all the anxiety disorders for which they met diagnostic criteria based on the grouping of symptoms that “troubles you the most.” We used this distinction to test our prediction that anxiety disorder type would not moderate the effects of the treatment. A doctoral-level staff psychologist qualified in SCID administration and training was responsible for training other relevant staff in the valid use of the SCID using standard training materials (First et al., 1989). All diagnostic decisions were made using a clinical consensus model with the principal investigator (PI; MGK), who adjudicated any cases in which the team could not reach consensus.
Characterizing alcohol consumption for the purpose of outcome analyses
The time line follow-back (TLFB) interview (Sobell & Sobell, 1995) was used to identify daily drinking patterns of patients in the 4 months before and after treatment. The TLFB has been shown to have adequate psychometric qualities in both clinical and nonclinical populations (Sobell & Sobell, 1995). Using a calendar, the respondent provides retrospective estimates of daily drinking over a specified amount of time. Several memory aids can be used to enhance recall (e.g., holidays, special weekend events). Interviewers were trained to record the number of drinking behaviors based on the manual provided by Sobell and Sobell (1995), with a standard drink defined as one ounce of alcohol spirits, four ounces of wine, or 12 ounces of beer. The primary dependent variables were derived from the TLFB daily drinking estimates and included any alcohol use, any binge (defined as four drinks for women and five drinks for men), and any 3 consecutive days of alcohol use. We derived additional alcohol outcomes by calculating counts of the number of times each of these categorical outcomes occurred.
Characterizing anxiety symptoms and clinical status at the outcome assessments
We used the Spielberger State-Trait Anxiety Inventory (STAI; Spielberger & Sydeman, 1994) to quantify anxiety disturbance both in terms of a continuous measure of symptoms and as a categorical measure of clinical “case” status. The STAI is a 20-item self-report measure with two versions: one reflecting anxiety symptoms “at this moment” (State version) and one reflecting anxiety symptoms “in general” (Trait version). Items are to be rated on a 4-point Likert-type scale with reference to symptoms such as “I feel frightened” and “I have disturbing thoughts,” with some items reverse coded (e.g., “I am a steady person”). The continuous scores on the STAI were based on a sum of the 20 items after reverse coding. The binary case categorizations were made on the basis of whether STAI scores were equal to or above 44 (a clinical anxiety “case”) versus below 44 (not a clinical anxiety “case”). Our decision to use a threshold score of 44 was based on data (e.g., Oei, Evans, & Crook, 1990) summarized by Antony, Orsillo, and Roemer (2001) in their comprehensive practitioner’s guide to anxiety assessment showing that this value was the lowest STAI threshold recommended for detecting any of the specific anxiety disorders included in this study.
There were multiple reasons why we identified the STAI to serve as the primary anxiety outcome measure. First, we sought a single transdiagnostic anxiety measure that would be relevant to all participants regardless of their principal anxiety diagnosis. This approach was consistent with our transdiagnostic conceptualization of the association between anxiety states and alcohol use (see the introduction). This approach also obviated the numerous analytic challenges associated with using a separate symptom measure for each of the qualifying anxiety syndromes. Second, we sought a measurement approach that could accommodate the disparate assessment time frames of the posttreatment versus the 4-month assessment. Although both versions of the STAI were given at both assessment points, the State version was considered more informative at the posttreatment assessment because it could better reflect anxiety levels in the brief time frame (a few hours to a few days) from the end of the study treatment to the postassessment occurring just prior to discharge from the residential AUD program. Alternatively, the Trait version was considered more informative at the 4-month assessment because it would better reflect anxiety levels in the months since the treatment ended.
Drug use
Drug use was characterized at baseline and follow-up using the validated, self-report version of the Addiction Severity Index (ASI-SR; McLellan et al., 1992; Rosen, Henson, Finney, & Moos, 2000). The ASI-SR asks questions about the use of various drugs of abuse in the 30 days prior to the assessment. In addition, the ASI-SR includes questions about problems resulting from drug use, level of self-concern regarding drug problems, and one’s subjective sense of need for drug use treatment. The self-reported ASI has demonstrated adequate reliability and validity (Leonhard, Mulvey, Gastfriend, & Schwartz, 2000; Mäkelä, 2004).
Treatments
AUD treatment as usual (TAU)
All participants were patients in a community-based 21-day residential AUD TAU program. The AUD TAU program is based on the “Minnesota Model” in which the primary goal is lifetime abstinence from alcohol with therapy based on principles of the 12-step philosophy, including frequent meetings with other recovering people, repair of family relationships, healthy changes in daily behaviors, and attention to spiritual growth. Patients live on-site over the course of the treatment in one- and two-person dorm rooms. Therapy programming occurs from 8 a.m. until 3 p.m. in 60- to 90-min blocks on Monday through Friday.
Study treatments: General
Both the CBT and PMRT treatments included six 1-hr sessions that, as far as possible, occurred on sequential business days just after the conclusion of daily programming in the AUD TAU at 3 p.m. Both the CBT and PMRT allowed for group delivery to enhance their fit with the standard substance abuse treatment model and to ensure that we could accommodate all eligible patients. (Due to the relatively slow influx of new participants into the study, however, the number of individuals in each study treatment at any given time was typically between one and three.) Both therapies were fully manualized and highly structured with semiautomated delivery (see details below) to ensure that all elements of each session of the therapies were being delivered to each participant with the same sequence and content. Finally, all participants were instructed to practice techniques introduced in treatment on their own between the sessions.
Participants were randomly assigned to treatment groups in blocks of four within each principal anxiety disorder (see above). The team statistician sealed each block of group assignments in an envelope to be opened by the study manager as participants were enrolled in the study.
Study treatments: The CBT
The CBT splits its six 1-hr sessions into three primary content domains (psychoeducation, cognitive restructuring, and exposure/habituation), each of which are the focus of two yoked sessions: one focused on anxiety symptoms exclusively and one focused on the association between anxiety feelings and alcohol use/craving. For example, in the cognitive-restructuring domain, one session focused on recognizing and modifying anxiety-related catastrophic thinking and one focused on recognizing and modifying inaccurate beliefs and expectancies about the effects of alcohol on anxiety symptoms. The content for the anxiety-only sessions was synthesized from a survey of published work such as that of Barlow (2001); Beck, Emery, and Greenberg (2005); and Foa and Kozak (1986). The content for material focused on the linkages between alcohol and anxiety was also synthesized by the investigators, including a psychoeducation session overviewing facts about comorbidity and the conceptual model on which the treatment is based (cf. Kushner, Abrams, & Borchardt, 2000), a cognitive restructuring session addressing beliefs and expectancies about alcohol’s effects on anxiety feelings (Beck et al., 1993; Darkes & Goldman, 1998; Kushner, Abrams, Thuras, & Hanson, 2000; Kushner et al., 1994), and an exposure/habituation session addressing conditioned associations between anxiety and alcohol use (e.g., Cooney et al., 1997; Litt et al., 1990; Sinha, 2009).
One of two doctoral-level psychologists delivered all CBT therapy sessions. The training entailed (a) reading completely through the treatment manual as well as pertinent scholarly articles (e.g., Kushner, Abrams, & Borchardt, 2000), (b) observing a trained therapist deliver the treatment with a discussion and questions of technique following, and (c) delivering the treatment to a live participant while another trained observer provided feedback. Group consultation between the therapists and PI took place on a semiweekly basis (or more frequently as needed) to discuss the progress of each case and to resolve any other treatment issues that arose. These case consultation meetings also served the purpose of providing ongoing calibration of method and decision making between the two study therapists.
Summaries of the major points and techniques for each of the six CBT sessions were developed into a Microsoft PowerPoint slideshow. The therapist conducted each session while projecting the slide set pertaining to that session so that all key points were always made and all techniques were always deployed. The slides also prompted the therapist when an in-session exercise was to take place. These exercises were aimed at allowing the participant to practice applying each general technique to their particular symptoms and circumstances. To ensure that there was time in each session to cover the required material, and to ensure that the sessions did not include extracurricular therapeutic interactions, the therapists were instructed to refer any clinical issues not directly pertaining to the therapy brought up by patients to a counselor in the AUD program, unless the issue was deemed an emergency, in which case appropriate action would be taken by study personnel.
Finally, to provide an identity for the CBT treatment that distinguishes it from the myriad CBT protocols developed for application in anxiety disorders, alcohol dependence, or both, we chose the distinctive and descriptive name: “Breaking the Drinking and Anxiety Connection” (BDAC) and, henceforth, refer to the hybrid CBT treatment by the acronym CBT-BDAC. However, note that we did not refer to the treatment by this name to participants in either group out of concern it could introduce experimental bias (e.g., positive in the CBT-BDAC group or negative in the PMRT group). Because of this, we referred to both the CBT and the PMRT with the patients as a treatment based on behavioral and cognitive principles that include stress and anxiety reduction components.
Study treatments: The PMRT
The comparison treatment, PMRT, was taken from Progressive Relaxation Training: A Manual for the Helping Professions (Bernstein & Borkovec, 1973). The program was adapted slightly to match the CBT-BDAC program in terms of session length (1 hr) and number (six). In Session 1, a 16-muscle group tension-release routine was taught and practiced. In Session 2, a seven-muscle group tension-release routine was taught and practiced. In Sessions 3–5, a four-muscle group tension-release routine was taught and practiced. In Session 6, a whole-body relaxation via cued (e.g., count) muscle memory was taught and practiced. Participants were instructed to practice the technique covered in each session on their own prior to the following session. The PMRT was read directly from a script in each session and so was necessarily delivered reliably and completely from session to session. Because the PMRT was 100% scripted with no participant–therapist interactivity, it was delivered by a postbachelorette research therapist.
Analytic Approach
Main effects
Categorical alcohol outcome variables were tested using chi-square and logistic regression analyses. Count-based alcohol outcomes were tested within Poisson regression models using negative binomial regression to adjust for some overdispersion (i.e., the variance exceeds the mean) in the outcome measures. We report effect sizes including Cohen’s d, partial η2, and odds ratios (with 95% confidence intervals). Note here that we chose to contrast groups on counts of days in which events occurred (e.g., number of drinking days) versus proportion of days in which events occurred (e.g., percent days drinking) because the former is better suited to manage the large number of zero cases (i.e., days in which no alcohol was used) in the statistical tests (Agresti, 2002). In order to control for differential numbers of follow-up days (e.g., if some days were not counted due to hospitalization or variations in the follow-up period among participants), count variables were calculated in per-month units using only days on which patients were eligible to drink. (Adjusted counts were rounded to whole numbers using conventional rounding rules.) Consistent with our focus on external validity and treatment effectiveness, we used an intent-to-treat strategy for all analyses.
Anxiety outcomes in response to treatment was examined using two methods, as alluded to above. First, mean State and Trait Anxiety scores at the posttreatment and 4-month assessments were entered into an analysis of covariance along with treatment group and mean score on State or Trait Anxiety at baseline as the covariate. Additionally, chi-square analyses were used to compare the proportion of individuals in each group exceeding a clinical cutoff score (44 or higher) for each anxiety measure at the posttreatment and 4-month assessment points. All cases were used for continuous (mean-based) anxiety outcome analyses; however, for the threshold analyses, we excluded the small number of cases that did not exceed the threshold on the anxiety measure at baseline (percentages noted in Table 4). This was done to ensure that a subthreshold status at posttreatment and the 4-month assessments indicated a change in status since baseline.
Table 4.
Anxiety Measures and Threshold Status at Baseline, Posttreatment, and 4-Month Follow-Up by Treatment Group
| CBT-BDAC |
PMRT |
||||||
|---|---|---|---|---|---|---|---|
| Variable | M | Adj. M | SD | M | Adj. M | SD | p |
| Trait Anxiety (Ms) | |||||||
| Baseline | 58.03 | — | 10.67 | 56.02 | — | 10.18 | .09† |
| Posttreatment | 42.86 | 42.01 | 10.81 | 42.82 | 43.27 | 10.42 | .27 |
| 4 month | 41.41 | 41.02 | 12.36 | 44.07 | 44.43 | 12.41 | .03* |
| State Anxiety (Ms) | |||||||
| Baseline | 52.90 | — | 12.95 | 50.35 | — | 12.36 | .07† |
| Posttreatment | 40.33 | 39.70 | 12.43 | 38.03 | 38.56 | 11.86 | .40 |
| 4 month | 37.50 | 37.31 | 12.89 | 39.09 | 39.99 | 13.03 | .11 |
| Trait Anxiety (below cutoff; %) | |||||||
| Baseline | 9.6 | 13.0 | .34 | ||||
| Posttreatmenta | 51.8 | 45.5 | .34 | ||||
| 4 montha | 53.5 | 39.3 | .04* | ||||
| State Anxiety (below cutoff; %) | |||||||
| Baseline | 25.3 | 30.1 | .34 | ||||
| Posttreatmentb | 53.9 | 55.9 | .79 | ||||
| 4 monthb | 65.8 | 58.0 | .30 | ||||
Note. CBT = cognitive behavioral therapy; BDAC = Breaking the Drinking and Anxiety Connection; PMRT = Progressive Muscle Relaxation Training; Adj. = Adjusted. Dashes indicate no adjusted data point was available.
The participants who did not exceed clinical cutoff threshold at baseline on Trait Anxiety (9.6% in CBT-BDAC and 13% in PMRT) were not used for these comparisons to ensure that all cases below threshold at the follow-up reflected a clinical change from baseline.
For the same reason, as in Trait Anxiety, the participants who did not exceed clinical cutoff threshold at baseline on State Anxiety (25.3% in CBT-BDAC and 30.1% in PMRT) were not used for these comparisons.
p < .10.
p < .05.
Moderator tests
We created interaction terms between treatment group and the following baseline moderators: (a) principal anxiety disorder (PD, SAD, or GAD); (b) baseline anxiety disorder “load” (one vs. more than one anxiety disorder); (c) presence of drug use at baseline (yes vs. no); (d) presence of major depression disorder at baseline (yes vs. no); (e) gender (male vs. female); (f) baseline psychiatric medication use (yes vs. no); and (h) anxiety threshold status at baseline (above vs. below the STAI clinical threshold). In addition to these baseline moderator variables, we also examined posttreatment anxiety threshold status (again, above vs. below the clinical threshold) as a moderator of 4-month alcohol outcomes. To eliminate redundancies and maintain brevity surrounding these secondary data analyses, moderator tests were limited to categorical (vs. count) alcohol outcomes. Logistic regression analyses were used to test the moderator models.
Mediator test
As noted in the introduction, we planned to conduct mediator analyses to determine whether group effects on posttreatment anxiety outcomes lead to group differences on 4-month alcohol outcomes. These analyses would only be conducted, however, if all preconditions for mediation testing outlined by Baron and Kenny (1986) are met, including (a) a significant effect of treatment group on 4-month alcohol outcomes; (b) a significant effect of treatment group on posttreatment anxiety; and (c) a significant effect of posttreatment anxiety on 4-month alcohol outcomes. Four-month anxiety outcomes were not considered relevant to mediator tests because this would leave the temporal/ causal relationship between the putative mediator (treatment effects on posttreatment anxiety) and the outcome of interest (treatment effects on alcohol outcomes) undetermined. This issue was considered especially problematic in the present study because anxiety symptoms and alcohol use can exercise reciprocal causal influence (e.g., Kushner, Abrams, & Borchardt, 2000; Kushner, Sher, & Erickson, 1999).
Results
Demographic and Clinical Characteristics by Group
Baseline
As shown in Table 1, the study groups did not differ significantly on any core demographic or clinical variables at baseline. As expected from the blocking used in the randomized group assignment scheme, rates of the various principal anxiety disorders were highly similar between groups. Also suggesting that the random assignment was successful in distributing key patient characteristics between the study groups, the number of anxiety disorders individuals had (an indicator of anxiety disorder load or severity) was highly similar between the groups.
Table 1.
Baseline Demographics and Clinical Characteristics by Group
| Variable | CBT-BDAC (n = 171) % |
PMRT (n = 173) % |
p |
|---|---|---|---|
| Gender (% female) | 37 | 42 | .33 |
| Racea | .34 | ||
| African American | 13 | 8 | |
| American Indian | 6 | 8 | |
| Asian | 0 | 2 | |
| Hispanic | 1 | 2 | |
| White | 81 | 76 | |
| Other | 0 | 4 | |
| Antianxiety/antidepressant medication use | 63 | 65 | .31 |
| Illicit drug use | 57 | 57 | .97 |
| Major depression diagnosis | 45 | 43 | .72 |
| Principal anxiety disorder | .97 | ||
| GAD | 39 | 38 | |
| PD | 17 | 17 | |
| SAD | 44 | 45 | |
| Number of anxiety disorders | .82 | ||
| =1 | 44 | 46 | |
| >1 | 56 | 54 | |
| Years |
Years |
||
| Age: M(SD) | 39.10 (9.72) | 39.49 (10.58) | .73 |
| Age of principal anxiety onset: M(SD) | 17.36 (11.13) | 17.49 (11.15) | .82 |
| Age of first regular drinking: M(SD) | 19.00 (5.90) | 18.91 (5.20) | .78 |
Note. CBT = cognitive behavioral therapy; BDAC = Breaking the Drinking and Anxiety Connection; PMRT = Progressive Muscle Relaxation Training; GAD = generalized anxiety disorder; PD = panic disorder; SAD = social anxiety disorder.
Because of small cell sizes, the significance test for race contrasts “White” versus all other categories.
Comparison of follow-up completers to noncompleters
In order to determine whether subject loss over the 4-month follow-up (see Figure 1) was systematic in any important way, we contrasted those who did versus those who did not provide follow-up data on all baseline variables. There were no significant main effects for follow-up status (collapsing across treatment groups) and only one significant interaction of group by follow-up status: gender (Wald χ2 = 3.93, p = .048, OR = .37, [.14, .99]). To explore this interaction, we ran chi-square comparisons on gender separately for each treatment group. We found that in the CBT-BDAC group, 64% of males and 78% of females provided follow-up data (χ2 = 3.90,p = .048, Cohen’s d = .31, OR = 2.05, [1.01, 4.17]). In contrast, males and females provided follow-up data at a nonsignificantly different rate in the PMRT group (78% of males and 73% of females provided follow-up data).
Effect of Treatment Group on Alcohol Outcomes at 4-Month Follow-Up
As shown in Table 2, the rates of relapse to any drinking and to any 3 consecutive days of drinking by the 4-month follow-up were significantly higher in the PMRT group compared with the CBT-BDAC group (any drinking: Wald χ2 = 4.05, p = .04, Cohen’s d = .26, OR = 1.68, [1.01, 2.78]; and 3 consecutive days drinking: Wald χ2 = 3.71, p = .05, Cohen’s d = .25, OR = 1.78, [.99, 3.20]). Similarly, the group difference for relapse to binge drinking was in the predicted direction, but this effect only approached statistical significance (Wald χ2 = 2.59, p = .11, Cohen’s d = .21, OR = 1.52, [.91, 2.52]). The CBT-BDAC group had superior outcomes in all analyses involving count-based outcomes, including drinks per month (Wald χ2 = 25.63, p < .001, Cohen’s d = .68, OR = 1.92, [1.49, 2.48]); drinking days per month (Wald χ2 = 10.23, p = .001, Cohen’s d = .42, OR = 1.62, [1.21, 2.18]); and number of binge days per month (Wald χ2 = 13.46, p < .001, Cohen’s d = .48, OR = 1.76, [1.30, 2.39]).
Table 2.
Alcohol Use Variables at Baseline and 4-Month Follow-Up by Treatment Group
| Variable | CBT-BDAC % | PMRT % | pa | ||
|---|---|---|---|---|---|
| Relapse to any alcohol use | |||||
| Baseline | |||||
| 4 month | 41.4 | 54.2 | .04 | ||
| Relapse to bingeb | |||||
| Baseline | |||||
| 4 month | 37.9 | 48.1 | .11 | ||
| Relapse to 3 consecutive days drinking | |||||
| Baseline | |||||
| 4 month | 19.8 | 30.5 | .05 | ||
| Total drinks per monthc |
M |
SD (SE) |
M |
SD (SE) |
|
| Baseline | 450.87 | 385.72 (29.94) | 399.02 | 330.55 (25.97) | .33 |
| 4 month | 27.03 | 77.05 (2.56) | 52.02 | 119.67 (4.59) | <.001 |
| Drinking days per month | |||||
| Baseline | 20.44 | 8.76 (.68) | 20.67 | 9.14 (.72) | .81 |
| 4 month | 2.03 | 5.59 (.23) | 3.30 | 6.85 (.33) | .001 |
| Binge days per month | |||||
| Baseline | 19.71 | 9.13 (.71) | 19.51 | 9.56 (.75) | .84 |
| 4 month | 1.71 | 4.95 (.20) | 3.01 | 6.66 (.30) | <.001 |
Note. Four-month count-based analyses are displayed in the section following the rows pertinent to the “Relapse to 3 consecutive days drinking” outcome. Analyses for all 4-month count-based outcomes use a Poisson negative binomial regression as a means of accounting for a high number of zero cases and overdispersion of the distribution. CBT = cognitive behavioral therapy; BDAC = Breaking the Drinking and Anxiety Connection; PMRT = Progressive Muscle Relaxation Training.
p values shown in bold indicate statistically significant effects.
Binge drinking is defined by National Institute on Alcohol Abuse and Alcoholism guidelines as four drinks per drinking episode for women and five drinks per drinking episode for men.
The p value for the group comparison on drinks per month at baseline was based on log-transformed values; however, raw values are shown in the table to facilitate comparison between baseline and the 4-month outcome.
Baseline Variables as Moderators of the Effect of Treatment Group on Alcohol Outcomes at 4-Month Follow-Up
We examined seven baseline variables as potential moderators of group effects on the three categorical alcohol outcomes: (a) principal anxiety disorder (PD vs. SAD vs. GAD); (b) anxiety load (one vs. more than one anxiety disorder); (c) presence of drug use (yes vs. no); (d) presence of major depressive disorder (yes vs. no); (e) gender (male vs. female); (f) prescription antianxiety/depression medication use (yes vs. no); and (g) State and Trait Anxiety threshold status (above vs. below the clinical cutoff). For each analysis, we entered treatment group and the moderator as main effects and then entered the interaction term for the Group × Moderator variable. Table 3 shows the percentages of those who did versus those who did not relapse to any drinking, binge drinking, and 3 consecutive days drinking separately for each treatment group by levels of the various moderators.
Table 3.
Baseline Variables as Moderators of the Effect of Treatment Group on Alcohol Outcomes at 4-Month Follow-Up
| Relapse to any alcohol use (%) |
Interaction term statistic (moderator by group) |
Relapse to binge (%) |
Interaction term statistic (moderator by group) |
Relapse to 3 consecutive days drinking (%) |
Interaction term statistic (moderator by group) |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline moderator | CBT-BDAC | PMRT | χ2 | p | CBT-BDAC | PMRT | χ2 | p | CBT-BDAC | PMRT | χ2 | p |
| Principal anxiety diagnosis | .50 | .78 | .76 | .68 | 1.63 | .44 | ||||||
| GAD (38.7%) | 44.7 | 52.0 | 40.4 | 44.0 | 23.4 | 26.0 | ||||||
| PD (16.9%) | 38.9 | 55.6 | 38.9 | 50.0 | 22.2 | 33.3 | ||||||
| SAD (44.5%) | 39.2 | 55.6 | 35.3 | 50.8 | 15.7 | 33.3 | ||||||
| Anxiety disorder count | 2.06 | .15 | 2.52 | .11 | 1.88 | .17 | ||||||
| = 1 anxiety disorder (45.6%) | 36.2 | 58.8 | 31.9 | 52.9 | 19.1 | 38.2 | ||||||
| > 1 anxiety disorder (54.4%) | 44.9 | 49.2 | 42.0 | 42.9 | 20.3 | 22.2 | ||||||
| Illicit drug use | .24 | .62 | .35 | .56 | .85 | .36 | ||||||
| Yes (56.7%) | 45.2 | 55.3 | 40.3 | 47.4 | 22.6 | 28.9 | ||||||
| No (43.3%) | 36.5 | 52.8 | 34.6 | 49.1 | 17.3 | 34.0 | ||||||
| Major depression diagnosis | 1.88 | .17 | 1.99 | .16 | .22 | .64 | ||||||
| Yes (43.6%) | 47.1 | 50.0 | 41.2 | 41.1 | 19.6 | 26.8 | ||||||
| No (56.4%) | 36.9 | 57.3 | 35.4 | 53.3 | 20.0 | 33.3 | ||||||
| Gender | .98 | .32 | 1.20 | .27 | 2.26 | .13 | ||||||
| Male (60.2%) | 40.3 | 48.1 | 37.3 | 41.8 | 20.9 | 24.1 | ||||||
| Female (39.8%) | 42.9 | 63.5 | 38.8 | 57.7 | 18.4 | 40.4 | ||||||
| Antianxiety/depression medication | .82 | .37 | .001 | .98 | .60 | .44 | ||||||
| Yes (63.7%) | 43.4 | 60.2 | 40.8 | 51.1 | 25.0 | 34.1 | ||||||
| No (36.3%) | 37.5 | 41.9 | 32.5 | 41.9 | 10.0 | 23.3 | ||||||
| Clinical cutoff on State Anxiety | .04 | .84 | .03 | .86 | 2.93 | .09† | ||||||
| Above (72.3%) | 40.0 | 52.2 | 35.0 | 44.6 | 16.3 | 32.6 | ||||||
| Below (27.7%) | 45.5 | 60.5 | 45.5 | 57.9 | 30.3 | 26.3 | ||||||
| Clinical cutoff on Trait Anxiety | 1.66 | .20 | 2.02 | .16 | 4.31 | .04* | ||||||
| Above (88.7%) | 38.1 | 53.2 | 34.3 | 46.8 | 17.1 | 31.2 | ||||||
| Below (11.3%) | 77.8 | 65.0 | 77.8 | 60.0 | 55.6 | 30.0 | ||||||
Note. CBT = cognitive behavioral therapy; BDAC = Breaking the Drinking and Anxiety Connection; PMRT = Progressive Muscle Relaxation Training; GAD = generalized anxiety disorder; PD = panic disorder; SAD = social anxiety disorder.
p < .10.
p < .05.
As shown in Table 3, only one of the seven potential moderators was associated with a significant interaction term. Specifically, clinical cutoff status (above or below) on baseline Trait Anxiety interacted significantly with group in predicting relapse to 3 consecutive days drinking (Wald χ2 = 4.31,p = .04, Cohen’s d = .27, OR = 6.39, [1.11, 36.80]). Although CBT-BDAC was associated with a superior outcome on this variable for those above the Trait Anxiety clinical cutoff (Wald χ2 = 5.60, p = .02, Cohen’s d = .33, OR = 2.19, [1.15, 4.20]), this was not the case for those below the Trait Anxiety clinical cutoff at baseline (Wald χ2 = 1.67, p = .20, Cohen’s d = .49, OR = .34, [.07, 1.74]). A similar pattern was detected for those who were above versus below the clinical cutoff on State Anxiety for the 3 consecutive days drinking outcome; however, this difference was a statistical trend but not significant (p < .10; see Table 3).
Effect of Treatment Group on Anxiety Outcome at the Posttreatment and 4-Month Assessments
Mean anxiety scores
Despite the randomization to group, Table 4 shows that the PMRT group was nearly significantly higher than the CBT-BDAC group on both baseline Trait Anxiety, F(1, 317) = 2.97, η2 = .01, p = .09, and baseline State Anxiety, F(1, 319) = 3.26, η2 = .01, p = .07. Table 4 also shows that both groups exhibited a large reduction on mean Trait and State Anxiety from baseline to posttreatment; a 15.17-point reduction in the CBT-BDAC group (SD = 11.68) and a 13.20-point reduction in the PMRT group (SD = 9.72) for Trait Anxiety and a 12.57-point reduction in the CBT-BDAC group (SD = 14.16) and a 12.32-point reduction for the PMRT group (SD = 12.63) for State Anxiety. We also found that both groups exhibited a large reduction of Trait and State Anxiety from baseline to the 4-month follow-up; a 16.62-point reduction in the CBT-BDAC group (SD = 14.62) and a 11.95-point reduction in the PMRT group (SD = 12.94) for Trait Anxiety and a 15.40-point reduction in the CBT-BDAC group (SD = 18.47) and an 11.26-point reduction for the PMRT group (SD = 14.45) for State Anxiety. However, even after controlling for the nearly significant baseline differences (above), group effects at posttreatment were not significant (see Table 4). As in the case of the posttreatment assessment, mean State Anxiety at the 4-month follow-up assessment was not different between the groups after controlling for baseline State Anxiety. However, there was a significant effect for Trait Anxiety at the 4-month follow-up after controlling for baseline Trait Anxiety, F(1, 234) = 4.79, η2 = .02, p = .03. As shown in Table 4, this effect indicates that mean Trait Anxiety was significantly lower in the CBT-BDAC group compared with the PMRT group at the 4-month follow-up assessment.
Comparison of clinical cutoff status
As shown in Table 4, we also found that a large proportion of individuals who were above the clinical cutoff threshold on State and/or Trait Anxiety at baseline were below these thresholds by the posttreatment and 4-month follow-up assessments. Also shown in Table 4, there were no group differences on clinical cutoff status on either State or Trait Anxiety at the posttreatment assessment. Additionally, there was no significant difference between the groups on clinical cutoff status on State Anxiety at 4-month follow-up. However, there was a significant difference on clinical cutoff status on Trait Anxiety at the 4-month follow-up, such that a greater proportion of individuals in the CBT-BDAC group were below clinical cutoff compared with the PMRT group (χ2 = 4.19, p = .04, Cohen’s d = .29, OR = 1.78, [1.03, 3.09]).
Integrating the Effects of Treatment Group on Anxiety Outcomes at the Posttreatment Assessment With Effects of Treatment Group on Alcohol Outcomes at the 4-Month Assessment
As noted in the introduction and Method sections, we planned to evaluate mediator effects of anxiety reduction at the posttreatment assessment on alcohol outcomes at the 4-month assessment. However, because there were not significant group differences on anxiety outcomes at the posttreatment assessment, mediation can be rejected without further tests (Baron & Kenny, 1986). (Also noted earlier, mediation tests based on 4-month anxiety outcomes were not considered appropriate due to temporal confounding between the mediator and outcomes.) With that said, we did investigate whether clinical cutoff status on State or Trait Anxiety at posttreatment exerted main effects on alcohol outcomes at the 4-month assessment. We found no significant main effects for State or Trait Anxiety cutoff status predicting relapse to any alcohol use, relapse to binge drinking, or relapse to 3 consecutive days of drinking. Additionally, we found no instances of State or Trait Anxiety cutoff status at posttreatment interacting significantly with group assignment in predicting any of the categorical alcohol outcomes at the 4-month assessment.
Discussion
The central finding of this randomized controlled trial is that augmenting AUD treatment with the CBT-BDAC resulted in significantly better alcohol outcomes for patients with co-occurring anxiety disorders than did augmenting AUD treatment with PMRT. We also found that both groups experienced a substantial but fairly equivalent degree of anxiety reduction from baseline to posttreatment (about 1-SD unit). These findings, along with other data discussed below, suggest that anxiety reduction did not account for the group differences in the alcohol outcomes that we observed. This, in turn, implicates the CBT-BDAC treatment elements focused on the decoupling of anxiety and drinking phenomena as the cause of the group difference on alcohol outcomes. However, these group comparisons do not clarify whether anxiety reduction played a role in the overall alcohol outcomes observed for the entire sample. In fact, the recent meta-analysis reported by Hobbs et al. (2011) identified a small but significant pooled effect (d = .22) for anxiety treatment (vs. control) in improving the alcohol outcomes of AUD treatment patients with a co-occurring anxiety disorder. These results suggest that the alcohol outcomes of both study groups may have benefited from anxiety reduction, with the CBT-BDAC group experiencing additional benefit from its focus on weakening the link between anxiety and alcohol phenomena. In this scenario, it is possible that treatment elements unique to the CBT-BDAC were additive to or interactive with the anxiety reduction shared by both groups. Alternatively, more anxiety reduction might obviate the need for decoupling anxiety from alcohol use, and vice versa, in terms of improving AUD treatment outcomes in those with co-occurring anxiety disorders.
To address these and related issues, it would have been useful to have had a third group randomized to receive the AUD TAU in the absence of either study treatment. For example, because significant anxiety reduction from AUD treatment alone is well documented (e.g., S. A. Brown, Irwin, & Schuckit, 1991), a reference group undergoing AUD TAU alone would reveal how much anxiety reduction was specifically due to the study interventions. Although the absence of a randomized AUD TAU control group is a significant limitation of this study, we can consider relevant quasi-experimental contrasts of the two randomized groups with a nonrandomized cohort of 100 AUD TAU-only patients (n = 115 before attrition) that we collected in the same patient population using selection criteria and assessments that paralleled those used in this randomized study. In this nonrandomized cohort, only 26% were below the clinical threshold cutoff on State Anxiety at a time point paralleling the posttreatment assessment in the study. This can be compared with the 54% in the CBT-BDAC group and the 56% in the PMRT group who were below the clinical threshold cutoff on State Anxiety at the posttreatment assessment (CBT-BDAC vs. AUD TAU only, Cohen’s d = .57, OR = 3.43, 95% CI [1.64, 7.16]; and, PMRT vs. AUD TAU only, Cohen’s d = .59, OR = 3.71, [1.80, 7.63]). Additionally, about 61% of the nonrandomized AUD TAU cohort had relapsed to drinking in the 4 months following treatment. By comparison, 54% in the PMRT group and 41% in the CBT-BDAC group returned to drinking over the same period of time. These differences translate to a significant medium effect size between the CBT-BDAC group and the AUD TAU-only cohort in rate of relapse to drinking (i.e., Cohen’s d = .39, OR = 2.31, 95% CI [1.28, 4.18]) and a nonsignificant small effect size between the PMRT group and AUD TAU-only cohort in rate of relapse to drinking (Cohen’s d = .14, OR = 1.38, 95% CI [.78, 2.46]).
Several aspects of these post hoc quasi-experimental contrasts are potentially informative concerning the influence of the two study treatments on anxiety and alcohol outcomes. First, the effect size of about .5 for anxiety reduction in both study groups relative to that resulting from AUD TAU is in line with the meta-analytic pooled effect size of standard anxiety treatment versus control on anxiety outcomes in AUD treatment patients with co-occurring anxiety disorder (i.e., d = .52) (Hobbs et al., 2011). This similarity in effect sizes suggests that the impact of both study treatments on anxiety was comparable to that of standard anxiety treatments when deployed in this population. Second, although both study groups demonstrated better anxiety outcomes than the AUD TAU cohort, only the CBT-BDAC group demonstrated better alcohol outcomes than the AUD TAU cohort. Taken together, these contrasts support the conclusion that anxiety reduction, although better in both study groups than would be expected from AUD TAU alone, did not contribute to improved alcohol outcomes in the study groups.
This conclusion is also consistent with moderator tests showing that anxiety status (above vs. below clinical threshold) at the posttreatment assessment did not predict 4-month alcohol outcomes either as a main effect or in interaction with the study group. In other words, those whose anxiety resolved to subclinical levels over the course of treatment in either group fared no better in terms of their alcohol outcomes than did those whose anxiety remained above clinical levels following treatment. However, the validity of these extended conclusions are limited by (a) the nonexperimental contrasts on which they were based; (b) the possibility that the degree of anxiety reduction provided by the study treatments, although greater than AUD TAU, was insufficient to exert an effect on alcohol outcomes; and (c) the possibility that our anxiety measurement approach (either the timing or method of assessment) served to obscure the effects of anxiety treatment on alcohol outcomes.
For example, it is possible that different findings and conclusions would have resulted if Diagnositc and Statistical Manual of Mental Disorders (DSM) diagnoses rather than State and Trait Anxiety had been used as the primary anxiety outcome. As noted earlier, we concluded that the posttreatment assessment—the key assessment point for testing anxiety effects as mediating later alcohol outcomes—did not allow an adequate time frame for validly assessing change in anxiety diagnostic status following the conclusion of the treatment. Importantly, our conclusion that the assessment time frame at posttreatment was too brief to make reasonable diagnostic judgments (an assessment time frame of at least 30 days is typically required to determine DSM anxiety disorder diagnoses) is not to say that our brief treatment did not affect the patients’ diagnostic status. In fact, a number of studies have shown that CBT treatments with as few as two to four sessions can reduce anxiety symptoms to below diagnostic thresholds for a large percentage of patients (cf. Otto et al., 2012). With that said, the absence of an assessment of posttreatment diagnostic status is a clear limitation of the study. For example, because the inclusion criteria centered on the presence of an anxiety disorder, measuring anxiety outcomes in terms of State and Trait Anxiety may not have provided the same information as diagnostic status; however, see discussion just below.
We can address the impact of this limitation in our study to some extent because diagnostic information from the SCID interview was available for a nonrandom subsample of study participants at the 4-month assessment (n = 189). About 50% of these cases did not meet diagnostic criteria for any of the anxiety disorders assessed at baseline, and about 70% no longer met diagnostic criteria for their principal anxiety diagnosis that qualified them for participation in the study. These rates can be compared with the 46% and 62% of cases that were below the clinical threshold cutoffs on Trait and State Anxiety (respectively) at the 4-month assessment after having been above these thresholds at baseline. Notably, this shows that at the 4-month assessment, there was a closer alignment of subclinical Trait Anxiety with the absence of any study qualifying DSM anxiety diagnoses (46% and 50%, respectively) and a closer alignment of subclinical State Anxiety with the absence of the principal study anxiety diagnosis (62% and 70%, respectively). These findings suggest that our method for establishing anxiety “caseness” using the State and Trait Anxiety clinical threshold was probably reasonably congruent with anxiety disorder diagnostic status.
In addition to how we established “caseness” at outcome, there are also potentially important issues regarding our decision to include cases with any of several common anxiety disorders versus restricting recruitment to a single target anxiety disorder. Suggesting that the “type” of anxiety disorder the patient had did not affect their response to the study treatment, we found that the principal (qualifying) anxiety disorder was not associated with alcohol outcomes, either alone or in interaction with treatment group (see Table 3). However, moderator tests also showed that the small number of cases that did not exceed the clinical threshold cutoff on Trait Anxiety at baseline (about 10%) experienced less benefit from the CBT-BDAC than other patients in terms of alcohol outcomes, although this interaction was significant for the “three consecutive days of drinking” outcome only. These cases are especially curious because they all necessarily met diagnostic criteria for an anxiety disorder for the purpose of inclusion. Although it is possible that these cases represent diagnostic errors made at the screening for inclusion, there is no necessary reason why a mismatch between two methods of identifying “caseness” indicates an error in one or the other. Although DSM diagnoses are considered the “gold standard” of “caseness” in many contexts (e.g., psychiatric epidemiological studies), this standard plus high Trait Anxiety may mark those cases that would benefit the most from supplementing AUD treatment with the CBT-BDAC. Moreover, AUD patients with elevated Trait Anxiety could benefit significantly from the CBT-BDAC even when they do not meet diagnostic criteria for any anxiety disorder. This conjecture is consistent with studies showing that level of general internalizing psychopathology is more predictive of alcohol dependence than is the presence of any specific anxiety disorder (Kushner et al., 2012) and that high levels of Trait Anxiety are associated with poor AUD treatment outcomes (e.g., Driessen et al., 2001).
Several other methodological features of this study should be considered as potential limitations. The clinical consensus strategy used in the diagnostic assessments offers different strengths and weaknesses relative to the alternative approach of using multiple interviewers who come to independent diagnostic conclusions. Although the latter approach provides the context for establishing formal interrater reliability indices to quantify the diagnostic agreement among multiple interviewers (e.g., kappa), the clinical consensus model used in this study seeks reliability of clinical decisions by involving the same key clinical staff in each diagnostic decision. However, because our interviews were not recorded for the purpose of demonstrating reliability, this remains an empirically open question. Mitigating concerns that this limitation affected the validity of the study results is the fact that randomization occurred after the diagnostic assessment. Therefore, any diagnostic errors should have been evenly distributed between our two treatment groups. Furthermore, because diagnostic status was not an outcome, the impact of any diagnostic discrepancies would be contained to inclusion in the study but not group differences found in the study. Finally, diagnostic errors, even if they occurred, would not be likely to violate the study’s broad aim of including those suffering with significant anxiety problems.
Another potential methodological concern stems from the loss of potential participants during recruitment phase. Nearly two thirds of the individuals seeking AUD treatment during the recruitment phase chose not to return the initial screening questionnaire (Screen Level 1, Figure 1). We cannot know whether this loss of potential participants was random with respect to important study parameters. We speculate that many individuals who did not experience strong anxiety may have concluded from the stated focus of the study (AUD with anxiety disorder) that it did not pertain to them. In any case, given that this loss occurred prior to randomization, it should not have affected the groups differentially; but it still could affect the generalizability of the findings.
There was also a greater loss of CBT-BDAC group members than PMRT group members over the course of the treatment (see Figure 1). This may have reflected the greater cognitive and behavioral demands of the CBT-BDAC therapy compared with the relatively passive PMRT therapy. The difference in effort demanded by the two therapies may have been particularly relevant because the study’s voluntary therapy sessions occurred after the end of a full day of mandatory programming in the AUD treatment. With that said, the actual reasons given by participants for dropout were similar between the groups (see Figure 1). It was also noted that more males than females failed to provide 4-month follow-up data in the CBT-BDAC group, whereas loss to follow-up did not differ by gender in the PMRT group. Given the absence of other reasonable explanations for this unexpected result, it may simply be a Type I error due to chance. With that said, gender should not be overlooked in future work as a potentially important moderator of treatment-related parameters.
It is important to note that although a substantial proportion of individuals in both groups remained completely abstinent by the 4-month follow-up, there was still many individuals in both groups drinking hazardously (e.g., binge drinking) by this point. Moreover, the alcohol outcomes in both study groups, in spite of the addition of the study treatments, experienced worse alcohol outcomes 4 months following treatment than would be expected among AUD treatment patients without any co-occurring anxiety disorders (e.g., Kushner et al., 2005). Therefore, although the CBT-BDAC program succeeded in improving alcohol outcomes relative to PMRT in AUD patients with a co-occurring anxiety disorder, it remains critical for additional research to identify even more effective treatments for this difficult-to-treat population.
Finally, although we focused in this study on psychosocial processes, there is a burgeoning literature linking basic neurobiological stress and affect response systems, such as the limbichypothalamic-pituitary-adrenal axis (e.g., Schepis, Rao, Yadav, & Adinoff, 2011) and the extended amygdala (e.g., Koob & Le Moal, 2008), to the development of and treatment for AUDs (Simpson et al., 2009; Sinha et al., 2011). We envision that advances in our knowledge of treatment and prevention strategies for AUDs among those with anxiety disorders will be furthered by approaches that integrate both psychological and emerging neurobiological perspectives (e.g., Kushner, Maurer, Menary, & Thuras, 2011; Kushner, Menary, Maurer, & Thuras, 2012).
Acknowledgments
This work was supported by National Institute on Alcohol Abuse and Alcoholism Grants R01-AA015069 and K02-AA0017886 awarded to Matt G. Kushner.
The authors wish to acknowledge and thank Jeffrey Powers and his staff at the Fairview-Riverside Lodging Plus Chemical Dependency program for their support of this and our other work over the past 15 years. We also wish to acknowledge and thank Allie Schumacher, who served as the data manager for this project.
References
- Agresti A. Categorical data analysis. 2nd ed. New York, NY: Wiley; 2002. [Google Scholar]
- Andrews G, Slade T, Issakidis C. Deconstructing current comorbidity: Data from the Australian National Survey of Mental Health and Well-Being. The British Journal of Psychiatry. 2002;181:306–314. doi: 10.1192/bjp.181.4.306. [DOI] [PubMed] [Google Scholar]
- Antony MM, Orsillo SM, Roemer L, editors. Practitioner’s guide to empirically based measures of anxiety. New York, NY: Kluwer Academic/Plenum Publishers; 2001. [Google Scholar]
- Barlow DH, editor. Clinical handbook of psychological disorders. 3rd ed. New York, NY: Guilford Press; 2001. [Google Scholar]
- Barlow DH, Craske MG, Cerny JA, Klosko JS. Behavioral treatment of panic disorder. Behavior Therapy. 1989;20:261–282. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beck AT, Emery G, Greenberg RL. Anxiety disorders and phobias: A cognitive perspective. New York, NY: Basic Books; 2005. [Google Scholar]
- Beck AT, Wright FD, Newman CF, Liese BS. Cognitive therapy of substance abuse. New York, NY: Guilford Press; 1993. [PubMed] [Google Scholar]
- Bernstein DA, Borkovec TD. Progressive relaxation training: A manual for the helping professions. Champaign, IL: Research Press; 1973. [Google Scholar]
- Book SW, Thomas SE, Randall PK, Randall CL. Paroxetine reduces social anxiety in individuals with a co-occurring alcohol use disorder. Journal of Anxiety Disorders. 2008;22:310–318. doi: 10.1016/j.janxdis.2007.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen RC, D’Arcy C, Keegan D, Senthilselvan A. A controlled trial of cognitive behavioral treatment of panic in alcoholic inpatients with comorbid panic disorder. Addictive Behaviors. 2000;25:593–597. doi: 10.1016/s0306-4603(99)00017-9. [DOI] [PubMed] [Google Scholar]
- Boyd JH, Burke JD, Gruenberg E, Holtzer CE, III, Rae DS, George LK, Nestadt G. Exclusion criteria of DSM-III: A study of co-occurrence of hierarchy-free syndromes. Archives of General Psychiatry. 1984;41:983–989. doi: 10.1001/archpsyc.1984.01790210065008. [DOI] [PubMed] [Google Scholar]
- Brown SA, Irwin M, Schuckit MA. Changes in anxiety among abstinent male alcoholics. Journal of Studies on Alcohol. 1991;52:55–61. doi: 10.15288/jsa.1991.52.55. [DOI] [PubMed] [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of Abnormal Psychology. 2001;110:585–599. doi: 10.1037//0021-843x.110.4.585. [DOI] [PubMed] [Google Scholar]
- Conrad A, Roth WT. Muscle relaxation therapy for anxiety disorders: It works but how? Journal of Anxiety Disorders. 2007;21:243–264. doi: 10.1016/j.janxdis.2006.08.001. [DOI] [PubMed] [Google Scholar]
- Cooney NL, Litt MD, Morse PM, Bauer LO, Gaupp L. Alcohol cue reactivity, negative mood reactivity, and relapse in treated alcoholics. Journal of Abnormal Psychology. 1997;106:243–250. doi: 10.1037//0021-843x.106.2.243. [DOI] [PubMed] [Google Scholar]
- Darkes J, Goldman MS. Expectancy challenge and drinking reduction: Process and structure in the alcohol expectancy network. Experimental and Clinical Psychopharmacology. 1998;6:64–76. doi: 10.1037//1064-1297.6.1.64. [DOI] [PubMed] [Google Scholar]
- Driessen M, Meier S, Hill A, Wetterling T, Lange W, Junghanns K. The course of anxiety, depression and drinking behaviours after completed detoxification in alcoholics with and without comorbid anxiety and depressive disorders. Alcohol and Alcoholism. 2001;36:249–255. doi: 10.1093/alcalc/36.3.249. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer R, Gibbon M, Williams J. Structural Clinical Interview for Axis-I DSM-IV Disorders Patient edition (SCID-I/P Version 2.0) New York, NY: Biometrics Research Department, New York State Psychiatric Institution; 1989. [Google Scholar]
- Foa EB, Kozak MJ. Emotional processing of fear: Exposure to corrective information. Psychological Bulletin. 1986;99:20–35. [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Dufour MC, Compton W, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Archives of General Psychiatry. 2004;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Hobbs JDJ, Kushner MG, Lee SS, Reardon SM, Maurer EW. Meta-analysis of supplemental treatment for depressive and anxiety disorders in patients being treated for alcohol dependence. The American Journal on Addictions. 2011;20:319–329. doi: 10.1111/j.1521-0391.2011.00140.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson E. Progressive relaxation. 2nd ed. Oxford, England: University of Chicago Press; 1938. [Google Scholar]
- Jorm AF, Christensen H, Griffiths KM, Parslow RA, Rodgers B, Blewitt KA. Effectiveness of complementary and self-help treatments for anxiety disorders. Medical Journal of Australia. 2004;181:29–46. doi: 10.5694/j.1326-5377.2004.tb06352.x. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry. 1997;54:313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- Koob GF, Le Moal M. Addiction and the brain antireward system. Annual Review of Psychology. 2008;59:29–53. doi: 10.1146/annurev.psych.59.103006.093548. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, Borchardt C. The relationship between anxiety disorders and alcohol use disorders: A review of major perspectives and findings. Clinical Psychology Review. 2000;20:149–171. doi: 10.1016/s0272-7358(99)00027-6. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Abrams K, Thuras P, Hanson KL. Individual differences predictive of drinking to manage anxiety among non-problem drinkers with panic disorder. Alcoholism: Clinical and Experimental Research. 2000;24:448–458. [PubMed] [Google Scholar]
- Kushner MG, Abrams K, Thuras P, Hanson KL, Brekke M, Sletten S. Follow-up study of anxiety disorder and alcohol dependence in comorbid alcoholism treatment patients. Alcoholism: Clinical and Experimental Research. 2005;29:1432–1443. doi: 10.1097/01.alc.0000175072.17623.f8. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Donahue C, Sletten S, Thuras P, Abrams K, Peterson J, Frye B. Cognitive behavioral treatment of comorbid anxiety disorder in alcoholism treatment patients: Presentation of a prototype program and future directions. Journal of Mental Health. 2006;15:697–707. [Google Scholar]
- Kushner MG, Krueger R, Frye B, Peterson J. Epidemiological perspectives on co-occurring anxiety disorder and substance use disorder. In: Stewart S, Conrod P, editors. Anxiety and substance use disorders co-morbidity. New York, NY: Springer Publishing; 2008. pp. 290–312. [Google Scholar]
- Kushner MG, Maurer EW, Menary K, Thuras P. Vulnerability to the rapid (“telescoped”) development of alcohol dependence in individuals with anxiety disorder. Journal of Studies on Alcohol and Drugs. 2011;72:1019–1027. doi: 10.15288/jsad.2011.72.1019. PMID: 22051216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner MG, Menary KR, Maurer EW, Thuras P. Greater elevation in risk for nicotine dependence per pack of cigarettes smoked among those with anxiety disorder. Journal of Studies on Alcohol and Drugs. 2012;73:920–924. doi: 10.15288/jsad.2012.73.920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Beitman BD. The relation between alcohol problems and the anxiety disorders. American Journal of Psychiatry. 1990;147:685–695. doi: 10.1176/ajp.147.6.685. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Erickson DJ. Prospective analysis of the relation between DSM-III anxiety disorders and alcohol use disorders. American Journal of Psychiatry. 1999;156:723–732. doi: 10.1176/ajp.156.5.723. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sher KJ, Wood MD, Wood PK. Anxiety and drinking behavior: Moderating effects of tension-reduction alcohol outcome expectancies. Alcoholism: Clinical and Experimental Research. 1994;18:852–860. doi: 10.1111/j.1530-0277.1994.tb00050.x. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Sletten S, Donahue C, Thuras P, Maurer EW, Schneider A, Van Demark J. Cognitive-behavioral therapy for panic disorder in patients being treated for alcohol dependence: Moderating effects of alcohol outcome expectancies. Addictive Behaviors. 2009;34:554–560. doi: 10.1016/j.addbeh.2009.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kushner MG, Wall MM, Krueger RF, Sher KJ, Maurer E, Thuras P, Lee S. Alcohol dependence is related to overall internalizing psychopathology load rather than to particular internalizing disorders: Evidence from a national sample. Alcoholism: Clinical and Experimental Research. 2012;36:325–331. doi: 10.1111/j.1530-0277.2011.01604.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonhard C, Mulvey K, Gastfriend D, Schwartz M. The Addiction Severity Index: A field study of internal consistency and validity. Journal of Substance Abuse Treatment. 2000;18:129–135. doi: 10.1016/s0740-5472(99)00025-2. [DOI] [PubMed] [Google Scholar]
- Litt MD, Cooney NL, Kadden RM, Gaupp L. Reactivity to alcohol cues and induced moods in alcoholics. Addictive Behaviors. 1990;15:137–146. doi: 10.1016/0306-4603(90)90017-r. [DOI] [PubMed] [Google Scholar]
- Magee WJ, Eaton WW, Wittchen HU, McGonagle KA, Kessler RC. Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Archives of General Psychiatry. 1996;53:159–168. doi: 10.1001/archpsyc.1996.01830020077009. [DOI] [PubMed] [Google Scholar]
- Mäkelä K. Studies of the reliability and validity of the Addiction Severity Index. Society for the Study of Addiction. 2004;99:398–410. doi: 10.1111/j.1360-0443.2003.00665.x. [DOI] [PubMed] [Google Scholar]
- Manzoni GM, Pagnini F, Castelnuovo G, Molinari E. Relaxation training for anxiety: A ten-years systematic review with meta-analysis. BMC Psychiatry. 2008:8. doi: 10.1186/1471-244X-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLellan T, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Argeriou M. The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Menary KR, Kushner MG, Maurer EW, Thuras P. The prevalence and clinical implications of self-medication among individuals with anxiety disorders. Journal of Anxiety Disorders. 2011;25:335–339. doi: 10.1016/j.janxdis.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oei TPS, Evans L, Crook GM. Utility and validity of the STAI with anxiety disorder patients. British Journal of Clinical Psychology. 1990;29:429–432. doi: 10.1111/j.2044-8260.1990.tb00906.x. [DOI] [PubMed] [Google Scholar]
- Otto MW, Tolin DF, Nations KR, Utschig AC, Rothbaum BO, Hofmann SG, Smits JAJ. Five sessions and counting: Considering ultra-brief treatments for panic disorder. Depression and Anxiety. 2012;29:465–470. doi: 10.1002/da.21910. [DOI] [PubMed] [Google Scholar]
- Poulos CX, Hinson RE, Siegel S. The role of Pavlovian processes in drug tolerance and dependence: Implication for treatment. Addictive Behaviors. 1981;6:205–211. doi: 10.1016/0306-4603(81)90018-6. [DOI] [PubMed] [Google Scholar]
- Randall CL, Thomas S, Thevos AK. Concurrent alcoholism and social anxiety disorder: A first step toward developing effective treatments. Alcoholism: Clinical and Experimental Research. 2001;25:210–220. [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse: Results from the Epidemiologic Catchment Area (ECA) Study. Journal of the American Medical Association. 1990;264:2511–2518. [PubMed] [Google Scholar]
- Rosen C, Henson B, Finney J, Moos R. Consistency of self-administered and interview-based Addiction Severity Index composite scores. Addiction. 2000;95:419–425. doi: 10.1046/j.1360-0443.2000.95341912.x. [DOI] [PubMed] [Google Scholar]
- Schadé A, Marquenie LA, Van Balkom AJLM, Koeter MW, DeBeurs E, Van den Brink W, Van Dyck R. Alcohol-dependent patients with comorbid phobic disorders: A comparison between comorbid patients, pure alcohol-dependent and pure phobic patients. Alcohol. 2004;39:241–246. doi: 10.1093/alcalc/agh039. [DOI] [PubMed] [Google Scholar]
- Schepis T, Rao U, Yadav H, Adinoff B. The limbic-hypothalamic-pituitary-adrenal axis and the development of alcohol use disorders in youth. Alcoholism: Clinical and Experimental Research. 2011;35:595–605. doi: 10.1111/j.1530-0277.2010.01380.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Segal DL, Hersen M, Van Hasselt VB. Reliability of the Structured Clinical Interview for DSM–III–R: An evaluative review. Comprehensive Psychiatry. 1994;35:316–327. doi: 10.1016/0010-440x(94)90025-6. [DOI] [PubMed] [Google Scholar]
- Siev J, Chambless DL. Specificity of treatment effects: Cognitive therapy and relaxation for generalized anxiety and panic disorders. Journal of Consulting and Clinical Psychology. 2007;75:513–522. doi: 10.1037/0022-006X.75.4.513. [DOI] [PubMed] [Google Scholar]
- Simpson TL, Saxon AJ, Meredith CW, Malte CA, McBride B, Ferguson LC, Raskind M. A pilot trial of the alpha-1 adrenergic antagonist, prazosin, for alcohol dependence. Alcoholism: Clinical and Experimental Research. 2009;33:255–263. doi: 10.1111/j.1530-0277.2008.00807.x. [DOI] [PubMed] [Google Scholar]
- Sinha R. Modeling stress and drug craving in the laboratory: Implications for addiction treatment development. Addiction Biology. 2009;14:84–98. doi: 10.1111/j.1369-1600.2008.00134.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha R, Fox HC, Hong KA, Siedlarz KA, Bergquist KT, Kreek MJ. Effects of adrenal sensitivity, stress and cue-induced craving and anxiety on subsequent alcohol relapse and treatment outcomes. Archives of General Psychiatry. 2011;68:942–952. doi: 10.1001/archgenpsychiatry.2011.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol time-line follow-back user’s manual. Toronto, Canada: Addiction Research Foundation; 1995. [Google Scholar]
- Spielberger CD, Sydeman SJ. State-Trait Anxiety Inventory and State-Trait Anger Expression Inventory. In: Maruish ME, editor. The use of psychological testing for treatment planning and outcome assessment. Hillsdale, NJ: Lawrence Erlbaum Associates; 1994. pp. 292–321. [Google Scholar]
- Summerfeldt LJ, Antony MM. Structured and semistructured diagnostic interviews. In: Antony MM, Barlow DH, editors. Handbook of assessment and treatment planning for psychological disorders. New York, NY: Guilford Press; 2004. pp. 3–37. [Google Scholar]
- Thomas SE, Randall PK, Book SW, Randall CL. A complex relationship between co-occurring social anxiety and alcohol use disorders: What effect does treating social anxiety have on drinking? Alcoholism: Clinical and Experimental Research. 2008;32:77–84. doi: 10.1111/j.1530-0277.2007.00546.x. [DOI] [PubMed] [Google Scholar]