Abstract
Background: Several large population-based studies have demonstrated associations between adverse childhood experiences and later development of psychotic symptoms. However, little attention has been paid to the mechanisms involved in this pathway and the few existing studies have relied on cross-sectional assessments. Methods: Prospective data on 6692 children from the UK Avon Longitudinal Study of Parents and Children (ALSPAC) were used to address this issue. Mothers reported on children’s exposure to harsh parenting and domestic violence in early childhood, and children self-reported on bullying victimization prior to 8.5 years. Presence of children’s anxiety at 10 years and their depressive symptoms at 9 and 11 years were ascertained from mothers, and children completed assessments of self-esteem and locus of control at 8.5 years. Children were interviewed regarding psychotic symptoms at a mean age of 12.9 years. Multiple mediation analysis was performed to examine direct and indirect effects of each childhood adversity on psychotic symptoms. Results: The association between harsh parenting and psychotic symptoms was fully mediated by anxiety, depressive symptoms, external locus of control, and low self-esteem. Bullying victimization and exposure to domestic violence had their associations with psychotic symptoms partially mediated by anxiety, depression, locus of control, and self-esteem. Similar results were obtained following adjustment for a range of confounders and when analyses were conducted for boys and girls separately. Conclusions: These findings tentatively suggest that specific cognitive and affective difficulties in childhood could be targeted to minimize the likelihood of adolescents exposed to early trauma from developing psychotic symptoms.
Key words: etiology, bullying, longitudinal, psychosis, trauma
Introduction
An increasing body of research has demonstrated associations between adverse childhood experiences and psychotic disorders. 1 Because psychosis is considered to reflect a quantitative continuum from normality through attenuated psychotic symptoms to full clinical disorder, an underlying etiological continuum is also assumed to exist. 2 Indeed, childhood adversity has been linked to subclinical expressions of psychosis. 3–5 These findings suggest that investigating samples with early manifestations of psychotic symptoms may provide useful insights into psychotic disorders. However, little is known about the mechanisms underlying the adversity—psychosis association. Improved understanding of these pathways is imperative because it may enable suitable interventions to be targeted at high-risk children and potentially prevent the emergence of psychotic disorder.
Several pathways are possible. First, traumatic events in childhood could directly increase the risk of developing psychotic symptoms, perceptual aberrations, or reality impairment. 6 , 7 For instance, subclinical hallucinations or delusions could be considered to be traumatic reactions to severe adversity whose content is directly reminiscent of the adversity. 7 , 8 A range of other more indirect pathways have also been suggested. For instance, Garety et al. 9 hypothesized that exposure to trauma in childhood may result in the development of negative beliefs about the self as vulnerable to threat. These negative schematic beliefs may in turn lower self-esteem and produce a tendency to attribute experiences to external causes, potentially giving rise to referential ideas, paranoia, and misattributions of perceptual anomalies. 9 , 10 Indeed, both low self-esteem and an external locus of control (LoC) have been shown to increase the risk of psychotic symptoms in prospective studies. 11 , 12 Other forms of psychopathology resulting from early victimization may also form a pathway to later psychotic symptoms. Adverse childhood experiences have been shown to predict later depression and anxiety 13 , 14 and these symptoms in turn appear to precede psychosis. 15 , 16
Further exploration of the pathways between childhood adversity and psychosis is warranted to test these postulated mechanisms. The handful of studies that have explored this issue to date 17–20 have all used cross-sectional designs with reliance on retrospective assessments of childhood adversity and potential mediators, thus preventing temporal relationships from being accurately established. Therefore, we investigated cognitive and affective pathways between a range of early adverse childhood experiences and psychotic symptoms in a prospective longitudinal study, the Avon Longitudinal Study of Parents and Children (ALSPAC). It has previously been demonstrated in this sample that bullying by peers is associated with greater endorsement of psychotic symptoms at around 13 years of age 5 and other studies have also found that early exposure to harsh parenting 3 and domestic violence within the family home 21 are related to the experience of psychotic symptoms in early adolescence. We considered it important to look at these types of victimization separately because they involve different perpetrators (parental figures vs peers) or different degrees of exposure (direct vs witnessing) and thus may potentially have different developmental effects. 22 , 23 We examined these exposures in early childhood and hypothesized that low self-esteem, an external LoC, and higher levels of depression and anxiety in the intervening period would constitute indirect pathways between childhood victimization and psychotic symptoms.
Methods
Participants
The sample was drawn from the ALSPAC that recruited 14 541 pregnant women resident in the former Avon Health Authority in the southwest of England, with expected dates of delivery being April 1, 1991 to December 31, 1992. There were 186 twin pairs in this sample and the twin with the lowest birth weight was removed from the dataset because this factor has previously been shown to have associations with psychotic symptoms in this cohort. 24 This also avoided the potentially confounding effect of the non-independence of observations provided on twins. Ethical approval for the study was obtained from the ALSPAC Law and Ethics Committee and the Local Research Ethics Committees. Parents provided informed written consent and children assent after receiving a full explanation of the study.
Measures
Victimization.
Mothers reported via a series of postal questionnaires on a range of life events and victimization experiences that their children had been exposed to since birth. Specifically, when the child was aged 8, 21, 33, 47, 61, and 73 months mothers were asked whether the following had occurred since the last assessment (or since birth for the first assessment point): “Your husband/partner was physically cruel to you” and “Your husband/partner was emotionally cruel to you.” A positive response to either of these two questions at any of the time points was considered to be evidence of domestic violence (see Bowen et al. 25 for further details).
Maternal hitting was considered present if mothers responded with “daily” or “every week” to the following item: “When you are at home with your child how often do you slap him” when the child was aged 2 or 3.5 years. 26 Preschool hostility was classed as present if 3 or all of the following items were answered positively by mothers: “mum feels that whining makes her want to hit child” (1.8 years), “mum often irritated by child” (1.8 years), “mum has battle of wills with child” (1.8 years), and “child gets on mums nerves” (1.8 years). 26 School hostility (since the age of 5) was considered present if all of the following 3 items were answered positively by mothers: “mum often irritated by child” (7 years), “mum has battle of wills with child” (7 years), and “child gets on mum’s nerves” (7 years). 26 These items have previously been shown to load onto a distinct hostility factor. 26 A harsh parenting composite was constructed by summing maternal hitting, preschool and school hostility, and coded as: none, mild (1 indicator of harsh parenting), moderate (2 indicators of harsh parenting), or severe (3 indicators of harsh parenting). This composite has previously been demonstrated to be associated with borderline personality disorder symptoms in this sample. 27
Children were interviewed with the Bullying and Friendship Interview Schedule 28 when they were on average 8.5 years of age as part of a face-to-face assessment clinic (see Griffiths et al. 29 for a detailed description of its use in the ALSPAC sample). Trained psychology graduates asked the children 10 questions concerning overt and relational bullying by peers over the previous 6 months and the frequency of its occurrence. Children were classified as having been severely bullied if they reported exposure to both overt and relational victimization at least 4 times each during the past 6 months or at least once a week for each type during this time period, while those who had only experienced one of these forms of bullying at this level of frequency were considered to have been moderately bullied, and all the remaining children were classified as not having been bullied. Reasonable levels of agreement have been demonstrated between child self-reports of bullying and those provided by mothers and teachers. 5
Locus of Control.
Children completed a 12-item version of the Nowicki-Strickland Internal-External scale (NSIE) 30 during face-to-face assessments when they were on average 8.5 years of age. A total score was created by summing scores for all of the items, with a higher score indicating a more external LoC. Children who responded “don’t know” to a question were coded as having an unknown LoC score and thus excluded from analyses that included this variable (see Thompson et al. 12 for full details).
Self-esteem.
Children also completed a shortened form of Harter’s Self Perception Profile for Children 31 when they were on average 8.5 years old as part of the face-to-face assessment clinic. This version consisted of the 12 items from the global self-worth and scholastic competence subscales of the original measure. To avoid overlap between scholastic competence and intelligence quotient (IQ), only the global self-worth subscale was used in this analysis and this was calculated by summing the scores for the 6 relevant items, with lower scores indicating poorer self-esteem.
Affective Symptoms.
Parents completed the Develop ment and Well-being Assessment (DAWBA) 32 when children were aged 10 years old. This semi-structured interview comprises open and closed questions about a range of symptoms relevant to childhood psychiatric disorders. An ordered categorical measure of anxiety was generated using computer algorithms (see Goodman et al. 33 for further details). This comprised 6 categories indicating the likelihood of each child having an anxiety disorder from level 0 (<0.1% of children in this band have anxiety disorder) up to level 5 (>70% of children in this band have anxiety disorder). Goodman et al. 33 have validated this measure of anxiety in epidemiological samples of British and Norwegian children. There was 1 child who was reported to be experiencing post-traumatic symptoms and so this individual was removed from the analysis.
Additionally, mothers completed the Short Moods and Feelings Questionnaire (SMFQ) 34 when the child was aged 9 and 11 years to provide a broader picture of the depressive symptoms their child had experienced over the previous 2 weeks. The SMFQ comprises 13 questions rated on a 3-point scale: true (score of 2), sometimes true (score of 1), and not true (score of 0). The ratings for all of the items were summed to produce a total score out of 26. In accordance with the guidance set out by Angold et al., 34 the scores at each time point were dichotomized into no/minimal depression (scores of 0–7) and clinically relevant depressive symptoms (scores of 8 or more). For the current analysis a variable was constructed indicating the presence of clinically relevant depressive symptoms at either 9 or 11 years vs absence of such symptoms at both time points.
Psychotic Symptoms.
At a mean age of 12.9 years, children were administered a semi-structured psychosis interview (PLIKSi) 35 derived from the Diagnostic Interview Schedule for Children version IV (DISC-IV) 36 and the Schedules for Clinical Assessment in Neuropsychiatry version 2.0 (SCAN). 37 The PLIKSi comprises 12 core questions concerning the occurrence of hallucinations, delusions, and thought interference over the previous 6 months. Trained interviewers rated each symptom as absent, suspected, or definitely present, with the latter rating requiring a credible example to have been provided. The average kappa value was 0.72 indicating good inter-rater reliability for this measure. 35 In the current analysis only symptoms that were not attributable to the effects of sleep, fever, or substance misuse were included in accordance with previous studies using this sample. 38 Two PLIKSi outcomes were examined: presence or absence of (1) any suspected or definite psychotic symptoms (“broad” symptoms), and (2) definite symptoms only (“narrow” symptoms).
Confounders.
Parent-reported ethnicity (split into white and non-white due to small numbers in more specific ethnic groupings) and sex of the child were included as potential confounders as they have previously been shown to be differentially associated with both childhood adversity and psychosis. 4 , 39 , 40 Birth weight was obtained from birth records and lower birth weight has been found to predict greater likelihood of childhood maltreatment 41 and PLIKSi symptoms 24 in this sample. IQ was derived from the alternative item form of the Wechsler Intelligence Scale for Children 3rd UK edition (WISC-III) 42 administered to children at around 8.5 years of age. The total IQ score was dichotomized into below average (89 or less) and average or higher (90 or more) because children in this sample with below average IQ scores have previously been shown to be at the greatest risk of experiencing psychotic symptoms. 35 Family psychiatric history was reported by the child’s parents via postal questionnaires completed during pregnancy and up until the child was 11 years of age. A history of schizophrenia in the biological parents or grandparents of the child, depression (ie, severe symptoms, seen a doctor for depression or prescribed antidepressants) or suicide attempts in the parents was included as a potential confounder as this has also been reported to be associated with elevated rates of childhood trauma 3 and psychotic symptoms. 38 Finally, a Family Adversity Index (FAI) 25 was included to account for the impact of multiple family risk factors. This comprised 17 items drawn from questionnaires completed by the mothers during their pregnancy (8, 12, 18, and 32 weeks gestation), including young maternal age, inadequate housing, financial difficulties, maternal affective disorder, parental substance abuse, and involvement in crime. The presence of each adversity was rated as 1 and a total FAI score was produced by summing all 17 items.
Analysis
Basic associations between each form of victimization and broad or narrow PLIKSi symptoms were investigated using binary logistic regression. Multiple mediation analysis was then performed in Stata (v11.0) to examine the extent to which each of these associations was mediated by the affective (depression and anxiety) and cognitive (LoC and self-esteem) variables. A diagrammatic representation of the model tested is presented in figure 1. The potential mediators were demonstrated to be statistically distinct from each other (data not shown) and thus were used as separate constructs. The meditational variables were first entered altogether to examine their combined effect on the association between each type of victimization and PLIKSi symptoms and then second they were entered on their own in separate models to investigate their individual impact on this relationship. The binary_mediation command was employed that can be used with a combination of dichotomous and continuous variables and provides standardized coefficients. Confidence intervals were estimated using bootstrapping with 500 replications. All logit coefficients and confidence intervals were exponentiated into odds ratios to facilitate interpretation and comparison between models. The final pathway models were adjusted for the potential confounding effects of sex, ethnicity, birth weight, family history of schizophrenia, depression or suicide, the child’s IQ, and general family adversity. Analyses were repeated for boys and girls separately to determine if similar pathways were evident.
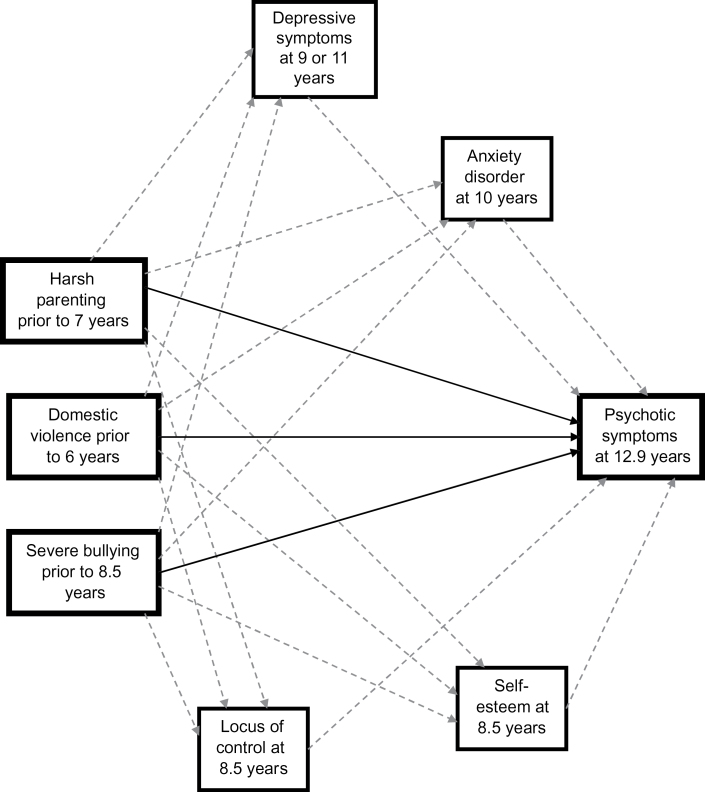
Fig. 1.
Conceptual path diagram of associations between victimization and psychotic symptoms. Hypothesized direct paths are indicated by solid arrows and indirect paths by dashed arrows.
Results
Data were available on 6692 children who completed the PLIKSi at an average age of 12.9 years (48% of the 14 062 live births in this cohort). Approximately half of this sample were female (50.9%) and few were of non-white ethnic origin (3.6%). Children who completed the PLIKSi were more likely to be female, of white ethnicity, born to married mothers, have been exposed to lower levels of family adversity and have a higher IQ than those who did not complete it (data not shown, but see Schreier et al. 5 for results on a slightly smaller subsample). Rates of all types of victimization were similar between PLIKSi completers and non-completers.
Of those with PLIKSi data, 11.3% reported probable or definite symptoms (“broad”) that were not due to sleep, fever, or substance use and 4.7% were considered to have definite symptoms (“narrow”), again not attributable to the aforementioned causes. Almost a quarter of PLIKSi completers had been exposed to domestic violence prior to 6 years of age (23.6%), 37.0% had experienced mildly, 9.9% moderately, and 4.2% severely harsh parenting prior to 7 years of age, while 10.1% of children reported having been severely bullied prior to 8.5 years of age. The strongest associations with psychotic symptoms were apparent for severe bullying victimization (broad: OR = 1.47, 95% CI 1.30–1.65; narrow: OR = 1.51, 95% CI 1.27–1.80) and exposure to domestic violence (broad: OR = 1.48, 95% CI 1.25–1.76; narrow: OR = 1.59, 95% CI 1.23–2.04), with the smallest effects for harsh parenting (broad: OR = 1.13, 95% CI 1.02–1.25; narrow: OR = 1.15, 95% CI 0.99–1.34).
Pathways to Psychotic Symptoms
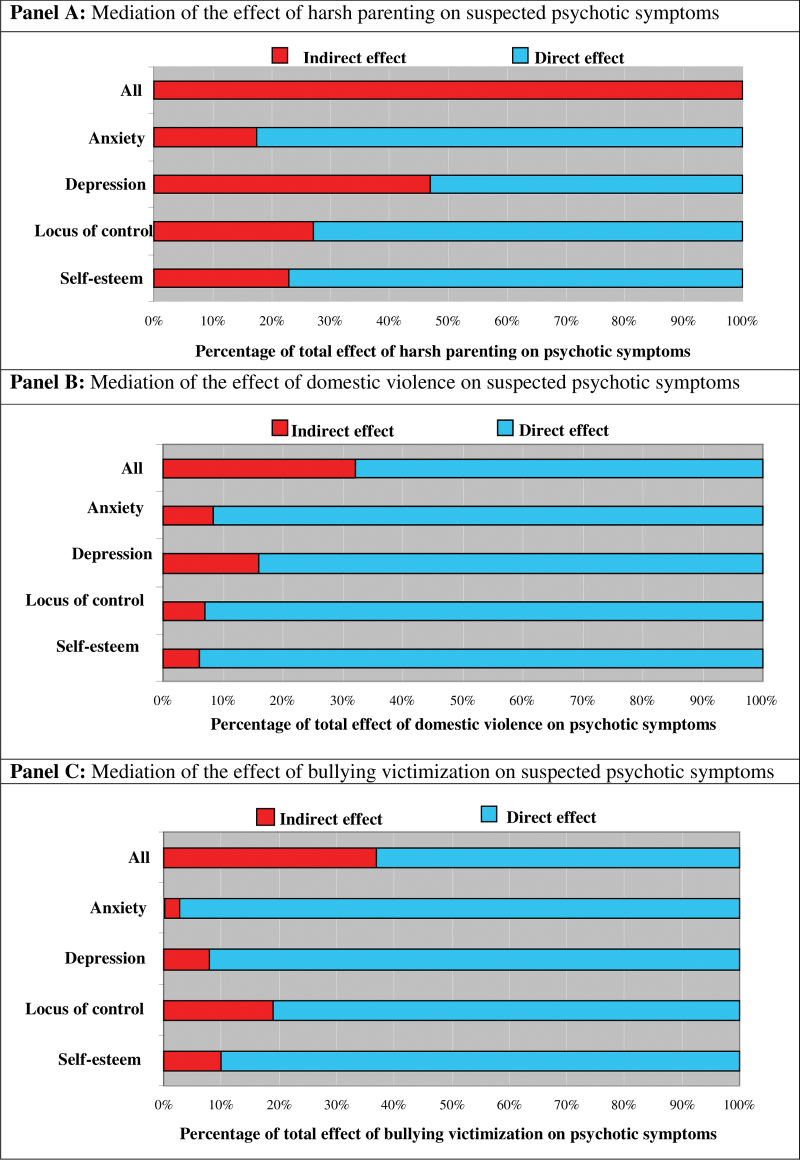
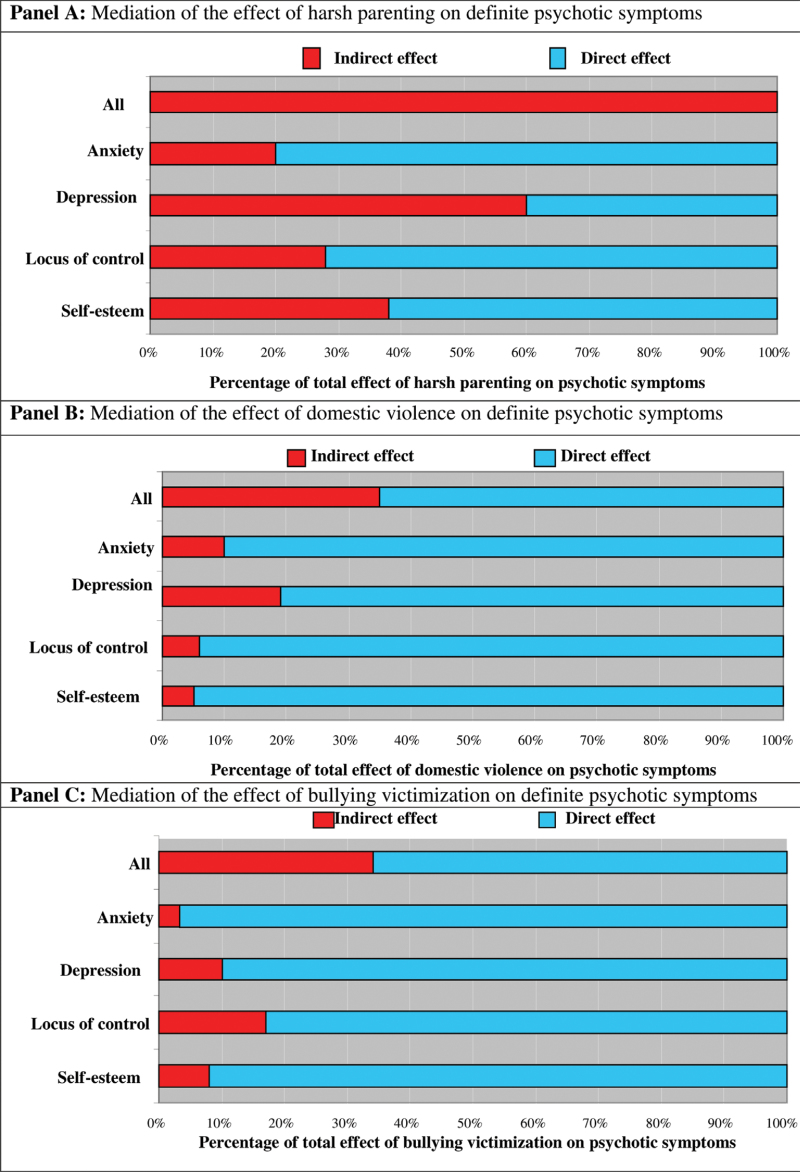
The direct and indirect pathways (via potential affective and cognitive mediators) between each form of victimization and broadly and narrowly defined PLIKSi symptoms are presented in tables 1 and 2, respectively. The odds ratio (OR) for each pathway is shown, along with 95% confidence intervals, both unadjusted and adjusted for sex, ethnicity, birth weight, family psychiatric history, child’s IQ, and general family adversity. The proportion of the total effect of each form of victimization on PLIKSi symptoms that is accounted for by all of the mediators together and individually is displayed in red in figures 2 and 3 (for broadly and narrowly defined symptoms, respectively).
Table 1.
Associations Between Different Forms of Victimization and Broadly Defined Psychotic Symptoms, Split Into Total Effects, Direct and Indirect Pathways Via All of the Potential Mediators Together and Then Via Each Individual Mediator on Its Own
| Type of Victimization and Potential Mediator | Unadjusted | Adjusted a | ||||||
|---|---|---|---|---|---|---|---|---|
| Total OR (95% CI) | Direct OR (95% CI) | Indirect OR (95% CI) | % Mediated | Total OR (95% CI) | Direct OR (95% CI) | Indirect OR (95% CI) | % Mediated | |
| Harsh parenting | n = 5143 | n = 4494 | ||||||
| All mediators | 1.05 (0.99–1.10) | 1.00 (0.95–1.06) | 1.05 (1.03–1.06) | 100 | 1.02 (0.95–1.08) | 0.98 0.92–1.04) | 1.04 (1.02–1.05) | 100 |
| Anxiety only | 1.05 (0.99–1.09) | 1.04 (0.99–1.09) | 1.01 (1.00–1.01) | 17 | 1.03 (0.98–1.08) | 1.02 (0.97–1.08) | 1.00 (1.00–1.01) | 16 |
| Depression only | 1.06 (1.01–1.11) | 1.03 (0.98–1.08) | 1.03 (1.01–1.04) | 47 | 1.04 (0.99–1.09) | 1.01 (0.96–1.07) | 1.03 (1.01–1.03) | 60 |
| LoC only | 1.06 (1.00–1.11) | 1.04 (0.99–1.09) | 1.02 (1.01–1.02) | 27 | 1.03 (0.98–1.09) | 1.02 (0.97–1.07) | 1.01 (1.01–1.02) | 36 |
| Self-esteem only | 1.05 (1.00–1.10) | 1.04 (0.99–1.09) | 1.01 (1.01–1.02) | 23 | 1.03 (0.98–1.08) | 1.02 (0.97–1.07) | 1.01 (1.00–1.02) | 33 |
| Domestic violence | n = 5781 | n=4904 | ||||||
| All mediators | 1.08 (1.02–1.13) | 1.05 (1.00–1.11) | 1.03 (1.01–1.04) | 32 | 1.04 (0.98–1.10) | 1.02 (0.96–1.08) | 1.02 (1.01–1.03) | 48 |
| Anxiety only | 1.10 (1.05–1.14) | 1.09 (1.04–1.13) | 1.01 (1.00–1.01) | 9 | 1.04 (0.99–1.10) | 1.04 (0.99–1.10) | 1.00 (1.00–1.01) | 9 |
| Depression only | 1.10 (1.06–1.14) | 1.08 (1.04–1.13) | 1.02 (1.01–1.02) | 16 | 1.03 (0.98–1.08) | 1.02 (0.97–1.07) | 1.01 (1.00–1.01) | 23 |
| LoC only | 1.08 (1.02–1.13) | 1.07 (1.02–1.12) | 1.01 (1.00–1.01) | 7 | 1.02 (0.97–1.08) | 1.02 (0.97–1.08) | 1.00 (1.00–1.01) | 2 |
| Self-esteem only | 1.09 (1.04–1.13) | 1.08 (1.04–1.13) | 1.01 (1.00–1.01) | 6 | 1.03 (0.98–1.09) | 1.03 (0.98–1.08) | 1.00 (1.00–1.01) | 9 |
| Bullying | n = 5136 | n = 4622 | ||||||
| All mediators | 1.14 (1.08–1.20) | 1.09 (1.03–1.14) | 1.05 (1.03–1.07) | 37 | 1.13 (1.06–1.19) | 1.09 (1.02–1.15) | 1.04 (1.02–1.06) | 31 |
| Anxiety only | 1.14 (1.09–1.19) | 1.14 (1.09–1.19) | 1.00 (1.00–1.01) | 3 | 1.13 (1.08–1.19) | 1.13 (1.08–1.19) | 1.00 (1.00–1.01) | 1 |
| Depression only | 1.15 (1.10–1.20) | 1.14 (1.09–1.19) | 1.01 (1.00–1.02) | 8 | 1.14 (1.09–1.19) | 1.13 (1.08–1.18) | 1.01 (1.00–1.02) | 7 |
| LoC only | 1.15 (1.10–1.20) | 1.12 (1.07–1.17) | 1.03 (1.02–1.04) | 19 | 1.14 (1.09–1.19) | 1.12 (1.06–1.17) | 1.02 (1.01–1.03) | 16 |
| Self-esteem only | 1.14 (1.10–1.20) | 1.13 (1.08–1.18) | 1.01 (1.01–1.02) | 10 | 1.14 (1.09–1.19) | 1.13 (1.07–1.18) | 1.01 (1.00–1.02) | 9 |
Note: CI, confidence interval; LoC, locus of control; OR, odds ratio.
aAdjusted for sex, ethnicity, birth weight, family psychiatric history, IQ, and general family adversity.
Table 2.
Associations Between Different Forms of Victimization and Narrowly Defined Psychotic Symptoms, Split Into Total Effects, Direct and Indirect Pathways Via All of the Potential Mediators Together and Then Via Each Individual Mediator on Its Own
| Type of Victimization and potential mediator | Unadjusted | Adjusted a | ||||||
|---|---|---|---|---|---|---|---|---|
| Total OR (95% CI) | Direct OR (95% CI) | Indirect OR (95% CI) | % Mediated | Total OR (95% CI) | Direct OR (95% CI) | Indirect OR (95% CI) | % Mediated | |
| Harsh parenting | n = 5150 | n = 4621 | ||||||
| All mediators | 1.03 (0.94–1.12) | 0.98 (0.89–1.06) | 1.06 (1.03–1.08) | 100 | 1.01 (0.93–1.09) | 0.97 (0.89–1.05) | 1.04(1.02–1.07) | 100 |
| Anxiety only | 1.05 (0.98–1.14) | 1.04 (0.97–1.22) | 1.01 (1.00–1.02) | 20 | 1.03 (0.93–1.11) | 1.02 (0.93–1.10) | 1.01 (1.00–1.01) | 21 |
| Depression only | 1.06 (0.99–1.13) | 1.03 (0.95–1.10) | 1.03 (1.02–1.06) | 60 | 1.03 (0.96–1.10) | 1.00 (0.93–1.08) | 1.03 (1.01–1.05) | 94 |
| LoC only | 1.05 (0.97–1.13) | 1.04 (0.96–1.12) | 1.01 (1.01–1.02) | 28 | 1.02 (0.94–1.10) | 1.01 (0.93–1.09) | 1.01 (1.00–1.02) | 47 |
| Self-esteem only | 1.04 (0.98–1.13) | 1.03 (0.98–1.13) | 1.01 (1.00–1.01) | 38 | 1.01 (0.94–1.08) | 1.00 (0.93–1.07) | 1.01 (1.01–1.02) | 97 |
| Domestic violence | n = 5780 | n = 4903 | ||||||
| All mediators | 1.08 (0.99–1.17) | 1.05 (0.97–1.13) | 1.03 (1.01–1.04) | 35 | 1.06 (0.97–1.14) | 1.03 (0.95–1.11) | 1.02 (1.01–1.04) | 42 |
| Anxiety only | 1.12 (1.04–1.19) | 1.10 (1.03–1.18) | 1.01 (1.00–1.02) | 10 | 1.06 (0.97–1.15) | 1.06 (0.97–1.14) | 1.00 (1.00–1.01) | 8 |
| Depression only | 1.11 (1.05–1.18) | 1.09 (1.03–1.16) | 1.02 (1.01–1.03) | 19 | 1.05 (0.96–1.13) | 1.04 (0.96–1.12) | 1.01 (1.00–1.02) | 18 |
| LoC only | 1.09 (1.02–1.17) | 1.08 (1.01–1.16) | 1.01 (1.00–1.01) | 6 | 1.03 (0.95–1.11) | 1.03 (0.95–1.11) | 1.00 (1.00–1.01) | 1 |
| Self-esteem only | 1.12 (1.05–1.19) | 1.11 (1.04–1.19) | 1.01 (1.00–1.01) | 5 | 1.04 (0.97–1.12) | 1.04 (0.97–1.12) | 1.00 (1.00–1.01) | 7 |
| Bullying | n = 5150 | n = 4621 | ||||||
| All mediators | 1.15 (1.06–1.24) | 1.10 (1.01–1.19) | 1.05 (1.03–1.07) | 34 | 1.14 (1.03–1.24) | 1.10 (1.00–1.19) | 1.04 (1.02–1.06) | 29 |
| Anxiety only | 1.15 (1.07–1.23) | 1.14 (1.06–1.22) | 1.00 (1.00–1.01) | 3 | 1.14 (1.04–1.22) | 1.14 (1.04–1.22) | 1.00 (1.00–1.01) | 2 |
| Depression only | 1.17 (1.08–1.24) | 1.15 (1.06–1.23) | 1.02 (1.01–1.02) | 10 | 1.15 (1.06–1.24) | 1.14 (1.05–1.22) | 1.01 (1.00–1.02) | 8 |
| LoC only | 1.17 (1.08–1.23) | 1.14 (1.05–1.20) | 1.03 (1.02–1.04) | 17 | 1.15 (1.06–1.24) | 1.13 (1.04–1.22) | 1.02 (1.01–1.03) | 13 |
| Self-esteem only | 1.16 (1.07–1.23) | 1.14 (1.06–1.22) | 1.02 (1.00–1.02) | 8 | 1.14 (1.05–1.22) | 1.13 (1.04–1.21) | 1.01 (1.00–1.02) | 10 |
aAdjusted for sex, ethnicity, birth weight, family psychiatric history, IQ, and general family adversity.
Fig. 2.
Proportion of the total effect of harsh parenting (Panel A), exposure to domestic violence (Panel B), and bullying victimization (Panel C) in childhood on broadly defined psychotic symptoms at 12.9 years of age mediated via affective and cognitive factors. The red portion of each bar indicates the percentage of the effect mediated (indirect effect), initially by all of the factors together and then separately for anxiety disorder, depressive symptoms, external locus of control, and low self-esteem.
Fig. 3.
Proportion of the total effect of harsh parenting (Panel A), exposure to domestic violence (Panel B), and bullying victimization (Panel C) in childhood on narrowly defined psychotic symptoms at 12.9 years of age mediated via affective and cognitive factors. The red portion of each bar indicates the percentage of the effect mediated (indirect effect), initially by all of the factors together and then separately for anxiety disorder, depressive symptoms, external locus of control, and low self-esteem.
The relatively modest association between harsh parenting and PLIKSi symptoms was entirely accounted for by the mediators. Specifically, harsh parenting was indirectly associated with both broadly and narrowly defined PLIKSi symptoms through clinically relevant depressive symptoms, and to a lesser extent via external LoC, low self-esteem, and level of anxiety. The strength of these indirect pathways remained largely unchanged after adjustment.
The association between exposure to domestic violence and psychotic symptoms was similar for suspected and definite psychotic symptoms but was attenuated after adjustment for confounders. Approximately one-third of the total effect was accounted for by depressive symptoms and, to a lesser extent, level of anxiety, external LoC, and low self-esteem. Adjusting for confounders explained slightly more of the effect for both broad and narrow PLIKSi symptoms.
Bullying victimization demonstrated the most robust association with both broad and narrow PLIKSi symptoms. Indirect pathways between bullying victimization and psychotic symptoms were apparent mainly via having an external LoC, and to a lesser degree via low self-esteem, depressive symptoms, and level of anxiety. Around one-third of the total effect of bullying victimization on PLIKSi symptoms was accounted for by these mediators. The results were largely unchanged when confounders were included in these models.
The mediating effects of the affective and cognitive factors were broadly similar when examined for boys and girls separately (see online supplementary tables 1 and 2). However, among boys, only around two-thirds of the effect of harsh parenting on narrowly defined psychotic symptoms was accounted for when all of the mediators were included in the model together whereas there appeared to be a much stronger meditational pathway to these definite PLISKi symptoms following exposure to domestic violence than there was for girls.
Discussion
This large longitudinal study is the first to investigate psychological and affective pathways between different forms of victimization and psychotic symptoms in adolescents using prospectively obtained and temporally ordered assessments. Across the whole sample, the weak effect of harsh parenting in childhood on psychotic symptoms in early adolescence was entirely accounted for by the presence of depressive symptoms, level of anxiety, having an external LoC, and low self-esteem in the intervening period. These pathways also seemed to be involved in the appearance of psychotic symptoms following exposure to bullying or domestic violence but accounted for smaller proportions of the overall effects. These results were similar for both suspected and definite psychotic symptoms, following adjustment for a range of confounders and also when examined separately for boys and girls. These findings are consistent with previous cross-sectional analyses that demonstrated mediation of victimization-psychosis associations via psychological and affective factors. 17–20
A substantial proportion of the association between bullying or domestic violence and psychotic symptoms was not mediated by affective or psychological factors. This could indicate “direct” traumatic reactions to these victimizations in the form of increased suspiciousness of others or detachment from reality. 6 , 7 Alternatively, the unexplained portion of the associations could represent residual confounding or mediating factors that were not measured in this study. For example, hostile attribution biases have been hypothesized to arise from early adverse experiences and may increase the risk for developing persecutory delusions. 9 , 10 Anxiety is also postulated to form a major pathway between victimization and psychosis 18 and it is possible that using a categorical measure of the likelihood of having a clinically diagnosed disorder in this study did not capture an appropriate range of anxiety symptoms to detect a more substantial pathway for bullying and domestic violence. Another possibility is that because reports of exposure to bullying were obtained fairly close to the assessment of affective and cognitive mechanisms, this form of victimization may not have had sufficient time to have a major impact upon the child’s psychological functioning. This is especially likely to be the case for LoC that is a fairly stable personality trait and is more likely to be altered following long-term rather than short-term victimization. 43 A range of other potential mechanisms may also be involved in the development of psychotic symptoms following exposure to early victimization (eg, epigenetic changes, interactions with genetic vulnerabilities, dysregulation of the HPA axis, post-traumatic stress disorder, stunted brain development, substance misuse), but these were beyond the scope of this article. The slight gender difference found for pathways to narrowly defined psychotic symptoms is intriguing and requires further investigation in independent samples.
Although the assessments were prospectively obtained, some (particularly bullying and the psychological mediators) were reasonably close together and thus there may have been some overlap in the timing of the experiences. Moreover, the possibility of reverse causality cannot be completely ruled out as the mediating variables and psychotic symptoms were not additionally assessed prior to the victimization exposures. However, it would have been difficult to reliably obtain these variables at younger ages. Additionally, the measure of harsh parenting was only available for mothers and, although domestic violence occurred within the family home after the child was born, it is not possible to ascertain whether the child was definitely present during incidences of domestic violence. These aspects limit the generalizability of the findings. There was also missing data on several of the confounding factors resulting in reduced sample sizes for the adjusted analyses, though previous analysis of this cohort has shown that selective dropout has only a minimal impact on associations between predictors and outcomes. 44 Finally, the psychotic symptoms were only assessed for their presence over the previous 6 months and for many of these children these phenomena may be transitory. Future research is therefore required to both replicate the current findings in other longitudinal cohorts and to investigate whether similar mechanisms also operate for persistent psychotic symptoms that index an even greater risk for the development of psychotic disorders. 45
Nevertheless, these findings tentatively suggest that specific cognitive and affective difficulties in childhood could be targeted to minimize the likelihood of adolescents exposed to early trauma from developing subclinical psychosis. Clearly, replication is required before these findings can be translated into clinical practice but preliminary studies indicate some beneficial effects of cognitive behavior therapy in victimized children. 46 Moreover, our findings highlight the importance of prevention programs to reduce bullying victimization and exposure to domestic violence in order to minimize the appearance of psychotic symptoms in early adolescence.
Funding
Wellcome Trust (GR072043MA); MRC Population Health Scientist postdoctoral fellowship (G1002366 to H.L.F.); The UK Medical Research Council (MRC), the Wellcome Trust, and the University of Bristol (core funding to ALSPAC).
Supplementary Material
Acknowledgments
We are extremely grateful to all the families who took part in this study, the midwives for their help in recruiting them, and the whole ALSPAC team, which includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists, and nurses. We are also grateful for statistical advice from Jon Heron. All authors declare that they have no conflicts of interest in relation to the subject of this study. This publication is the work of the authors and Dr Fisher and Professor Wolke will serve as guarantors for the contents of this article. It does not reflect the views of the ALSPAC executive.
References
- 1. Varese F, Smeets F, Drukker M, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies [Epub ahead of print 2012]. Schizophr Bull.10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39:179–195 [DOI] [PubMed] [Google Scholar]
- 3. Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, Caspi A. Childhood trauma and children’s emerging psychotic symptoms: a genetically sensitive longitudinal cohort study. Am J Psychiatry. 2011;168:65–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Morgan C, Fisher H, Hutchinson G, et al. Ethnicity, social disadvantage and psychotic-like experiences in a healthy population based sample. Acta Psychiatr Scand. 2009;119:226–235 [DOI] [PubMed] [Google Scholar]
- 5. Schreier A, Wolke D, Thomas K, et al. Prospective study of peer victimization in childhood and psychotic symptoms in a nonclinical population at age 12 years. Arch Gen Psychiatry. 2009;66:527–536 [DOI] [PubMed] [Google Scholar]
- 6. Allen JG, Coyne L, Console DA. Dissociative detachment relates to psychotic symptoms and personality decompensation. Compr Psychiatry. 1997;38:327–334 [DOI] [PubMed] [Google Scholar]
- 7. Read J, van Os J, Morrison AP, Ross CA. Childhood trauma, psychosis and schizophrenia: a literature review with theoretical and clinical implications. Acta Psychiatr Scand. 2005;112:330–350 [DOI] [PubMed] [Google Scholar]
- 8. Hardy A, Fowler D, Freeman D, et al. Trauma and hallucinatory experience in psychosis. J Nerv Ment Dis. 2005;193:501–507 [DOI] [PubMed] [Google Scholar]
- 9. Garety PA, Bebbington P, Fowler D, Freeman D, Kuipers E. Implications for neurobiological research of cognitive models of psychosis: a theoretical paper. Psychol Med. 2007;37:1377–1391 [DOI] [PubMed] [Google Scholar]
- 10. Freeman D, Garety P, Fowler D, et al. The London-East Anglia randomized controlled trial of cognitive-behaviour therapy for psychosis. IV: self-esteem and persecutory delusions. Br J Clin Psychol. 1998;37 (Pt 4):415–430 [DOI] [PubMed] [Google Scholar]
- 11. Thewissen V, Bentall RP, Oorschot M, et al. Emotions, self-esteem, and paranoid episodes: an experience sampling study. Br J Clin Psychol. 2011;50:178–195 [DOI] [PubMed] [Google Scholar]
- 12. Thompson A, Sullivan S, Lewis G, et al. Association between locus of control in childhood and psychotic symptoms in early adolescence: results from a large birth cohort. Cogn Neuropsychiatry. 2011;16:385–402 [DOI] [PubMed] [Google Scholar]
- 13. Reijntjes A, Kamphuis JH, Prinzie P, Telch MJ. Peer victimization and internalizing problems in children: a meta-analysis of longitudinal studies. Child Abuse Negl. 2010;34:244–252 [DOI] [PubMed] [Google Scholar]
- 14. Johnson RM, Kotch JB, Catellier DJ, et al. Adverse behavioral and emotional outcomes from child abuse and witnessed violence. Child Maltreat. 2002;7:179–186 [DOI] [PubMed] [Google Scholar]
- 15. Freeman D, Stahl D, McManus S, et al. Insomnia, worry, anxiety and depression as predictors of the occurrence and persistence of paranoid thinking. Soc Psychiatry Psychiatr Epidemiol. [DOI] [PubMed] [Google Scholar]
- 16. Krabbendam L, Myin-Germeys I, Hanssen M, et al. Development of depressed mood predicts onset of psychotic disorder in individuals who report hallucinatory experiences. Br J Clin Psychol. 2005;44:113–125 [DOI] [PubMed] [Google Scholar]
- 17. Gracie A, Freeman D, Green S, et al. The association between traumatic experience, paranoia and hallucinations: a test of the predictions of psychological models. Acta Psychiatr Scand. 2007;116:280–289 [DOI] [PubMed] [Google Scholar]
- 18. Freeman D, Fowler D. Routes to psychotic symptoms: trauma, anxiety and psychosis-like experiences. Psychiatry Res. 2009;169:107–112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bebbington P, Jonas S, Kuipers E, et al. Childhood sexual abuse and psychosis: data from a cross-sectional national psychiatric survey in England. Br J Psychiatry. 2011;199:29–37 [DOI] [PubMed] [Google Scholar]
- 20. Fisher HL, Appiah-Kusi E, Grant C. Depression and anxiety mediate the association between childhood maltreatment and paranoia. Psychiatry Res. 2012;196(2–3):323–324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kelleher I, Harley M, Lynch F, Arseneault L, Fitzpatrick C, Cannon M. Associations between childhood trauma, bullying and psychotic symptoms among a school-based adolescent sample. Br J Psychiatry. 2008;193:378–382 [DOI] [PubMed] [Google Scholar]
- 22. Fisher HL, Jones PB, Fearon P, et al. The varying impact of type, timing and frequency of exposure to childhood adversity on its association with adult psychotic disorder. Psychol Med. 2010;40:1967–1978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hughes HM. Psychological and behavioral correlates of family violence in child witnesses and victims. Am J Orthopsychiatry. 1988;58:77–90 [DOI] [PubMed] [Google Scholar]
- 24. Thomas K, Harrison G, Zammit S, et al. Association of measures of fetal and childhood growth with non-clinical psychotic symptoms in 12-year-olds: the ALSPAC cohort. Br J Psychiatry. 2009;194:521–526 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bowen E, Heron J, Waylen A, Wolke D. Domestic violence risk during and after pregnancy: findings from a British longitudinal study. BJOG. 2005;112:1083–1089 [DOI] [PubMed] [Google Scholar]
- 26. Waylen A, Stallard N, Stewart-Brown S. Parenting and health in mid-childhood: a longitudinal study. Eur J Public Health. 2008;18:300–305 [DOI] [PubMed] [Google Scholar]
- 27. Winsper C, Zanarini M, Wolke D. Prospective study of family adversity and maladaptive parenting in childhood and borderline personality disorder symptoms in a non-clinical population at 11 years [Epub ahead of print 2012]. Psychol Med.10.1017/S0033291712000542. [DOI] [PubMed] [Google Scholar]
- 28. Wolke D, Woods S, Bloomfield L, Karstadt L. The association between direct and relational bullying and behaviour problems among primary school children. J Child Psychol Psychiatry. 2000;41:989–1002 [PubMed] [Google Scholar]
- 29. Griffiths LJ, Wolke D, Page AS, Horwood JP. ALSPAC Study Team. Obesity and bullying: different effects for boys and girls. Arch Dis Child. 2006;91:121–125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Nowicki S, Strickland B. A locus of control scale for children. J Consult Clin Psychol. 1973;42:148–155 [Google Scholar]
- 31. Harter S. Manual for the Self-Perception Profile for Children. Denver, CO: University of Denver, 1985 [Google Scholar]
- 32. Goodman R, Ford T, Richards H, Gatward R, Meltzer H. The Development and Well-Being Assessment: description and initial validation of an integrated assessment of child and adolescent psychopathology. J Child Psychol Psychiatry. 2000;41:645–655 [PubMed] [Google Scholar]
- 33. Goodman A, Heiervang E, Collishaw S, Goodman R. The ‘DAWBA bands’ as an ordered-categorical measure of child mental health: description and validation in British and Norwegian samples. Soc Psychiatry Psychiatr Epidemiol. 2011;46:521–532 [DOI] [PubMed] [Google Scholar]
- 34. Angold A, Costello EJ, Messer SC, Pickles A, Winder F, Silver D. Development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. Int J Methods Psychiatr Res. 1995;5:237–249 [Google Scholar]
- 35. Horwood J, Salvi G, Thomas K, et al. IQ and non-clinical psychotic symptoms in 12-year-olds: results from the ALSPAC birth cohort. Br J Psychiatry. 2008;193:185–191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnoses. J Am Acad Child Adolesc Psychiatry. 2000;39:28–38 [DOI] [PubMed] [Google Scholar]
- 37. World Health Organisation. Schedules for Clinical Assessment in Neuropsychiatry Version 2.0. Washington, DC: American Psychiatric Research, 1994 [Google Scholar]
- 38. Zammit S, Horwood J, Thompson A, et al. Investigating if psychosis-like symptoms (PLIKS) are associated with family history of schizophrenia or paternal age in the ALSPAC birth cohort. Schizophr Res. 2008;104:279–286 [DOI] [PubMed] [Google Scholar]
- 39. Fisher H, Morgan C, Dazzan P, et al. Gender differences in the association between childhood abuse and psychosis. Br J Psychiatry. 2009;194:319–325 [DOI] [PubMed] [Google Scholar]
- 40. Fisher HL, Morgan C, Hutchinson G, et al. Childhood abuse and psychosis in different ethnic groups: a case-control study. Adv Psychol Res. 2011;85:173–181 [Google Scholar]
- 41. Sidebotham P, Heron J. ALSPAC Study Team. Child maltreatment in the “children of the nineties”: the role of the child. Child Abuse Negl. 2003;27:337–352 [DOI] [PubMed] [Google Scholar]
- 42. Wechsler D, Golombok S, Rust J. WISC-IIIUK Wechsler Intelligence Scale for Children. Sidcup, England: Psychological Corp, 1992 [Google Scholar]
- 43. Garbarino J, Gilliam G. Understanding Abusive Families. Lexington, MA: Lexington Books, 1980 [Google Scholar]
- 44. Wolke D, Waylen A, Samara M, et al. Does selective dropout in longitudinal studies lead to biased prediction of behaviour disorders? Br J Psychiatry. 2009;195:249–256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Wigman JT, van Winkel R, Raaijmakers QA, et al. Evidence for a persistent, environment-dependent and deteriorating subtype of subclinical psychotic experiences: a 6-year longitudinal general population study. Psychol Med. 2011;41:2317–2329 [DOI] [PubMed] [Google Scholar]
- 46. Cohen JA. Treating traumatized children: current status and future directions. J Trauma Dissociation. 2005;6:109–121 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.