Abstract
Background: Nonverbal communication is a critical feature of successful social interaction and interpersonal rapport. Social exclusion is a feature of schizophrenia. This experimental study investigated if the undisclosed presence of a patient with schizophrenia in interaction changes nonverbal communication (ie, speaker gesture and listener nodding). Method: 3D motion-capture techniques recorded 20 patient (1 patient, 2 healthy participants) and 20 control (3 healthy participants) interactions. Participants rated their experience of rapport with each interacting partner. Patients’ symptoms, social cognition, and executive functioning were assessed. Four hypotheses were tested: (1) Compared to controls, patients display less speaking gestures and listener nods. (2) Patients’ increased symptom severity and poorer social cognition are associated with patients’ reduced gesture and nods. (3) Patients’ partners compensate for patients’ reduced nonverbal behavior by gesturing more when speaking and nodding more when listening. (4) Patients’ reduced nonverbal behavior, increased symptom severity, and poorer social cognition are associated with others experiencing poorer rapport with the patient. Results: Patients gestured less when speaking. Patients with more negative symptoms nodded less as listeners, while their partners appeared to compensate by gesturing more as speakers. Patients with more negative symptoms also gestured more when speaking, which, alongside increased negative symptoms and poorer social cognition, was associated with others experiencing poorer patient rapport. Conclusions: Patients’ symptoms are associated with the nonverbal behavior of patients and their partners. Patients’ increased negative symptoms and gesture use are associated with poorer interpersonal rapport. This study provides specific evidence about how negative symptoms impact patients’ social interactions.
Key words: schizophrenia, nonverbal communication, rap port, symptoms, social exclusion
Introduction
Schizophrenia affects approximately 1% of the population. 1 An important feature of this disorder is social exclusion. Patients with a diagnosis of schizophrenia have smaller social networks and less satisfactory interpersonal relationships than healthy people or patients with other psychiatric disorders. 2 Recent statistics suggest that at best 15% of patients are in employment in the United Kingdom, 3 far lower than any other group of disabled people. 4 These factors all adversely affect prognosis.
There is a range of, not mutually exclusive, factors that potentially contribute to patients’ social exclusion. For example, bizarre behavior eliciting fear in others, lack of social motivation on the part of the patient, difficulties in interaction arising from different experiences of reality, stigma, and patients’ social functioning deficits. Two of these causes in particular have received much attention: (i) that it is driven by social functioning deficits intrinsic to the disorder and (ii) that it is due to stigmatization by others with knowledge of patients’ diagnosis. Research on possible deficits in social function typically focuses on “offline” tests of social cognition such as the ability to discriminate facial expressions in pictures, attribute emotional states to the protagonists in short narratives, and infer intentions in abstract problem solving contexts. 5 Research on stigma traditionally focuses on the effect of explicitly labeling people as “mentally ill” or “schizophrenic” on the attitudes of others toward them. These attitudinal data are typically gathered using postfacto interview or questionnaire methods. 6 , 7
These approaches to understanding social exclusion focus on the assessment of offline social abilities and attitudes. However, the primary locus of these effects is in “online” social interactions. Patients’ behavior during interactions may be another reason for their social exclusion. Although patients may overtly display bizarre behavior, even in the absence of such overt signs more subtle behavioral anomalies may influence patients’ social inclusion. The phrase “praecox feeling” was part of the working language of early psychiatrists, describing the intuitive feeling of a lack of rapport or connection with the schizophrenia patient. 8 Rumke suggested that this feeling was based on the nonverbal features of patients (ie, motor behavior and facial expressions) and could be determined in the absence of any verbal indicators. 8 Live conversation involves a complex choreography of speech and nonverbal cues such as nodding, gesture, posture, and body movements that help to define the following: who is talking to whom, who will speak next, the structure, meaning and social force of what is being said, and each participant’s level of understanding and alignment with their conversational partners. 9 Effective conversation depends on the close moment-to-moment coordination of these nonverbal cues between interacting partners. 9 This has been associated with greater interpersonal rapport in naturally occurring 10 and experimental settings 11 and greater therapeutic relationship in clinical settings. 12
A number of ethological studies have assessed the nonverbal behavior of patients’ 2-way interactions with clinically trained partners (eg, a psychiatrist) in a treatment context. They report an overall reduction in patients’ nonverbal behavior. Prosocial expressions of facial affect, 13 head movement, body movement, eye gaze, and gesture appear to be particularly reduced. 13 , 14 The association between patients’ nonverbal communication and their symptoms has been mixed, with some studies reporting no association 15 and others reporting a greater nonverbal reduction in patients with more negative symptoms. 13
If nonverbal communication is crucial to interactional success and is reduced in patients’ interactions, this may impact on the success of their interactions with others. Interaction adaptation theory suggests that anomalies in the behavior of one individual results in compensatory behavior being displayed by others. 16 Thus, patients’ unusual nonverbal behavior will be visible in the compensatory behavior of their interacting partners. Few studies have investigated the impact of the patient on the behavior of others. The studies that have, focused on clinical interactions and found that clinicians appear to also reduce their nonverbal behavior rather than compensate. 14 Perhaps, this is a feature of the therapeutic nature of the interaction, and different patterns might arise in first interactions with unfamiliar others outside of a clinical context.
Developing a fuller understanding of social exclusion and possible routes for addressing it depends on obtaining a more accurate picture how this is realized in patients’ online interactions. This study aimed to achieve this by investigating nonverbal communication during patients’ interactions with those unfamiliar to them and unaware of their diagnosis. It focused on 2 central nonverbal behaviors: (i) speaker gesture, used to secure the attention and engagement of listeners, 17 , 18 and (ii) listener nodding, used to demonstrate understanding and provide nonverbal feedback to the speaker. 19 The present study analyzed the pattern of these nonverbal behaviors in small group discussion because they are more typical of the conversations encountered in daily life and in patients’ clinical encounters. 20 , 21 In multiparty interactions nonverbal communication becomes increasingly important. In a 3-person interaction, each person needs to monitor not only their own nonverbal actions and reactions with respect to 2 other people but also 2 other people monitoring each other. Thus, the ability to read and interpret nonverbal cues from multiple participants becomes critical for regulation of the interaction.
The following hypotheses will be addressed:
1. Compared with controls, patients display less speaking gestures and listener nods.
2. Patients’ increased symptom severity and poorer social cognition are associated with patients’ reduced gesture and nods.
3. Patients’ partners compensate for patients’ reduced nonverbal behavior by gesturing more when speaking and nodding more when listening.
4. Patients’ reduced nonverbal behaviors, increased symptom severity, and poorer social cognition are associated with others experiencing poorer rapport with the patient.
Method
This experimental study compared 3-way interaction in 2 conditions: (i) a patient condition, involving 1 patient with a diagnosis of schizophrenia and 2 healthy participants (ie, patients’ partners) and (ii) a control condition, involving 3 healthy participants (ie, controls).
Sample
Twenty patients with a diagnosis of schizophrenia (6 male, 14 female) and 100 nonpsychiatric healthy participants, 40 in the patient condition (21 male, 19 female) and 60 in the control condition (34 male, 26 female) participated in the study. All procedures were approved by a NHS Research Ethics Committee (07/H0711/90). All participants gave written informed consent. Patients were recruited at routine psychiatric outpatient clinics, on the basis of a clinical diagnosis of schizophrenia. Of all patients approached, 25% agreed to participate. Diagnosis was confirmed using the Structured Clinical Interview for Diagnostic symptoms. 22 All patients were categorized as paranoid subtype. Patients presenting with motor side effects from antipsychotic medication (eg, muscle stiffness and involuntary muscle spasms) were excluded from the study based on clinicians’ assessment. Nonfluent English speakers were also excluded. Dosage of antipsychotic medication was converted into chlorpromazine equivalents (CPZE mg/day) according to the standard formula suggested by Woods (2003).23 Three patients were medication free at the time of the study, and the remaining 17 were taking typical (2 patients) or atypical (15 patients) antipsychotic medication.
Nonpsychiatric healthy participants were recruited through advertising on local community Web sites. Of those who responded to the advertisement, 40% participated. Participants with a diagnosis of psychosis or affective disorders in themselves or any first-degree relatives, and those who were not fluent English speakers were excluded. Participants within each group had not met prior to the study. Healthy participants were informed that the study was an investigation of social interaction; they were not aware that there was a psychiatric patient present. All interactions were conducted outside of a psychiatric department (ie, in a nonmedical university department).
Clinical Assessment
Patients’ diagnosis of schizophrenia, paranoid subtype was confirmed using the structured clinical interview for diagnostic symptoms (SCID-IV). 24 The positive and negative syndrome scale for schizophrenia (PANSS) 25 assessed patients’ positive, negative, and general symptoms.
Cognitive Assessments
The Brixton spatial anticipation test (BSAT) and the Hayling sentence completion test (HSCT) assessed participants executive functioning. 26 The BSAT assessed participants’ ability to detect, follow, and adapt to changing patterns. The HSCT assessed participants’ ability to generate or suppress an appropriate response. The Standard Progressive Matrices of Raven 27 was administered to participants to assess nonverbal intelligence quotient (IQ). The profile of nonverbal sensitivity (PONS) test, “the face and body PONS” evaluated patients’ social cognition. 28
Rapport
Each participant rated the level of rapport or connection they felt with each interacting partner on a 10-point scale, with a higher score indicating stronger rapport. 29
Procedure
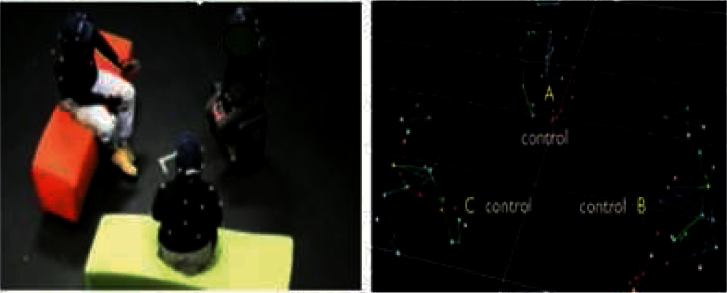
Interactions were recorded in a human interaction laboratory fitted with an optical-based Vicon motion-capture system, consisting of 12 infrared cameras and Vicon iQ software. Participants wore a top and a cap with 27 reflective markers attached (figure 1). Cameras detected the markers at 60 frames per second, resulting in a highly accurate 3D representation of participants’ movements over time (figure 1). After participants were seated, participants were instructed to discuss a moral dilemma called the Balloon Task (described elsewhere). 30 Participants were interviewed after the interaction to complete the rapport questionnaire, to complete the cognitive assessments, and to briefly discuss their experience of the task. ML administered the PANSS and had a high inter-rater reliability score with her trainer RM (Cohen’s Kappa = 0.75).
Fig. 1.
2D image of 3-way interaction (with participants wearing the reflective markers) and the wire-frame representation in 3D.
Identification of Speaker and Listener
This analysis focused on the active speaker-listener pair in the 3-way interaction. At all points during each interaction, the speaker was hand coded from 2D videos using ELAN annotational software. 31 The listener was determined by the speakers’ head orientation, on a frame-by-frame basis, using Python software. 32 Speakers’ head orientation was calculated using the coordinates of their 4 head markers. Head orientation was compared with the centre line, falling between the other 2 participants. If the head orientation was greater than 2° from the centre line, the participant the speaker was orientated toward was identified as the listener. This procedure has been used successfully in previous studies to index listener role in 3-way interactions. 32 Frames with speaker head orientations falling less than 2° from the centre line were excluded from the analysis eliminating frames, where the listener identity was ambiguous (15% of the data).
Nodding
The change in vertical axis head movement per frame, in millimeters, was calculated for each participant. The mean rate of vertical axis head movement (mm/frame) was calculated for each individual. Based on previous research, 33 a head nod was defined as a vertical movement at a speed >0.3mm/frame, with 7 frames between the top and bottom of the nod. Python software 32 identified all head movements falling within this range as nods. This measure was consistent across all participants to allow for direct comparison across participant types. Percentage of nodding in the role of listener was calculated individually.
Gesture
Unlike head nods, hand gestures may occur in any direction. Therefore, change in any direction of the fastest moving hand marker was coded frame-by-frame. The mean rate of hand movement (mm/frame) was calculated for each individual. Hand movements at speeds >1 SD from the mean individual hand movement rate (mm/frame) were defined as a gesture. 32 Percentage of gesture produced when speaking was calculated individually.
Statistical Analysis
Statistical analyses were conducted using SPSS Version 19 (Copyright SPSS Inc, 2010). Patient and healthy participants’ socio-demographic characteristics (age and age leaving education) and their performance on assessments of IQ, executive functioning, and social cognition were compared using an independent samples t test. Distribution of gender was compared between participants in the patient condition (ie, patients and their healthy participant partners), and participants in the control condition (ie, controls) using a Chi square test.
Due to the potential correlations between interacting partners within a triadic group, all analyses of nonverbal behavior and rapport were performed using generalized estimating equations (GEE), which cluster participants by the triadic group they belong to using an exchangeable correlation matrix. This accounts for any within-group interrelatedness between interacting partners. Gamma distributions were used to account for the data distribution. In each model, variables were adjusted for by including them as covariates (continuous variables) or factors (categorical variables).
In order to identify if patients differed in their rate of movement, GEE models compared head movement rate (model 1) and hand movement rate (model 2) (mm/frame) between participant types (ie, patients, patients’ partners, and controls), adjusting for participants’ age and gender.
Differences between participant types (ie, patients, patients’ partners, and controls) in the percentage of time speaking (model 3), listener nodding (model 4), and speaker gesture (model 5) was investigated using 3 separate GEE models, adjusting for participants’ age, gender, and executive functioning. Executive functioning was adjusted for in the analysis to account for the potential cognitive demands of completing the task.
The interrelationships between patients’ clinical characteristics (ie, symptoms [PANSS], duration of illness [in years], antipsychotic medication dose [in CPZE]) and social cognition (PONS) were assessed on a bivariate level. Two GEE models assessed the relationship between patients’ symptoms (PANSS) and social cognition (PONS) with their listener nodding (model 7) and their speaking gesture (model 8). Patients’ medication dose (in CPZE) and duration of illness (in years) were adjusted for in these analyses. Two GEE models assessed the relationship between patients’ symptoms (PANSS) and social cognition (PONS) and their partners’ listener nodding (model 9) and speaking gesture (model 10).
The mean rapport score participants received from their interacting partners was compared between participant types using a GEE analysis adjusting for age and gender (model 6). The relationship between the rapport score patients received from their interacting partners and their symptoms (PANSS), nonverbal behavior (ie, listener nodding and speaker gesture) and social cognition (PONS) was explored using a GEE analysis adjusting for antipsychotic medication dose (CPZE) and duration of illness (in years) (model 11).
Results
Interactions lasted on average 5min 24 s (SD = 1min 55 s). The distribution of gender in the patient 3-way conditions (female = 46.7%) and control 3-way conditions (female = 56.7%) did not significantly differ (X2 (1) = 1.20, P = .27). Patients’ clinical characteristics are displayed in table 1. Three patients were medication free; of those taking medication, their mean antipsychotic medication dose fell within the low dose range (CPZE = 50–200mg/day).34
Table 1.
Patients’ Clinical Information
| Variables | Min | Max | M | SD | ||||
|---|---|---|---|---|---|---|---|---|
| Years diagnosed | 2 | 46 | 15.00 | 10.26 | ||||
| Number of previous admissions | 0 | 20 | 3.85 | 5.01 | ||||
| Previous admissions (weeks) | 0 | 60 | 19.59 | 18.45 | ||||
| Medication dose (CPZE) (mg/day) | 0 | 400 | 167.87 | 109.29 | ||||
| PANSS positive | 7 | 37 | 15.80 | 6.76 | ||||
| PANSS negative | 7 | 19 | 9.95 | 3.36 | ||||
| PANSS general | 16 | 59 | 28.41 | 10.42 |
Participants’ socio-demographic characteristics and scores on assessments of IQ, executive functioning, and social cognition are displayed in table 2. Patients were significantly older than healthy participants (P ≤ .01) and displayed poorer performance on assessments of executive functioning (P ≤ .01) and social cognition (P < .01). Patients did not differ from healthy participants on IQ (P = .75).
Table 2.
Participants’ Socio-Demographic and Cognitive Characteristics
| Variables | Patients (n = 20) | Healthy Participants (n = 100) | T | df | P | ||
|---|---|---|---|---|---|---|---|
| M | SD | M | SD | ||||
| Age | 41.50 | 8.64 | 31.10 | 9.60 | −4.51 | 119 | <.01 |
| Age leaving education | 19.37 | 3.78 | 21.10 | 5.60 | 1.29 | 119 | .19 |
| IQ | 46.67 | 3.09 | 45.89 | 1.30 | −0.26 | 119 | .75 |
| Executive functioning: spatial | 3.07 | 0.51 | 5.10 | 0.22 | 3.65 | 119 | <.01 |
| Executive functioning: verbal | 3.79 | 0.43 | 4.91 | 0.18 | 2.52 | 119 | <.01 |
| Social cognition: PONS | 26.28 | 2.97 | 28.11 | 24.35 | 2.94 | 118 | <.01 |
Participants’ head movement rate (model 1), hand movement rate (model 2), time speaking (model 3), listener nodding (model 4), and speaking gesture (model 5) are displayed in table 3. Patients did not differ from controls on head (P = .83) or hand (P = .59) movement rate. However, male participants had a greater rate of head movement than female participants (P = .01). Compared with control participants, patients spoke less (P = .02) and gestured less when speaking (P < .03), while their healthy participant partners spoke more (P = .05).
Table 3.
Time Speaking, Nonverbal Behavior and Rapport by Participant Type
| Model | 95% CI | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | M | SD | ß | SE | Lower | Upper | Chi2 | df | P | |
| 1. Head movement rate (mm/frame) | ||||||||||
| Patients | 20 | 0.22 | 0.03 | −0.026 | 0.12 | −0.260 | 0.207 | 0.05 | 1 | .83 |
| Patients’ partners | 40 | 0.26 | 0.02 | 0.132 | 0.10 | −0.061 | 0.327 | 1.82 | 1 | .18 |
| Controls | 60 | 0.22 | 0.02 | — | — | — | — | — | — | — |
| Gender male | 62 | 0.26 | 0.02 | 0.226 | 0.09 | 0.047 | 0.404 | 6.13 | 1 | .01 |
| Gender female | 58 | 0.21 | 0.02 | — | — | — | — | — | — | — |
| 2. Hand movement rate (mm/frame) | ||||||||||
| Patients | 20 | 1.01 | 0.15 | −0.084 | 0.16 | −0.399 | 0.230 | 0.28 | 1 | .59 |
| Patients’ partners | 40 | 1.31 | 0.09 | 0.186 | 0.12 | −0.042 | 0.419 | 2.54 | 1 | .11 |
| Controls | 60 | 1.09 | 0.11 | — | — | — | — | — | — | — |
| 3. Time speaking (%) | ||||||||||
| Patients | 20 | 25.64 | 12.64 | −0.262 | 0.11 | −0.478 | −0.047 | 5.68 | 1 | .02 |
| Patients’ partners | 40 | 37.18 | 12.86 | 0.109 | 0.04 | 0.035 | 0.184 | 8.28 | 1 | <.01 |
| Controls | 60 | 33.33 | 12.68 | — | — | — | — | — | — | — |
| 4. Nodding as listener (%) | ||||||||||
| Patients | 20 | 12.49 | 9.32 | −0.042 | 0.23 | −0.501 | 0.417 | 0.03 | 1 | .86 |
| Patients’ partners | 40 | 13.13 | 7.32 | 0.243 | 0.19 | −0.128 | 0.614 | 1.65 | 1 | .19 |
| Controls | 60 | 16.55 | 9.21 | — | — | — | — | — | — | — |
| 5. Gesture as speaker (%) | ||||||||||
| Patients | 20 | 12.08 | 10.96 | −0.505 | 0.24 | −0.976 | −0.035 | 4.43 | 1 | .03 |
| Patients’ partners | 40 | 16.07 | 14.80 | −0.194 | 0.14 | −0.472 | 0.084 | 1.87 | 1 | .17 |
| Controls | 60 | 12.59 | 12.43 | — | — | — | — | — | — | — |
| 6. Rapport | ||||||||||
| Patients | 20 | 6.21 | 2.31 | −0.004 | −0.19 | 0.186 | 0.001 | 0.00 | 1 | .96 |
| Patients’ partners | 40 | 7.18 | 1.32 | 0.085 | −0.03 | 0.195 | 2.305 | 2.51 | 1 | .11 |
| Controls | 60 | 6.68 | 1.22 | — | — | — | — | — | — | |
Model 1. Goodness of fit QICC = 32.51
Model 2. Goodness of fit QICC = 51.68
Model 3. Goodness of fit QICC = 26.38
Model 4. Goodness of fit QICC = 123.66
Model 5. Goodness of fit QICC = 64.14
Model 6. Goodness of fit QICC = 12.62
On a bivariate level, patients’ social cognitive scores were not associated with their clinical characteristics. Patients’ higher general symptoms were significantly associated with higher positive symptoms (ρ[20] = 0.71, P < .01) and higher antipsychotic medication dose (ρ[20] = 0.48, P = .03). Because such patients’ general symptom scores were not included in the GEE analyses, no other significant relationships were identified.
The relationships between nonverbal communication and patients’ symptoms and social cognition are dis played in table 4. Patients with more negative symptoms nodded less when listening and gestured more when speaking. Patients with more positive symptoms nodded more when listening. Patients’ partners displayed less listener nodding when patients were more symptomatic (ie, positive or negative symptoms). Patients’ partners’ increased speaking gesture was associated with patients having more negative symptoms. Patients’ social cognition was not associated with nonverbal behaviors displayed by patients or their partners.
Table 4.
Relationship Between Patients’ Clinical Features, Nonverbal Behavior and Rapport
| 95% CI | |||||||
|---|---|---|---|---|---|---|---|
| Model | ß | SE | Lower | Upper | Chi2 | df | P |
| 7. Patients’ listener nodding | |||||||
| PANSS negative | −0.276 | 0.05 | −0.370 | −0.183 | 33.61 | 1 | <.01 |
| PANSS positive | 0.117 | 0.04 | 0.030 | 0.205 | 6.86 | 1 | <.01 |
| 8. Patients’ speaking gesture | |||||||
| PANSS negative | 0.126 | 0.05 | 0.031 | 0.221 | 6.71 | 1 | .01 |
| 9. Patients’ partners’ listener nodding | |||||||
| PANSS positive | −0.036 | 0.01 | −0.057 | −0.015 | 11.44 | 1 | <.01 |
| PANSS negative | −0.070 | 0.04 | −0.140 | −0.001 | 3.92 | 1 | .04 |
| 10. Patients’ partners’ speaking gesture | |||||||
| PANSS negative | 0.081 | 0.02 | 0.037 | 0.125 | 12.95 | 1 | <.01 |
| 11. Others’ experience of rapport with the patient | |||||||
| Patients’ speaking gesture | −0.065 | 0.01 | −0.079 | −0.052 | 86.61 | 1 | <.01 |
| PANSS positive | 0.053 | 0.01 | 0.040 | 0.067 | 58.43 | 1 | <.01 |
| PANSS negative | −0.081 | 0.02 | −0.124 | −0.038 | 13.46 | 1 | <.01 |
| Social cognition | 0.027 | 0.01 | 0.011 | 0.054 | 3.92 | 1 | .05 |
Model 7. Goodness of fit QICC = 26.29
Model 8. Goodness of fit QICC = 17.30
Model 9. Goodness of fit QICC = 34.41
Model 10. Goodness of fit QICC = 26.70
Model 11. Goodness of fit QICC = 10.19
Rapport score did not significantly differ between participant types (table 3, model 6). In the postinteraction interview with the researcher, healthy participants did not report anything unusual about the patient, nor did they differentiate between the patient and the other healthy participant they were interacting with. Others experiencing poorer rapport with the patient was associated with patients gesturing more when speaking, having more negative symptoms, fewer positive symptoms, and poorer social cognition (table 4, model 11).
Discussion
This study has 3 main findings. First, patients speak less and make less use of gesture when speaking. Second, patients’ symptoms were associated with the nonverbal behavior of patients and their interacting partners. Specifically, patients’ increased negative symptoms were associated with patients and their partners nodding less when listening and gesturing more when speaking. Patients with more positive symptoms displayed more listener nodding, while their partners displayed less. Third, patients’ increased speaking gesture was associated with others experiencing poorer rapport with the patient. Patients’ increased negative symptoms, reduced positive symptoms, and poorer social cognition were also associated with others experiencing poorer rapport with the patient.
Patients were distinguishable from controls by their reduced speaking gesture. This suggests that patients use fewer nonverbal cues to gain and maintain the attention of their listeners and add clarity or emphasis to their speech. 18 This was seen in the absence of an overall reduction in patients’ rate of movement (mm/frame), which is consistent with findings of ethological studies in clinical setting, 35 although the methods of coding gesture differ significantly.
Patients’ nonverbal expression was associated with their symptom profile. Patients with more positive symptoms used more nonverbal behaviors used to demonstrate understanding and feedback to their speaking partner. Their partners appear to compensate for this by providing less of these cues when they are listening. Patients with more negative symptoms displayed less nodding when listening, thus providing fewer indicators of their understanding to their speaking partner. Their partners appear to respond to this by gesturing more when speaking. Studies in nonclinical populations have found that speakers use more gesture when conversation is problematic (eg, when the speaker feels that the listener is not attending to or understanding their speech). 18 In the current study, patients’ partners may be responding to a perceived difficulty with patients’ attentiveness or comprehension of their speech by gesturing more to gain their attention or aid comprehension of their verbal message. Patients in the current study had only mild negative symptoms. Hence, it would appear that, even when negative symptoms are mild, others, who are unaware of the patient’s diagnosis, are responding to the behavioral manifestations of these symptoms.
Patients with more negative symptoms also gestured more when speaking. This finding could be accounted for by a number of explanations. First, the motion-based methods used to detect gesture may also be detecting additional movements such as scratching or displacement behaviors and movements that would be classified as a gesture in observational analysis (eg, McNeill, 1992). 36 Although all detected hand movements may be communicative, their functional meaning may differ, with scratching or displacement behaviors possibly conveying anxiety. 37 Observational analysis, identifying the form of patients’ hand movements with their speech, would be required to see if this is the case. A second explanation is that patients may be increasing their use of gesture while speaking in response to the reduced nonverbal feedback being displayed by their listening partners. Thus, it is unclear if patients’ increased speaking gesture is inappropriate, or a response to the reduced feedback of their interacting partners. Patients’ increased speaking gesture was significantly associated with others experiencing poorer rapport with the patient during the interaction. This finding highlights patients’ gesture use as a possible indicator of the interpersonal relationships within the interaction. Nonverbal movements are highly coordinated with the temporal features of speech. 38 Previous studies have shown that reduced coordination between speech and gesture is problematic and distracting for the listener. 38 Furthermore, coordination of nonverbal behavior is associated with rapport. 10 Perhaps patients’ speaking gestures are less coordinated with their speech, which impacts on others’ experience of rapport with them.
Although patients’ poorer social cognition was not associated with speaking gesture or listener nodding, it was associated with others experiencing less rapport with the patient. The exploratory nature of this study and its small sample size may have limited the power to detect associations between patients’ nonverbal behavior and their social cognition. However, perhaps patients’ social cognition influences features of patients’ communication beyond those measured in this study. Future studies with larger sample sizes should investigate the interrelationships between patients’ social cognitive skills, their verbal, and nonverbal communication and others’ experience of rapport.
Patients’ increased negative symptoms were also associated with others experiencing poorer rapport with the patient. This finding emulates those from clinical interactions 39 and role play tasks where patients’ negative symptoms were associated with confederates’ increased interpersonal distance. 40 Contrary to predictions, patients’ increased positive symptoms were associated with others experiencing better rapport with the patient. In the current study, the variance on patients’ positive symptoms was relatively low, with most patients experiencing mild to moderate positive symptoms. Perhaps mild positive symptoms manifest as better engagement in the interaction (eg, increased speech). It would be expected that patients with more severe positive symptoms, displaying more unusual or threatening behavior such as responding verbally to internal stimuli, may not show this association with rapport.
Strengths and Limitations
These findings should be considered in the context of the study’s limitations and strengths. First, this is the first controlled experimental study to examine how others respond to patients when they are unaware of their presence. This removes the possible confounding elements of clinical context such as prior knowledge of diagnosis, the history between the clinician and the patient, and the balance of roles in the institutional relationship. Second, this is the first study to use 3D motion-capture techniques to investigate nonverbal behavior in patients’ social interactions. This provided precise 3D coordinates of nonverbal activity that can at best be approximated from 2D video, and this removes the element of error in human coding of 2D video. Third, the statistical analyses adjusted for intragroup influences within each 3-person interaction, avoiding overinflating differences between participant types.
First, this was an exploratory study and as such had a relatively small sample size. Patients with motor side effects from antipsychotic medication such as stiffness or spasm were excluded from the study. In addition, patients were taking low doses of medication and this was adjusted for in the analyses. However, a direct comparison between medicated and nonmedicated patients would be necessary to identify the precise influence of medication on patients’ nonverbal behavior. Second, there was the limited variance on symptoms, with most patients having mild symptom profiles. This may be due to the selection bias of the study because those who are less symptomatic may be more willing to participate in a study of this kind. Despite this, individuals interacting with patients responded to the behavioral manifestation of patients’ symptoms, suggesting that nonverbal adaptation in patients’ interactions occurs when symptom levels are relatively low. Third, detection of gesture was based on speed of movement rather than observational coding. Thus, other hand movements and gestures may have been detected. Fourth, interactions in the current study were short and representative of a patients’ first meeting with unfamiliar others. Others’ response patterns may not be generalizable to longer interactions or those between patients and familiar others. Future studies should investigate how nonverbal patterns of patients and their partners unfold over longer or repeated interactions and its impact on others’ experience of rapport.
Overall, this study suggests that peoples’ nonverbal behavior and experience of rapport changes in response to the behavior of a patient even when they are unaware of their diagnosis. These findings advance our knowledge of nonverbal patterns of behavior in first meetings between patients with schizophrenia and unfamiliar others, providing the first evidence of a link with patients’ symptoms, their nonverbal communication, and the rapport experienced by others. This study demonstrates the importance of looking not just at patients in isolation but the impact of their presence on others in online interaction.
Conclusions
Patients’ symptoms are associated with the nonverbal behavior of patients and their partners. Patients’ increased negative symptoms and gesture use are associated with poorer interpersonal rapport. These results demonstrate how the dynamic equilibrium of nonverbal communication is disrupted, for all participants, in patients’ conversations, and this influences others’ experience of interpersonal rapport. This study provides specific evidence about how negative symptoms impact patients’ interactions with others. This may have implications for therapeutic interventions designed to target patients’ social outcomes.
Funding
Engineering and Physical Sciences Research Council Doctoral Training Programme (EP/P502683/1).
Acknowledgments
We thank Stuart Battersby for development of the Python program used in the data analysis. The Authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1. World Health Organization. The global burden of disease: 2004 Update. Geneva, Switzerland: WHO Library; 2004. [Google Scholar]
- 2. Erickson DH, Beiser M, Iacono WG, Fleming JA, Lin TY. The role of social relationships in the course of first-episode schizophrenia and affective psychosis. Am J Psychiatry. 1989;146:1456–1461. [DOI] [PubMed] [Google Scholar]
- 3.Social Exclusion Unit. Mental Health and Social Exclusion: A Social Exclusion Unit Report. London: Office of the Deputy Prime Minister; 2004. [Google Scholar]
- 4. Perkins R, Rinaldi M. Unemployment rates among patients with long-term mental health problems: a decade of rising unemployment. Psychiatr Bull. 2002;26:295–298. [Google Scholar]
- 5. Penn DL, Sanna LJ, Roberts DL. Social cognition in schizophrenia: an overview. Schizophr Bull. 2007;34:408–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Penn DL, Martin J. The stigma of severe mental illness: some potential solutions for a recalcitrant problem. Psychiatr Q. 1998;69:235–247. [DOI] [PubMed] [Google Scholar]
- 7. Thompson AH, Stuart H, Bland RC, et al. WPA. World Psychiatric Association. Attitudes about schizophrenia from the pilot site of the WPA worldwide campaign against the stigma of schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2002;37:475–482. [DOI] [PubMed] [Google Scholar]
- 8. Rumke HC. Das Kernsyndrom der Schizophrenie und das ‘Praecox-Gefuhl’. Zentralblatt gesamte Neurologie und Psychiatrie. 1941;102:168–169. [Google Scholar]
- 9. Clark HH, Schaefer EF. Contributing to discourse. Cogn Sci. 1989;13:259–294. [Google Scholar]
- 10. Bernieri F, Rosenthal R. Interpersonal coordination: behavior matching and interactional synchrony. Feldman RS, Rimé B. Fundamentals of nonverbal behavior. Cambridge: Cambridge University Press; 1991:401–432. [Google Scholar]
- 11. Chartrand TL, Bargh JA. The chameleon effect: the perception-behavior link and social interaction. J Pers Soc Psychol. 1999;76:893–910. [DOI] [PubMed] [Google Scholar]
- 12. Ramseyer F, Tschacher W. Nonverbal synchrony in psychotherapy: coordinated body movement reflects relationship quality and outcome. J Consult Clin Psychol. 2011;79:284–295. [DOI] [PubMed] [Google Scholar]
- 13. Brüne M, Sonntag C, Abdel-Hamid M, Lehmkämper C, Juckel G, Troisi A. Nonverbal behavior during standardized interviews in patients with schizophrenia spectrum disorders. J Nerv Ment Dis. 2008;196:282–288. [DOI] [PubMed] [Google Scholar]
- 14. Kupper Z, Ramseyer F, Hoffmann H, Kalbermatten S, Tschacher W. Video-based quantification of body movement during social interaction indicates the severity of negative symptoms in patients with schizophrenia. Schizophr Res. 2010;121:90–100. [DOI] [PubMed] [Google Scholar]
- 15. Gaebel W, Wölwer W. Facial expressivity in the course of schizophrenia and depression. Eur Arch Psychiatry Clin Neurosci. 2004;254:335–342. [DOI] [PubMed] [Google Scholar]
- 16. Burgoon JK, Stern LA, Dillman L. Interpersonal Adaptation: Dyadic Interaction Patterns. Cambridge: Cambridge University Press; 1995. [Google Scholar]
- 17. Bavelas JB, Kenwood C, Johnson T, Phillips B. An experimental study of when and how speakers use gestures to communicate. Gesture. 2002;2:1–17. [Google Scholar]
- 18. Holler J, Beattie GW. Pragmatic aspects of representational gestures: do speakers use them to clarify verbal ambiguity for the listener? Gesture. 2003;3:127–154. [Google Scholar]
- 19. Boholm M, Allwood J. Repeated head movements, their function and relation to speech. In: Proceedings of the seventh international conference on Language Resources and Evaluation (LREC) Malta; 2010. [Google Scholar]
- 20. Eshghi A. Uncommon Ground: The Distribution of Dialogue Contexts. London: School of Electronic Engineering and Computer Science, Queen Mary University of London; 2009. [Google Scholar]
- 21. McCabe R, Skelton J, Heath C, Burns T, Priebe S. Engagement of patients with psychosis in the consultation: conversation analytic study commentary: understanding conversation. Br Med J. 2002;325:1148–1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Health Disorders. 4th ed. Washington, DC: American Psychiatric Association; 2000. [Google Scholar]
- 23. Woods SW. Chlorpromazine equivalent doses for the newer atypical antipsychotics. J Clin Psychiatry. 2003;64:663–667. [DOI] [PubMed] [Google Scholar]
- 24. Michael B, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition. (SCID-I/P). New York: New York State Psychiatric Institute Biometrics Research; 2002. [Google Scholar]
- 25. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. [DOI] [PubMed] [Google Scholar]
- 26. Burgess P, Shallice T. The Hayling and Brixton Tests. Bury St. Edmunds, UK: Thames Valley Test Company; 1997. [Google Scholar]
- 27. Raven JC, Court JH. Manual for Raven’s Progressive Matrices and Vocabulary Scales. Oxford, UK: Oxford University Press; 1992. [Google Scholar]
- 28. Rosenthal R, Hall JA, DiMatteo MR, Rogers PL, Archer D. Sensitivity to Nonverbal Communication. The PONS Test. Baltimore, MD: John Hopkins University Press; 1979. [Google Scholar]
- 29. Drolet AL, Morris MW. Rapport in conflict resolution: accounting for how nonverbal exchange fosters coordination on mutually beneficial settlements to mixed motive conflicts. J Exp Soc Psychol. 2000;36:26–50. [Google Scholar]
- 30. Purver M, Healey P, King J, Ginzburg J, Mills G. Answering clarification questions. In: Proceedings of the 4th SIGdial Workshop on Discourse and Dialogue. Sapporo, Japan; 2003. [Google Scholar]
- 31. Wittenberg P, Burgman H, Russel A, Klassmann A, Sloetjes H. ELAN: a professional framework for multimodality research. Paper presented at Fifth International Conference on Language Resources and Evaluation (LREC) Paris: ELRA; 2006. [Google Scholar]
- 32. Battersby SA, Healey PGT. Head and hand movements in the orchestration of dialogue. Paper presented at Thirty-Second Annual Conference of the Cognitive Science Society; 11th–14th August; Portland, OR; 2010. [Google Scholar]
- 33. Cerrato L, Svanfeldt G. A method for the detection of communicative head nods in expressive speech. In: Proceedings from The Second Nordic Conference on Multi-modal Communication Gothenburg, Sweden: Gothenburg University; 2005. [Google Scholar]
- 34. Barbui C, Saraceno B, Liberati A, Garattini S. Low-dose neuroleptic therapy and relapse in schizophrenia: meta- analysis of randomized controlled trials. Eur Psychiatry. 1996;11:306–313. [DOI] [PubMed] [Google Scholar]
- 35. Mittal VA, Tessner KD, McMillan AL, Delawalla Z, Trotman HD, Walker EF. Gesture behavior in unmedicated schizotypal adolescents. J Abnorm Psychol. 2006;115:351–358. [DOI] [PubMed] [Google Scholar]
- 36. McNeill D. Hand and Mind: What Gestures Reveal About Thought. Chicago: University of Chicago Press; 1992. [Google Scholar]
- 37. Troisi A. Displacement activities as a behavioral measure of stress in nonhuman primates and human subjects. Stress. 2002;5:47–54. [DOI] [PubMed] [Google Scholar]
- 38. Bavelas JB, Gerwing J. The listener as ddressee in face-to-face dialogue. Int J Listen. 2011;25:178–198. [Google Scholar]
- 39. Grube M. Towards an empirically based validation of intuitive diagnostic: Rümke’s ‘praecox feeling’ across the schizophrenia spectrum: preliminary results. Psychopathology. 2006;39:209–217. [DOI] [PubMed] [Google Scholar]
- 40. Penn DL, Kohlmaier JR, Corrigan PW. Interpersonal factors contributing to the stigma of schizophrenia: social skills, perceived attractiveness, and symptoms. Schizophr Res. 2000;45:37–45. [DOI] [PubMed] [Google Scholar]