Abstract
Objectives
Little is known about how recent system-wide increases in demand for critical care have affected U.S. emergency departments (EDs). This study describes changes in the amount of critical care provided in U.S. EDs between 2001 and 2009.
Design
Analysis of data from the National Hospital Ambulatory Medical Care Survey for the years 2001–2009.
Setting
National multistage probability sample of U.S. ED data. U.S. ED capacity was estimated using the National Emergency Department Inventory-United States.
Patients
ED patients admitted a critical care unit.
Interventions
None.
Measurements
Annual hours of ED-based critical care and annual number critical care ED visits. Clinical characteristics, demographics, insurance status, setting, geographic region, and ED length of stay for critically ill ED patients.
Main Results
Annual critical care unit admissions from U.S. EDs increased by 79% from 1.2 to 2.2 million. The proportion of all ED visits resulting in critical care unit admission increased from 0.9% to 1.6% (ptrend < 0.001). Between 2001 and 2009, the median ED length of stay for critically ill patients increased from 185 to 245 minutes (+ 60 min; ptrend < 0.02). For the aggregated years 2001–2009, ED length of stay for critical care visits was longer among black patients (12.6% longer) and Hispanic patients (14.8% longer) than among white patients, and one third of all critical care ED visits had an ED length of stay greater than 6 hrs. Between 2001 and 2009, total annual hours of critical care at U.S. EDs increased by 217% from 3.2 to 10.1 million (ptrend < 0.001). The average daily amount of critical care provided in U.S. EDs tripled from 1.8 to 5.6 hours per ED per day.
Conclusions
The amount of critical care provided in U.S. EDs has increased substantially over the past decade, driven by increasing numbers of critical care ED visits and lengthening ED length of stay. Increased critical care burden will further stress an already overcapacity U.S. emergency care system.
Keywords: critical care, crowding, emergency service, health care disparities, hospital/workforce
The burden of caring for critically ill patients in the United States is massive, currently accounting for nearly 1% of the gross domestic product and affecting large sectors of the U.S. healthcare system including the emergency department (ED) (1–3). The majority of critical care in the United States are provided to patients over the age of 65, and this population is predicted to grow by 50% from 2000 to 2020 (4, 5). The rising demand for critical care in the face of already insufficient capacity has become an area of concern for clinicians, hospital administrators, and policymakers (6–9). In 2000, the American College of Chest Physicians, the American Thoracic Society, and the Society of Critical Care Medicine Committee on Manpower for Pulmonary and Critical Care Societies forecast large shortfalls in the critical care workforce. A 2006 Health Resources and Services Administration report to Congress not only confirmed the predicted shortages, but also projected worsening shortages into the future (4). There currently exist little data on how system-wide increases in the demand for critical care are affecting U.S. EDs.
Most patients, critically ill patients in the United States are admitted from an ED (10). These patients typically require medically complex and resource intensive care often begins outside the ICU in the ED (2, 3, 10, 11). The provision of critical care in the ED is a potentially important factor in ED crowding. The Institute of Medicine report “Hospital-Based Emergency Care: At The Breaking Point” identified that the inability to promptly admit critically ill ED patients to inpatient beds can lead to boarding and contributes to ED crowding (12). Several studies suggest that the proportion of critically ill patients presenting to U.S. EDs is increasing (13–15). Additionally, other studies have questioned the ability of many EDs to provide optimal care for critically ill patients in crowded conditions and linked prolonged ED stays by critically ill patients with increased mortality (16–18).
This study investigates changes in the total hours of ED care provided to patients ultimately admitted to an ICU from U.S. EDs between 2001 and 2009. To evaluate the hypothesis that EDs are providing an increasing amount of critical care, we examined both trends in ED visit ICU admissions and trends in the median ED length of stay (EDLOS) for these patients. Additionally, we analyzed trends in the national ED capacity to estimate changes in the average daily hours of care provided to patients admitted to an ICU at an average U.S. ED.
MATERIALS AND METHODS
Study Design
We analyzed publically available data from the National Hospital Ambulatory Medical Care Survey (NHAMCS) between 2001 and 2009. NHAMCS is an annual survey of U.S. ED visits conducted by the National Center for Health Statistics. NHAMCS uses a four-stage probability design to collect a nationally representative sample of all visits to EDs based in general and short stay hospitals, excluding federal hospitals, hospital units of institutions, and hospitals with fewer than six staffed beds.
EDs were defined as facilities that provide emergency care 24 hours per day and 7 days per week, and they are accessible by the general public; urgent care centers with known hours of closure are not included in NHAMCS. U.S. Census Bureau workers train hospital staff to collect data on a random sample of ED patient visits during a randomly assigned 4-week period each year. Briefly, ED surveys are submitted to a central processing facility where they are checked both manually and by computerized algorithm to detect data inconsistencies (19). The NHAMCS methodology is described in detail elsewhere (19). We extracted data on ED visit characteristics, including demographics, insurance status, LOS, diagnosis, disposition, and hospital characteristics, including setting and location.
A comprehensive list of all nonfederal U.S. hospitals with EDs was obtained using the National ED Inventories (NEDI)-United States database (http://www.emnet-usa.org/) (20). The NEDI-United States database was created by integrating data from three sources: the SMG Marketing Group’s Hospital Market Profiling Solution Database, the American Hospital Association Annual Survey of Hospitals, and data collected independently by staff from the Emergency Medicine Network at Massachusetts General Hospital. The NEDI-United States database contains hospital-level data, including ED visit volume, region, and urban vs. rural setting for the years 2001, 2003, 2005, 2007, and 2009 (20). For the intervening years, the average number of EDs from the two adjacent years was used in our calculations. We only used (NEDI)-United States A data to determine the annual total number of operational EDs by region in the United States; no ED visit level data were used in our analysis.
We calculated total patient care hours provided over the course of 1 year using EDLOS data contained in NHAMCS where EDLOS is defined as the minutes elapsed from the time of a patient’s registration to the time of the patient’s discharge from the ED. EDLOS data were missing from 26,863 visit records (8.3% of all visits). Visits without information about EDLOS showed small but statistically significant differences in race/ethnicity, region, ownership, and metropolitan statistical area designation from visits with information on EDLOS (data not shown). We excluded visits with missing EDLOS data from all subsequent analysis. Our analysis was exempted from human subjects review by the Alameda County Medical Center Institutional Review Board and the Partners Healthcare Human Research Committee.
Case Definitions
We chose a simple operational definition, adapted from Fromm et al (21) to identify ED visits where critical care was provided—all ED visits that ultimately resulted in admission to an ICU were assumed to have required critical care during their ED stay. Previous investigations have shown increased use of diagnostic testing, advanced, imaging, and procedures among patients admitted to an ICU from the ED, suggesting active care for these patients while in the ED (2, 15, 21, 22). Beginning in 2005, NHAMCS data contain additional disposition information on ED visits where critical care was likely provided—those resulting in discharge to an operating room or cardiac catheterization lab. To maintain a consistent year-to-year case definition, these ED visits resulting in discharge to an operating room or cardiac catheterization lab were excluded from all years in our analysis.
Statistical Analysis
We used Stata 10.0 software (StataCorp, College Station, TX) to calculate nationally representative estimates with 95% confidence intervals (CIs) using assigned weights, which adjust for selection probability and nonresponse. We accounted for non-normal distribution of the EDLOS variable by utilizing median EDLOS in our univariate comparisons and transforming EDLOS, using the natural logarithm, when performing parametric tests. To describe the distribution of EDLOS, we computed median EDLOS and the interquartile range (IQR). Time trends were analyzed using bivariate weighted linear regression with time included as a continuous variable. Ptrend values less than 0.05 were considered statistically significant.
To best account for data skewing due to outliers with very long EDLOS, we use natural log-transformed EDLOS prior to regression analyses. The linear regression beta-coefficient is reported as percent change in EDLOS based on the mean of the natural log-transformed data. Predictors of EDLOS were analyzed by multivariate regression using the natural log-transformed EDLOS as the outcome variable. Although in the United States there are no established benchmarks for optimal EDLOS for critically ill patients, we considered EDLOS of 6 hours or greater as prolonged based on the research of Chalfin et al (23) who demonstrated an association between increased mortality and EDLOS greater than 6 hours for critically ill ED patients.
The total hours of ED care provided in a given year were calculated by a summation of the EDLOS recorded in NHAMCS for that year. To calculate the daily hours of ED critical care per U.S. ED, weighted NHAMCS estimates of the annual total of hours of ED critical care were used as numerators over the denominator of the number of operational U.S. EDs obtained from NEDI-United States data. This result was then divided by 365 calendar days to yield an estimate of the average burden critical care per ED per day; these results were then stratified by metropolitan service area and geographic region.
For our primary outcome of total annual hours of ED care provided to patients admitted to an ICU, we were able to test for temporal trends using a weighted linear regression; however, direct testing for interaction between strata was not possible with our methodology. Interaction testing was performed using logistic regression for total number of annual critical care ED visits. For median EDLOS, a linear regression was used to evaluate strata interactions in temporal trends.
RESULTS
Between 2001 and 2009, annual visits by critically ill patients to U.S. EDs increased by 79% from 1.2 to 2.2 million. The proportion of ED visits resulting in admission to a critical care bed increased by 75% from 0.9% to 1.6% (ptrend < 0.001). Among ED patients ultimately admitted to the hospital, the proportion admitted to an ICU increased from 7.9% to 15.1% (ptrend < 0.001).
We found large increases in the number of annual ED visits by critically ill patients in all age groups; surprisingly, a disproportionate increase among older patients was not found (pinteraction > 0.10). There were smaller increases in the number of critical care ED visits by whites than by blacks (pinteraction < 0.06) or Hispanics (pinteraction < 0.03). Increases in critical care ED visits did not differ by expected source of payment (pinteraction > 0.10). ED visits’ increases by critically ill patients were primarily at urban EDs (Table 1).
TABLE 1.
Estimated Burden of Critical Care in U.S. Emergency Departments, 2001–2009
| Emergency Department Visit Characteristics | Critical Care Emergency Department Visits,a
n = 4,605b
|
|||||||
|---|---|---|---|---|---|---|---|---|
| Estimate Number of Visits, in Tens of Thousands
|
Median Length of Stay (Min) (Interquartile Range)
|
Estimated Burden of Critical Care, in Hundreds of Thousands of Hours Per Year (95% Confidence Interval)
|
||||||
| 2001c | 2009c | 2001c | 2009c | 2001c | 2009c | % Change | ptrendd | |
| All | 120 | 220 | 185 (125, 291) | 245 (157, 380) | 32 (22–42) | 100 (76–130) | + 217 | < 0.001 |
|
| ||||||||
| Age (yr) | ||||||||
| < 18 | 5.5 | 7.0 | 213 (14, 258) | 185 (75, 274) | 2.1 (0.9–3.3) | 2.0 (0.9–3.1) | −5 | 0.41 |
| ≥ 18 | 115 | 205 | 198 (137, 304) | 245 (155, 367) | 41 (30–52) | 98 (77–118) | + 139 | < 0.001 |
| 18–44 | 20 | 36 | 204 (140, 310) | 294 (157, 401) | 7.4 (4.7–10.2) | 19 (13–25) | + 158 | 0.007 |
| 45–64 | 36 | 65 | 196 (140, 310) | 258 (166, 359) | 14 (8.7–19) | 31 (23–39) | + 129 | < 0.001 |
| ≥ 65 | 60 | 105 | 195 (130, 295) | 227 (145, 349) | 20 (14–26) | 47 (37–58) | + 137 | 0.001 |
|
| ||||||||
| Sex | ||||||||
| Female | 55 | 105 | 205 (145, 306) | 250 (150, 360) | 21 (14–27) | 49 (37–61) | + 135 | < 0.001 |
| Male | 65 | 110 | 190 (137, 282) | 236 (155, 367) | 22 (16–29) | 51 (39–62) | + 128 | < 0.001 |
|
| ||||||||
| Race/ethnicity | ||||||||
| White, non- Hispanic | 95 | 140 | 193 (137, 295) | 233 (150, 348) | 33 (23–43) | 61 (47–74) | + 86 | 0.002 |
| Black, non- Hispanic | 18 | 41 | 220 (146, 312) | 295 (173, 417) | 6.9 (4.4–9.4) | 24 (15–33) | + 250 | < 0.001 |
| Hispanic | 5.5 | 28 | 240 (163, 385) | 244 (159, 360) | 2.7 (0.1–5.2) | 11 (7.4–15) | + 328 | < 0.001 |
|
| ||||||||
| Insurance | ||||||||
| Private insurance | 34 | 45 | 198 (137, 310) | 229 (141, 343) | 13 (7.6–18) | 19 (14–23) | + 47 | 0.02 |
| Medicare/Medicaid | 65 | 140 | 137 (200, 298) | 246 (157, 373) | 25 (17–32) | 68 (53–83) | + 177 | < 0.001 |
| Uninsured | 10 | 13 | 179 (80, 248) | 248 (115, 403) | 2.8 (1.7–4.0) | 6.3 (2.6–9.9) | + 123 | 0.03 |
|
| ||||||||
| Hospital setting | ||||||||
| Rural | 27 | 25 | 180 (117, 255) | 187 (147, 240) | 8.9 (2.1–16) | 7.9 (2.7–13) | −11 | 0.18 |
| Urban | 95 | 190 | 209 (140, 307) | 255 (155, 378) | 34 (24–44) | 92 (71–113) | + 168 | < 0.001 |
|
| ||||||||
| Hospital location | ||||||||
| Northeast | 15 | 47 | 219 (164, 316) | 264 (171, 371) | 5.4 (2.8–8) | 20 (11–30) | + 277 | 0.004 |
| Midwest | 33 | 47 | 188 (134, 254) | 236 (141, 367) | 10 (6.2–14) | 23 (12–34) | + 128 | 0.003 |
| South | 47 | 70 | 225 (140, 310) | 243 (153, 350) | 17 (9.6–25) | 32 (22–43) | + 89 | 0.001 |
| West | 26 | 50 | 186 (130, 302) | 245 (151, 350) | 10 (3.5–17) | 24 (12–35) | + 129 | 0.01 |
Emergency department visits that resulted in admission to an ICU.
Unweighted total number of emergency department visits by critically ill patients, 2001–2009.
Stratified analysis of subgroups were done using the average of years 2001–2002 and 2008–2009 due to some small subpopulations.
p value for 8-yr trend in burden of critical care.
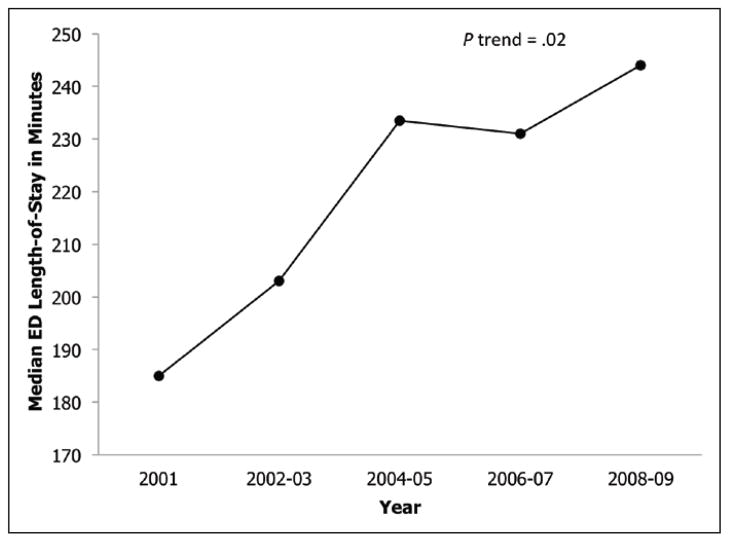
The median EDLOS for visits resulting in ICU admission increased by 60 minutes from 185 to 245 minutes (+ 32%; ptrend = 0.02) (Fig. 1). In multivariable analysis of all critically ill ED visits between 2001 and 2009, adult patients had 30% (95% CI, 14% to 45%) longer EDLOS than children. Increased LOS among critically ill ED patients was associated with visits by blacks (17% longer) and Hispanics (15% longer) vs. visits by white patients. Visits by critically ill patients to urban EDs were associated with a 20% increase in EDLOS compared with visits to rural EDs (Table 2). One third of critical care ED visits had prolonged EDLOS greater than 6 hours (33%; 95% CI, 30% to 35%). The median wait to see a physician was 17 minutes (IQR 5, 40).
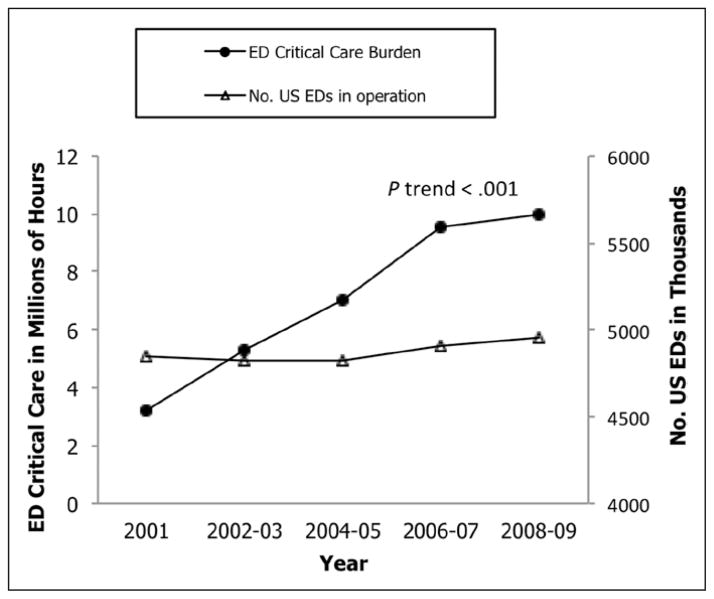
Figure 1.
Estimated annual burden of critical care and emergency department (ED) capacity in the United States, 2001–2009.
TABLE 2.
Multivariable Adjusted Percent Change in Length of Stay for Critical Care Visits to U.S. Emergency Departments, 2001–2009, by Patient and Hospital Characteristicsa
| Emergency Department Visit Characteristics | Adjusted Percent Change, n = 5,295
|
p |
|---|---|---|
| % (95% Confidence Interval) | ||
| Critical care visits by age | ||
| 18–44 | Reference | |
| 45–64 | −1.2 (−10.5 to 8) | 0.80 |
| ≥ 65 | −14.9 (−26.9 to −2.9) | 0.02 |
|
| ||
| Critical care visits by sex | ||
| Female | Reference | |
| Male | −6.1 (−13.5 to 1.3) | 0.11 |
|
| ||
| Critical care visits by race/ethnicity | ||
| White, non-Hispanic | Reference | |
| Black, non-Hispanic | 12.6 (2.1–23) | 0.02 |
| Hispanic | 14.8 (2.6–27.1) | 0.02 |
| Other | −2.8 (−20.2 to 14.7) | 0.76 |
|
| ||
| Critical care visits by insurance | ||
| Private insurance | Reference | |
| Medicare/Medicaid | 8.0 (−1.5 to 17.6) | 0.10 |
| Uninsured | −14.8 (−28.1 to −1.5) | 0.03 |
|
| ||
| Critical care visits by hospital setting | ||
| Rural | Reference | |
| Urban | 26.2 (14.1–38.3) | < 0.001 |
|
| ||
| Critical care visits by hospital location | ||
| Northeast | 21.3 (−36.9 to −5.8) | < 0.01 |
| Midwest | Reference | |
| South | 7.4 (−7.4 to 22.2) | 0.33 |
| West | 12.0 (−6.3 to 30.2) | 0.20 |
Critical care visits are defined as emergency department visits that resulted in admission to an ICU.
The total annual hours of critical care provided in U.S. EDs increased from 3.2 to 10.1 million hours (+ 217%; ptrend < 0.001) (Fig. 2). Estimated increases in critical care burden likely resulted from both greater numbers of annual ED visits by critically ill patients and an increasing LOS for these patients. Over the study period, this increased burden was distributed over a stable population of operational U.S. EDs (4,861 in 2001 vs. 4,967 in 2009). As a result, the estimated average daily burden of critical care per U.S. EDs more than tripled from 1.8 to 5.6 hours per day (+ 210%; ptrend < 0.001). Although there were significant increases among all ethnic/racial groups, increases among blacks (+ 250%; ptrend = 0.001) and Hispanics (+ 328%; ptrend < 0.001) were apparently larger than those among whites (+ 86%; ptrend < 0.001). The increases in ED critical care burden were primarily at EDs in urban settings; there were no significant increases in critical care ED visits to rural EDs (ptrend = 0.18) (Table 1).
Figure 2.
Estimated median emergency department (ED) length of stay in United States for ED visits resulting in admission to an ICU, 2001–2009.
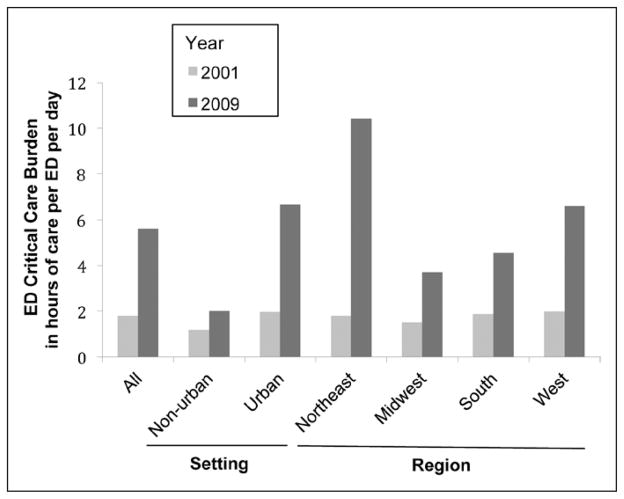
Urban EDs in all regions of the county experienced significant increases in the average daily burden of critical care per ED; by contrast, we found no significant increase at rural EDs. Regionally, the largest increase was observed at EDs in the Northeast (Fig. 3).
Figure 3.
Estimated daily burden of critical care per emergency department (ED) in the United States, 2001–2009, by region and setting.
DISCUSSION
We estimate that the total amount of critical care provided in U.S. EDs more than tripled between 2001 and 2009—corresponding to an additional 6.9 million hours of critical care provided each year in U.S. EDs. The observed increases in ED critical care was spread over a stable national ED capacity, resulting in an average increase of 3.8 hours (+ 210%) of additional critical care provided each day per U.S. ED. The clear annual increase in the burden of critical care at urban U.S. EDs, across all regions nation-wide, suggests that future increases are likely.
The direct explanation for the observed increases in critical care at U.S. EDs is the combination of both increasing ED visits by critically ill patients and increasing EDLOS for these patients. ED visits by critically ill patients increased both in absolute terms and as a proportion of all hospitalizations. From 2001 to 2009, critical care ED visits increased by 87%, and the proportion of critically ill patients increased from 7.9% to 15.1% of all ED-based hospital admissions. While our finding of increasing critical care ED visits is consistent with nation-wide trends in overall ED visits, our analysis indicates that there was a disproportionate increase in visits by critically ill patients (24).
We found large increases in critical care ED visits by adults of all age groups. Surprisingly, the increase in ED critical care burden does not appear to be driven by an aging population alone. There are several possible explanations for increasing critical care ED visits among these younger patients. Increasing rates of hospitalization and mortality from severe sepsis could potentially lead to increasing critical care ED visits among younger patients (25). Additionally, increases in the prevalence of chronic medical conditions (e.g., diabetes) that predispose patients to episodes of critical illness may have contributed to increased critical care ED visits (26). Although the role of access to outpatient care on ED utilization is complex, it is possible ongoing shortages in access to primary care due to lack of insurance could have contributed to some patients delaying care, resulting in increases in the numbers of patients presenting with decompensated disease (27).
In addition to the increasing number of ED critical care visits, we found that the median EDLOS before transfer to an ICU increased by over 30% (60 min). Given the relatively short wait time to be seen by a physician we observed, the vast majority of time spent in the ED likely represents active hands-on care by ED physicians, nurses, and ancillary staff. Although there are no consensus EDLOS benchmarks in the United States, research suggests that for critically ill ED patients EDLOS greater than 6 hrs carries with it an increased risk of mortality and morbidity (28). We found prolonged EDLOS greater than 6 hours was present in over one-third of all critical care ED visits. Additionally, despite widespread attention to racial and ethnic health disparities, our data suggest that critically ill black and Hispanic ED patients continue to experience longer EDLOS than their white counterparts (15). Increases in ED critical care were largest in the northeastern United States, consistent with the well-described pattern of an overall increased rate of health care utilization in this region.
Our results join a growing body of evidence that there is a trend toward increasing volume of higher acuity patients in U.S. EDs who undergo more testing, procedures, and advanced diagnostic imaging while in the ED (10, 13–15, 28, 29). This may be, in part, driven by recent advances in the ED-based care of critically ill and injured patients, such as early goal-directed therapy and increased use of advanced imaging in patients with traumatic injuries (22, 30–32). As the ED-based care of critically ill patients becomes more complex and involves an increasing number of diagnostic tests (such as computed tomography imaging), invasive procedures (such as placement of central venous catheters), and implementation of complex therapies some degree of EDLOS prolongation may be inevitable (15, 28, 30). A recent study by Pitts et al (28) found both increased rates of high-acuity patients in U.S. EDs and large increases in the volume of diagnostic testing, medications given, and EDLOS, suggesting that increased intensity of ED care may be a major driver of worsening ED crowding in the United States.
Although the total number of critical care beds increased modestly by 6.5%, the total number of hospitals with critical care medicine beds actually decreased by 12.2% between 2001 and 2005 (2). Limitations in the availability of inpatient critical care beds likely prolong EDLOS in many EDs as patients are boarded in the ED. The 2002 report commissioned by the American Hospital Association entitled “Emergency Department Overload: a growing crisis—the results of the American Hospital Association Survey of Emergency Department (ED) and Hospital Capacity” found that the most common reason for ED diversion was lack of staffed inpatient critical care beds (16). Accordingly, increasing inpatient ICU capacity has been shown to reduce time spent on ED diversion and shorten EDLOS for critically ill ED patients (14).
In 2000, the Committee on Manpower for Pulmonary and Critical Care Societies expressed concern that the U.S. health system was unprepared for the predicted growth in the critical care disease burden (5). Our results suggest that a significant portion of the critical care burden has shifted to the ED setting. While most U.S. EDs have staffing and equipment to provide ICU-level care, the ED is designed for initial diagnosis and stabilization with additional care to be provided in the appropriate setting. However, the ED has, by necessity, absorbed deficiencies in the capacity of inpatient ICUs. The traditional, staged model of care in which a patient moves from outpatient to ED to critical care bed is clearly strained by both the volume of critical care and the need to rapidly coordinate time-sensitive diagnostics, interventions, and specialty consultations. Continued exploration of patient centered models of care that deploy ICU level care wherever the patient’s geographic location would appear warranted as does increased emphasis on critical care within emergency medicine training and certification (29, 33).
Critical care is resource intensive and draws staff away from the care of other ED patients, which may impede the overall ED throughput and detract from the care of other patients. The decision to admit a patient to an ICU is in itself potentially time consuming and may involve multiple consultants with differing thresholds for admission and complex end of life discussions. Additionally, there is little standardization in the critical care capacity of U.S. EDs, and some are not designed or appropriately staffed to adequately care for critically ill patients over prolonged periods of time. Both during times of clinically active care and time spent in the ED awaiting ICU admission, critically ill patients are resource intensive and may strain limited ED resources. Though the research is limited, there are several studies that suggest delay in the transfer of critically ill patients to the ICU is associated with poor outcomes including increased mortality (23, 34–38). As implementation of the Patient Protection and Affordable Care Act proceeds, adequate resource allocation to improve critical care capacity in U.S. EDs should be a priority.
There are several potential limitations to our study. First, our methodology to identify critically ill patients is based on ED visit disposition alone without objective physiologic parameters. Various institutions may have different criteria for admission to a critical care inpatient bed and significant heterogeneity may exist between institutions. Alternate methods to identify critically ill patients, such as the Acute Physiology and Chronic Health Evaluation (APACHE) require data not collected in NHAMCS. An advantage of our operational case definition based on ultimate disposition is that it allows for a clear assessment of national trends in ED utilization of inpatient critical care resources. Second, it is not possible to distinguish active care vs. time spent boarding patients waiting for transfer to an inpatient unit. In support of our findings, previous studies have shown large increases in the volume of ED-based diagnostic testing and utilization of computed tomography and magnetic resonance imaging in recent years, suggestive of an intensification of ED care (15, 28). In particular, patients admitted to the ICU appear to undergo more testing and have more treatments than patients admitted to a lower level of care, supporting our assumption that these patients likely have clinically more severe disease (15). Finally, our results likely represent an underestimation of critically ill patients. NHAMCS began collecting data on ED patients discharged to an operating room or cardiac catheterization laboratory in 2005 and to maintain a consistent case definition we did not include these visits in our analysis. Additionally, we were not able to identify critically ill patients who were cared for in the ED but were not admitted to an ICU, such as those transferred to another facility. A strength of our study is that we based our calculations of ED capacity on NEDI-United States data, the most complete available inventory of operational U.S. EDs.
CONCLUSIONS
Our study suggests there is a strong trend toward an increasing amount of critical care being provided in U.S. EDs. EDs have been traditionally designed to provide initial evaluation and treatment of critically ill patients, with transfer of these patients in a timely manner to an inpatient ICU. The rising burden of ED critical care is a significant stress on the already over-capacity U.S. system of ED-based care, threatening the ability of U.S. EDs to fulfill their mission to be always available to receive acutely ill and injured patients and to provide them with the highest quality care.
Footnotes
Presented at the Society for Academic Emergency Medicine annual meeting, June 2011, Boston, MA.
Dr. Maselli received funding from the CDC. The remaining authors have not disclosed any potential conflicts of interest.
References
- 1.Rivers EP, Nguyen HB, Huang DT, et al. Critical care and emergency medicine. Curr Opin Crit Care. 2002;8:600–606. doi: 10.1097/00075198-200212000-00020. [DOI] [PubMed] [Google Scholar]
- 2.Halpern NA, Pastores SM. Critical care medicine in the United States 2000–2005: An analysis of bed numbers, occupancy rates, payer mix, and costs. Crit Care Med. 2010;38:65–71. doi: 10.1097/CCM.0b013e3181b090d0. [DOI] [PubMed] [Google Scholar]
- 3.Halpern NA. Can the costs of critical care be controlled? Curr Opin Crit Care. 2009;15:591–596. doi: 10.1097/MCC.0b013e328332f54f. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Department of Health and Human Services. Health Resources and Services Administration Report to Congress: The critical care workforce. [Accessed June 14, 2011];A study of the supply and demand for critical care physicians. Available at: http://bhpr.hrsa.gov/healthworkforce/reports/studycriticalcarephys.pdf.
- 5.Angus DC, Kelley MA, Schmitz RJ, et al. Caring for the critically ill patient. Current and projected workforce requirements for care of the critically ill and patients with pulmonary disease: Can we meet the requirements of an aging population? JAMA. 2000;284:2762–2770. doi: 10.1001/jama.284.21.2762. [DOI] [PubMed] [Google Scholar]
- 6.Angus DC, Shorr AF, White A, et al. Critical care delivery in the United States: Distribution of services and compliance with Leapfrog recommendations. Crit Care Med. 2006;34:1016–1024. doi: 10.1097/01.CCM.0000206105.05626.15. [DOI] [PubMed] [Google Scholar]
- 7.Wunsch H, Rowan KM, Angus DC. International comparisons in critical care: A necessity and challenge. Curr Opin Crit Care. 2007;13:725–731. doi: 10.1097/MCC.0b013e3282f1bb56. [DOI] [PubMed] [Google Scholar]
- 8.Kelley MA, Angus D, Chalfin DB, et al. The critical care crisis in the United States: A report from the profession. Chest. 2004;125:1514–1517. doi: 10.1378/chest.125.4.1514. [DOI] [PubMed] [Google Scholar]
- 9.Wunsch H, Angus DC, Harrison DA, et al. Variation in critical services across North America and Western Europe. Crit Care Med. 2008;36:2787–93. e1. doi: 10.1097/CCM.0b013e318186aec8. [DOI] [PubMed] [Google Scholar]
- 10.Lilly CM, Zuckerman IH, Badawi O, et al. Benchmark data from more than 240,000 adults that reflect the current practice of critical care in the United States. Chest. 2011;140:1232–1242. doi: 10.1378/chest.11-0718. [DOI] [PubMed] [Google Scholar]
- 11.Halpern NA, Pastores SM, Greenstein RJ. Critical care medicine in the United States 1985–2000: An analysis of bed numbers, use, and costs. Crit Care Med. 2004;32:1254–1259. doi: 10.1097/01.ccm.0000128577.31689.4c. [DOI] [PubMed] [Google Scholar]
- 12.Institute of Medicine Committee on the Future of Emergency Care in the U.S. Health System. Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: National Academy Press; 2006. [Google Scholar]
- 13.Lambe S, Washington DL, Fink A, et al. Trends in the use and capacity of California’s emergency departments, 1990–1999. Ann Emerg Med. 2002;39:389–396. doi: 10.1067/mem.2002.122433. [DOI] [PubMed] [Google Scholar]
- 14.McConnell KJ, Richards CF, Daya M, et al. Effect of increased ICU capacity on emergency department length of stay and ambulance diversion. Ann Emerg Med. 2005;45:471–478. doi: 10.1016/j.annemergmed.2004.10.032. [DOI] [PubMed] [Google Scholar]
- 15.Herring A, Wilper A, Himmelstein DU, et al. Increasing length of stay among adult visits to US emergency departments, 2001–2005. Acad Emerg Med. 2009;16:1–8. doi: 10.1111/j.1553-2712.2009.00428.x. [DOI] [PubMed] [Google Scholar]
- 16.Lewin Group. Emergency Department Overload: A growing crisis—The results of the American Hospital Association Survey of Emergency Department (ED) and Hospital Capacity. Falls Chuch: Lewin Group; 2002. [Google Scholar]
- 17.Chalfin DB, Trzeciak S, Likourezos A, et al. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483. doi: 10.1097/01.CCM.0000266585.74905.5A. [DOI] [PubMed] [Google Scholar]
- 18.Tilluckdharry L, Tickoo S, Amoateng-Adjepong Y, et al. Outcomes of critically ill patients. Am J Emerg Med. 2005;23:336–339. doi: 10.1016/j.ajem.2005.02.038. [DOI] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention. NHAMCS description. U.S. Centers for Disease Control and Prevention; [Accessed September 8, 2009]. Web site. Available at: http://www.cdc.gov/nchs/about/major/ahcd/sampham.htm. [Google Scholar]
- 20.Sullivan AF, Richman IB, Ahn CJ, et al. A profile of US emergency departments in 2001. Ann Emerg Med. 2006;48:694–701. doi: 10.1016/j.annemergmed.2006.08.020. [DOI] [PubMed] [Google Scholar]
- 21.Fromm RE, Jr, Gibbs LR, McCallum WG, et al. Critical care in the emergency department: A time-based study. Crit Care Med. 1993;21:970–976. doi: 10.1097/00003246-199307000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Varon J, Fromm RE, Jr, Levine RL. Emergency department and length of stay for critically ill medical patients. Ann Emerg Med. 1994;23:546–549. doi: 10.1016/s0196-0644(94)70075-3. [DOI] [PubMed] [Google Scholar]
- 23.Chalfin DB, Trzeciak S, Likourezos A, et al. Impact of delayed transfer of critically ill patients from the emergency department to the intensive care unit. Crit Care Med. 2007;35:1477–1483. doi: 10.1097/01.CCM.0000266585.74905.5A. [DOI] [PubMed] [Google Scholar]
- 24.Tang N, Stein J, Hsia RY, et al. Trends and characteristics of US emergency department visits, 1997–2007. JAMA. 2010;304:664–670. doi: 10.1001/jama.2010.1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dombrovskiy VY, Martin AA, Sunderram J, et al. Rapid increase hospitalization and mortality rates for severe sepsis in the United States: A trend analysis from 1993 to 2003. Crit Care Med. 2007;35:1244–1250. doi: 10.1097/01.CCM.0000261890.41311.E9. [DOI] [PubMed] [Google Scholar]
- 26.Steinberger J, Daniels SR. Obesity, insulin resistance, diabetes, and cardiovascular risk in children: An American Heart Association scientific statement from the Atherosclerosis, Hypertension, and Obesity in the Young Committee (Council on Cardiovascular Disease in the Young) and the Diabetes Committee (Council on Nutrition, Physical Activity, and Metabolism) Circulation. 2003;107:1448–1453. doi: 10.1161/01.cir.0000060923.07573.f2. [DOI] [PubMed] [Google Scholar]
- 27.Richman IB, Clark S, Sullivan AF, et al. National study of the relation of primary care shortages to emergency department utilization. Acad Emerg Med. 2007;14:279–282. doi: 10.1197/j.aem.2006.10.093. [DOI] [PubMed] [Google Scholar]
- 28.Pitts SR, Pines JM, Handrigan MT. National trends in emergency department occupancy, 2001 to 2008: Effect of inpatient admissions versus emergency department practice intensity. Ann Emerg Med. 2012;60:679–686. doi: 10.1016/j.annemergmed.2012.05.014. [DOI] [PubMed] [Google Scholar]
- 29.Kocher KE, Meurer WJ, Fazel R, et al. National trends in use of computed tomography in the emergency Department. Ann Emerg Med. 2012;58:452–462. doi: 10.1016/j.annemergmed.2011.05.020. [DOI] [PubMed] [Google Scholar]
- 30.Schuur JD, Venkatesh AK. The growing role of departments in hospital admissions. N Engl J Med. 2012;367:391–393. doi: 10.1056/NEJMp1204431. [DOI] [PubMed] [Google Scholar]
- 31.Gardner RL, Sarkar U, Maselli JH, et al. Factors associated with longer ED lengths of stay. Am J Emerg Med. 2007;25:643–650. doi: 10.1016/j.ajem.2006.11.037. [DOI] [PubMed] [Google Scholar]
- 32.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–1377. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 33.Ghosh R, Pepe P. The critical care cascade: A systems approach. Curr Opin Crit Care. 2009;15:279–283. doi: 10.1097/MCC.0b013e32832faef2. [DOI] [PubMed] [Google Scholar]
- 34.Cowan RM, Trzeciak S. Clinical review: Emergency department overcrowding and the potential impact on the critically ill. Crit Care. 2005;9:291–295. doi: 10.1186/cc2981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sprivulis PC, Da Silva JA, Jacobs IG, et al. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. Med J Aust. 2006;184:208–212. doi: 10.5694/j.1326-5377.2006.tb00416.x. [DOI] [PubMed] [Google Scholar]
- 36.Richardson DB. Increase in patient mortality at 10 days associated with emergency department overcrowding. Med J Aust. 2006;184:213–216. doi: 10.5694/j.1326-5377.2006.tb00204.x. [DOI] [PubMed] [Google Scholar]
- 37.Carter AW, Pilcher D, Bailey M, et al. Is ED length of stay before ICU admission related to patient mortality? Emerg Med Australas. 2010;22:145–150. doi: 10.1111/j.1742-6723.2010.01272.x. [DOI] [PubMed] [Google Scholar]
- 38.Rivers EP, Nguyen HB, Huang DT, et al. Critical care and emergency medicine. Curr Opin Crit Care. 2002;8:600–606. doi: 10.1097/00075198-200212000-00020. [DOI] [PubMed] [Google Scholar]