Abstract
This study examined treatment needs of men and women in Substance Use Disorder treatment. The sample (n = 489) was recruited between 2006 and 2007 from a Midwestern state in the US, and participants were grouped based on injury occurring in partner and non-partner relationships in the past year. Rates of injury across relationship types were alarming with over 54.8% reporting injuring another person and 55.4% reporting being injured. Overall, those injuring non-partners or both partners/non-partners had more severe problems. Implications of the findings for SUD treatment settings and a model for integrated violence prevention are discussed.
Keywords: Aggression, Injury, Alcohol, Drugs, Treatment, Subtypes
Introduction
Violence is a common problem for individuals in substance use disorder (SUD) treatment. Studies of SUD samples have found rates of past year violence towards partners to be about 50% (Chermack, Fuller, and Blow, 2000, 2001; O’Farrell and Murphy, 1995), approximately two to three times greater than rates found in community-based samples (Schafer, Caetano, and Clark, 1998). A study of a SUD treatment sample found that violence towards non-partners (e.g., friends, strangers) exceeded 66% for men and 39% for women, and that rates of violence exceeded 70% for both men and women when collapsing across partner and non-partner relationships (Chermack et al., 2000; 2001). Involvement with violence (both towards others as well as victimization) is a marker for substance misuse problem severity, poor treatment response and legal problems (Brown, et al., 1998; Schuckit and Russell, 1984). Moreover, violence has numerous costs with regard to physical, mental health, interpersonal, and occupational functioning. Thus, it is crucial to develop and implement effective intervention approaches in SUD treatment settings.
Despite high rates of violence among people in SUD treatment, there is very little information regarding treatment approaches that impact violence with this population. Further, there is some evidence that SUD settings do not employ systematic assessment of interpersonal violence, that relatively few individuals in SUD settings are referred for domestic violence prevention interventions, and that even fewer follow-up with referrals to outside agencies for treatment for domestic violence (Schumacher, Fals-Stewart and Leonard, 2003). SUD treatment settings provide an important point of access for targeted violence prevention treatment, and offer an ideal context for incorporating therapies targeting violence related problems. For example, research has demonstrated that Behavioral Couples Therapy (BCT) (O’Farrell and Fals-Stewart, 2000; O’Farrell and Murphy, 1995) has sound empirical support in terms of impacting both substance use and aggression in couples’ relationships. However, BCT requires participants to have a partner willing and able to attend treatment, is focused on the partner relationship, and does not address violence in non-partner relationships. Thus, there clearly is a need for more broad-based and empirically supported violence prevention interventions for men and women in SUD treatment for whom BCT may not be available, possible or indicated [e.g., violence is with non-partners (e.g., friends, strangers), partner refuses to participate, violence may be with dating partners and/or others but there is no stable “partner” relationship]. A few studies have suggested that cognitive-behavioral approaches have some promise (Beck and Fernandez, 1998; Edmondson and Conger, 1996; Reilly and Shopshire, 2000), but we are not aware of any studies with randomized controlled designs testing such interventions in SUD samples that have included measurement of violence outcomes. In order to develop, test and implement more broad-based violence prevention interventions in SUD treatment settings, it is necessary to obtain a better understanding of factors related to violence across both partner and non-partner relationships. This study examines the nature and extent of violence resulting in injury to partners, non-partners and both partners/non-partners, as well as injury to participants caused by partners, non-partners, and both partners/non-partners in SUD treatment, and is designed to identify potential violence prevention treatment needs for SUD treatment settings.
There is evidence from studies of martially violent men that there are “subtypes” of aggressors (Holtzworth-Munroe and Meehan, 2004; Huss and Langhinrichsen-Rohling, 2006). Many studies have identified what has been characterized as “family only” aggressors, as well as “generally violent and antisocial” (GVA) aggressors. In general, “family only” aggressors have relatively low levels of psychopathology and substance misuse, and are more similar to nonviolent men than other aggressor subtypes. The GVA individuals are aggressive towards their partners as well as others, tend to have more substance use problems, antisocial behaviors (Holtzworth-Munroe and Meehan, 2004; Huss and Langhinrichsen-Rohling, 2006), high scores on depression measures (Huss and Langhinrichsen-Rohling, 2006), and are more likely to drop out of domestic violence treatment interventions (Stalans and Seng, 2007). However, these studies tended to focus on only male violence towards partners, and were conducted using non-substance use disorder treatment samples. Thus, information regarding potential gender differences and whether correlates of violence subtypes differ for those enrolled in SUD treatment is limited. Further, there is very little data regarding whether there are differences in groups who report being injured by partners, non-partners or both. Nevertheless, prior findings raise concerns that individuals reporting violence in non-partner or both partner and non-partner relationships may have somewhat different characteristics and potential treatment needs than those reporting only partner violence.
Factors Related To Violence
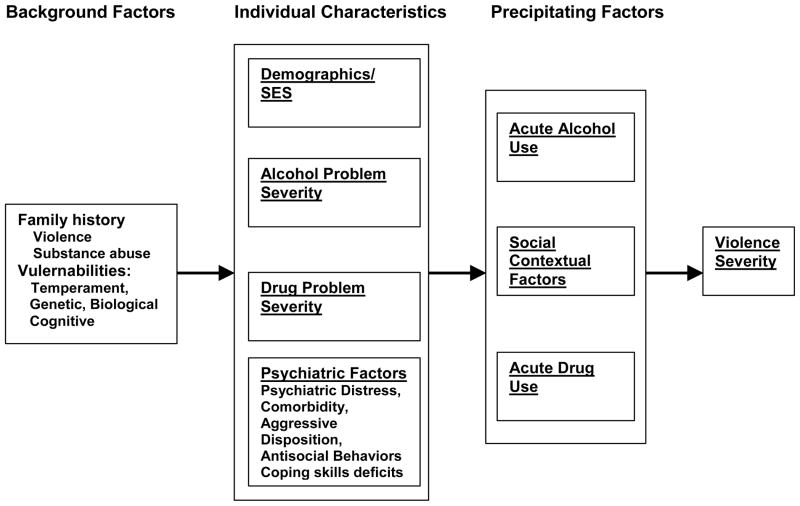
Prior research findings and theory can help identify potential areas to investigate to identify potential treatment needs for men and women in SUD treatment with violence problems. Figure 1 summarizes factors associated with violence based on prior findings and theory (Chermack and Giancola, 1997, Goldstein, 1985; Pernanen, 1991; Quigley and Leonard, 2000). Distal background factors related to violence include family history of substance misuse and/or violence, as well as other vulnerabilities (e.g., executive cognitive functioning deficits, difficult temperament). Several individual characteristic factors also have been linked to violence perpetration and victimization, including demographics, substance use- and psychiatric- problem severity, aggressive personality traits, and alcohol and drug-problem severity. Further, a number of studies have found that aggressive individuals have poor coping skills and cognitive styles conducive to aggression. Copenhaver (2000) found that men in SUD treatment with violence problems had less competent coping skills with regard to marital situations, as well as greater attribution of negative intent to their partner, and Lee et al. (1997) found violent cocaine dependent men had greater difficulty with relaxation skills. Holtzworth-Munroe and Anglin (1991) found that violent men had less competent coping responses to certain marital situations (rejection, jealousy, challenges from partner) compared to distressed and non-distressed non-violent men. Finally, immediate precipitating factors include social and contextual factors (relationship type, social influences, situational factors) as well as acute alcohol and drug effects (Brown et al., 1998; Chermack and Blow, 2002; Chermack and Giancola, 1997; Fagan, 1993; Schuckit and Russell, 1984; Walton et al., 2003).
Figure 1.
Factors related to Violence
The issue of comorbid psychiatric problems may be an important risk factor for violence perpetration and victimization among men and women in SUD treatment. Studies with SUD samples have revealed high rates of comorbid psychiatric disorders, many of which (PTSD, Antisocial Personality Disorder, Depressive Disorders, other serious mental illness - SMI) have also been linked to violence risk (Arboleda-Florez, 1998; Dinwiddie, 1992; Pan, Neidig, and O’Leary, 1994; Swanson et al., 1990). Psychiatric distress has also been shown to be associated with violence cross-sectionally (Chermack et al., 2001), and to be predictive of violence during a subsequent 2-year follow-up interval in SUD samples (Walton, Chermack and Blow, 2002). There is evidence that individuals with depressive symptoms or SMI have higher risks of violence involvement, particularly if they are using substances and are not receiving treatment with psychiatric medications (Fava, 1998; Swartz et al., 1998a; 1998b; Swanson et al., 1997). For example, Huss and Langhinrichsen-Rohling (2006) found that generally violent aggressive men had relatively high levels of depression symptoms. This also appears to hold true for violence victimization; for example, Stuart et al. (2006) found that women victimized by partners had higher rates of depression, PTSD and Generalized Anxiety Disorder. Finally, there also is some evidence that psychopathology may be related to dropping out of treatment for domestic violence (Daly and Pelowsky, 2000).
Although there is a paucity of data on effective treatment interventions targeting violence in SUD samples, there is some evidence to support that addressing domains of risk is related to reductions in substance use and/or violence. For example, studies have found that lower post-treatment substance use is linked to reductions in violence (Walton et al., 2002, O’Farrell and Fals-Stewart, 2000; O’Farrell and Murphy, 1995; O’Farrell et al., 2003), that interventions based on cognitive and behavioral strategies (e.g., BCT) can impact both substance use and violence, and that treatment of psychiatric disorders appears related to reduced violence (Fava, 1998; Swartz et al., 1998a; 1998b; Swanson et al., 1997). A recent study found that for patients admitted to a hospital for violence related injuries, an intervention including extensive outpatient follow-up, psychotherapy and assistance with SUD treatment resulted in significantly reduced likelihood of further arrests and convictions for violent crimes compared to standard care conditions (Cooper et al., 2007). Further, evidence suggests that treatment engagement/ retention and compliance is related to improved violence outcomes. Specifically, studies of SUD and domestic violence samples have suggested that retention in such treatment appears linked to reductions in violence (Gondolf and Jones, 2001; O’Farrell et al., 2004), and studies of those with comorbid psychiatric disorders and substance misuse have found that compliance with psychiatric interventions appears related to reductions in violence (Swartz et al., 1998). Additionally, O’Farrell et al. (2004) have found that treatment engagement/retention is an important mediator of the impact of BCT on violence and substance use outcomes. It is possible that interventions demonstrated to impact treatment engagement, retention and/or compliance, such as those based on Motivational Interviewing (Dunn et al., 2001; Miller and Rollnick,, 2002) could have a role in programming designed to impact interpersonal violence.
The present study was designed to identify potential treatment needs of men and women in SUD treatment, and to examine for potential differences according to violence typologies. Additionally, we looked for potential differences based upon the role of the participant in aggressive incidents. More specifically, based on violence resulting in injury towards partners and non-partners, participants were categorized into four groups (no injury - NI, partner injury only - PIO, non-partner injury only – N-PIO, both partner and non-partner injury - BI). Similar categorizations were made for violence directed towards the participant (no injury – NI), injury by partner only (IPO), injury by non-partner only (IN-PO), and injured by both partners and non-partners (IB). This study focused on violence resulting in injury due to our desire to focus on severe forms of aggression, and because findings from prior studies suggest that it is important to measure injury to better identify potential gender differences in violence (Cantos et al., 1994; Cascardi et al., 1992; Hamby, 2005). Analyses examined differences among the groups in terms of demographics and clinical presenting characteristics (history of reported mental health problems, recent problems with depressive symptoms, and alcohol and other drug use) that have been linked to violence. Based on prior findings (Chermack et al., 2001; Huss and Langhinrichsen-Rohling, 2006), it was hypothesized that participants reporting both partner and non-partner violence would have the most severe substance use and psychiatric problems and were more likely to be males, and that those reporting partner violence only would be most similar to those reporting no violence resulting in injury. Finally, it was hypothesized that female participants would be more likely to report being injured only by a partner. This study provides important information regarding factors associated with violence groups that has implications for development and implementation of assessment and intervention strategies targeting violence among men and women in treatment for SUDs. Further, based on an integration of the present findings with other research, a conceptual model of treatment needs and approaches will be described.
Methods
Procedure
Participants entering treatment in a variety of SUD programs (community residential centers, intensive outpatient, and regular outpatient treatment programs) were approached about participation in the present study. Participants were screened within the first 2 weeks of treatment to take part in a randomized controlled trial pilot study of a six session violence prevention intervention. For the larger study, inclusion criteria included having a positive history for past year violence. Data used for the present study was collected during the screening process for inclusion in the larger clinical trial, and thus, includes those with and without past year violence. Participants received ten dollars compensation for time spent completing the study screen which consisted of brief measures of demographics, abuse history, family history variables, psychiatric symptoms, alcohol and drug use, and a modified version of the CTS-2. About 95 % of those approached about the study provided informed consent to participate in the screening and larger intervention study.
Participants
Participants were 489 men (76.1%) and women (23.9%) currently seeking treatment for a substance use disorder (SUD). Most participants were from residential treatment programs (64.4%) with slightly over a third from outpatient treatment programs (35.3%). The average age was 35.9 (SD = 10.8), with a range of 18 to 63 years. The ethnicity of the sample was 54.4% Caucasian, 35.4% African American, 3.9% Native-American, 2.5% Hispanic, and 3.9% other ethnicities. Most of the participants were single and never married (46.3%) with 9.5% married, 4.8% separated, 17.9% divorced, 1.3% widowed, and 9.5% living with a significant other. About seven percent (6.7%) of participants had less than an eighth grade education, 38.7% had some high school education (but did not graduate) high school, 26.2% graduated from high school, 23.9% attended college, and 4.3% graduated from college.
Measures
Violence in Partner and Non-Partner Relationships
For the year prior to treatment, physical violence was assessed with a modified version of the Revised Conflict Tactics Scale (CTS-2; Straus, Hamby, Boney-McCoy, and Sugarman, 1996). The CTS was based on the assumption that various tactics (including violence) may be used to deal with the inherent conflict in life. The revision of the CTS added items to the original scales, added new scales, and provided a simpler response format. Thus, the CTS-2 is a widely used measure which provides information on expressed and received negotiation, psychological abuse, physical abuse, sexual coercion, and injury. The CTS-2 has been shown to have good internal consistency and has been well validated (Simpson and Christensen, 2005). In the present study, a modification was made so that each participant indicated expressed and received abuse and injury related to intimate partners, and then completed the same items regarding non-partner conflict. For the purposes of the present study, the injury scales were utilized in the formation of violence groups. Thus, to examine factors related to participants injuring others, scores on the participant-to-partner and participant-to-non-partners injury scales were dichotomized to reflect whether the participant had injured their partner (or someone else for non-partner scale score) in the past year. Next, scores on the participant-to-partner violence and participant-to-non-partner violence scales were then combined to form 4 groups: No injury (NI), partner injury only (PIO), non-partner injury only (N-PIO), and both partner and non-partner injury (BI). Similarly, to examine factors related to participants being injured by others, scores on the non-partner-to-participant injury scales were dichotomized to reflect whether the participant had been injured their partner (or someone else for non-partner scale score) in the past year. Scores on the partner-to-participant violence and non-partner-to-participant violence scales were then combined to form 4 groups: No injury (NI), injury by partner only (IPO), injury by non-partner only (IN-PO), and injured by both partners and non-partners (IB).
Alcohol and drug consumption
The University of Arkansas Substance Abuse Outcomes Module (SAOM; Smith et al., 1996) was used to assess alcohol and drug use for the 28 days prior to entering treatment. The number of days of alcohol use and the number of days involving binge drinking (more than five drinks consumed) were assessed for alcohol use. Drug use was assessed by having participants indicate the number of days that they used marijuana, cocaine, stimulants (unprescribed), opiates (unprescribed), sedatives (unprescribed), heroin. The SAOM has good psychometric properties including internal consistency (Chermack et al., 2000), testretest reliability (Smith et al., 2006), and concurrent validity with widely used substance use measures such as the Addiction Severity Index (McLellan et al., 1992).
Depression
Evidence of depression was assessed using the Patient Health Questionnaire (PHQ-9; Spitzer, Kroenke, and Williams, 1999). The PHQ-9 is a 9 item questionnaire frequently used by primary care physicians to assess patient depression severity. It has been shown to have adequate reliability and validity (Kroenke, Spitzer, and Williams, 2001; Lowe et al., 2004). The nine items of the PHQ-9 reflect the DSM-IV criteria for a Major Depressive Disorder (MDD) and the suggested cutoff score of 10 was used to indicate evidence of depression. This cutoff score has been found to have high sensitivity and specificity (88% for each) for MDD (Kroenke et al., 2001).
Mental Health History
To assess for mental health history, participants were asked to indicate if the had ever been told by a psychiatrist, other doctor, or other behavioral health professional that they had an emotional or substance use disorder. Participants indicating that they had been told this, were then asked to indicate which problem was mentioned from a list of 17 possible disorders including alcohol abuse/dependence, heroin abuse/dependence, marijuana abuse/dependence, cocaine abuse/dependence, schizophrenia, depression, bipolar disorder/manic depression, post traumatic stress disorder (PTSD), panic disorder, and others. These items provide information regarding the extent to which participants may have received psychiatric diagnoses by healthcare providers, and may provide some indication of the general nature of their psychiatric problems.
Other Participant Characteristics
Numerous demographic characteristics of the sample were assessed by participant self-report including age, gender, and employment status (employed or not). Participants rated their annual gross income level on a 6 point scale ranging from less than $10,000 to $80,000 or more, midpoints of the categories were used for descriptive purposes. Race was assessed using 7 categories, but due to sample characteristics, was recoded to reflect White/Caucasian and of other racial group for the present study. Similarly, high school education was assessed on a six-point scale, but recoded to reflect either up to a high school education or more than a high school education. Additionally, participants were asked to indicate whether or not they lived with their intimate partner, had health insurance (including Medicare, Medicaid or other public medical assistance) had previously attended an anger management program, and were on parole or probation. To assess prior treatment history, participants were asked how often in the past 5 years they had been hospitalized for mental health reasons and asked similarly for substance use reasons. Number of outpatient mental health and substance use sessions received over the past 2 years were assessed on a 5 point scale ranging from 0 to 26 or more sessions, and data were recoded to reflect midpoints of these categories.
Data Analysis
It was elected to examine participant-to-others injury groups and others-to-participants injury groups in separate analyses given that they were strongly related to each other (Spearman = .87, p < .001). The same analysis strategy was used to examine factors related to participant-to-others injury groups, as well as factors related to others-to-participants injury groups. Specifically, the relationship between injury groups and participant variables (age; gender; race; living with partner; health insurance; on parole/probation; prior anger management; employment; income; prior mental health and substance use treatment; binge drinking; marijuana, cocaine, stimulant, sedative, heroin, and opiate use; history of alcohol, heroin, marijuana, or cocaine problem; history of schizophrenia, depression, bipolar/manic depression, PTSD, and panic disorder; and evidence of depression) was calculated using chi-square analyses for discrete variables and ANOVA’s with post hoc analyses using Tukey’s HSD for continuous variables. Next, multinomial logistic regression analyses were used to examine the predictors of violence groups. For these models (one focusing on predictors of participants injuring others, one focusing on predicting participants being injured by others), age, gender and race were included, as well as variables with significant bivariate relationships to the respective violence groups.
Results
Analyses focusing of variables related to Participant-to-Others injury groups
In terms of the violence groups, 45.2% were in the “no injury” group (NI), 8.2% in the “partner injury only” group (PIO), 22.3% in the non-partner injury only group (N-PIO), and 24.3% were in the “both partner and non-partner” injury group (BI). Analyses examining group differences in participant factors are displayed in Table 1. In regards to participant characteristics, significant differences were found with regard to age, gender, living with partner, health insurance, treatment program type (outpatient vs. residential), parole/probation status, and prior anger management/domestic violence treatment. Significant differences were also found for evidence of recent depression; binge drinking; and marijuana, cocaine, sedative, and opiate use, as well as being told by health care providers of having alcohol abuse/dependence, cocaine abuse/dependence, schizophrenia, bipolar disorder, and panic disorder. The groups did not differ in race, income, employment, stimulant or heroin use, prior mental health and substance use disorder treatment, or in having been told by healthcare providers of having heroin abuse/dependence, marijuana abuse/dependence, depression, and PTSD. Overall, the sample the sample appeared to have significant psychosocial challenges in terms of low rates of employment and having healthcare insurance, low household income, relatively few prior SUD treatment visits on average, high levels of legal involvement, and most participants did not have prior “anger-management/domestic violence” treatment. Further, the majority in each group (including the “partner injury” only group) were not presently married or living with a partner.
Table 1.
Bivariate differences between participant to others injury groups
| Variable | No injury (NI) (n=221) % or mean (sd) | Partner Injury only (PIO) (n = 40) % or mean (sd) | Non-partner Injury only (N-PIO) (n = 109) % or mean (sd) | Both Partner and Non-partner Injury (BI) (n = 119) % or mean (sd) | P value |
|---|---|---|---|---|---|
| Participant characteristics: | |||||
| Age | 37.7 (11.0)ab | 38.2 (9.7)b | 34.0 (11.0)ab | 33.5 (10.1)a | .001 |
| Male | 77.6% | 60.0% | 73.1% | 81.5% | .038 |
| Employed | 16.7% | 20.0% | 15.6% | 16.8% | .939 |
| Income | 20,868 (18,297) | 18,461 (16,390) | 21,806 (19,568) | 17,627 (14,288) | .251 |
| High school education or less | 71.9% | 67.5% | 67.9% | 75.6% | .566 |
| Live in spouse/partner | 24.9% | 45.0% | 26.6% | 21.0% | .027 |
| Caucasian race | 56.6% | 42.5% | 58.7% | 50.4% | .233 |
| Have health insurance | 50.2% | 77.5% | 49.5% | 48.7% | .009 |
| On Parole/Probation | 72.4% | 59.0% | 78.0% | 84.0% | .008 |
| Prior Anger Management | 26.8% | 46.2% | 38.5% | 62.2% | .000 |
| Treatment Type (% residential) | 68% | 55% | 71% | 85% | .001 |
| Inpatient mental health admissions | .6 (1.6) | 1.0 (1.4) | .9 (2.7) | .6 (1.3) | .324 |
| Inpatient substance use admissions | 1.5 (2.5) | 1.6 (1.9) | 1.4 (2.2) | 1.6 (1.9) | .944 |
| Outpatient mental health visits | 4.1 (7.3) | 4.1 (5.9) | 5.3 (8.6) | 4.6 (7.5) | .596 |
| Outpatient substance use visits | 6.0 (7.8) | 6.7 (7.9) | 7.6 (9.4) | 6.9 (8.4) | .431 |
|
| |||||
| Recent substance use and Depression Symptoms: | |||||
| Binge drinking | 4.9 (8.4)a | 5.4 (8.8)a | 8.3 (9.9)ab | 10.1 (10.2)b | .000 |
| Marijuana use | 4.3 (8.6)a | 4.4 (8.9)a | 5.9 (10.1)ab | 9.1 (11.6)b | .000 |
| Cocaine use | 5.4 (8.7)a | 10.4 (10.8)b | 7.4 (10.4)ab | 10.6 (11.1)b | .000 |
| Illicit Stimulant use | 0.3 (1.9) | 1.2 (5.4) | 0.7 (3.1) | 1.2 (4.5) | .124 |
| Illicit Sedative use | .7 (4.1)ab | .4 (2.4)a | 1.2 (4.5)ab | 2.4 (6.4)b | .010 |
| Heroin use | 2.3 (7.2) | 1.6 (5.7) | 3.2 (8.2) | 3.6 (8.9) | .350 |
| Illicit Opiate use | 1.2 (5.1) | 1.1 (4.3) | 2.0 (5.9) | 3.1 (7.0) | .034 |
| Evidence of Depression: | 44.3% | 57.5% | 53.2% | 71.4% | .000 |
|
| |||||
| Previously told by professional they have: | |||||
| Alcohol Abuse/Dependence | 38.5% | 50.0% | 43.1% | 54.6% | .032 |
| Heroin Abuse/Dependence | 14.0% | 12.5% | 14.7% | 20.2% | .445 |
| Marijuana Abuse/Dependence | 24.9% | 27.5% | 26.6% | 37.8% | .083 |
| Cocaine Abuse/Dependence | 40.3% | 60.0% | 40.4% | 50.4% | .047 |
| Schizophrenia | 6.8% | 10.0% | .9% | 2.5% | .024 |
| Depression | 42.1% | 57.5% | 47.7% | 42.9% | .281 |
| Bipolar/Manic | 18.6% | 32.5% | 30.3% | 29.4% | .030 |
| PTSD | 4.5% | 7.5% | 8.3% | 8.4% | .435 |
| Panic Disorder | 7.2% | 15.0% | 16.5% | 7.6% | .031 |
Note.
Same superscript indicates that group means were not significantly different at α = .05.
Multinomial logistic regression results are listed in Table 2. Results indicate that those in the PIO group were more likely to be living with their partner, have health insurance, and have prior anger management treatment than those in the no-injury group. Individuals in the N-PIO group were younger, less likely to report having been told they have schizophrenia, more likely to have a history of being told they have Bipolar or Panic disorder, and binge drank more frequently than those in the NI group. Finally, those in the BI group were more likely to be men, younger, a member of a racial minority, recruited from residential treatment, depressed, more frequent binge drinkers and cocaine users, but were less likely to report being told they have schizophrenia than NI participants.
Table 2.
Multinomial logistic regression results (Odds ratios and 95% Confidence Intervals) examining predictors of participant to others injury groupsa
| Partner Injury only (PIO) OR (CI) |
Non-partner Injury only (N-PIO) OR (CI) |
Both Partner and Non-partner Injury (BI) OR (CI) |
|
|---|---|---|---|
| Age | 0.98 (0.95 – 1.02) | 0.96 (0.94 – 0.99)*** | 0.95 (0.92 – 0.98)*** |
| Male Gender | 0.59 (0.24 – 1.45) | 1.13 (0.58 – 2.19) | 2.33 (1.09 – 4.95)* |
| Race | 2.00 (0.90 – 4.44) | 1.36 (0.80 – 2.32) | 1.88 (1.06 – 3.32)* |
| Live with spouse/partner | 2.42 (1.11 – 5.28)* | 0.96 (0.54 – 1.69) | 0.77 (0.41 – 1.46) |
| Health Insurance | 3.24 (1.32 – 7.94)** | 1.14 (0.67 – 1.95) | 1.20 (0.68 – 2.11) |
| Treatment Type | 0.78 (0.27 – 2.25) | 1.05 (0.51 – 2.18) | 3.17 (1.34 -- 7.50)** |
| Alcohol Abuse/Dependence | 1.25 (0.55 – 2.84) | 1.01 (0.57 – 1.77) | 1.28 (0.71 – 2.34) |
| Cocaine Abuse/Dependence | 1.25 (0.52 – 3.00) | 0.97 (0.53 – 1.78) | 1.06 (0.56 – 2.00) |
| Schizophrenia | 0.53 (0.13 – 2.28) | 0.07 (0.01 – 0.62)* | 0.14 (0.03 – 0.66)* |
| Bipolar | 1.12 (0.46 – 2.77) | 1.97 (1.04 – 3.75)* | 1.72 (0.88 – 3.38) |
| Panic Disorder | 2.06 (0.61 – 6.97) | 2.85 (1.18 – 6.91)* | 0.86 (0.30 – 2.50) |
| Parole/Probation | 1.15 (0.37 – 3.54) | 1.58 (0.71 – 3.51) | 0.94 (0.39 – 2.27) |
| Binge drinking | 1.01 (0.96 – 1.06) | 1.04 (1.01 – 1.07)** | 1.04 (1.01 – 1.07)** |
| Marijuana use | 0.98 (0.93 – 1.02) | 0.99 (0.97 – 1.02) | 1.01 (0.98 – 1.04) |
| Cocaine use | 1.03 (0.98 – 1.07) | 1.03 (1.00 – 1.06) | 1.05 (1.02 – 1.08)** |
| Sedative use | 0.95 (0.81 – 1.11) | 1.00 (0.93 – 1.07) | 1.03 (0.96 – 1.11) |
| Opiate use | 0.98 (0.89 – 1.07) | 1.00 (0.94 – 1.06) | 1.01 (0.94 – 1.07) |
| Evidence of depression | 1.25 (0.56 – 2.78) | 1.04 (0.59 – 1.82) | 2.78 (1.53 – 5.04)** |
| Prior Anger Management | 2.47 (1.15 – 5.33)* | 1.62 (0.94 – 2.77) | 3.67 (2.11 – 6.39)*** |
Note. Model Chi-Square (57 df) = 195.55, p < .001
indicates p ≤ .05,
indicates p≤.01,
indicates p≤ .001
The reference group for the violence group outcomes was the NI group.
Analyses focusing of variables related to Others-to-Participant injury groups
In terms of the violence groups, 44.6% were in the “no injury” group (NI), 9% in the “injured by partner only” group (IPO), 22.9% in the injured by non-partner only group (IN-PO), and 23.5% were in the injured by “both partner and non-partner” group (IB). Analyses examining group differences in participant factors are displayed in Table 3. In regards to participant characteristics, significant differences were found with regard to age, gender, race, living with a partner, health insurance, treatment program type, parole/probation status, and prior anger management/domestic violence treatment. Significant differences were also found for evidence of recent depression; binge drinking; and marijuana, cocaine, sedative, and opiate use, as well as being told by health care providers of having marijuana abuse/dependence and bipolar disorder. The groups did not differ in income, employment, stimulant or heroin use, prior mental health and substance use disorder treatment, or in having been told by healthcare providers of having heroin abuse/dependence, alcohol abuse/dependence, cocaine abuse/dependence, depression, schizophrenia and PTSD.
Table 3.
Bivariate differences between others-to-participants injury groups
| Variable | No injury (NI) (n=218) % or mean (sd) | Injury by partner only (IPO) (n = 44) % or mean (sd) | Injury by Non- partner only (IN-PO) (n = 112) % or mean (sd) | Injury by Both Partner and Non-partner (IB) (n = 115) % or mean (sd) | P value |
|---|---|---|---|---|---|
| Participant characteristics: | |||||
| Age | 38.0 (10.6)a | 35.1 (10.4)ab | 34.9 (11.5)ab | 33.1 (10.0)b | .001 |
| Male | 78.7% | 47.7% | 80.2% | 78.3% | .000 |
| Employed | 17.0% | 18.2% | 16.1% | 16.5% | .990 |
| Income | 21,170 (19,107) | 18,605 (15,672) | 21,727 (18,725) | 16,99 (13305) | .133 |
| High school education or less | 71.6% | 68.2% | 67.9% | 75.6% | .50 |
| Live in spouse/partner | 24.8% | 43.2% | 25.0% | 22.6% | .053 |
| Caucasian race | 55.0% | 50.0% | 58.9% | 50.4% | .565 |
| Have health insurance | 52.3% | 70.5% | 45.5% | 50.4% | .046 |
| On Parole/Probation | 72.0% | 62.8% | 83.0% | 79.1% | .024 |
| Prior Anger Management | 26.3% | 41.9% | 44.6% | 59.1% | .000 |
| Treatment Type (% residential) | 67.7% | 59.1% | 76.6% | 78.3% | .032 |
| Inpatient mental health admissions | .7 (2.3) | .9 (1.4) | .7 (1.2) | .6 (1.4) | .833 |
| Inpatient substance use admissions | 1.5 (2.6) | 1.6 (1.9) | 1.5 (1.9) | 1.6 (2.0) | .987 |
| Outpatient mental health visits | 4.0 (7.1) | 4.2 (6.2) | 5.7 (8.8) | 4.5 (7.5) | .268 |
| Outpatient substance use visits | 6.1 (7.9) | 6.3 (7.9) | 8.1 (9.6) | 6.3 (8.0) | .190 |
|
| |||||
| Recent substance use and Depression Symptoms: | |||||
| Binge drinking | 4.5 (8.1)a | 8.5 (10.6)b | 7.3 (9.2)ab | 10.7 (10.4)b | .000 |
| Marijuana use | 4.2 (8.6)a | 5.9 (8.9)ab | 6.4 (10.7)ab | 8.5 (11.3)b | .002 |
| Cocaine use | 5.9 (9.2)a | 9.2 (10.1)ab | 6.9 (9.6)ab | 10.5 (11.4)b | .001 |
| Illicit Stimulant use | 0.4 (2.6) | 0.7 (3.2) | 0.6 (2.4) | 1.4 (4.9) | .091 |
| Illicit Sedative use | 0.8 (4.1) | 0.7 (2.7) | 1.0 (3.6) | 2.5 (6.9) | .009 |
| Heroin use | 2.4 (7.3) | 1.2 (5.1) | 3.2 (8.4) | 3.6 (8.8) | .275 |
| Illicit Opiate use | 1.0 (4.7)a | 3.4 (7.4)ab | 1.8 (5.3)ab | 2.9 (7.0)b | .007 |
| Evidence of Depression: | 45.0% | 61.4% | 55.4% | 67.0% | .001 |
|
| |||||
| Previously told by professional they have: | |||||
| Alcohol Abuse/Dependence | 39.0% | 47.7% | 49.1% | 48.7% | .200 |
| Heroin Abuse/Dependence | 15.1% | 9.1% | 17.0% | 17.4% | .595 |
| Marijuana Abuse/Dependence | 22.5% | 31.8% | 29.5% | 38.3% | .023 |
| Cocaine Abuse/Dependence | 42.7% | 50.0% | 45.5% | 44.3% | .829 |
| Schizophrenia | 6.4% | 9.1% | 1.8% | 2.6% | .087 |
| Depression | 41.3% | 56.8% | 47.3% | 44.3% | .266 |
| Bipolar/Manic | 18.8% | 34.1% | 30.4% | 27.8% | .035 |
| PTSD | 5.0% | 6.8% | 6.3% | 9.6% | .469 |
| Panic Disorder | 7.3% | 15.9% | 13.4% | 9.6% | .182 |
Note.
Same superscript indicates that group means were not significantly different at α = .05.
Multinomial logistic regression results are listed in Table 4. Results indicate that those in the IPO group were older, less likely to be men (more likely to be women), more likely to be living with their partner, with more frequent binge drinking and illicit opiate use those in the no-injury group. Individuals in the IN-PO group were younger, more likely to have a history of being told they have Bipolar, a history of prior anger-management treatment, and binge drank more frequently than those in the NI group. Finally, those in the IB group were younger, more frequent binge drinkers and cocaine users, more likely to be depressed, and to have a history of anger-management treatment than NI participants.
Table 4.
Multinomial logistic regression results (Odds ratios and 95% Confidence Intervals) examining predictors of others-to-participant injury groupsa
| Injury by Partner only (IPO) OR (CI) |
Injury by Non-partner only (IN-PO) OR (CI) |
Injury by Both Partner and Non-partner (IB) OR (CI) |
|
|---|---|---|---|
| Age | 0.96 (0.92 – 0.99)* | 0.97 (0.94 – 0.99)** | 0.94 (0.92 – 0.97)*** |
| Male Gender | 0.30 (0.13 – 0.70)** | 1.18 (0.60 – 2.31) | 1.45 (0.71 – 2.96) |
| Race | 1.91 (0.89 – 4.13) | 1.09 (0.65 – 1.83) | 1.71 (0.98 – 2.98) |
| Live with spouse/partner | 2.34 (1.10 – 4.96)* | 1.07 (0.61 – 1.89) | 0.89 (0.48 – 1.64) |
| Health Insurance | 1.89 (0.85 – 4.20) | 0.86 (0.52 – 1.44) | 0.95 (0.55 – 1.64) |
| Treatment Type | 0.74 (0.42 – 3.35) | 1.30 (0.63 – 2.67) | 1.75 (0.79 – 3.88) |
| Marij. Abuse/Dependence | 1.27 (0.52 – 3.04) | 1.10 (0.59 – 2.05) | 1.29 (0.68 – 2.45) |
| Bipolar | 1.37 (0.59 – 3.16) | 1.99 (1.08 – 3.64)* | 1.34 (0.70 – 2.58) |
| Parole/Probation | 1.05 (0.36 – 3.11) | 1.55 (0.69 – 3.46) | 0.88 (0.38 – 2.05) |
| Binge drinking | 1.06 (1.02 – 1.10)** | 1.04 (1.01 – 1.07)* | 1.07 (1.04 – 1.10)*** |
| Marijuana use | 0.99 (0.95 – 1.03) | 1.00 (0.97 – 1.03) | 1.00 (0.97 – 1.03) |
| Cocaine use | 1.00 (0.97 – 1.04) | 1.01 (0.99 – 1.04) | 1.04 (1.01 – 1.07)** |
| Sedative use | 0.91 (0.81 – 1.02) | 0.98 (0.91 – 1.06) | 1.03 (0.95 – 1.10) |
| Opiate use | 1.08 (1.01 – 1.15)* | 1.02 (0.96 – 1.09) | 1.01 (0.95 – 1.08) |
| Evidence of depression | 1.25 (0.53 – 2.58) | 1.25 (0.73 – 2.14) | 1.98 (1.11 – 3.53)* |
| Prior Anger Management | 1.83 (0.86 – 3.91) | 1.93 (1.15 – 3.25)* | 3.34 (1.94 – 5.77)*** |
Note. Model Chi-Square (48 df) = 159.85, p < .001
indicates p ≤ .05,
indicates p≤.01,
indicates p≤ .001
The reference group for the violence group outcomes was the NI group.
Discussion
The present findings reveal high rates of men and women reporting violence resulting in injury to others across relationship types (~54.8%), and that partner only violence resulting in injury was less common than injuring non-partners or injuring both partners and non-partners. Similar rates were found for participants being injured across relationship types (~55.4%), with injuries by partner only being less common than by non-partners or both. Further, there was a strong association between injuring others and being injured. One obvious implication of these findings is the need to establish more thorough assessment protocols of interpersonal violence that include information regarding injury and violence in both partner and non-partner relationships. These findings also highlight the need for intervention approaches targeting factors related to more general violence involvement (in addition to interventions such as BCT). According to bivariate analyses, those in the BI and IB groups tended to have the highest levels of substance use and depressive symptoms. For many variables, the injury groups had higher rates of problems (e.g., binge drinking, cocaine use, marijuana use, evidence of depression, being told by healthcare providers that they have bi-polar disorder) than the NI groups. Those in the partner only groups had higher rates of living with a spouse/partner, having healthcare insurance, a higher percentage of women, lower rates of being on parole/probation, and were most similar to the respective NI groups on several measures.
In terms of multivariate findings regarding participants injuring others, factors distinguishing the PIO group from the NI group were presence of healthcare insurance, presently living with a partner, and a history of prior anger-management/domestic violence treatment. For the N-PIO, younger age and binge drinking were significant; there was an increased likelihood of a history being told by a provider that they have bipolar disorder and panic disorder, and a decreased likelihood of reporting a history of schizophrenia. Finally, for the BI group, younger age, male gender, being of minority status, binge drinking, cocaine use, recent depression symptoms and a history of prior anger-management/domestic violence treatment were significant.
With respect to participants being injured, factors distinguishing the IPO group from the NI group were somewhat different (more significant predictors) from what was found for the analyses of participants injuring others. For the IPO group, younger age, female gender, presently living with spouse/partner, binge drinking, and opiate use were significant. For the IN-PO group, younger age, binge drinking, being on parole/probation, and having a previous history of anger management/ domestic violence treatment were significant, and participants in this group also had an increased likelihood of reporting they had been told by a healthcare professional that they had bipolar disorder. Participants in the IB group were more likely to be younger, engaged in binge drinking and cocaine use, had recent depression symptoms, and a history of prior anger management/domestic violence treatment. Overall, younger age and greater binge drinking were the only variables related to being in each of the injury by others groups.
The findings reveal participants with a history of injuring others and/or being injured by others have more serious problems than those without such histories. In terms of injuring others, those in the N-PIO and BI groups had the most variables distinguishing them from those without a history of violence resulting in injury, and analyses focusing on being injured by others illustrated that women were more likely to be in injured by partner only group. These findings appear consistent with other samples in that the more “generalized” aggressors appear to have the greatest overall clinical problem severity, and that women are more likely to be injured by their partner only (Holtzworth-Munroe and Meehan, 2004; Huss and Langhinrichsen-Rohling, 2006; Walton et al., 2007). Further, although there was a strong association between injuring others and being injured (r = .87), the pattern of factors associated with the respective risk groups was somewhat different. Overall, the high rates of non-partner and “generalized” violence, as well as the pattern of results clearly indicate a need for violence prevention treatment approaches in addition to BCT and those targeting only intimate partner violence.
A Conceptual Model of Violence Risk Factors and Treatment Needs: Motivational Enhancement Approaches, Cognitive Behavioral Approaches and Problem Service Matching
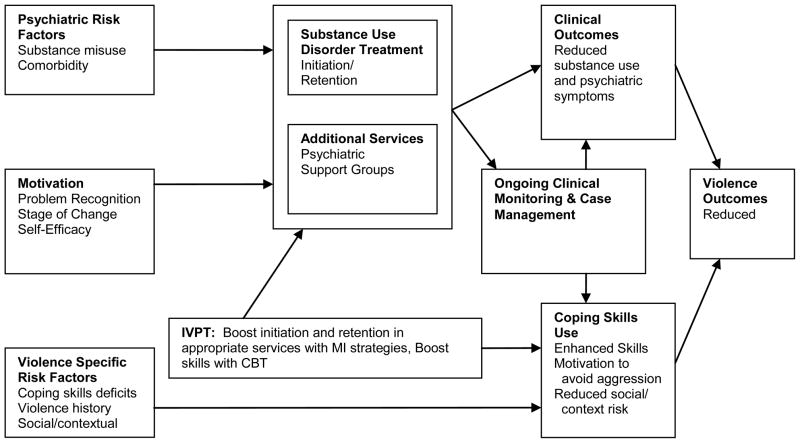
Figure 2 displays a conceptual model of violence risk factors and treatment needs for SUD treatment populations. The model is designed to highlight clinical need areas (substance use and psychiatric problems; motivational issues and violence specific risk factors), the role of general treatment interventions (substance use disorder and psychiatric), “integrated violence prevention treatment” (IVPT) approaches, and factors related to reductions in violence (reduced substance use and psychiatric problems, increased motivation to avoid violence consequences, enhanced coping skills). The model also integrates key aspects related to treatment engagement/involvement (motivation, accessibility/availability of needed interventions), participant need characteristics (coping skills deficits, untreated substance misuse and psychopathology), and other factors potentially related to substance misuse and violence outcomes (social/contextual factors, continued clinical monitoring and case management) (Aday and Anderson, 1974; Anderson, 1995; Chermack et al., 1997; O’Farrell et al., 2004; Scott & Dennis, 2003; Scott, Dennis, & Foss, 2005). Thus, it is proposed that to reduce violence risk for men and women in SUD treatment, there are important roles for interventions that facilitate motivation and treatment engagement and retention, treatment interventions addressing substance use and psychiatric issues, and interventions targeting specific violence risk factors (e.g., coping skills deficits). More specifically, the figure suggests there is a role for an “Integrated Violence Prevention Treatment” (IVPT) model involving the integration of motivational enhancement approaches, CBT targeting violence specific risk factors, the principal of problem-service matching in SUD treatment, and ongoing clinical monitoring and case-management.
Figure 2.
Model of violence risk factors and the role of IVPT
Scientific Basis for Integrated Violence Prevention Treatment (IVPT)
The importance of motivation in SUD treatment and partner violence intervention has been documented in several studies. For example, in a large naturalistic study of SUD treatment outcomes (N=5037), Joe and colleagues (1998) found pre-treatment motivation was related to retention in treatment, and De Leon (1996) found that initial motivation appeared as a significant predictor of treatment retention across populations of primary alcohol, marijuana, heroin, cocaine, and crack cocaine users. In another study, higher motivation for treatment was associated with twofold increases in the likelihood of having favorable follow-up outcomes on alcohol use, illicit drug use, and criminal involvement (Simpson, Joe, and Rowan-Szal, 1997). Pretreatment motivation measured at intake has also been shown to be related to greater treatment engagement (Joe et al., 1998). Interventions based on motivational interviewing (“Adapted Motivational Interviewing” – AMI) have been demonstrated to increase follow-through with referrals for SUD treatment, and subsequent treatment retention and outcome. For example, a review by Dunn, Deroo, and Rivara (2001) found that AMI interventions have their greatest impact on enhancing entry into and retention in SUD treatment. A separate review supports the effectiveness of interventions based on motivational interviewing with regard to substance use and other target behaviors (Burke, 2002). Finally, participant’s high in anger benefited most from an AMI intervention (MET) in terms of alcohol use outcomes in Project MATCH (1997), and recent findings demonstrate that motivation to change is related to treatment outcome for men in abuser intervention programs (Scott and Wolfe, 2003). These findings suggest that motivational enhancement approaches have a role in impacting factors related to violence risk through boosting treatment engagement and compliance with regard to SUD and psychiatric issues, and/or increasing motivation to use skills to prevent violence and its associated consequences. Further, given evidence that “general” aggressors appear more likely to drop out of treatment (Stalans and Seng, 2007), AMI or other treatment engagement interventions may be particularly important for those reporting violence in non-partner or both partner and non-partner violence.
Although the impact of BCT has been well established, there has been a paucity of research examining other CBT violence prevention interventions in SUD treatment. Prior studies have had significant limitations, including the lack of a randomized controlled designs, measures of behavioral aggression, and longitudinal post-treatment assessments. Nevertheless, there is some evidence to support the effectiveness of CBT in reducing problems related to anger and aggression. The results of meta-analyses and reviews support CBT strategies for non-SUD samples, including cognitive restructuring, problem solving, relaxation training, anger management and communication skills focused approaches (Beck and Fernandez, 1998; Edmondson and Conger, 1996).
In terms of problem service matching, as noted by McLellan et al. (1997) supplemental treatment services matched to client problems enhances overall treatment outcome (McLellan, et al., 1997). Consistent with the problem service matching model, there is evidence that treatment of psychiatric disorders appears related to reduced violence (Fava, 1998; Swartz et al., 1998a; 1998b; Swanson et al., 1997). There also is some evidence that anger management delivered as a supplement to treatment for cocaine problems reduced anger and improved anger control (Reilly and Shopshire, 2000). Further, the intervention approach described by Cooper et al. (2007) for patients admitted to a hospital for violent injuries appeared to apply a problem-service model along with ongoing monitoring and case-management, in that the intervention consisted of extensive outpatient follow-up, case-management, individual and/or group psychotherapy and assistance with SUD treatment if indicated.
Within the last decade, new clinical paradigms for SUD treatment have involved the principle of tailoring aspects of treatment to the needs of the individual client in domains related not only to substance abuse but to overall psychiatric and physical health, appropriate treatment placement (e.g., residential versus intensive outpatient), and monitoring of progress during and after treatment (Alexander et al., 2008, McLellan et al., 2005). We would argue that treatment tailoring (including ongoing monitoring and case management services) may be especially important for individuals presenting with violence problems given their greater overall clinical problem severity (e.g., alcohol and drug problem severity, high risk for relapse, psychiatric comorbidity, involvement with the justice system) and substantial psychosocial needs (e.g., unemployment, housing instability, lack of financial and healthcare resources).
Options to help provide and increase overall ongoing psychosocial support for these individuals may include the use of recovery management checkup (RMC) or case management (CM) services. RMC works under the supposition that a proportion of individuals who have been in SUD treatment will relapse and need services once again (Dennis, Scott, and Funk, 2003); therefore, the RMC model provides “managers” who meet with SUD clients on a regular basis after discharge from treatment to help monitor slippage (Scott, Dennis, and Foss, 2005). Evidence suggests that RMC, when compared to control conditions, leads to faster re-entry into treatment, longer retention in treatment, and decreased need for treatment over a two-year period (Dennis, Scott, and Funk, 2003; Scott, Dennis, and Foss, 2005). Similarly, CM can also provide services to facilitate such as facilitating medical and social service referrals and monitoring substance use upon release from treatment (McLellan et al., 1999). Although CM services has been found to improve post treatment outcomes (McLellan et al., 1999), less than half of nonresidential treatment facilities offer CM activities such as providing referrals for appropriate services outside of the SUD realm or following up on referrals when made (Alexander et al., 2008). Thus, CM and RMC can help facilitate a smoother transition from outpatient and/or residential services to community living by providing referrals and follow-up services for those identified as either having a history of such behavior or being at risk for violence.
It should be noted, however, that application of problem-service matching and ongoing monitoring with case management models face substantial challenges in terms of availability of appropriate and accessible services at the community level, coordination of services among different agencies, and billing and funding issues. Means of addressing such challenges are beyond the scope of this paper, but would appear to include improving training in both substance use disorder and psychiatric treatment, additional research identifying factors related to violence reduction (e.g., treatment approaches, health services delivery models), and translational and cost effectiveness research of approaches found to have an impact. Further, issues regarding billing and funding of appropriate services are critical to address, and this likely would include examining/revising public policy regarding treatment for substance use disorders, as well as issues related to both government and private health insurance funding of needed services. Despite such challenges, initiatives and research from correctional reintegration into the community programs offers some pertinent information regarding how to facilitate improved community functioning for high risk individuals. Reintegration programs rely on strong transitional programming, in which key figures are worked with who can help identify service needs upon discharge (e.g., housing, substance use treatment, medication) and ensure that barriers to treatment access (e.g., limited finances, lack of transportation or job skills) are limited (for a review, see Osher, Steadman, and Barr, 2003). Best practices indicate that a multitude of agencies need to be involved to help effect change, as relying solely on one practitioner or agency leaves too many opportunities for individuals to “fall through the cracks” (Wormith et al., 2007). This type of collaborative interface between multiple agencies may provide the best opportunity for SUD patients with violence histories to receive continuous care.
The conceptual model outlined in Figure 2 suggests a number of possibilities in terms of future research and clinical implementation of intervention approaches. For example, integrated violence prevention interventions could be implemented either as a supplement to standard SUD treatment for those men and women reporting problems with violence, or violence prevention strategies could be more heavily integrated into CBT oriented SUD treatment protocols. Future research could examine such issues, as well as whether individual or group approaches appear to have differential impact on violence outcomes. Further, it is possible that certain patient characteristics may have important implications in terms of interventions that have their greatest impact on violence risk. For example, “partner only” aggressors may benefit more from interventions targeting partner relationships (e.g., BCT), and individuals with psychiatric comorbidities may require treatment/stabilization of comorbid psychopathology. It is possible that at the individual level, factors such as violence prevention coping skills, attitudes towards violence and alcohol/drug use and intoxication effects, all also impact violence risk.
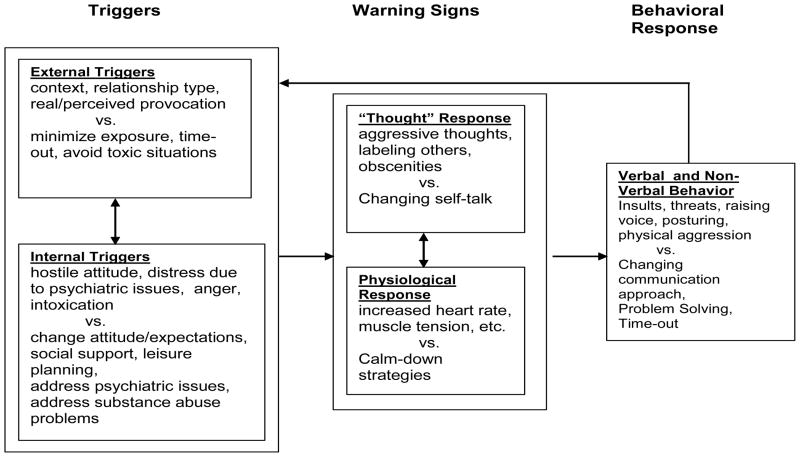
Figure 3 presents a heuristic model of the anger arousal/conflict escalation process, illustrating how specific therapeutic techniques can be used to target the aforementioned factors that impact violence risk. For example, the impact of “external triggers” (e.g., association with aggressive/angry people, buying/selling drugs, violent parts of their community) on violence risk may be reduced by avoiding or minimizing exposure to certain “triggers” (e.g, use of “time-out” approaches, disengaging from the drug subculture). For reactions to internal triggers (e.g., hostile attitude, aggressive self-talk, physiological arousal) skills such as changing attitudes, expectations, cognitions (“changing self-talk”), and/or the use of strategies to “calm” physiological and emotional arousal (distraction, relaxation, mindfulness, deep breathing, etc.) may help reduce violence risk. Finally, communication and collaborative problem solving approaches may be useful to address verbal and non-verbal behaviors that could contribute to conflict escalation.
Figure 3.
Cognitive Behavioral Framework: Matching coping options to different aspects
Thus, individuals reporting significant skills deficits or positive attitudes toward violence may require treatment directly addressing such issues, whereas as suggested by Fals-Stewart and Kennedy (2005) those whose violence is related to intoxication effects and/or immersment in a drug using sub-culture may benefit from completing standard SUD treatment. At the systems level, the model suggests that an array of intervention services appear needed to more realistically match interventions to common risk domains for men and women in SUD treatment. At present, unfortunately, most if not all of these issues discussed above (e.g., supplemental treatment sessions vs. integration in standard CBT SUD treatments, individual vs. group treatment, “matching” interventions/services to individual risk profiles, ongoing monitoring and case-management, etc.) remain to be studied systemically, much less implemented and available in clinical settings.
To summarize, our suggested IVPT model integrates information from research regarding factors related to violence risk, motivational enhancement interventions, CBT, problem-service matching and ongoing monitoring and case-management. Researchers have advocated the integration of motivational enhancement interventions and CBT strategies (Baer, Kivlahan, and Donovan, 1999; Barrowclough et al., 2001) for individuals with substance related problems, and Barrowclough et al. (2001) found that such an integrated approach produced significantly better outcomes for a sample with comorbid substance use problems and serious mental illness. It is suggested that early use of motivational enhancement strategies (AMI) could boost problem recognition and motivation to change, and be followed by CBT approaches, such as identifying and recognizing triggers for conflict/violence and developing new strategies to manage triggers more effectively. Given evidence of the effectiveness of AMI in improving treatment engagement/retention with SUD samples, reducing targeted problems (alcohol/drug use, medication non-compliane), CBT as a treatment for anger problems, the impact of matching treatment services to identified problems (McLellan et al., 1997), and research supporting ongoing monitoring and case-management services, application of an IVPT model could be expected to impact both substance use and violence outcomes.
While the present study provides important novel information regard violence across both partner and non-partner relationships in SUD settings, and factors associated with violence subgroups, the present study has a number of limitations. First, the data consisted exclusively of participant self-report information. Thus, there was no corroboration of measures of violence, substance use, or mental health history. However, we used several strategies to support self-report validity (e.g., use of psychometrically sound measures for substance use and violence, ensuring confidentiality of self-report information including obtaining a certificate of confidentiality). There is evidence to support validity of participants’ self-report of substance use in research studies and in samples of participants in the early phase of SUD treatment (e.g., Chermack et al., 1998; Chermack et al., 2000; Darke, 1998; O’Farrell et al., 2003). Moreover, when compared to community-based and forensic samples, accuracy of reports of violence may be somewhat higher in treatment samples (Panuzio et al., 2006). Clearly, our measures of past psychiatric history has questionable validity as diagnostic indicators given that it was based on participants’ recollections of being told about psychiatric diagnoses by healthcare providers. These items need to be interpreted with caution in that they are not based on structured clinical interviews, and could be influenced by the degree to which participants have previously engaged with behavioral healthcare providers. Thus, we do not feel that they accurately represent actual clinical diagnoses. Rather, these items provide some rough indication of the extent to which participants may have received psychiatric diagnoses, and the general nature of their psychiatric problems. Further, from a pragmatic clinical perspective, given that most SUD treatment settings do not include structured diagnostic interviews, it appears that even rough assessment of mental health history may provide some useful information regarding factors related to violence and/or participant clinical needs.
The present study also relied on a cross-sectional design. Although a number of findings (e.g., relationship of binge drinking and cocaine use to aggression) are consistent with methodologies that allow for inferring causation (e.g., experimental studies) (Chermack and Giancola, 1997; Licata et al., 1993), we are not able to make conclusions regarding causal relationships among variables. Further, our measure of violence (modified CTS-II) does not measure a number of important factors that may be related to our violence groups, such as motivational, emotional and social/contextual issues potentially associated with aggressive acts (e.g., establishing control, instigation of aggression, self-defense or retaliation, fear, setting of conflicts, reasons for aggression, escalatory processes). Finally, the sample for the present studies was selected from clinics in a single Midwestern state. Although rates of partner violence in this sample were similar to many prior studies (approximately 50%) (Chermack et al., in review; Fals-Stewart, Golden and Schumacher, 2003; O’Farrell and Murphy, 1995) it is possible that rates of violence in partner and non-partner relationships could differ in other samples or geographic regions. Nevertheless, the present findings do suggest the need for future studies to measure violence in non-partner relationships.
In conclusion, this study illustrated alarming rates of violence resulting in injury across groups. The findings indicate the need for interventions or models of care that address general violence. We have proposed that such interventions or models of care should involve the integration of interventions targeting motivation and treatment engagement (for substance use, psychiatric issues and violence specific risk factors), CBT for specific violence risk factors, problem-service matching (e.g., psychiatric care, case-management, employment) for other areas of need, and ongoing clinical monitoring and case-management. Because only BCT has strong empirical support as an SUD approach to reduce violence, it is critical to develop and test additional approaches. It is hoped that proposing such an integrated care model will assist clinicians and researchers in developing new intervention approaches or models of care designed to reduce violence.
Acknowledgments
Funding for this study was provided by NIDA Grant R01 DA017295; the NIDA had no further role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
The views expressed in this article are those of the authors and do not necessarily represent the views of the University of Michigan, University of Arkansas or the Department of Veterans Affairs.
References
- Aday LA, Andersen RM. A framework for the study of access to medical care. Health Services Research. 1974;9:208–220. [PMC free article] [PubMed] [Google Scholar]
- Alexander JA, Nahra TA, Lemak CH, Pollack H, Campbell CI. Tailored treatment in the outpatient substance abuse treatment sector: 1995–2005. Journal of Substance Abuse Treatment. 2008;34:282–292. doi: 10.1016/j.jsat.2007.04.009. [DOI] [PubMed] [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Arboleda-Florez J. Mental illness and violence: An epidemiological appraisal of the evidence. The Canadian Journal of Psychiatry. 1998;43:989–996. doi: 10.1177/070674379804301002. [DOI] [PubMed] [Google Scholar]
- Baer JS, Kivlahan DR, Donovan DM. Integrating skills training and motivational therapies: Implications for the treatment of substance dependence. Journal of Substance Abuse Treatment. 1999;17:15–23. doi: 10.1016/s0740-5472(98)00072-5. [DOI] [PubMed] [Google Scholar]
- Barrowclough C, Haddock G, Tarrier N, Lewis SN, Moring J, O’Brien R, et al. Randomized controlled trial of motivational interviewing, cognitive behavior therapy, and family intervention for patients with comorbid schizophrenia and substance use disorders. American Journal of Psychiatry. 2001;158:1706–1713. doi: 10.1176/appi.ajp.158.10.1706. [DOI] [PubMed] [Google Scholar]
- Beck R, Fernandez E. Cognitive-behavioral therapy in the treatment of anger: A meta-analysis. Cognitive Therapy and Research. 1998;22:63–74. [Google Scholar]
- Brown TG, Werk A, Caplan T, Shields N, Seraganian P. The incidence and characteristics of violent men in substance abuse treatment. Addictive Behaviors. 1998;23:573–586. doi: 10.1016/s0306-4603(98)00004-5. [DOI] [PubMed] [Google Scholar]
- Burke AC. Triple jeopardy: Women marginalized by substance abuse, poverty and incarceration. In: Figueira-McDonough J, Sarri RC, editors. Women at the margins: Neglect, punishment, and resistance. New York, NY: Haworth Press; 2002. pp. 175–202. [Google Scholar]
- Cantos AL, Neidig PH, O’Leary KD. Injuries of women and men in a treatment program for domestic violence. Journal of Family Violence. 1994;9:112–124. [Google Scholar]
- Cascardi M, Langhinrichsen J, Vivian D. Marital aggression: Impact, injury and health correlates for husbands and wives. Arcives of Interna Medicine. 1992;152:1178–1184. doi: 10.1001/archinte.152.6.1178. [DOI] [PubMed] [Google Scholar]
- Chermack ST, Blow FC. Violence among individuals in substance abuse treatment: The role of alcohol and cocaine consumption. Drug and Alcohol Dependence. 2002;66:29–37. doi: 10.1016/s0376-8716(01)00180-6. [DOI] [PubMed] [Google Scholar]
- Chermack ST, Fuller BE, Blow FC. Predictors of expressed partner and non-partner violence among patients in substance abuse treatment. Drug and Alcohol Dependence. 2000;58:43–54. doi: 10.1016/s0376-8716(99)00067-8. [DOI] [PubMed] [Google Scholar]
- Chermack ST, Giancola PR. The relation between alcohol and aggression: An integrated biopsychosocial conceptualization. Clinical Psychology Review, Special Issue: Biopsychosocial Conceptualizations of Human Aggression. 1997;17:621–649. doi: 10.1016/s0272-7358(97)00038-x. [DOI] [PubMed] [Google Scholar]
- Chermack ST, Murray RL, Walton MA, Booth BA, Wryobeck J, Blow FC. Partner Aggression among Men and Women in Substance Use Disorder Treatment: Predictors of Psychological and Physical Aggression and Injury. Drug and Alcohol Dependence. doi: 10.1016/j.drugalcdep.2008.04.010. (in review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chermack ST, Singer K, Beresford TP. Screening for alcoholism among medical inpatients: How important is corroboration of patient self-report? Alcoholism: Clinical and Experimental Research. 1998;22:1393–1398. doi: 10.1111/j.1530-0277.1998.tb03925.x. [DOI] [PubMed] [Google Scholar]
- Chermack ST, Walton MA, Fuller BE, Blow FC. Correlates of expressed and received violence across relationship types among men and women substance abusers. Psychology of Addictive Behaviors. 2001;15:140–151. doi: 10.1037//0893-164x.15.2.140. [DOI] [PubMed] [Google Scholar]
- Copenhaver MM. Testing a social-cognitive model of intimate abusiveness among substance-dependent males. American Journal of Drug and Alcohol Abuse. 2000;24:603–628. doi: 10.1081/ada-100101898. [DOI] [PubMed] [Google Scholar]
- Daly JE, Pelowski S. Predictors of dropout among men who batter: A review of studies with implications for research and practice. Violence and Victims. 2000;15:137–160. [PubMed] [Google Scholar]
- Darke S. Self-report among injecting drug users: A review. Drug and Alcohol Dependence. 1998;51:253–263. doi: 10.1016/s0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- De Leon G. Integrative recovery. Substance Abuse. 1996;17:51–63. [Google Scholar]
- Dennis M, Scott CK, Funk R. An experimental evaluation of recovery management Checkups (RMC) for people with chronic substance use disorders. Evaluation and Program Planning. 2003;26:339–352. doi: 10.1016/S0149-7189(03)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinwiddie SH. Psychiatric disorders among wife batterers. Comprehensive Psychiatry. 1992;33:411–416. doi: 10.1016/0010-440x(92)90064-w. [DOI] [PubMed] [Google Scholar]
- Dunn C, Deroo L, Rivara FP. The use of brief interventions adapted from motivational interviewing across behavioral domains: A systematic review. Addiction. 2001;96:1725–1742. doi: 10.1046/j.1360-0443.2001.961217253.x. [DOI] [PubMed] [Google Scholar]
- Edmondson CB, Conger JC. A review of treatment efficacy for individuals with anger problems: Conceptual, assessment, and methodological issues. Clinical Psychology Review. 1996;16:251–275. [Google Scholar]
- Fagan J. NIAAA Research Monograph No. 24: Alcohol and Interpersonal Violence: Fostering multidisciplinary perspectives. 1993. Set and setting revisited: Influences of alcohol and illicit drugs on the social context of violent events. NIH Publication No. 93-34-96. [Google Scholar]
- Fals-Stewart W, Golden J, Schumacher J. Intimate partner violence and substance use: A longitudinal day-to-day examination. Addictive Behaviors. 2003;28:1555–1574. doi: 10.1016/j.addbeh.2003.08.035. [DOI] [PubMed] [Google Scholar]
- Fals-Stewart W, Kennedy C. Addressing intimate partner violence in substance-abuse treatment. Journal of Substance Abuse Treatment. 2005;29:5–17. doi: 10.1016/j.jsat.2005.03.001. [DOI] [PubMed] [Google Scholar]
- Fava M. Depression with anger attacks. Journal of Clinical Psychiatry. 1998;59 (suppl 18):18–22. [PubMed] [Google Scholar]
- Goldstein PJ. The drugs/violence nexus: A tripartite conceptual framework. Journal of Drug Issues. 1985;15:493–506. [Google Scholar]
- Gondolf EW, Jones AS. The program effect of batterer programs in three cities. Violence and Victims. 2001;16:693–704. [PubMed] [Google Scholar]
- Hamby SL. Measuring gender differences in partner violence: Implications from research on other forms of violence socially undesirable behavior. Sex Roles. 2005;52:725–742. [Google Scholar]
- Holtzworth-Munroe A, Anglin K. The competency of responses given by maritally violent versus non-violent men to problematic marital situations. Violence and Victims. 1991;6:257–269. [PubMed] [Google Scholar]
- Holtzworth-Munroe A, Meehan JC. Typologies of men who are maritally violent: Scientific and clinical implications. Journal of Interpersonal Violence. 2004;19:1369–1389. doi: 10.1177/0886260504269693. [DOI] [PubMed] [Google Scholar]
- Huss MT, Langhinrichsen-Rohling J. Assessing the generalization of psychopathy in a clinical sample of domestic violence perpetrators. Law and Human Behavior. 2006;30:571–586. doi: 10.1007/s10979-006-9052-x. [DOI] [PubMed] [Google Scholar]
- Joe GW, Simpson DD, Broome KM. Effects of readiness for drug abuse treatment on client retention and assessment of process. Addiction. 1998;93:1177–1190. doi: 10.1080/09652149835008. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee WV, Gottheil E, Sterling RC, Weinstein SP, Serota RD. Characteristics of cocaine-addicted individuals who abuse their partners. Journal of Substance Abuse Treatment. 1997;14:367–371. doi: 10.1016/s0740-5472(97)00011-1. [DOI] [PubMed] [Google Scholar]
- Licata A, Taylor S, Berman M, Cranston J. Effects of cocaine on human aggression. Pharmacology Biochemistry and Behavior. 1993;45:549–552. doi: 10.1016/0091-3057(93)90504-m. [DOI] [PubMed] [Google Scholar]
- Lowe B, Unutzer J, Callahan CM, Perkins AJ, Kroenke K. Monitoring depression treatment outcomes with the Patient Health Questionnaire-9. Medical Care. 2004;42:1194–1201. doi: 10.1097/00005650-200412000-00006. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Grissom GR, Zanis D, Randall M. Problem-service ’matching’ in addiction treatment: A prospective study in 4 programs. Archives of General Psychiatry. 1997;54:730–735. doi: 10.1001/archpsyc.1997.01830200062008. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Hagan TA, Levine M, Meyers K, Gould F, Bencivengo M, Durell J, Jaffe J. Does clinical case management improve outpatient addiction treatment. Drug and Alcohol Dependence. 1999;55:91–103. doi: 10.1016/s0376-8716(98)00183-5. [DOI] [PubMed] [Google Scholar]
- McLellan AT, McKay JR, Forman R, Cacciola J, Kemp J. Reconsidering the evaluation of addiction treatment: from retrospective follow-up to concurrent recovery monitoring. Addiction. 2005;100:447–458. doi: 10.1111/j.1360-0443.2005.01012.x. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people to change. 2. New York: The Guilford Press; 2002. [Google Scholar]
- O’Farrell TJ, Fals-Stewart W. Behavioral couples therapy for alcoholism and drug abuse. Journal of Substance Abuse Treatment. 2000;18:51–54. doi: 10.1016/s0740-5472(99)00026-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Farrell TJ, Fals-Stewart W, Murphy M, Murphy CF. Partner violence before and after individually based alcoholism treatment for male alcoholic patients. Journal of Consulting and Clinical Psychology. 2003;71:92–102. doi: 10.1037//0022-006x.71.1.92. [DOI] [PubMed] [Google Scholar]
- O’Farrell TJ, Murphy CM. Marital violence before and after alcoholism treatment. Journal of Consulting and Clinical Psychology. 1995;63:256–262. doi: 10.1037//0022-006x.63.2.256. [DOI] [PubMed] [Google Scholar]
- O’Farrell TJ, Murphy CM, Stephan SH, Fals-Stewart W, Murphy M. Partner violence before and after couples-based alcoholism treatment for male alcoholic patients: The role of treatment involvement and abstinence. Journal of Consulting and Clinical Psychology. 2004;72:202–217. doi: 10.1037/0022-006X.72.2.202. [DOI] [PubMed] [Google Scholar]
- Osher F, Steadman HJ, Barr H. A best practice approach to community reentry from jails for inmates with co-occurring disorders: The APIC model. Crime and Delinquency. 2003;49:79–96. [Google Scholar]
- Pan H, Neidig P, O’Leary D. Predicting mild and severe husband to wife physical aggression. Journal of Consulting and Clinical Psychology. 1994;62:975–981. doi: 10.1037//0022-006x.62.5.975. [DOI] [PubMed] [Google Scholar]
- Panuzio J, O’Farrell TJ, Marshall AD, Murphy CM, Murphy M, Taft CT. Intimate partner aggression reporting concordance and correlates of agreement among men with alcohol use disorders and their female partners. Assessment. 2006;13:266–279. doi: 10.1177/1073191106287792. [DOI] [PubMed] [Google Scholar]
- Pernanen K. Alcohol in human violence. New York, NY: Guilford Press; 1991. [Google Scholar]
- Project MATCH Research Group. Matching alcoholism treatments to client heterogeneity: Project MATCH posttreatment drinking outcomes. Journal of Studies on Alcohol. 1997;58:7–29. [PubMed] [Google Scholar]
- Quigley BM, Leonard KE. Alcohol, drugs and violence. In: Van Hasselt V, editor. Aggression and violence: An introductory text. Needham Heights, NJ: Allyn and Bacon; 2000. pp. 259–283. [Google Scholar]
- Reilly PM, Shopshire MS. Anger management group treatment for cocaine dependence: Preliminary outcomes. American Journal of Drug and Alcohol Abuse. 2000;26:161–177. doi: 10.1081/ada-100100598. [DOI] [PubMed] [Google Scholar]
- Schafer J, Caetano R, Clark CL. Rates of intimate partner violence in the United States. American Journal of Public Health. 1998;88:1702–1704. doi: 10.2105/ajph.88.11.1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuckit MA, Russell JW. An evaluation of primary alcoholics with histories of violence. Journal of Clinical Psychiatry. 1984;45:3–6. [PubMed] [Google Scholar]
- Schumacher JA, Fals-Stewart W, Leonard KE. Domestic violence treatment referrals for men seeking alcohol treatment. Journal of Substance Abuse Treatment. 2003;24:279–83. doi: 10.1016/s0740-5472(03)00034-5. [DOI] [PubMed] [Google Scholar]
- Scott CK, Dennis ML, Foss MA. Utilizing recovery management checkups to shorten the cycle of relapse, treatment reentry, and recovery. Drug and Alcohol Dependence. 2005;78:325–338. doi: 10.1016/j.drugalcdep.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott KL, Wolfe DA. Readiness to change as a predictor of outcome in batterer treatment. Journal of Consulting and Clinical Psychology. 2003;71:879–889. doi: 10.1037/0022-006X.71.5.879. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Rowan-Szal GA. Drug abuse treatment retention and process effects on follow-up outcomes. Drug and Alcohol Dependence. 1997;47:227–235. doi: 10.1016/s0376-8716(97)00099-9. [DOI] [PubMed] [Google Scholar]
- Simpson LE, Christensen A. Spousal agreement regarding relationship aggression on the Conflict Tactics Scale-2. Psychological Assessment. 2005;17:423–432. doi: 10.1037/1040-3590.17.4.423. [DOI] [PubMed] [Google Scholar]
- Smith GR, Babor T, Burnam MA, Mosley CL, Rost K, Burns B. Substance Abuse Outcomes Module user’s guide manual. Little Rock, AR: University of Arkansas for Medical Sciences; 1996. [Google Scholar]
- Smith GR, Burnam MA, Mosley CL, Hollenberg JA, Mancino M, Grimes W. Reliability and validity of the substance abuse outcomes module. Psychiatry Services. 2006;57:1452–1460. doi: 10.1176/ps.2006.57.10.1452. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD: The PHQ Primary Care Study. JAMA. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Stalans LJ, Seng M. Identifying subgroups at high risk of dropping out of domestic batterer treatment: The buffering effects of a high school education. International Journal of Offender Therapy and Comparative Criminology. 2007;51:151–169. doi: 10.1177/0306624X06290204. [DOI] [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised Conflict Tactics Scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues. 1996;17:283–316. [Google Scholar]
- Stuart GL, Moore TM, Gordon KC, Ramsey SE, Kahler CW. Psychopathology in women arrested for domestic violence. Journal of Interpersonal Violence. 2006;21:376–389. doi: 10.1177/0886260505282888. [DOI] [PubMed] [Google Scholar]
- Swanson JW, Estroff S, Swartz M, Borum R, Lachicotte W, Zimmer C, Wagner R. Violence and severe mental disorder in clinical and community populations: The effects of psychotic symptoms, comorbidity, and lack of treatment. Psychiatry: Interpersonal and Biological Processes. 1997;60:1–22. doi: 10.1080/00332747.1997.11024781. [DOI] [PubMed] [Google Scholar]
- Swanson JW, Holzer CE, Ganju VK, Jono RT. Violence and psychiatric disorder in the community: Evidence from the epidemiologic catchment area surveys. Hospital and Community Psychiatry. 1990;41:761–770. doi: 10.1176/ps.41.7.761. [DOI] [PubMed] [Google Scholar]
- Swartz MS, Swanson JW, Hiday VA, Borum R, Wagner R, Burns RJ. Taking the wrong drugs: The role of substance abuse and medication noncompliance in violence among severely mentally ill individuals. Social Psychiatry and Psychiatric Epidemiology. 1998a;33(Suppl 1):S75–S80. doi: 10.1007/s001270050213. [DOI] [PubMed] [Google Scholar]
- Swartz MS, Swanson JW, Hiday VA, Borum R, Wagner R, Burns RJ. Violence and severe mental illness: The effects of substance abuse and nonadherence to medication. American Journal of Psychiatry. 1998b;155:226–231. doi: 10.1176/ajp.155.2.226. [DOI] [PubMed] [Google Scholar]
- Walton MA, Blow FC, Bingham CR, Chermack ST. Individual and social/ environmental predictors of alcohol and drug use 2 years following substance abuse treatment. Drug and Alcohol Dependence. 2003;67:1–12. [Google Scholar]
- Walton MA, Cunningham RM, Chermack ST, Maio R, Blow FC, Weber J. Correlates of violence history among injured patients in an urban emergency department: Gender, substance use, and depression. Journal of Addictive Diseases. 2007;26:61–75. doi: 10.1300/J069v26n03_07. [DOI] [PubMed] [Google Scholar]
- Walton MA, Chermack ST, Blow FC. Correlates of received and expressed violence persistence following substance abuse treatment. Drug and Alcohol Dependence. 2002;67:1–12. doi: 10.1016/s0376-8716(02)00016-9. [DOI] [PubMed] [Google Scholar]
- Wormith JS, Althouse R, Simpson M, Reitzel LR, Fagan TJ, Morgan RD. The rehabilitation and reintegration of offenders: The current landscape and some future directions for correctional psychology. Criminal Justice and Behavior. 2007;34:879–892. [Google Scholar]