Abstract
Conventional hemorrhoidectomy is applied for the treatment of prolapsing internal hemorrhoids. Recently, less-invasive treatments such as sclerotherapy using aluminum potassium sulphate/tannic acid (ALTA) and a procedure for prolapse and hemorrhoids (PPH) have been introduced. We compared the results of sclerotherapy with ALTA and an improved type of PPH03 with those of hemorrhoidectomy. Between January 2006 and March 2009, we performed hemorrhoidectomy in 464 patients, ALTA in 940 patients, and PPH in 148 patients with second- and third-degree internal hemorrhoids according to the Goligher's classification. The volume of ALTA injected into a hemorrhoid was 7.3 ± 2.2 (mean ± SD) mL. The duration of the operation was significantly shorter in ALTA (13 ± 2 minutes) than in hemorrhoidectomy (43 ± 5 minutes) or PPH (32 ± 12 minutes). Postoperative pain, requiring intravenous pain medications, occurred in 65 cases (14%) in hemorrhoidectomy, in 16 cases (1.7%) in ALTA, and in 1 case (0.7%) in PPH. The disappearance rates of prolapse were 100% in hemorrhoidectomy, 96% in ALTA, and 98.6% in PPH. ALTA can be performed on an outpatient basis without any severe pain or complication, and PPH is a useful alternative treatment with less pain. Less-invasive treatments are beneficial when performed with care to avoid complications.
Keywords: ALTA, Hemorrhoids, PPH
Conventional hemorrhoidectomy is widely applied for the treatment of prolapsing internal hemorrhoids.1 Recently, however, less-invasive treatments such as sclerotherapy using aluminum potassium sulphate/tannic acid (ALTA)2 and a procedure for prolapse and hemorrhoids (PPH)3 have been introduced for prolapsing internal hemorrhoids. ALTA (Zione, Mitsubishi Pharma Corp, Osaka, Japan) is a novel sclerosing therapy for internal hemorrhoids.2 An early clinical study by Hachiro et al indicated that the disappearance rate of prolapsing hemorrhoids after ALTA was over 90%, similar to surgery.2 For PPH, a new improved type of circular stapler (PPH03, Ethicon Endosurgery, Tokyo, Japan) has been available in the clinical setting in Japan since 2004. We compared the results of ALTA and PPH03 with conventional hemorrhoidectomy, retrospectively.
Patients and Methods
Between January 2006 and March 2009, we performed conventional hemorrhoidectomy in 464 patients (282 males and 182 females), ALTA in 940 patients (601 males and 339 females), and PPH in 148 patients (55 males and 93 females) with second- and third-degree internal hemorrhoids according to the Goligher's classification.4 The selection of the procedure depended basically on the patient's choice, although patients with relatively large external hemorrhoids tended to choose hemorrhoidectomy, while those with a relatively weak sphincter tone were more likely to choose PPH, according to their surgeon's advice.
In hemorrhoidectomy, ligation and excision (LE) of hemorrhoids were performed in a jackknife position under lumbar block according to the procedure reported elsewhere.1 ALTA treatment was carried out according to the 4-step injection procedure of ALTA, as described elsewhere.2 Briefly, ALTA was injected into the 4 parts of the hemorrhoid, the submucosa at the superior pole of the hemorrhoid, the submucosa in the central part, the mucous lamina propria in the central part, and the submucosa at the inferior pole, with the patient in a jackknife position under local anesthesia. In the PPH group, surgery was performed in a jackknife position under lumbar block according to the standard procedure using PPH03.3,5,6 This study has been approved by the Institutional Review Board of Clinical Trials.
Clinical outcomes
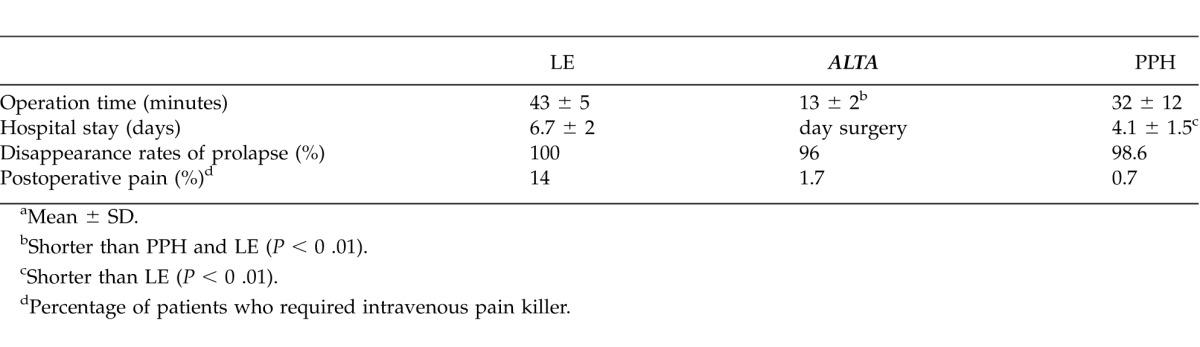
We compared the results of ALTA and PPH03 with LE in terms of clinical outcomes including the duration of the operation, hospital stay, disappearance rate, and postoperative morbidity. Disappearance rate was defined as the disappearance of prolapsing hemorrhoid, which required another treatment. The follow-up period ranged from 15 to 40 months.
Statistics
Differences between means were tested with the Student t test, and the differences between proportions were tested with the χ2 test or Fisher exact test. Probability values from 2-tailed test less than 0.05 were considered statistically significant.
Results
In patients with LE and ALTA, there were more male than female patients, whereas there were more female than male patients with PPH. The average age of patients who underwent LE, ALTA, and PPH was 54 ± 16 years old (mean ± SD), 53 ± 14 years old, and 63 ± 12 years old, respectively. The number of patients with third-degree hemorrhoids was 380 (82%) in LE, 733 (78%) in ALTA, and 136 (92%) in PPH. In the LE group, LE was performed for 1 hemorrhoid in 228 patients (49%), for 2 hemorrhoids in 190 patients (41%), and for 3 hemorrhoids in 46 patients (10%). In the ALTA group, ALTA was injected into 1 hemorrhoid in 235 patients (25%), 2 hemorrhoids in 470 patients (50%), and 3 hemorrhoids in 235 patients (25%). The volume of ALTA injected into a hemorrhoid was 7.3 ± 2.2 mL and 14.6 ± 4.5 mL with 7.3 mL per hemorrhoid and 14.6 mL per patient. The duration of the operation was significantly shorter (P < 0 .01) in ALTA (13 ± 2 minutes) than in LE (43 ± 5 minutes) or PPH (32 ± 12 minutes) (Table 1). No patient in any group developed tissue necrosis or anal stricture that required surgical treatment. After the procedures, a single suppository (indomethacin 25 mg) and/or oral painkiller (loxoprofen 60 mg) was administered for prophylaxis of pain. Postoperative pain, requiring intravenous pain medication (flurbiprofen 50 mg) even after suppository and/or oral painkiller, occurred in 65 cases (14%) in LE, 16 cases (1.7%) in ALTA, and 1 case (0.7%) in PPH. ALTA could be performed on an outpatient basis without any severe complications such as abscess, ulcer, or stenosis. Postoperative morbidity, which did not require any surgical treatment, such as minor bleeding, constipation, and anal swelling, were observed in less than 15 patients (1.5%). The hospital stay was significantly shorter (P < 0 .01) in PPH (4.1 ± 1.5 days) than in LE (6.7 ± 2.0 days) (Table 1). The disappearance rates of prolapse were 100% (464 of 464 patients) in LE, 96% (902 of 940 patients) in ALTA, and 98.6% (146 of 148 patients) in PPH (Table 1).
Discussion
Hemorrhoidectomy is widely applied for the treatment of prolapsing internal hemorrhoids. Although surgery is superior to drug treatment in terms of complete cure, patients are frequently reluctant to undergo surgery because of the hospital stay, excessive fear of postoperative pain, and the potential for other complications. As an alternative to surgery, less-invasive treatments such as sclerotherapy using ALTA and PPH have been introduced recently. ALTA is a promising new sclerosing agent thought to induce rapid termination of blood flow in the hemorrhoids, resulting in hemostasis and reduction of hemorrhoid size. Thereafter, the fibrosis and fixation occur gradually, and the aim of sclerotherapy is achieved.2
To prevent complications from the injection of ALTA, it is important to accurately follow the 4-step injection procedure. Inappropriate injection techniques may induce severe complications such as prostatitis, tissue necrosis, and anal stricture. The authors were careful to avoid overdosage or injection into the muscle layer and gave adequate massage to the injection site after administration.
Regarding the outcome of PPH, a systematic review of the prototype PPH of 25 randomized, controlled trials with a total of 1918 procedures showed that PPH was associated with less operating time, earlier return of bowel function, and a shorter hospital stay.7 Furthermore, there was less pain after PPH, as evidenced by lower pain score at rest and on defecation. Patient satisfaction was significantly higher with PPH than hemorrhoidectomy. The recurrence of hemorrhoids over 1 year after PPH was similar to hemorrhoidectomy.7
PPH03 is a new type of circular stapler device.5 Technically, the new PPH03 stapler device has a quick-close knob, which allows rapid opening and closing. Its weight is less than the prototype PPH and the closed staple height of 0.75 mm increases staple-line compression on tissue and key blood vessels, hence minimizing bleeding. Comparing the results with PPH03 and those with the prototype, several researchers reported that the number of sutures needed for hemostasis after stapling was significantly less with PPH03 than with the prototype.6,8 As a result, the duration of the operation decreased with PPH03 compared with the prototype.6,8
Among the severe complications associated with PPH, rectovaginal fistula,9 rectal perforation,10 and rectal obstruction11 have been reported. They are considered to be the result of inappropriate manipulation or extra-indication of the PPH and are avoidable complications.
Hospital stays after LE and PPH were relatively long in the present study, probably not due to morbidity but because of the low cost of a hospital stay in Japan. Most patients preferred several days hospital stay after surgery, since the cost and fee for a hospital stay are relatively low under the medical insurance system in our country. In the past few decades, ambulatory surgery and systems of home follow-up with easy access to the surgical desk or unit have developed in most countries in America and Europe.12,13 In Japan, by contrast, most patients prefer hospitalization after hemorrhoidectomy. As a result, hemorrhoidectomy is accompanied by hospitalization in most areas of our country. In recent days, however, anorectal procedures such as ALTA and PPH on an outpatient basis have become available and popular. In the near future, we expect ambulatory anorectal surgery including hemorrhoidectomy to become common practice here.
Conclusions
Conventional hemorrhoidectomy is widely applied for prolapsing internal hemorrhoids, but it is accompanied by postoperative pain and hospitalization in our country. ALTA is feasible on an outpatient basis without any severe pain or complication. PPH03 is a useful alternative treatment with a shorter period of hospitalization and less pain compared with conventional hemorrhoidectomy. Less-invasive treatments are beneficial when performed with care to avoid complications.
Acknowledgments
This article was presented in part at the International Surgical Week 2011 in Yokohama, Japan, and at Digestive Disease Week 2012 in San Diego, California.
Table 1 .
Comparison of the resultsa
References
- 1.Hosch SB, Knoefel WT, Pichlmeier U, Schilze V, Busch C, Gawad KA, et al. Surgical treatment of piles: prospective randomized study of Parks vs. Milligan-Morgan hemorrhoidectomy. Dis Colon Rectum. 1998;41(2):159–164. doi: 10.1007/BF02238242. [DOI] [PubMed] [Google Scholar]
- 2.Hachiro Y, Kunimoto M, Abe T, Kusano M. A new sclerosing therapy for internal hemorrhoids: experience in 200 cases with Zione injection. J Jpn Soc Coloproctol. 2006;59(6):317–321. [Google Scholar]
- 3.Longo A. Treatment of hemorrhoids disease by reduction with circular stapler stapling device; a new procedure: Proceedings of the 6th World Congress of Endoscopic Surgery. Rome, Italy: 1998. [Google Scholar]
- 4.Goligher J, Duthie H, Nixon H. Hemorrhoids or piles. In: Goligher J, Duthie H, Nixon H, editors. Surgery of the Anus, Rectum and Colon. 5th ed. London, UK: Baillière Tindall; 1984. pp. 98–149. In. eds. [Google Scholar]
- 5.Lim YK, Eu KW, Ho KS, Ooi BS, Tang CL. PPH03 stapled hemorrhoidopexy: our experience. Tech Coloproctol. 2006;10(1):43–46. doi: 10.1007/s10151-006-0249-3. [DOI] [PubMed] [Google Scholar]
- 6.Tsujinaka Y, Hamahata Y, Matsuo K, Tsutsumi O. Hemorrhoid operation using circular stapler (PPH) [in Japanese] Gastrointest Surg. 2005;28(3):331–337. [Google Scholar]
- 7.Tjandra JJ, Chan MK. Systemic review on the procedure for prolapse and hemorrhoids (stapled hemorrhoidopexy) Dis Colon Rectum. 2007;50(6):878–892. doi: 10.1007/s10350-006-0852-3. [DOI] [PubMed] [Google Scholar]
- 8.Renzi A, Brillantino A, Di Sarno G, D'Aniello F, Giordano A, Stefanuto A, et al. PPH-01 versus PPH-03 to perform STARR for the treatment of hemorrhoids associated with large internal rectal prolapse: a prospective multicenter randomized trial. Surg Innov. 2011;18(3):241–247. doi: 10.1177/1553350611412794. [DOI] [PubMed] [Google Scholar]
- 9.Ravo B, Amato A, Bianco V, Boccasanta P, Bottini C, Carriero A, et al. Complications after stapled hemorrhoidectomy: can they be prevented? Tech Coloproctol. 2002;6(2):83–88. doi: 10.1007/s101510200018. [DOI] [PubMed] [Google Scholar]
- 10.Ripetti V, Caricato M, Arullani A. Rectal perforation, pneumoperitoneum, and pneumomediastinum after stapling procedure for prolapsed hemorrhoids: report of a case and subsequent consideration. Dis Colon Rectum. 2002;45(2):268–270. doi: 10.1007/s10350-004-6159-3. [DOI] [PubMed] [Google Scholar]
- 11.Cipriani S, Pescatori M. Acute rectal obstruction after PPH stapled hemorrhoidectomy. Colorectal Dis. 2002;4(5):367–370. doi: 10.1046/j.1463-1318.2002.00409.x. [DOI] [PubMed] [Google Scholar]
- 12.Martel E, Bernard D, Tasse D, Wassef R. Ambulatory anal surgery: a feasibility study. Ann Chir. 1996;50(8):589–592. [PubMed] [Google Scholar]
- 13.Place R, Hyman N, Simmang C, Cataldo P, Church J, Cohen J, et al. Practice parameters for ambulatory anorectal surgery. Dis Colon Rectum. 2003;46(5):573–576. doi: 10.1007/s10350-004-6610-5. [DOI] [PubMed] [Google Scholar]


