Abstract
It is unknown whether reduced-port gastrectomy has a less invasive nature than conventional laparoscopy-assisted distal gastrectomy (C-LADG). So we compared 30 cases of dual-port laparoscopy-assisted distal gastrectomy (DP-LADG; using an umbilical port plus a right flank 5-mm port) as a reduced-port gastrectomy with 30 cases of C-LADG alternately performed by a single surgeon. No significant differences were observed in blood loss, intraoperative complications, the number of dissected lymph nodes, postoperative complications, the day of first defecation, analgesic agents required, changes in body temperature, heart rate, white blood cell count, serum albumin level, or lymphocyte count between the 2 groups. The amounts of oral intake in the DP-LADG group were significantly higher on postoperative days 9 and 10. We concluded that the amount of oral intake in the DP-LADG group was superior to that in the C-LADG group; however, no other evidence of DP-LADG being less invasive than C-LADG was obtained.
Keywords: Laparoscopy, Gastrectomy, Single incision, Single port, Reduced port
In recent years, single-port surgery, or reduced-port surgery (RPS), has been used in various surgeries, such as splenectomy, colectomy, and gynecologic surgeries,1–14 and its cosmetic merit has been widely accepted.3,4,6,9,11,13 The use of bariatric sleeve gastrectomy and partial gastrectomy for gastrointestinal stromal tumors reported in the field of gastric surgery, however, RPS in gastrectomy for gastric cancer, has just begun.1,7,15–17 We started performing reduced-port laparoscopy-assisted distal gastrectomy through an umbilical port and an additional port [dual-port laparoscopy-assisted distal gastrectomy (DP-LADG)] for gastric cancer located in the lower or middle part of the stomach as an applied laparoscopic gastrectomy in December 2009, and we reported on its safety and feasibility in 2011.17
Laparoscopic gastrectomy is widely recognized as a less invasive surgery that entails a longer operation time but results in a lower bleeding volume, lesser pain, fewer days until first defecation, and earlier recovery of body temperature, heart rate, white blood cell (WBC) count, C-reactive protein (CRP) level, serum albumin level, and lymphocyte count than open gastrectomy.18–21 However, no report has compared invasiveness parameters for reduced-port laparoscopic gastrectomy to those for conventional laparoscopic gastrectomy. So it is unknown whether RPS for gastrectomy is less invasive than conventional laparoscopic gastrectomy.
In this study, to research the less invasive nature of RPS with regard to gastrectomy, we compared intraoperative and postoperative outcomes of DP-LADG and conventional laparoscopy-assisted distal gastrectomy (C-LADG).
Patients and Methods
In this study, the indication for DP-LADG and C-LADG was preoperative clinical Stage IA (cStage IA) gastric cancer located in the lower and middle part of the stomach. Sixty consecutive patients without history of upper abdominal surgery underwent DP-LADG (30 patients) and C-LADG (30 patients) alternately between November 2010 and December 2011 by a single surgeon who had performed more than 300 C-LADG procedures and 20 DP-LADG procedures before starting this study. Informed consent was obtained from all of the patients by the surgeon. The information provided to DP-LADG patients included notification that the surgeon had adequate experience with laparoscopic gastrectomy and RPS, but also that RPS for gastric cancer has not been an established procedure and there was the possibility of conversion to C-LADG.
The extent of lymph node dissection and the degree of cancer stage were classified using the Japanese classification of gastric carcinoma, 3rd English edition, and the Japanese gastric cancer treatment guidelines of 2010, published by the Japanese Gastric Cancer Association.22,23
Operative procedures
Both straight graspers and curved-type graspers (Roticulator Endo Grasp, Covidien Ltd, Hamilton, Bermuda) were used for grasping the tissue in DP-LADG. Activating laparoscopic coagulating shears were used for dissection, and Roux-en-Y reconstructions were performed in all patients. D1+ (N0.8a, 9, 11p) lymph node dissection was performed in all cases.
Port settings in C-LADG
One camera port was inserted into the subumbilical region, two 5-mm ports were inserted into the bilateral hypochondriac region, and two 12-mm ports were inserted into the bilateral flank region. We used a 10-mm flexible scope during C-LADG. A 4-cm–long upper midline abdominal incision was made to extract and reconstruct the stomach (Fig. 1A).
Fig. 1 .
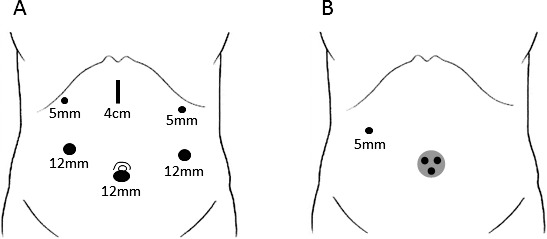
Port settings in C-LADG (A) and DP-LADG (B).
Port settings in DP-LADG
Patients were placed in the Fowler position with legs abducted. A SILS port (Covidien) was inserted into an umbilical incision while another 5-mm port was inserted into the right flank region (Fig. 1B). A 5-mm flexible scope was inserted into the 5-mm trocar at the extreme caudal part of the SILS port. The operator used either 1 trocar of the SILS port and the right flank port, or 2 trocars of the SILS port. The assistant used the remaining trocar for support. The SILS port was removed and a wound protector was attached to the umbilical incision. The stomach was extracted from the umbilical incision and a Y-limb anastomosis was created directly.
Collection of invasiveness parameters
Operation time, blood loss, day of first defecation, number of analgesic agents required, vital signs, hematologic examination, and amount of oral intake were collected for invasiveness parameters. Body temperature and heart rate were analyzed on postoperative days (PODs) 1 to 7 using daily maximum values. Hematologic examination was performed on PODs 1, 4, and 7. The amount of oral intake was analyzed on PODs 4 to 10 using daily maximum values from 3 meals per day.
Clinical pathway
The same postoperative care was provided for all patients using the same clinical pathway; full liquid and walking was resumed on POD 1. Soft diet was resumed on POD4. Regular diet was resumed on POD 8.
Statistical analysis
Student t test and Pearson χ2 test were used for statistical evaluation of the differences between the 2 groups. SPSS 16.0 for Windows (SPSS Inc, Chicago, Illinois) was used for statistical analysis. P < 0.05 was considered statistically significant.
Results
Patient characteristics
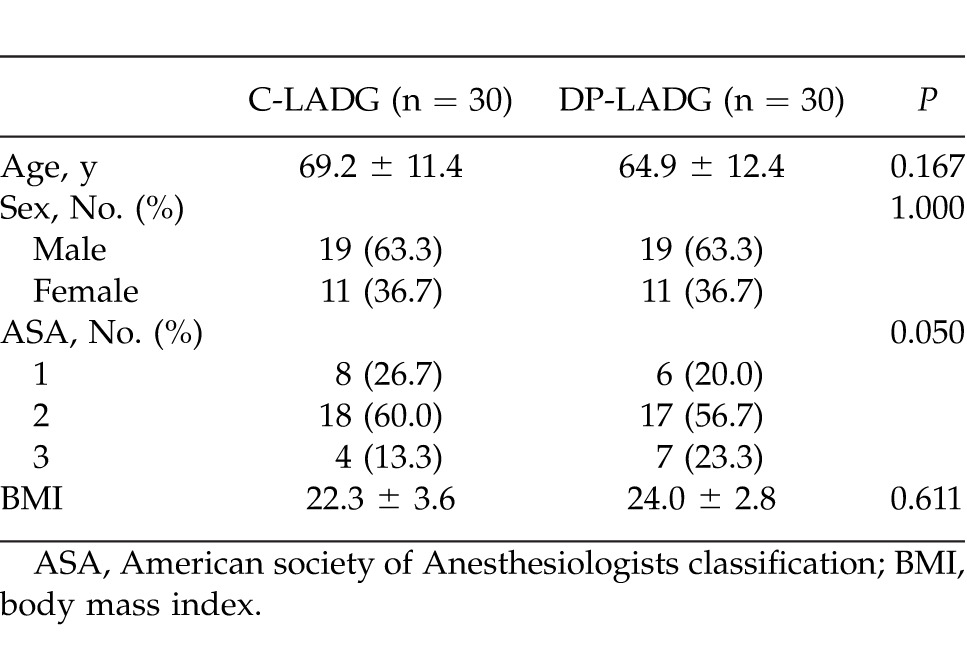
Age, sex, American Society of Anesthesiologists classification, and body mass index did not differ significantly between the 2 groups (Table 1).
Table 1 .
Backgrounds of patients
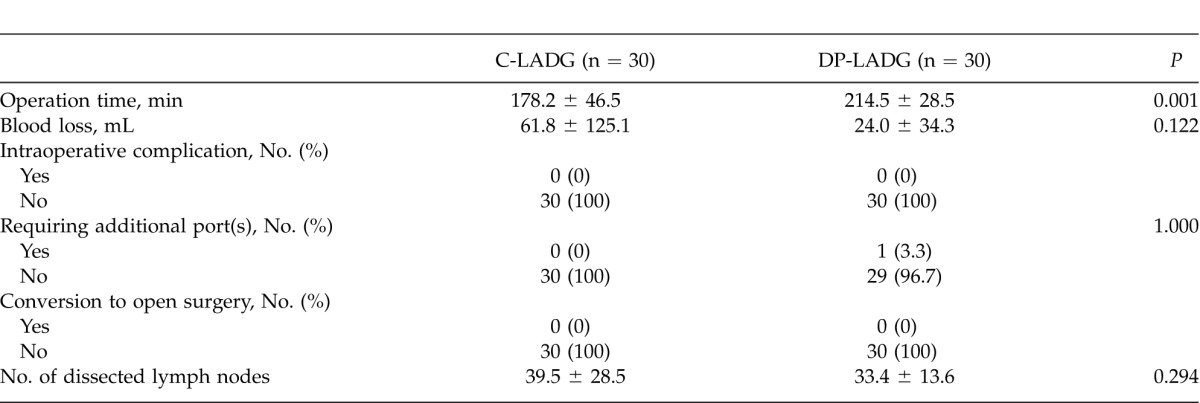
Operative findings
All 30 cases of DP-LADG were accomplished without the addition of a port. All 30 cases of C-LADG were accomplished without conversion to open surgery. Operation time in the DP-LADG group was significantly longer (mean, 214.5 minutes) than that in the C-LADG group (mean, 178.2 minutes). No significant difference in blood loss was observed between the 2 groups. There were no incidences of intraoperative complications requiring additional ports or conversion to open surgery in either group. No significant difference was observed in the number of dissected lymph nodes (Table 2).
Table 2 .
Operative findings
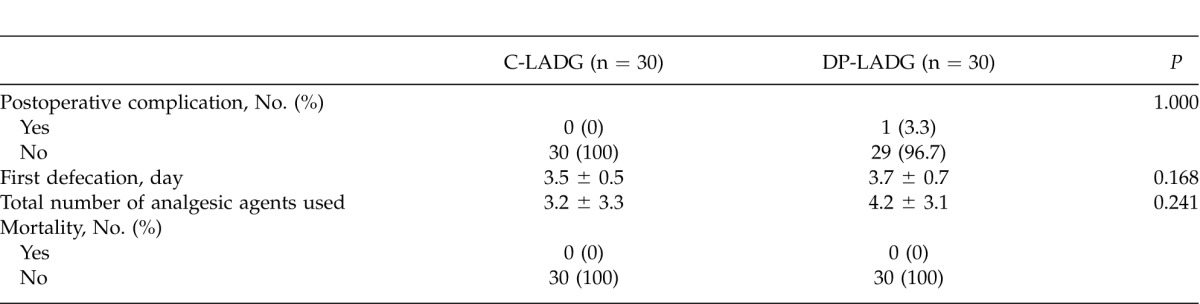
Postoperative course
Pancreatic juice leakage occurred in 1 patient in the DP-LADG group; however, no significant difference was observed in the incidence of postoperative complications between the 2 groups. No significant difference was observed in the day of first defecation and the number of analgesic agents required. There was no incidence of mortality in either group (Table 3).
Table 3 .
Postoperative course
Changes in vital signs and blood examination
Mean body temperature and heart rate in the DP-LADG group normalized in the same manner as they did in the C-LADG group (Fig. 2). WBC counts in the DP-LADG group normalized in the same manner as they did in the C-LADG group (Fig. 3A). On POD 1, CRP levels were significantly higher in the DP-LADG group (5.0 ± 2.1 mg/dL) than in the C-LADG group (3.3 ± 1.9 mg/dL; P = 0.003; Fig. 3B). Serum albumin levels and lymphocyte counts in the DP-LADG group increased to the same extent as those in the C-LADG group (Fig. 3C and 3D).
Fig. 2 .
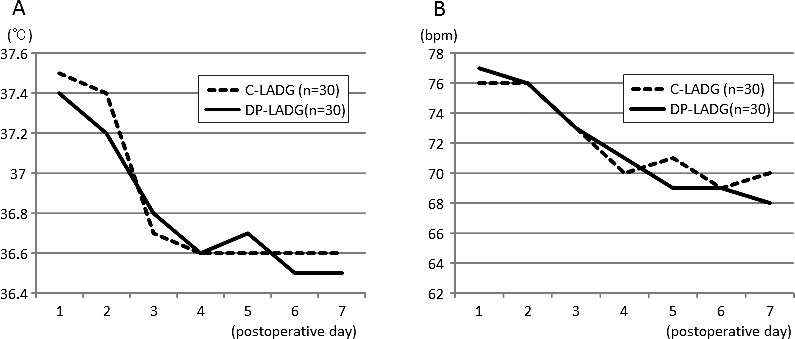
Comparison of body temperature (A) and heart rate (B) in the C-LADG and DP-LADG groups.
Fig. 3 .
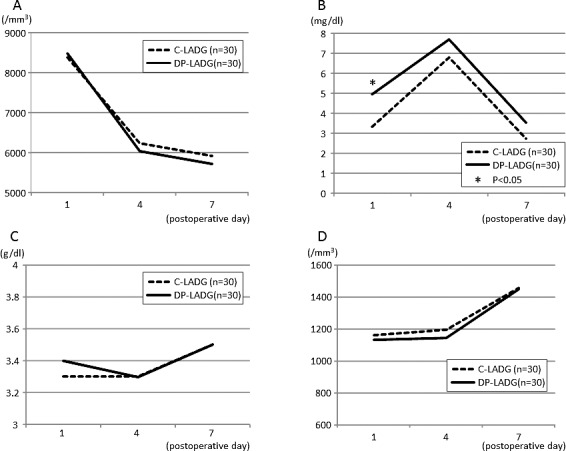
Comparison of changes in WBC counts (A), CRP levels (B), serum albumin levels (C), and lymphocyte counts (D) in the C-LADG and DP-LADG groups.
Changes in the amount of oral intake of food
The amount of oral intake of food in the DP-LADG group was the same as that in the C-LADG group in the early phases; however, the amount of oral intake in the DP-LADG group increased at a greater rate than that in the C-LADG group. The amount of food intake in the DP-LADG group was significantly higher than that in the C-LADG group on PODs 9 (69% versus 55%; P = 0.025) and 10 (67% versus 54%; P = 0.026; Fig. 4).
Fig. 4 .
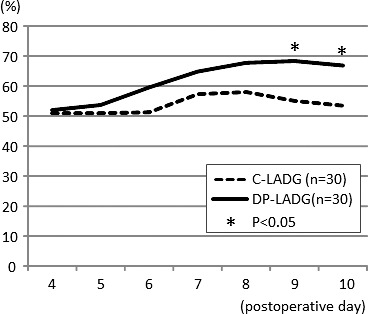
Comparison of amount of oral intake of food in the C-LADG and DP-LADG groups.
Discussion
There have been some previous studies of the safety and feasibility of RPS in gastrectomy for gastric cancer.16,17 These studies had a small sample size and were retrospective in nature. Therefore, the present study is the first prospective report on the safety and feasibility of RPS in gastrectomy. In this study, no significant differences were observed with regard to the amount of blood loss, the rate of intraoperative and postoperative complications, the rate of requiring additional ports, the rate of conversion to open surgery, and the number of dissected lymph nodes between the DP-LADG and C-LADG groups. One disadvantage of DP-LADG compared with C-LADG is that it needs a longer operation time. However, the mean operation time for DP-LADG was 36 minutes longer, which we believe is not a significant prolongation and is within the permissible range. These results demonstrate that the safety and feasibility of DP-LADG are permissible compared with those of C-LADG with regard to gastrectomy with D1+ lymph node dissection. However, we consider that it may be difficult performing D2 lymph node dissection on a morbidly obese patient. In such cases, an additional port (or ports) may be needed to ensure the accuracy of lymph node dissection.
Laparoscopic gastrectomy provides the potential for less pain, early recovery of bowel movement, early normalization of WBC counts and CRP levels, and less of a decrease in serum albumin levels and lymphocyte counts.18–21 RPS is cosmetically superior to conventional laparoscopic surgery; however, it is unknown whether RPS is less invasive than conventional laparoscopic surgery, because there are no detailed reports on this topic. In this comparative study of gastrectomy, no significant differences were observed in the day of first defecation or the number of analgesic agents required. Furthermore, most vital signs and blood examinations in the DP-LADG group changed in the same manner as those in the C-LADG group. CRP levels in the DP-LADG group were significantly higher on POD 1 but not on any other PODs. From our results, we conclude that there is no evidence that DP-LADG is less invasive than C-LADG in commonly used parameters measuring invasiveness.
In this study, we compared the recovery of the amount of oral intake of food between the DP-LADG and C-LADG groups. This is not a commonly used parameter for invasiveness; however, the amount of oral intake in the DP-LADG group increased at a greater rate than that in the C-LADG group. The amount in the DP-LADG group was significantly higher than that in the C-LADG group on PODs 9 and 10. The interpretation for this phenomenon should be prudent because no significant difference was observed in the recovery of bowel function (the day of first defecation) between the 2 groups. We suggest that mental status may be one of the possibilities because the amount of oral intake of food has a close relationship with mental status.24 Patients who underwent DP-LADG had an almost invisible umbilical scar and one small (around 5 mm long) wound, and this might result in a better mental status for them than for patients who underwent C-LADG. In fact, patients in the DP-LADG group often expressed their surprise about the small size of the wound. To make a definitive conclusion about this suggestion, assessment of quality of life, including mental status, would be required.
In conclusion, DP-LADG with D1+ lymph node dissection for early gastric cancer can be performed with the same level of safety and accuracy as C-LADG. There is no evidence that DP-LADG is less invasive than C-LADG in commonly used parameters for invasiveness, such as the day of first defecation, the number of analgesic agents required, changes in vital signs, and blood examinations. The amount of oral intake of food in the DP-LADG group was superior to that in the C-LADG group; however, the reasons for this are unclear. Given the results mentioned above, DP-LADG can be regarded as an optional procedure that is cosmetically superior at present.
References
- 1.Reavis KM, Hinojosa MW, Smith BR, Nguyen NT. Single-laparoscopic incision transabdominal surgery sleeve gastrectomy. Obes Surg. 2008;18(11):1492–1494. doi: 10.1007/s11695-008-9649-x. [DOI] [PubMed] [Google Scholar]
- 2.Nguyen NT, Hinojosa MW, Smith BR, Reavis KM. Single laparoscopic incision transabdominal (SLIT) surgery-adjustable gastric banding: a novel minimally invasive surgical approach. Obes Surg. 2008;18(12):1628–1631. doi: 10.1007/s11695-008-9705-6. [DOI] [PubMed] [Google Scholar]
- 3.Gill IS, Canes D, Aron M, Haber GP, Goldfarb DA, Flechner S, et al. Single port transumbilical (E-NOTES) donor nephrectomy. J Urol. 2008;180(2):637–641. doi: 10.1016/j.juro.2008.04.028. [DOI] [PubMed] [Google Scholar]
- 4.Teixeira J, McGill K, Binenbaum S, Forrester G. Laparoscopic single-site surgery for placement of an adjustable gastric band: initial experience. Surg Endosc. 2009;23(6):1409–1414. doi: 10.1007/s00464-009-0411-9. [DOI] [PubMed] [Google Scholar]
- 5.Fader AN, Escobar PF. Laparoendoscopic single-site surgery (LESS) in gynecologic oncology: technique and initial report. Gynecol Oncol. 2009;114(2):157–161. doi: 10.1016/j.ygyno.2009.05.020. [DOI] [PubMed] [Google Scholar]
- 6.Hernandez JM, Morton CA, Ross S, Albrink M, Rosemurgy AS. Laparoendoscopic single site cholecystectomy: the first 100 patients. Am Surg. 2009;75(8):681–685. ; discussion 685–686. [PubMed] [Google Scholar]
- 7.Saber AA, Elgamal MH, Itawi EA, Rao AJ. Single incision laparoscopic sleeve gastrectomy (SILS): a novel technique. Obes Surg. 2008;18(10):1338–1342. doi: 10.1007/s11695-008-9646-0. [DOI] [PubMed] [Google Scholar]
- 8.Goel RK, Kaouk JH. Single port access renal cryoablation (SPARC): a new approach. Eur Urol. 2008;53(6):1204–1209. doi: 10.1016/j.eururo.2008.03.003. [DOI] [PubMed] [Google Scholar]
- 9.Remzi FH, Kirat HT, Kaouk JH, Geisler DP. Single-port laparoscopy in colorectal surgery. Colorectal Dis. 2008;10(8):823–826. doi: 10.1111/j.1463-1318.2008.01660.x. [DOI] [PubMed] [Google Scholar]
- 10.Desai MM, Rao PP, Aron M, Pascal-Haber G, Desai MR, Mishra S, et al. Scarless single port transumbilical nephrectomy and pyeloplasty: first clinical report. BJU Int. 2008;101(1):83–88. doi: 10.1111/j.1464-410X.2007.07359.x. [DOI] [PubMed] [Google Scholar]
- 11.Hong TH, You YK, Lee KH. Transumbilical single-port laparoscopic cholecystectomy: scarless cholecystectomy. Surg Endosc. 2009;23(6):1393–1397. doi: 10.1007/s00464-008-0252-y. [DOI] [PubMed] [Google Scholar]
- 12.Langwieler TE, Nimmesgern T, Back M. Single-port access in laparoscopic cholecystectomy. Surg Endosc. 2009;23(5):1138–1141. doi: 10.1007/s00464-009-0389-3. [DOI] [PubMed] [Google Scholar]
- 13.Tacchino R, Greco F, Matera D. Single-incision laparoscopic cholecystectomy: surgery without a visible scar. Surg Endosc. 2009;23(4):896–899. doi: 10.1007/s00464-008-0147-y. [DOI] [PubMed] [Google Scholar]
- 14.Barbaros U, Dinççağ A. Single incision laparoscopic splenectomy: the first two cases. J Gastrointest Surg. 2009;13(8):1520–1523. doi: 10.1007/s11605-009-0869-8. [DOI] [PubMed] [Google Scholar]
- 15.Saber AA, El-Ghazaly TH. Early experience with SILS port laparoscopic sleeve gastrectomy. Surg Laparosc Endosc Percutan Tech. 2009;19(6):428–430. doi: 10.1097/SLE.0b013e3181c48993. [DOI] [PubMed] [Google Scholar]
- 16.Omori T, Oyama T, Akamatsu H, Tori M, Ueshima S, Nishida T. Transumbilical single-incision laparoscopic distal gastrectomy for early gastric cancer. Surg Endosc. 2011;25(7):2400–2404. doi: 10.1007/s00464-010-1563-3. [DOI] [PubMed] [Google Scholar]
- 17.Kawamura H, Tanioka T, Funakoshi T, Takahashi M. Dual-ports laparoscopy-assisted distal gastrectomy compared with conventional laparoscopy-assisted distal gastrectomy. Surg Laparosc Endosc Percutan Tech. 2011;21(6):429–433. doi: 10.1097/SLE.0b013e318238063c. [DOI] [PubMed] [Google Scholar]
- 18.Miura S, Kodera Y, Fujiwara M, Ito S, Mochizuki Y, Yamamura Y. Laparoscopy-assisted distal gastrectomy with systemic lymph node dissection: a critical reappraisal from the viewpoint of lymph node retrieval. J Am Coll Surg. 2004;198(6):933–938. doi: 10.1016/j.jamcollsurg.2004.01.021. [DOI] [PubMed] [Google Scholar]
- 19.Shiraishi N, Yasuda K, Kitano S. Laparoscopic gastrectomy with lymph node dissection for gastric cancer. Gastric Cancer. 2006;9(3):167–176. doi: 10.1007/s10120-006-0380-9. [DOI] [PubMed] [Google Scholar]
- 20.Kawamura H, Okada K, Isizu H, Masuko H, Yamagami H, Honma S. Laparoscopic gastrectomy for early gastric cancer targeting as a less invasive procedure. Surg Endosc. 2008;22(1):81–81. doi: 10.1007/s00464-007-9373-y. [DOI] [PubMed] [Google Scholar]
- 21.Memon MA, Khan S, Yunus RM, Barr R, Memon B. Meta-analysis of laparoscopic and open gastrectomy for gastric carcinoma. Surg Endosc. 2008;22(8):1781–1789. doi: 10.1007/s00464-008-9925-9. [DOI] [PubMed] [Google Scholar]
- 22.Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma–3rd English edition. Gastric Cancer. 2011;14:101–112. doi: 10.1007/s10120-011-0041-5. [DOI] [PubMed] [Google Scholar]
- 23.Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010. Gastric Cancer. 2011;14:113–123. doi: 10.1007/s10120-011-0042-4. [DOI] [PubMed] [Google Scholar]
- 24.Davison KM, Kaplan BJ. Nutrient intakes are correlated with overall psychiatric functioning in adults with mood disorders. Can J Psychiatry. 2012;57(2):85–92. doi: 10.1177/070674371205700205. [DOI] [PubMed] [Google Scholar]


