Increasingly Hard to Swallow – 18 Years of Changing Tonsillectomy Practice in Northern Ireland.
Editor,
The clinical and economic value of tonsillectomy has been the subject of debate for decades. The McKinsey Report1 considered tonsillectomy (along with a number of other procedures) to be a ‘relatively ineffective, and often unjustified’ procedure, stating that reducing tonsillectomies by 90 percent could save the NHS £45 million each year. Subsequently ENT UK2 showed an association between a decreasing number of tonsillectomies performed within the UK and an increasing number of hospital admissions for tonsil-related complications.
The aim of our study was to determine if there was an association between the number of tonsillectomies performed and the number of admissions for tonsillitis and peri-tonsillar abscesses in Northern Ireland. Using a computer-aided system data was collected and analyzed for all tonsillectomies performed within the Southern Trust from 1994 until 2012, and compared to the admission rate for tonsillitis and peritonsillar abscesses during the same time period.
From 1994 until 2001 the number of tonsillectomies performed decreased from 1,235 to 497 per year, while the number of admissions for tonsillitis and peri-tonsillar abscesses increased from 226 to 452 per year. The decrease in the number of tonsillectomies performed was largely attributed to financial constraints and waiting-list times within the Trust. From 2001 until 2012 the number of tonsillectomies performed increased from 497 to 973 per year, while the number of admissions for tonsillitis and peritonsillar abscesses decreased from 452 to 239 per year. Our results show a general trend between the decreasing number of tonsillectomies performed and an increased number of admissions for tonsillitis and peri-tonsillar abscesses, and vice-versa, over the 18 year period assessed (Figure 1). Studies in England and Wales have shown similar results with admissions for tonsillitis increasing over the last decade while the number of tonsillectomies has generally declined.3,4
With ever increasing pressure on governments to curtail spending in healthcare budgets it is important for both doctors in primary and secondary healthcare practices to be aware of the potential impact on the quality of life of their patients from reducing the number of operations
performed that are deemed “ineffective” by government. The impact of tonsillitis and peri-tonsillar abscesses on both the patients’ quality of life and the economy is considerable with the debilitating nature of these conditions resulting in an average of 35 million days being lost from school and work in the UK each year2.
Effective referral and selection practices are essential for members of the medical profession to justify the procedures they perform and ensure autonomy of our practice is continued and not dictated by government budgetary policies. Evidencebased national guidelines are available to aid clinicians in identifying patients who are suitable for referral and would benefit most from surgery across a number of specialities5. Within Otorhinolaryngology increasing the annual number of tonsillectomies performed in selected patient groups is likely to result in an overall decreased number of hospital admissions for tonsil-related pathology and potential cost savings as a result.
The authors have no conflict of interest.
Department of Otolaryngology, Southern HSC Trust, Craigavon, Northern Ireland.
Gary Ferguson
Philip R Bell
Samuel J Hall.
References
- 1.McKinsey and Company. Department of Health. London: 2009. Achieving world class productivity in the NHS 2009/10 – 2013/14: detailing the size of the opportunity. Available from: http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_116521.pdf. Last accessed March 2009. [Google Scholar]
- 2.ENT UK. 2009. Indications for tonsillectomy: Position paper. London: ENT.UK at The Royal College of Surgeons of England; 2009. Available from: https://entuk.org/docs/prof/position_papers/tonsillectomy_position_paper. Last accessed March 2013.
- 3.Koshy E, Murray J, Bottle A, Aylin P, Sharland M, Majeed A, Saxena S. Significantly increasing hospital admissions for acute throat infections among children in England: is this related to tonsillectomy rates? Arch Dis Child. 2012;97(12):1064–8. doi: 10.1136/archdischild-2012-301755. [DOI] [PubMed] [Google Scholar]
- 4.Mcleod R, Fishpool S, Owens D, Backhouse S. Is there a link between the changing incidence of peritonsillar abscess and the rates of tonsillectomy in Wales and England? Int J Surg. 2012;10(8 Suppl 1):S38. [Google Scholar]
- 5.Scottish Intercollegiate Guidelines Network. 2012. [SIGN] Management of sore throat and indications for tonsillectomy: a national clinical guideline 117. Edinburgh: Scottish Intercollegiate Guidelines Network;. Available from: http://www.sign.ac.uk/pdf/sign117.pdf Last accessed March 2013.
Closed Talar Dislocation After Low Energy Trauma
Editor,
Abstract
A closed dislocation of the talus, without fracture, occurring after low energy trauma is extremely rare. We report our experience of a 47 year old gentleman who presented with a closed posteromedial dislocation of his talus following forced pronation of his foot while playing football. This was reduced urgently in the Emergency Department under conscious sedation and managed in a short leg cast for 6 weeks. Early CT imaging revealed osteochondral injury to the talar dome, not visible on plain radiographs. There are few reported cases in the literature and no guidelines regarding the optimal method of treating this injury. We advocate attempted urgent reduction to preserve function and early CT imaging to assess for injuries that are not apparent on plain radiographs.
Case Report
A 47 year old gentleman presented to our Emergency Department (ED) after sustaining a forced pronation of his foot while playing football. Clinical examination in the ED revealed a closed deformity of the ankle with tense skin over the medial aspect.
Plain radiographs revealed a postero-medial dislocation of the talus with no obvious associated fracture (Fig1a). He underwent urgent closed reduction under conscious sedation in the ED. Reduction occurred relatively easily on the first attempt and was confirmed with plain radiographs (Fig).
Fig 1a.

Fig 1b.

A short leg cast was applied for six weeks. Outpatient CT scan at two weeks revealed an osteochondral injury to the midlateral talar dome with resultant small intra-articular loose body.
Discussion
Complete dislocation of the talus is an extremely rare injury that normally occurs after high energy trauma1, 2 and most reported cases are open injuries.
Total talar dislocation is thought to be the endpoint of maximum pronation or supination coupled with a plantar-flexion force placed across it4. Forced supination will cause antero-lateral dislocation (most common) and pronation will dislocate postero-medially3. Leitner5 described a three-stage mechanism of dislocation; firstly dislocation of the subtalar joint, followed by talonavicular and then total extrusion as supination or pronation forces progress.
For closed injuries, Ritsema suggests a rapid open reduction is optimal6. A further argument for open reduction is the possibility of tibialis posterior tendon preventing reduction of lateral dislocations4, or extensor digitorum brevis or peroneals blocking lateral dislocations8. However, Taymaz and Gunal2 report excellent results of a case treated by closed means and Hadji et al7 report positive findings at 3 year follow up of a closed reduction.
De Palma9 suggested that final functional outcome may also be related to the direction of dislocation. while medial dislocations generally have good outcomes, lateral dislocations have been associated with the more significant disability. These injuries are most commonly complicated by Avascular necrosis (AVN), post traumatic arthritis and infection.
Summary
Closed dislocation of the talus is an extremely rare injury. We advocate early attempted reduction under sedation in the ED, thus preserving talar blood supply, before considering surgery, and routine early CT scanning to look for osteochondral injury not seen on plain radiographs.
Gerard Kelly
Frederick Reid
David Kealey
Department of Trauma and Orthopaedics, Royal Victoria Hospital, Grosvenor Road, Belfast BT12 6BA.
The authors have no conflict of interest.
References
- 1.Heylen S, De Baets T, Verstraete P. Closed total talus dislocation: a case report. Acta Orthop Belg. 2011;77(6):838–42. [PubMed] [Google Scholar]
- 2.Taymaz A, Gunal I. Complete dislocation of the talus - Unaccompanied by fracture. J Foot Ankle Surg. 2005;44(2):156–8. doi: 10.1053/j.jfas.2005.01.008. [DOI] [PubMed] [Google Scholar]
- 3.Xarchas KC, Psillakis IG, Kazakos KJ, Pelekas S, Ververidis AN, Verettas DA. Total dislocation of the talus without a fracture. Open or closed treatment? Report of two cases and review of the literature. Open Orthop J. 2009;3:52–5. doi: 10.2174/1874325000903010052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turhan Y, Cift H, Ozkan K, Ozkut A, Eren A. Closed total talar extrusion after ankle sprain. Foot Ankle Spec. 2012;5(1):51–3. doi: 10.1177/1938640011418497. [DOI] [PubMed] [Google Scholar]
- 5.Leitner B. The mechanism of total dislocation of the talus. J Bone Joint Surg Am. 1955;37A(1):89–95. [PubMed] [Google Scholar]
- 6.Ritsema GH. Total talar dislocation. J Trauma. 1988;28(5):692–4. doi: 10.1097/00005373-198805000-00025. [DOI] [PubMed] [Google Scholar]
- 7.Hadji M, Golli M, Moalla R, Kmantar L, Hamdi A. [Conservative treatment of talar dislocation: a case report.] Rev Chir Orthop Reparatrice Appar Mot. 2004;90(3):285–8. doi: 10.1016/s0035-1040(04)70107-5. French. [DOI] [PubMed] [Google Scholar]
- 8.Banaszkiewicz PA, Kader DF, editors. Postgraduate orthopaedics: the candidate’s guide to the FRCS (Tr & Orth) examination. Cambridge: Cambridge University Press; 2012. [Google Scholar]
- 9.de Palma L, Santucci A, Marinelli M, Borgogno E, Catalani A. Clinical outcome of closed isolated subtalar dislocations. Arch Orthop Trauma Surg. 2008;128(6):593–8. doi: 10.1007/s00402-007-0459-8. [DOI] [PubMed] [Google Scholar]
The Great Pretender: Gastrointestinal Stromal Tumour in Pregnancy Presenting with Liver Metastases
Editor,
Gastrointestinal Stromal Tumours (GISTs) constitute approximately 3% of all neoplasms of the gastrointestinal tract (GIT). Reported incidence is estimated between 1 and 20 per million people.1
Case
A 22-year-old woman presented to surgical outpatients at 21 weeks gestation reporting a 17 month history of a ‘lump’ in her upper abdomen, associated with abdominal pain, nausea, early satiety and vomiting. A swelling in the left upper quadrant of her abdomen was noted in addition to tender hepatomegaly. Abdominal ultrasound confirmed multiple liver lesions, the largest in the right lobe of the liver measuring 10 cm (Figure 1a).
Inpatient OGD demonstrated submucosal tumour of the stomach, and MRI of the abdomen confirmed the liver lesions and a 4.4 cm lesion arising from the stomach (Figure 1b). Examination of core liver biopsies revealed metastasis from a GIST thought to be of gastric origin. Tumour cells showed positive immunoreactivity for c-Kit, DOG1 and CD99. Mutational analysis demonstrated it was wild type for c-Kit, platelet-derived growth factor receptor a (PDGFRA) and B-Raf. A diagnosis of GIST, stage 4 was concluded.
A repeat MRI scan at 25 weeks gestation demonstrated rapid progression of the tumour within the stomach and liver. Subsequently, treatment with Imatinib was commenced.
The patient reported increasing pain due to pressure exerted by the gravid uterus on her liver. Antenatal steroids were administered at 28 weeks gestation and an elective caesarean section was performed. A live male infant was delivered weighing 1200g. He was transferred to the neonatal intensive care unit where he remained for six weeks. Our patient was admitted to the palliative care unit for symptom control.
Fig 1a.

Ultrasound of liver: Well-defined heterogenous lesion measuring 10 cm within the right lobe of the liver.
Fig 1b.
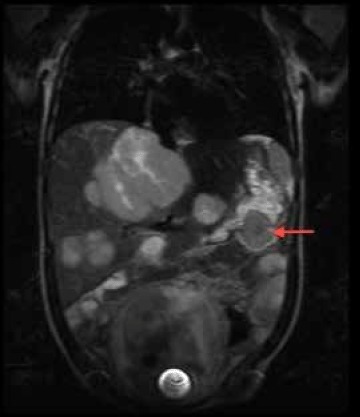
MRI of abdomen: Coronal T2 weighted sequence demonstrating an extra-hepatic lesion arising from the greater. A repeat MRI scan at 25 weeks gestation demonstrated rapid progression of the tumour within the stomach and liver. Subsequently, treatment with Imatinib was commenced.
title>Discussion
Discerning a diagnosis of GIST in pregnancy is difficult as symptoms mimic complaints associated with uncomplicated pregnancy. Lesions are found most commonly in the stomach (50%) however they may arise throughout the GIT.1 Due to the potential risk of fetal carcinogenesis, MRI is the preferred investigative method in pregnancy.2
We note little consensus as to how these women should be managed. Primary surgical resection forms the mainstay of treatment for limited disease; more recently, Imatinib mesylate, a targeted molecular therapy which inhibits the KIT receptor tyrosine kinase, has improved management of GIST in patients expressing KIT or PDGFRA mutations.3 Tumour response to Imatinib is poor in patients with wild-type GIST. Nilotinib, a second generation tyrosine kinase inhibitor has been developed to overcome Imatinib resistance. Trials examining its effectiveness as a first-line treatment for patients with metastatic or inoperable GISTs are ongoing.4
The effects of Imatinib in pregnancy are largely unknown; Pye et al report 180 cases of women on Imatinib for treatment of chronic myeloid leukaemia in pregancy. Outcome data for 125 cases were known (69%); there were eight live births and one stillbirth with congenital abnormalities. Three infants displayed similar findings of exomphalus, craniosynostosis and bony abnormalities.5
Managing GIST in pregnancy is fraught with uncertainty: the effect of pregnancy on GIST, timing and mode of delivery, initiation of Imatinib, its effects on the fetus and the long-term prognosis for the patient and her child.
Kelly-Ann Eastwood
Keith Johnston
Martin Eatock
Eddie Gibson
Eunice Minford
The authors have no conflict of interest
References:
- 1.Varras M, Vlachakos N, Akrivis C, Vasilakaki T, Skafida E. Malignant gastrointestinal stromal tumor presenting with hemoperitoneum in puerperium: report of a case with review of the literature. World J Surg Oncol. 2010;8(95):1–7. doi: 10.1186/1477-7819-8-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Casali PG, Blay JY. Gastrointestinal stromal tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21(Suppl 5):v98–v102. doi: 10.1093/annonc/mdq208. [DOI] [PubMed] [Google Scholar]
- 3.Miettinen M, Sobin LH, Lasota J. Gastrointestinal stromal tumors of the stomach: a clinicopathologic, immunohistochemical, and molecular genetic study of 1765 cases with long-term follow-up. Am J Surg Pathol. 2005;29(1):52–68. doi: 10.1097/01.pas.0000146010.92933.de. [DOI] [PubMed] [Google Scholar]
- 4.Benjamin RS, Blanke CD, Blay JY, Bonvalot S, Eisenberg B. Management of gastrointestinal stromal tumors in the Imatinib era: selected case studies. Oncologist. 2006;1(1):9–20. doi: 10.1634/theoncologist.11-1-9. [DOI] [PubMed] [Google Scholar]
- 5.Pye SM, Cortes J, Ault P, Hatfield A, Kantarjian H, Pilot R. The effects of imatinib on pregnancy outcome. Blood. 2008;111(12):5505–08. doi: 10.1182/blood-2007-10-114900. [DOI] [PMC free article] [PubMed] [Google Scholar]
A Case of Severe Hypocalcaemia
Editor,
Abstract:
There have been increased reports linking the use of Proton Pump Inhibitor Drugs (PPIs) to electrolyte disturbance. We report a case of a 71 year old lady who was troubled by intermittent pins and needles for six months before she was found to be severely hypocalcaemic. Further investigations suggested that her low calcium level was secondary to hypomagnesemia which, in turn, was secondary to treatment with Omeprazole.
Case Report:
A 71 year old woman was referred to hospital after she was found to be severely hypocalcaemic by her General Practitioner (GP). She had attended her GP with a six months history of intermittent sensation of pins and needles in her legs and arms. Her past medical history is of folic acid deficiency, hypertension, depression, and bladder cancer. She was taking the following medications: Aspirin 75 mg, Bisoprolol 10mg, Flurazepam 30mg, Dosulepin 150mg, Doxazocin 4mg, Ramipril 10mg, Pravastatin 40mg, Omeprazole 20mg, and Ropinirole 250mcg.
She was still complaining of numbness on arrival to hospital but Chvostek’s and Trousseau’s signs were not present. Her blood tests showed a magnesium level of 0.19mmol/L (0.7–1), a calcium level of 1.39mmol/L (2.1–2.6) [corrected levels], and a potassium level of 3.2mmol/L (3.5–5.3).
She was initially treated with intravenous magnesium and calcium supplements, and oral potassium. Following correction of her magnesium levels she became hyperkalemic with potassium of 6.3mmol/L. Her Ramipril was therefore stopped. When her electrolyte levels were normalised her tingling stopped. Further investigations showed a vitamin D level of 13nmol/L (<25 is defficient), a parathormone level of 65pg/ml (15–65), a negative coeliac screen, and a normal vitamin B12 and folate levels.
Her medications review raised the possibility that Omeprazole was causing her electrolyte disturbances. She had been on Omeprazole for six years. This was changed to Ranitidine during her admission.
She was discharged home on calcium and vitamin D supplements.
Her electrolytes were repeated two months following her discharge and they were all in the normal range.
Discussion:
The patient’s electrolyte abnormalities resolved after Omeprazole was withdrawn. There have been previous reports linking Omeprazole and other PPIs to electrolyte disturbance1,2. The presumed mechanism is impaired intestinal absorption since urinary magnesium excretion is usually appropriately low 1. The resulting hypomagnesaemia may cause hypoparathyroidism, hypocalcaemia, and hypokalaemia3.
The symptoms of magnesium deficiency relate to the central role of magnesium in ATP metabolism and neuromuscular transmission2. However, symptomatic magnesium depletion is often associated with multiple biochemical abnormalities such as hypokalemia, hypocalcemia, and metabolic alkalosis3. As a result it is often difficult to ascribe specific clinical manifestations solely to hypomagnesemia3. The organ systems commonly affected by magnesium deficiency are the cardiovascular system and the central and peripheral nervous systems4.
The U.S Food and Drug Administration currently recommends that healthcare professionals should consider obtaining serum magnesium levels prior to initiation of PPIs treatment and checking levels periodically thereafter for patients expected to be on prolonged treatment or who take PPIs with medications such as Digoxin or drugs that may cause hypomagnesaemia (e.g. diuretics)5.
Habeichi W,
Ahmed G.
Daisy Hill Hospital
The authors have no conflict of interest
References:
- 1.Yu AS, Ahluwalia GK. In: Cause of hypomagnesemia. Basow DS, editor. Waltham, MA: 2013. UpToDate; [Google Scholar]
- 2.Shabajee N, Lamb EJ, Sturgess I, Sumathipala RW. Omeprazole and refractory hypomagnesaemia. BMJ. 2008;337(7662):173–5. doi: 10.1136/bmj.39505.738981.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agus ZS. In: Signs and symptoms of magnesium depletion. Basow DS, editor. Waltham, MA: 2012. UpToDate. [Google Scholar]
- 4.Fulop T, Agraharkar M, Fahlen MT, Rondon-Berrios H. Hypomagnesemia. In: Batuman V, editor. Medscape Reference. Drugs, diseases and procedures. New York Medscape: LLC; 2011. Available from: http://emedicine.medscape.com/article/2038394-overview. Last accessed March 2013. [Google Scholar]
- 5.Shepherd J. FDA Drug Safety Podcast for Healthcare Professionals: Low magnesium levels can be associated with long-term use of Proton Pump Inhibitor drugs (PPIs) Silver Spring, MD: U.S. Food and Drug Administration; 2011. Available from: http://www.fda.gov/Drugs/DrugSafety/DrugSafetyPodcasts/ucm245455.htm. Last accessed March 2013. [Google Scholar]


