Abstract
OBJECTIVE
To describe trends in the surgical management of female stress urinary incontinence (SUI) in the United States from 2002 to 2007.
METHODS
As part of the Urologic Diseases of America Project, we analyzed data from a 5% national random sample of female Medicare beneficiaries aged 65 and older. Data were obtained from the Centers for Medicare and Medicaid Services carrier and outpatient files from 2002 to 2007. Women who were diagnosed with urinary incontinence identified by the International Classification of Diseases, Ninth Edition (ICD-9) diagnosis codes and who underwent surgical management identified by Current Procedural Terminology, Fourth Edition (CPT-4) procedure codes were included in the analysis. Trends were analyzed over the 6-year period. Unweighted procedure counts were multiplied by 20 to estimate the rate among all female Medicare beneficiaries.
RESULTS
The total number of surgical procedures remained stable during the study period, from 49,340 in 2002 to 49,900 in 2007. Slings were the most common procedure across all years, which increased from 25,840 procedures in 2002 to 33,880 procedures in 2007. Injectable bulking agents were the second most common procedure, which accounted for 14,100 procedures in 2002 but decreased to 11,320 in 2007. Procedures performed in ambulatory surgery centers and physician offices increased, although those performed in inpatient settings declined. Hospital outpatient procedures remained stable.
CONCLUSION
The surgical management of women with SUI shifted toward a dominance of procedures performed in ambulatory surgery centers from 2002 to 2007, although the overall number of procedures remained stable. Slings remained the dominant surgical procedure, followed by injectable bulking agents, both of which are easily performed in outpatient settings.
Published guidelines recommend that women with stress urinary incontinence (SUI) who fail conservative management should be considered for all acceptable surgical options. The American (American Urologic Association, AUA, and American College of Obstetricians and Gynecologists, ACOG), and European (European Association of Urology, EAU) guidelines consider slings, laparoscopic suspensions, and injectable bulking agents as acceptable treatment options.1-3
The past decades have witnessed a shift in the surgical management of SUI toward a dominance of sling procedures.4 As part of the Urologic Diseases in America Project, we previously analyzed data from Medicare beneficiaries from 1992 to 2001 and found rapid shifts in surgical procedures for female SUI.5 In 1992, urethropexy (Burch, Marshall-Marchetti-Krantz) was the most commonly performed procedure. However, it was surpassed by the sling and the suburethral bulking procedures by 2001. Similar declines were seen with urethropexy and needle suspensions. Conversely, we demonstrated an increase in slings from among the least commonly performed procedures in 1992 to the most commonly performed procedure in 2001. Herein we sought to describe more recent trends in the surgical management of SUI.
MATERIALS AND METHODS
We analyzed data from a 5% national random sample of female Medicare beneficiaries aged 65 and older as part of the Urologic Diseases of America Project.6 Data were obtained from the Centers for Medicare and Medicaid Services carrier and outpatient files from 2002 to 2007, which comprised approximately 11 million records per year. Subjects diagnosed with urinary incontinence identified by the International Classification of Diseases, Ninth Edition (ICD-9) diagnosis codes were included in the analysis (See Appendix 1).
Treatment for urinary incontinence was identified using Current Procedural Terminology, Fourth Edition (CPT-4) procedure codes and women were categorized based on their procedure code (Appendix 1). Procedure location information was obtained from the same outpatient files and grouped into four categories (ambulatory surgery center, hospital outpatient, inpatient, and physician office). Unweighted procedure counts were multiplied by 20 to estimate the rate among all female Medicare beneficiaries. Trends in surgical management were analyzed over the 6-year period by grouping procedures by location.
RESULTS
A total of 291,180 procedures for SUI were identified during the study period. Procedure count was estimated by multiplying the procedure count of a sample of 5% of Medicare beneficiaries by 20. The annual number of surgical procedures remained stable, from 49,340 in 2002 to 49,900 in 2007 (Table 1). Slings were the most common procedure across all years, which increased from 25,840 procedures in 2002 to 33,880 in 2007. The rate of slings also increased during the study period from 5270 to 6693 per 100,000 female Medicare beneficiaries with a primary diagnosis of urinary incontinence. Rates were reported per 100,000 female Medicare beneficiaries with a primary diagnosis of urinary incontinence.
Table 1.
Trends in the surgical management of stress urinary incontinence among female Medicare beneficiaries*
| Procedure | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | Total |
| Pubovaginal sling | 25,840 (5270) | 28,580 (5749) | 31,480 (6269) | 31,640 (6185) | 33,300 (6525) | 33,880 (6693) | 184,720 |
| Injectable bulking agents | 14,100 (2875) | 12,100 (2434) | 11,300 (2250) | 10,160 (1986) | 10,980 (2151) | 11,320 (2236) | 69,960 |
| Urethropexy | 4340 (885) | 2480 (499) | 1820 (362) | 1360 (266) | 1080 (212) | 820 (162) | 11,900 |
| Hysterectomy with colpo-urethropexy | 2900 (591) | 3320 (668) | 2740 (546) | 2280 (446) | 2440 (478) | 3100 (612) | 16,780 |
| Raz-type suspension | 1100 (224) | 680 (137) | 480 (96) | 320 (63) | 220 (43) | 100 (20) | 2900 |
| Laparoscopic repair | 680 (139) | 600 (121) | 540 (108) | 480 (94) | 500 (98) | 560 (111) | 3360 |
| Pereyra procedure | 240 (49) | 140 (28) | 100 (20) | 160 (31) | 40 (8) | 40 (8) | 720 |
| Kelly plication | 140 (29) | 120 (24) | 140 (28) | 220 (43) | 140 (27) | 80 (16) | 840 |
| Total | 49,340 | 48,020 | 48,600 | 46,620 | 48,700 | 49,900 | 291,180 |
Data are presented as counts, which were calculated from unweighted counts multiplied by 20, and the data in parenthesis are rates per 100,000 female Medicare beneficiaries with a primary diagnosis of urinary incontinence.
Injectable urethral bulking agents were the second most commonly performed procedure, although the number of procedures performed decreased from 14,100 in 2002 to 11,320 in 2007. The rate of injections also declined slightly from 2875 to 2236 procedures per 100,000. Urethropexy declined dramatically from 4340 procedures in 2002 to 820 in 2007. Similarly, the Raz-type suspension declined from 1100 procedures in 2002 to 100 in 2007. Hysterectomy with colpo-urethropexy remained relatively stable, at 2900 procedures in 2002 and 3100 procedures in 2007, as did laparoscopic repairs, with 680 procedures in 2002 and 560 procedures in 2007. The least common procedures were the Kelly plication, which decreased from 140 procedures in 2002 to 80 in 2007, and the Pereyra procedure, which decreased from 240 procedures in 2002 to 40 in 2007.
During the study period there was an increase in procedures performed in ambulatory surgery centers from 20,220 to 26,300 (Fig. 1). All procedures were recorded as being performed at least once in all surgical settings during the study period except the Kelly placation, which was not performed in physician offices. Similarly, the number of procedures performed in physician offices increased from 3760 to 5280. Procedures performed in inpatient settings declined from 22,900 to 15,460, and those in hospital outpatient settings remained relatively stable, at 2460 procedures in 2002 and 2860 in 2007.
Figure 1.
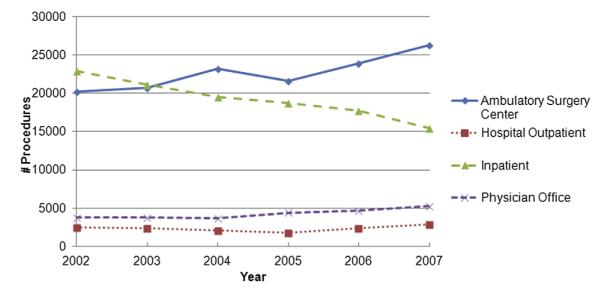
Trends in the surgical management of stress urinary incontinence by setting. (Color version available online.)
COMMENT
Our data demonstrate that although the overall number of surgical procedures performed for SUI in female Medicare beneficiaries remained stable from 2002 to 2007, there was a shift toward a dominance of outpatient procedures, including slings and injections. This shift is consistent with our previous data describing the onset of this shift from 1992 to 2001 and other data noting similar changes in other populations.5,7
Slings have become the most widely performed surgical procedure for SUI and have demonstrated good long-term durability. After successful introduction of retropubic and transobturator synthetic polypropylene slings, more than 35 additional slings have been introduced into the commercial market, although most are only minor modifications of the originals.8-10 Long-term data on the retropubic tension-free-vaginal tape (TVT; Gynecare, Somerville, NJ) for uncomplicated SUI suggest 77%-93% of patients remain cured 10 years after the sling placement.11,12 This compares to the Burch procedure, the previous standard of care for SUI surgery, which has a reported 72%-94% cure rate after 10 years.13 Randomized trials comparing the two procedures demonstrate superior outcomes with the Burch procedure14,15; however, systematic review of the literature found slings to have a long-term cure/dry rate of 84%-96% compared with 73% for the Burch procedure.1 The same review found success rates to vary by sling material and placement method and concurrent prolapse repair. Retention rates requiring intervention are similar for the two procedures (3%).1 Interestingly, the dominance of the sling procedure occurred before the presence of level I data to support its efficacy over other procedures.
A decline in surgical procedures performed in the hospital inpatient setting has been demonstrated for urinary incontinence and pelvic organ prolapse.16,17 This decline may be in part because of an increase in minimally invasive treatment options and shifts in insurance reimbursement supporting procedures in less-expensive ambulatory settings. Our results demonstrate a continued trend from that reported in the previous decade5 and we anticipate this trend will continue in future studies.
Among female Medicare beneficiaries, approximately 10% of those diagnosed with urinary incontinence undergo surgical management, which remained unchanged over the past two decades.5 The overall incidence of urinary incontinence in this population has also remained stable at approximately 37%.18,19 This finding is somewhat surprising given the significant increase found in the previous decade. Other groups have described an increase in the complexity of patients presenting to care for incontinence with current patients having more comorbidities, an increase in prior pelvic surgeries, and a greater likelihood of concomitant prolapse.1 The discrepancy between anticipated surgery rates and those demonstrated in our study may be because of the relatively short duration of the study period. We anticipate that in the coming decades, as these patients become eligible for Medicare, we will see an increase in the percentage undergoing surgical management.
Administrative data have been used in a number of studies to estimate trends in incontinence procedures in a wide variety of clinical settings; however, we recognize that it carries important limitations. When de-identified administrative data are used, it is impossible to perform complete risk adjustment and account for all possible confounding factors such as relative difficulty of procedures, subject history, and particular preferences of individual subjects and surgeons. An individual patient may have undergone more than one procedure, as is common with injectable bulking agents. Another limitation is that women were selected based on ICD-9 diagnosis and CPT-4 procedure codes that may have been inaccurately assigned. In addition, the CPT-4 code for sling procedure (57288) encompasses all slings, so we could not differentiate between minimally invasive synthetic slings and classic bladder neck slings. Medicare patients are only a subset of women who suffer from urinary incontinence, and our results may not be generalizable to the general population.
CONCLUSION
The surgical management of stress urinary incontinence among female Medicare beneficiaries shifted toward a dominance of procedures performed in ambulatory surgery centers from 2002 to 2007, although the overall number of procedures remained stable. Slings remain the dominant surgical procedure, followed by injectable bulking agents, both of which are easily performed in outpatient settings. This trend represents a continuation of the rise in slings performed in this population over the previous reporting period (1991-2002). Kelly and Pereyra procedures have declined with the fall in inpatient procedures.
Supplementary Material
Acknowledgments
Funding Support: National Institute of Diabetes and Digestive and Kidney Diseases, Grant # N01 DK012460 (MSL, CSS).
Footnotes
APPENDIX Supplementary data Supplementary data associated with this article can be found in the online version, at http://dx.doi.org/10.1016/j.urology.2012.10.087.
Financial Disclosure: The authors declare that they have no relevant financial interests.
References
- 1.Dmochowski RR, Blaivas JM, Gormley EA, et al. Update of AUA guideline on the surgical management of female stress urinary incontinence. J Urol. 2010;183:1906–1914. doi: 10.1016/j.juro.2010.02.2369. [DOI] [PubMed] [Google Scholar]
- 2.ACOG Practice Bulletin No. 63: urinary Incontinence in Women. Obstet Gynecol. 2005;105:1533–1545. doi: 10.1097/00006250-200506000-00069. [DOI] [PubMed] [Google Scholar]
- 3.Thuroff JW, Abrams P, Andersson KE, et al. EAU guidelines on urinary incontinence. Eur Urol. 2010;59:387–400. doi: 10.1016/j.eururo.2010.11.021. [DOI] [PubMed] [Google Scholar]
- 4.Rehman H, Bezerra CC, Bruschini H, et al. Traditional suburethral sling operations for urinary incontinence in women. Cochrane Database Syst Rev. 2011:CD001754. doi: 10.1002/14651858.CD001754.pub3. [DOI] [PubMed] [Google Scholar]
- 5.Anger JT, Weinberg AE, Albo ME, et al. Trends in surgical management of stress urinary incontinence among female Medicare beneficiaries. Urology. 2009;74:283–287. doi: 10.1016/j.urology.2009.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Litwin MS, Saigal CS, editors. Urologic Diseases in America. US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases; Washington, DC: 2012. Urinary incontinence; pp. 97–160. 2012. [Google Scholar]
- 7.Jonsson Funk M, Levin PJ, Wu JM. Trends in the surgical management of stress urinary incontinence. Obstet Gynecol. 2012;119:845–851. doi: 10.1097/AOG.0b013e31824b2e3e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ulmsten U, Falconer C, Johnson P, et al. A multicenter study of tension-free vaginal tape (TVT) for surgical treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1998;9:210–213. doi: 10.1007/BF01901606. [DOI] [PubMed] [Google Scholar]
- 9.Delorme E, Droupy S, de Tayrac R, et al. Transobturator tape (Uratape): a new minimally-invasive procedure to treat female urinary incontinence. Eur Urol. 2004;45:203–207. doi: 10.1016/j.eururo.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 10.Washington JL. Commercial products for pelvic repair. Female Pelvic Med Reconstr Surg. 2012;17:218–225. doi: 10.1097/SPV.0b013e31822d407a. [DOI] [PubMed] [Google Scholar]
- 11.Nilsson CG, Palva K, Rezapour M, et al. Eleven years prospective follow-up of the tension-free vaginal tape procedure for treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1043–1047. doi: 10.1007/s00192-008-0666-z. [DOI] [PubMed] [Google Scholar]
- 12.Serati M, Ghezzi F, Cattoni E, et al. Tension-free vaginal tape for the treatment of urodynamic stress incontinence: efficacy and adverse effects at 10-year follow-up. Eur Urol. 2012;61:939–946. doi: 10.1016/j.eururo.2012.01.038. [DOI] [PubMed] [Google Scholar]
- 13.Alcalay M, Monga A, Stanton SL. Burch colposuspension: a 10-20 year follow up. Br J Obstet Gynaecol. 1995;102:740–745. doi: 10.1111/j.1471-0528.1995.tb11434.x. [DOI] [PubMed] [Google Scholar]
- 14.Jelovsek JE, Barber MD, Karram MM, et al. Randomised trial of laparoscopic Burch colposuspension versus tension-free vaginal tape: long-term follow up. BJOG. 2008;115:219–225. doi: 10.1111/j.1471-0528.2007.01592.x. [DOI] [PubMed] [Google Scholar]
- 15.Tellez Martinez-Fornes M, Fernandez Perez C, Fouz Lopez C, et al. A three year follow-up of a prospective open randomized trial to compare tension-free vaginal tape with Burch colposuspension for treatment of female stress urinary incontinence. Actas Urol Esp. 2009;33:1088–1096. [PubMed] [Google Scholar]
- 16.Erekson EA, Lopes VV, Raker CA, et al. Ambulatory procedures for female pelvic floor disorders in the United States. Am J Obstet Gynecol. 2010;203:497.e1–497.e5. doi: 10.1016/j.ajog.2010.06.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu JM, Kawasaki A, Hundley AF, et al. Predicting the number of women who will undergo incontinence and prolapse surgery, 2010 to 2050. Am J Obstet Gynecol. 2011;205:230.e1–230.e5. doi: 10.1016/j.ajog.2011.03.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mardon RE, Halim S, Pawlson LG, et al. Management of urinary incontinence in Medicare managed care beneficiaries: results from the 2004 Medicare Health Outcomes Survey. Arch Intern Med. 2006;166:1128–1133. doi: 10.1001/archinte.166.10.1128. [DOI] [PubMed] [Google Scholar]
- 19.Chang CH, Gonzalez CM, Lau DT, et al. Urinary incontinence and self-reported health among the U.S. Medicare managed care beneficiaries. J Aging Health. 2008;20:405–419. doi: 10.1177/0898264308315853. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


