Abstract
The notion of applying microwave imaging to breast cancer imaging has been studied at various levels by numerous scientists. The earliest appeal of this concept related to the presumably high property contrast between benign and malignant tissue that was unique to the breast. Subsequent published studies have shown that this assumption was overly simplistic and that the tissue property heterogeneity is considerable within the breast. As we have expanded the clinical use of our microwave tomographic system, we are now using this approach to monitor tumor progressions during neoadjuvant chemotherapy. In these cases, while we can still characterize and track the tumor progression, we have observed a new phenomenon. Very often these cancer patients exhibit skin thickening near the tumor site. Our images have reconstructed elevated dielectric properties along the breast surface associated with the accompanying edema. These observations further add to the complex nature of breast dielectric properties and the challenges for imaging them using microwave interrogation.
I. INTRODUCTION
Much of our early microwave tomographic imaging work was aimed primarily at breast cancer screening and diagnosis [1]. Tumors detected in those early studies were often small and enmeshed within an otherwise normal breast. Even so, these studies provided real world experience into the level of variability and gave us confidence with our early stage imaging results. For instance, our results indicated that while both recovered properties (permittivity and conductivity) were statistically significant in distinguishing tumor from normal and benign tissue, the conductivity provided a higher level of significance [1]. Equally important, we found that denser breasts typically had higher dielectric properties and that there were often high property concentrations in our images corresponding to focal and dispersed zones of fibroglandular tissue [2].
Since then, we have also been applying our imaging technique to several new applications including monitoring of neoadjuvant chemotherapy of breast cancer [3]. For these experiments we imaged women at the start of the therapy and at regular intervals during it to determine whether the microwave images were correlating to the overall response. For this evaluation, we generally compared our images against MR images and physical exams at less frequent intervals. These examinations were quite useful for this early stage microwave tomography evaluation in that the tumors were often quite large (generally greater than 3 cm in diameter), and generally more obvious within the complex reconstructed breast images. However, we also observed artifacts along segments of the breast perimeter that we initially didn’t fully appreciate. Curiously, for quite a few women with breast cancer, there is often some level of skin thickening associated with the neoplasm. If the cancer is sufficiently advanced, large enough, and relatively close to the skin surface, the skin thickening may occur near the tumor. The extra layers of skin in this situation are often dead, but there is usually some subcutaneous edema corresponding to the associated inflammation [4]. Edema usually implies very high dielectric properties and should have a pronounced effect on the microwave images [5]. This new information builds on earlier data to paint an increasingly more complex picture of the possible dielectric properties of breast tissue [6]. From the microwave imaging technology development standpoint, visualizing this phenomenon is exciting in that it further confirms that our technology is capable of accurately recovering even more complex dielectric property distributions.
II. METHODS
Our image reconstruction algorithm is a Gauss-Newton iterative approach utilizing a log transformation [7,8] for which the minimization statement is written as:
Where Γm and Γc are the measured and computed signal log magnitudes, respectively, and Φm and Φc are the associated phase values [9]. k2 is the complex wavenumber squared where k2=ω2με+ jωμσ, ω is the frequency in radians, μ is the magnetic permeability, ε is the electrical permittivity and σ is the electrical conductivity. We utilize a circular array of monopole antennas (for the 2D reconstructions) surrounding the target immersed in a lossy coupling liquid which acts to suppress unwanted multi-path signals and simultaneously resistively loads the antennas so that they achieve good characteristic impedance (< −10dB return loss) over our full band of operation. These antennas can be readily modeled in 2D as point sources and in 3D as line sources. We have also developed mutual coupling compensation techniques for these antennas [10].
At each iteration the algorithm computes a Jacobian matrix from which the property updates are derived. The algorithm utilizes a Marquardt regularization where the associated weighting parameters have been empirically determined [11]. The strength of this algorithm stems from the log transformation where we have developed simple strategies for tracking the absolute phase values for both the measured and computed values even in the presence of phase wrapping [9]. For the measured phases, this is accomplished by recording the phases over a broad frequency range and unwrapping based on the notion that the phases measured at a single point will not vary dramatically between those at close frequencies and that at the lowest frequency, where the wavelengths are long, we can assume that all phase values fall between −π and +π. For the computed phases, we apply simple algorithms developed in the MR arena to spatially unwrap them [12]. Utilizing the log transform technique, we have not observed convergence to local minima and only initiate the algorithm with the uniform distribution of the background medium (i.e. no a priori information).
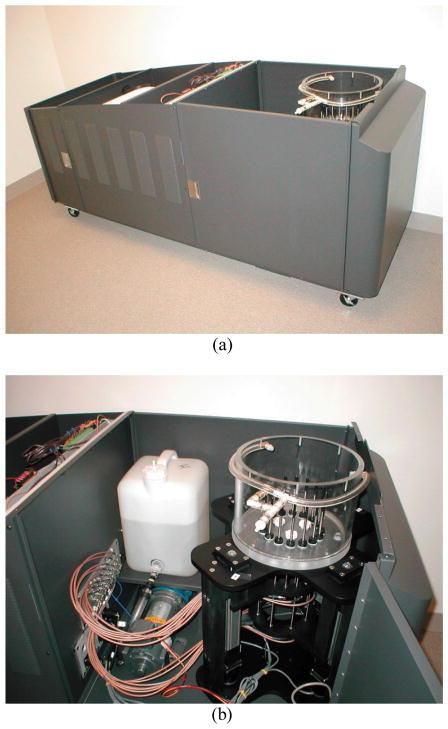
For these images we used our microwave tomographic imaging system with an 86:14 mixture of glycerin and water as the coupling bath. For this patient’s breast density, this liquid was a suitable medium. Figure 1 includes photographs of the system without the bed to the relationship of the imaging tank to the associated data acquisition electronics. The 16 monopole antennas were positioned around the breast on a 15.2 cm circle and could be moved to multiple vertical heights via computer controlled motors. At each of the 7 vertical positions (separated by 1 cm increments) each transmitter broadcast a continuous wave (CW) signal, which was detected in parallel by the remaining 15 antennas for a total of 240 measurements per imaging plane. This data acquisition was repeated at all planes for seven frequencies from 500 to 1700 MHz in 200 MHz increments. The total exam time was roughly 4 minutes for each breast.
Figure 1.
Photographs of the microwave breast imaging system: (a) full system with bed removed, and (b) tank and pump compartment – microwave electronics are behind the firewall to the left.
The 2D images were reconstructed using our finite difference time domain (FDTD)-based algorithm with log transformation that allows us to reconstruct un-biased images without the use of a priori information [7,8,13]. For a single, 2D planar image and allowing the algorithm to run for 13 iterations, the reconstruction time was under 1 minute using a single processor in a Dell Blade workstation.
III. RESULTS
For this test case, the woman being imaged was 60 years old, had radiographically scattered density breasts and a 3.9 × 2.6 × 4.2 cm tumor in her right breast located 7.5 cm from the nipple. The MR and microwave images shown here are for the baseline set before treatment. Figures 3a, b and c show the T2 weighted, gadolinium enhanced, and subtraction axial images of the breasts, respectively. The difference image is formed by subtracting the fat-suppressed T1 image prior to contrast agent infusion from the same after infusion. It is difficult to distinguish the tumor from the fibroglandular tissue in just the T2 image. It is more pronounced in the gadolinium enhanced, T1 image but it is still difficult to separate out from the fibroglandular. Only the difference image truly separates the tumor from the remainder of the normal tissue. Interestingly, the skin thickening effect is visible in both the T2 and T1- fat-suppressed images, but not in the subtraction image. This is because the edema would appear similarly during the full course of the gadolinium infusion so that a difference image would subtract out its presence while the dynamic nature of the tumor washout behavior would be quite different over time allowing for enhancement of just the tumor zone. This is a quite complex imaging problem in that there is a substantial amount of fibroglandular tissue, a large tumor and a considerable span of edema under the thickened skin.
Figure 3.

(a) Axial view of the T2-weighted right breast, (b) gadolinium-enhanced T1-weighted, fat-suppressed axial view of both breasts, and (c) subtraction images for the axial view of both breasts.
Figures 2a and b show the en face 1300 MHz reconstructed permittivity and conductivity images for planes 1–5 (Plane 1 is closest to the chestwall and the subsequent planes are separated in 1 cm increments) for the right and left breasts, respectively, for this volunteer just prior to treatment. In the right breast conductivity (σ) images, the breast region is reasonably visible as a large low property zone, which shrinks in size in progression from the chestwall (plane 1) towards the nipple with two enhancing features inside its boundary. For the permittivity (εr) images there is a local elevated property region roughly at 10:00 for all five planes and a secondary focal zone at 4:00 for planes 4 and 5. The corresponding conductivity images show two enhanced spots in the same locations as the εr image. We hypothesize that the upper left one is the tumor and the latter a concentration of fibroglandular tissue. In addition, along the lower right surface of the breast contour there is a band of quite high values in both permittivity and conductivity image sets. This correlates well with the edema viewed in the MR images. It should be noted that this feature did disappear along with the tumor after therapy. The corresponding imaging sets for the contralateral breast (left) also show large low property, round regions corresponding to the breast usually with only a single enhancing spot and rising to less subdued levels than for the right breast. These also shrink in size from chestwall towards the nipple. The breast perimeters in the permittivity images are not as easily discernible given the various internal features observable. None of these features rise to the level of the tumor as seen in the right breast images. As hypothesized earlier [2], we have consistently observed that the permittivity images are better indicators of the fibroglandular tissue while the conductivity images do not enhance as much for this tissue. There also appears to be a ring-like elevated property artifact surrounding the breast. This tends to surround the entire breast and doesn’t seem to rise to the elevated values for that in the right breast. We suspect this is more consistent with normal imaging artifacts when reconstructing a large, high contrast object such as the breast. The comparison of the right and left breast images suggests that the elevated properties around only a portion of the right breast are really due to the subcutaneous edema.
Figure 2.
1300 MHz reconstructed permittivity (top row) and conductivity (bottom row) images for planes 1–5 of the (a) right and (b) left breasts.
IV. CONCLUSION
As demonstrated in various studies, we have shown that microwave imaging can be a powerful tool for breast cancer imaging. As we proceed, it is clear that the breast dielectric properties can vary widely with almost arbitrary distributions. More recently in conjunction with our neoadjuvant chemotherapy trial, we have shown that the property distributions can be even more complex than recent publications suggest, especially in the presence of skin-thickening associated edema. It is particularly encouraging that these important features in the breast are visible even under our 2D imaging configuration. While various groups have proposed and worked towards full 3D imaging of the breast for several years, our 2D approach remains the state of the art with respect to actual clinical imaging. There is no doubt that 3D imaging is the future for microwave imaging; however, it is also clear that 2D imaging has made an important mark in this ongoing research and will continue to do so for clinical exams for the near future.
Acknowledgments
This work was supported by NIH/NCI Grant PO1-CA080139.
Contributor Information
Paul M. Meaney, School of Engineering at Dartmouth College, Hanover, NH USA
Margaret W. Fanning, School of Engineering at Dartmouth College, Hanover, NH USA
Roberta M. di Florio-Alexander, Dartmouth Hitchcock Medical Center in Lebanon, NH USA
Peter A. Kaufman, Dartmouth Hitchcock Medical Center in Lebanon, NH USA
Shireen D. Geimer, School of Engineering at Dartmouth College, Hanover, NH USA
Tian Zhou, School of Engineering at Dartmouth College, Hanover, NH USA.
Keith D. Paulsen, School of Engineering at Dartmouth College, Hanover, NH USA
References
- 1.Poplack SP, Paulsen KD, Hartov A, Meaney PM, Pogue B, Tosteson T, Grove M, Soho S, Wells W. Electromagnetic breast imaging: pilot results in women with abnormal mammography. Radiology. 2007;243:350–359. doi: 10.1148/radiol.2432060286. [DOI] [PubMed] [Google Scholar]
- 2.Meaney PM, Fanning MW, Raynolds T, Fox CJ, Fang Q, Kogel CA, Poplack SP, Paulsen KD. Initial clinical experience with microwave breast imaging in women with normal mammography. Academic Radiology. 2007;14:207–218. doi: 10.1016/j.acra.2006.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meaney PM, Kaufman PA, Muffly LS, Poplack SP, Geimer SD, Kogel CA, Fanning MW, Zhou T, Paulsen KD. Microwave imaging for neoadjuvant chemotherapy monitoring: initial clinical experience. Breast Cancer Research and Treatment. 2009 doi: 10.1186/bcr3418. (submitted) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shaw E. deParedes, Atlas of Mammography. Lippincott, Williams and Wilcox; Philadelphia, PA: 2007. [Google Scholar]
- 5.Foster KR, Schepps JL. Dielectric properties of tumor and normal tissues at radio through microwave frequencies. Jourmal of Microwave Power. 1981;16:107–119. doi: 10.1080/16070658.1981.11689230. [DOI] [PubMed] [Google Scholar]
- 6.Lazebnik M, Popovic D, McCartney L, Watkins CB, Lindstrom MJ, Harter J, Sewall S, Ogilvie T, Magliocco A, Breslin TM, Temple W, Mew D, Booske JH, Okoniewski M, Hagness SC. A large-scale study of the ultrawideband microwave dielectric properties of normal, benign and malignant breast tissues obtained from cancer surgeries. Physics in Medicine and Biology. 2007;52:6093–6115. doi: 10.1088/0031-9155/52/20/002. [DOI] [PubMed] [Google Scholar]
- 7.Box GEP, Cox DR. An analysis of transformations. J R Stat Soc Ser B – Methodol. 1964;35:211–252. [Google Scholar]
- 8.Meaney PM, Fang Q, Rubaek T, Demidenko E, Paulsen KD. Log transformation benefits parameter estimation in microwave tomographic imaging. Medical Physics. 2007;34:2014–2023. doi: 10.1118/1.2737264. [DOI] [PubMed] [Google Scholar]
- 9.Meaney PM, Paulsen KD, Pogue BW, Miga MI. Microwave image reconstruction utilizing log-magnitude and unwrapped phase to improve high-contrast object recovery. IEEE Trans Medical Imaging. 2001;20:104–116. doi: 10.1109/42.913177. [DOI] [PubMed] [Google Scholar]
- 10.Paulsen KD, Meaney PM. Compensation for nonactive array element effects in a microwave imaging system: part I – forward solution vs. measured data comparison. IEEE Trans on Med Imag. 1999;18:496–507. doi: 10.1109/42.781015. [DOI] [PubMed] [Google Scholar]
- 11.Meaney PM, Paulsen KD, Hartov A, Crane RK. An active microwave imaging system for reconstruction of 2-D electrical property distributions. IEEE Trans Biomed Eng. 1995;42:1017–1026. doi: 10.1109/10.464376. [DOI] [PubMed] [Google Scholar]
- 12.Glover GH, Schneider E. Three-point Dixon technique for true water/fat decomposition with B inhomogeneity correction. Magn Reson Med. 1991;18:371–383. doi: 10.1002/mrm.1910180211. [DOI] [PubMed] [Google Scholar]
- 13.Taflove A, editor. Computational electrodynamics: the finite difference time domain method. Artech House; Boston, MA: 1995. [Google Scholar]