Abstract
Background
Hip resurfacing is an alternative to total hip arthroplasty.
Questions/Purpose
We aimed to compare an experienced hip surgeon’s initial clinical results of hip resurfacing with a new cementless total hip arthroplasty (THA).
Methods
The first 55 consecutive hip resurfacing arthroplasties were compared to 100 consecutive cementless THAs using a cylindrical tapered femoral stem. The learning curve between the two procedures was compared utilizing the incidence of reoperation, complications, Harris Hip Scores (HHS), and implant survivorship.
Results
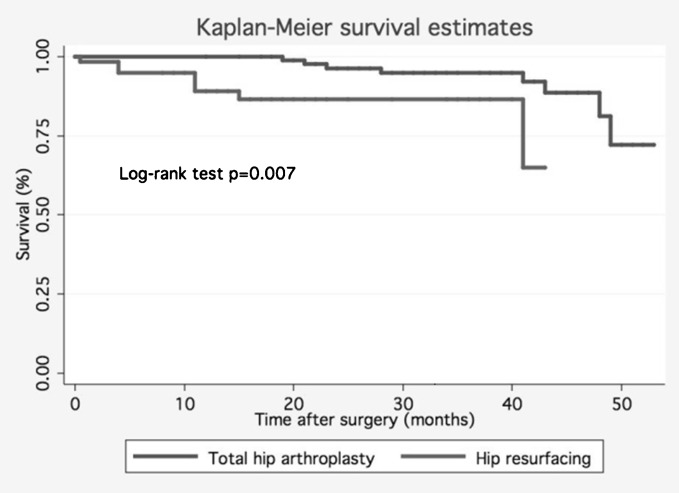
The reoperation rate was significantly higher (p = 0.019) for hip resurfacing (14.5%) versus THA (4%). The overall complication rate between the two groups was not significantly different (p = 0.398). Preoperative HHS were similar between the two groups (p = 0.2). The final mean HHS was similar in both the resurfacing and THA groups (96 vs. 98.3, respectively, p < 0.65). Kaplan–Meier survival analysis with an endpoint of reoperation suggests complications occurred earlier in the resurfacing group versus the THA group (log-rank test, p = 0.007).
Conclusions
In comparison to our initial experience with a cementless THA stem, operative complications occur earlier and more often after hip resurfacing during the learning period. The clinical outcomes in both groups however are similar at 5 year follow-up.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-013-9333-0) contains supplementary material, which is available to authorized users.
Keywords: hip resurfacing, total hip arthroplasty, learning curve
Introduction
An increase in younger, high-demand patients requesting surgical intervention for hip arthrosis has developed with the baby-boomer population [20]. End-stage arthritis of the hip in patients who have exhausted nonsurgical management has traditionally been treated with conventional total hip arthroplasty (THA). However, failure does occur as a result of aseptic loosening, bone loss, and wear-related osteolysis [7]. Nevertheless, cementless THA and hip resurfacing remain popular options to manage hip arthritis [14]. Press fit, cementless femoral stems represent the standard of care for this population undergoing conventional THA with reproducible, satisfactory results [24]. Fiber metal taper (Zimmer, Warsaw, IN, USA) stems are associated with successful results in cementless THA [1, 23]. Despite excellent long and intermediate term results associated with THA, important long-term concerns such as: dislocation, activity restrictions, future revision, and leg length discrepancy have lead many patients to consider hip resurfacing.
Metal-on-metal hip resurfacing presents an alternative to total hip arthroplasty which may allow patients the potential to return to their presurgical activities without restrictions due to lower rates of dislocation [3, 25], improved wear rates [9, 15], conservation of bone stock [12, 28], and better preservation of femoral anatomy [16, 17]. Early generation hip resurfacing was associated with historically unacceptable rates of failure primarily due to rapid wear and osteolysis related to the conventional bearing surfaces [11, 19]. Current generation implants, utilizing larger, cobalt–chromium femoral heads with metal-on-metal bearing surfaces, have generated interest in this procedure with potentially improved wear rates [10]. Hip resurfacing does however have associated complications including femoral neck fracture [4], generation of metal ions [21], and loosening secondary to osteonecrosis [8]. Some studies have demonstrated short-term results with similar complication and reoperation rates but clinically superior postoperative activity scores and range of motion after hip resurfacing [27].
Little midterm data exists describing the surgeon’s initial experience with hip resurfacing using current generation implants compared with conventional, cementless THA [26]. The purpose of this investigation is to compare (1) the incidence of reoperation, (2) complications, (3) Harris Hip Score (HHS), and (4) survivorship during one surgeon’s initial experience with adopting hip resurfacing in comparison to a new, cementless THA.
Materials and Methods
We retrospectively reviewed the first 55 consecutive patients who underwent metal-on-metal hip resurfacing utilizing the Conserve Plus prosthesis (Wright Medical Technology, Arlington, TN, USA) from 2002 to 2005 in our institution. We compared this group to our first 97 patients who underwent total hip arthroplasty utilizing 100 fibermetal taper stems between 1997 and 2001 (Zimmer). All procedures were performed in a consecutive series by the senior author (VMG) at a single institution with clinical data being gathered prospectively.
Hip resurfacing was indicated in high demand patients with hip arthrosis but without femoral or acetabular deficiency. The mean age was 49.6 years (range, 29–70 years). There were 38 men and 17 women who had resurfacing performed. The etiology was osteoarthritis (OA) in 46 patients, osteonecrosis in 1 patient, posttraumatic arthritis in 2 patients, and developmental dysplasia in 6 patients. All patients were followed for a minimum of 31 months (mean, 50.3 months; range, 31–70 months; Table 1). No patient was lost to follow-up in the hip resurfacing group.
Table 1.
Preoperative clinical features of the resurfacing versus total hip arthroplasty groups
| Parameter | THA | Resurfacing | p Value |
|---|---|---|---|
| Sex | |||
| Male | 74 | 38 | |
| Female | 26 | 17 | |
| Bilateral procedures | 3 | 0 | |
| Total procedures | 100 | 55 | |
| Age (years) | 56.5 (33–73) | 49.6 (29–70) | <0.001 |
| Diagnosis | |||
| Osteoarthritis | 83 | 46 | |
| Osteonecrosis | 8 | 1 | |
| Rheumatoid arthritis | 0 | 0 | |
| Developmental dysplasia | 9 | 6 | |
| Post-traumatic arthritis | 0 | 2 | |
| Follow-up mean (range) | 56.8 months | 48.6 months | |
| Revision operation needed | 4 | 8 | 0.019 |
In the total hip arthroplasty group, one patient died at 1.3 years postoperatively from unrelated medical causes and was excluded from the study. Ninety-seven patients (100 hips) returned for follow-up with a mean of 6.0 years (range, 3.9–9 years). The mean age in the entire THA group was 56.5 years (range, 33.7–73.5). Eighty-three patients had a diagnosis of primary osteoarthritis. The remaining patients had secondary osteoarthritis from osteonecrosis or developmental dysplasia of the hip.
The Conserve Plus® prosthesis (Wright Medical Technology) was utilized in all cases of hip resurfacing. The implant system is a high carbon cast cobalt–chrome one-piece cup with a porous coating for the acetabular component. A detailed description of the prosthesis has been published [2–5].
All of the hip resurfacing cases were performed using the technique as described by Amstutz et al. via a posterior approach [2, 5]. All cups were implanted with a 1 mm press fit. Postoperative management included 50% weight bearing restriction for the first six postoperative weeks. All patients participated in inpatient physical therapy programs after surgery until discharge.
In the total hip arthroplasty group, the VERSYS® fibermetal taper (FMT) stem (Zimmer) was utilized. This system is characterized by a fibermetal layer proximally and a roughened, grit-blasted surface in the midportion of the stem. Distally, the stem is polished to discourage distal fixation and tapered to increase flexibility and avoid contact with cortical bone in narrow femurs. Femoral head sizes varied from 28 to 36 mm in diameter in 4-mm increments. All THA patients had a porous cup (Trilogy; Zimmer) with an ultrahigh-molecular-weight cross-linked polyethylene liner sterilized by gamma irradiation in nitrogen ranging in size from 48 to 66 mm (Longevity; Zimmer). The acetabular fixation was achieved with 1 mm press fit with one to three screws. The fibermetal taper stems were inserted using the technique previously described [1]. Total hip arthroplasties were performed through a standard posterolateral approach to the hip. After THA, patients were kept 50% weight bearing for 6 weeks after which they proceeded with weight bearing as tolerated.
Both the resurfacing and total hip arthroplasty patients received the same deep venous thrombosis/pulmonary embolism (DVT/PE) and infection prophylaxis regimens. Anticoagulation with oral warfarin to maintain an international normalized ratio of 2.0 was initiated on the postoperative evening and continued for 3 weeks. Prophylactic antibiotics were administered intravenously prior to incision and for a course of 24 h postoperatively with cefazolin or vancomycin in the case of cephalosporin allergy. In-patients wore antithromboembolic stockings and were managed with sequential compression devices on both legs. All procedures in both groups were performed in a laminar airflow operating room and the surgeons wore body exhaust isolation suits. Suction drains were utilized in both groups.
All patients were evaluated at 3 and 5 months postoperatively, then at 2-year intervals thereafter. Examination findings were confirmed by the senior author (VMG) and a research nurse. During each visit pain, function, and activity were evaluated via HHS [18]. Collected patient data was also reviewed for complications defined in this study as: fracture, DVT/PE, dislocation, aseptic loosening, periprosthetic infection, and other.
Unpaired, two-tailed Student’s t tests were utilized to compare variables between the two study groups; a paired Student’s t test was used within groups. A Kaplan–Meier survivorship analysis was performed with reoperation as an endpoint. The log-rank test was used to evaluate the differences between survival curves. All p values <0.05 were considered significant.
Results
The reoperation rates for the THA and resurfacing groups were significantly different, 4 versus 14.5%, respectively (p = 0.019). Eight patients in the resurfacing group required revision operations. Three (5.5%) resurfacing patients sustained femoral neck fractures. Fractures occurred at 1 week, 8 months, and 14 months from the index procedure. In this series, the last patient to undergo reoperation after hip resurfacing was the 55th of 92 consecutive cases. All hips were revised through a posterolateral approach. Two cases were revised with cementless, press fit proximally coated femoral stems and one was revised with a cemented femoral stem. Four (7.3%) patients developed aseptic loosening and were revised to THA. A single resurfacing patient, 4 years status post the index procedure, presented with signs and symptoms of impingement. The patient was revised to total hip arthroplasty utilizing an extensively coated femoral stem with a porous acetabular revision shell. There were no dislocations after conversion of these failed hip resurfacing cases.
Four patients from the THA group required revision operations. One patient, 6 months postoperatively, sustained a greater trochanter fracture after a fall. This patient underwent open reduction with internal fixation with a hook plate and cerclage wiring. Two THA patients underwent acetabular shell revision for recurrent instability. One patient in the THA group, 4 years postoperatively, sustained a fracture of a zirconium femoral head which was replaced with a cobalt–chromium head at the time of revision (Table 2).
Table 2.
Complications compared between THA and resurfacing groups
| Parameter | THA (%) | Resurfacing (%) | p Value |
|---|---|---|---|
| Fracture | 6 (6) | 3 (5.5) | 1.00 |
| DVT/PE | 0 | 0 | Not applicable |
| Dislocation | 2 (2) | 0 | 0.54 |
| Aseptic loosening | 0 | 4 (7.3) | 0.02 |
| Joint infection | 0 | 0 | Not applicable |
| Other | 2 (2) | 1 (1.8) | 1.00 |
| Total number | 10 (10) | 8 (14.5) | 0.44 |
The total complication rates for the THA and resurfacing groups were not significantly different (p = 0.44). Six (6%) THA patients sustained incomplete intraoperative femoral fractures without extension distal to the lesser trochanter (Table 2). The fractures occurred during the preparation of the canal while using the broach in three cases. The other three fractures were noted upon final impaction of the femoral stem. A stem diameter of 16 mm or larger was utilized in four of the patients who sustained fractures. Four of the fractures occurred during the first 50 procedures while two occurred in the final 47. All fractures were treated with one or two cerclage cables below the level of the fracture. There was no stem subsidence or further complications associated with these fractures. Similarly, there were no cases of aseptic loosening within the THA group at last follow-up.
Preoperative HHS were similar at 58 for the THA group and 55.7 for all the patients in the resurfacing group (p = 0.2). Upon most recent follow-up, HHSs were significantly improved (p < 0.005) with scores of 98.3 and 96.0 for the THA group and resurfacing group, respectively. The mean final HHS for the six THA patients who sustained periprosthetic fractures during the index case was 97 (range, 87–100).
Survival analysis utilizing Kaplan–Meier survival estimates with reoperation for the end point revealed complications in the hip resurfacing group occurred earlier in the postoperative course compared to the total hip arthroplasty group (log-rank test p = 0.007; Fig. 1).
Fig. 1.
Kaplan–Meier survivorship curves using time of reoperation for any reason as the end point reveals complications in the resurfacing group occur earlier in the postoperative course compared to the total hip arthroplasty group.
Discussion
This study was unique in that we compared an experienced hip surgeon’s results between a new cementless total hip arthroplasty and contemporary MOM hip resurfacing. Although the rate of complication was similar in both groups, the higher reoperation rate after hip resurfacing suggests that this novel procedure is different enough from THA to justify additional training measures with this relatively new procedure [13]. We quantified the pitfalls of either procedure by comparing reoperation, complications, hip scores, and overall survivorship. In regards to reoperation, we identified a notable difference between the two groups. The resurfacing group demonstrated earlier revisions whereas the total hip arthroplasty group demonstrated fewer complications of which even fewer went on to revision. A similar trend was demonstrated by Scandinavian registry data [22].
The limitations of this investigation stemmed from comparisons made between the groups. Namely, the age at index surgery was older among THA patients versus hip resurfacing with mean ages of 56.5 and 49.6, respectively (p < 0.001). Similarly, the length of follow-up was longer among THAs versus hip resurfacing. It is possible that additional complications associated with hip resurfacing may have been encountered with equal follow-up. This difference reflects our institutional practice pattern and the specific indications for hip resurfacing. In this analysis, we included the four reoperations after THA for the sake of accurate reporting. However, the greater trochanter fracture after a fall is not necessarily attributable to the implant or index procedure. Whereas, the two dislocations and one ceramic head fracture were intrinsic to the total hip arthroplasty arm of this investigation. Also, a true quantification of a surgeon’s learning curve can be difficult to obtain. Therefore, we quantified the effect of surgeon experience on these two procedures using clinical results and the type and timing of surgical complications. Similarly, Callaghan et al. demonstrated superior radiographic results including femoral canal fill and acetabular abduction during the surgeon’s second 50 cementless THAs versus initial 50 cementless THAs [6]. Other markers such as operative time, length of stay, and surgical blood loss could be valuable in future investigations. However, we reported (1) reoperations, (2) complications, (3) hip scores, and (4) survivorship because they reflect the ultimate success of the surgeon and procedure.
The complications associated with each procedure are quite distinct (Table 2). The THA patients were more likely to have intraoperative femur fractures, which occurred and were fixed during the index operation. Fracture rate for this initial cementless THA experience was 6%, pattern and timing were amenable to fixation during the index procedure. Fracture rates then were diminished without any clinical impact on the patient or revision requirements. In contrast, hip resurfacing patients demonstrated a 5.5% fracture rate; however, these occurred after the index procedure and required a revision surgery.
The individual surgeon’s learning curve ranges from 25 to over 100 cases depending on outcome measure [26]. Our initial experience of 92 cases of hip resurfacing suggests that approximately 55 cases represent the threshold for complications leading to early revision. Similarly, the rate of intraoperative femur fracture dropped by 50% from the first 50 to the subsequent 50 cases in the total hip arthroplasty group. This study and current data on the US experience with hip resurfacing suggest that even experienced hip surgeons should expect a learning curve associated with this new procedure [13, 26].
Electronic Supplementary Material
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)
Acknowledgments
We would like to acknowledge Sam Akhavan MD for his assistance with the study design. We would like to acknowledge Patty Conroy-Smith for her assistance with clinical data.
Disclosures
ᅟ
Conflict of Interest:
Justin Arndt, BS and Glenn D. Wera, MD have declared that they have no conflict of interest. Victor M. Goldberg MD is a paid consultant for Zimmer (Warsaw, Indiana) and Wright Medical (Arlington, TN), outside the work.
Human/Animal Rights:
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent:
Informed consent was waived for all patients included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Work was performed at University Hospitals Case Medical Center; Case Western Reserve University Cleveland, OH.
Level of Evidence: Therapeutic Study Level III. Please see Levels of Evidence for a complete description.
References
- 1.Akhavan S, Goldberg VM. Clinical outcome of a fibermetal taper stem: minimum 5-year followup. Clin Orthop Relat Res. 2007;465:106–111. doi: 10.1097/BLO.0b013e3181576080. [DOI] [PubMed] [Google Scholar]
- 2.Amstutz HCBP, Le Duff M. Hybrid metal on metal surface arthroplasty of the hip. Oper Tech Orthop. 2001;11:253–262. doi: 10.1016/S1048-6666(01)80039-2. [DOI] [Google Scholar]
- 3.Amstutz HC, Grigoris P, Dorey FJ. Evolution and future of surface replacement of the hip. J Orthop Sci. 1998;3:169–186. doi: 10.1007/s007760050038. [DOI] [PubMed] [Google Scholar]
- 4.Amstutz HC, Beaule PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg Am. 2004;86-A:28–39. [PubMed] [Google Scholar]
- 5.Amstutz HC, Beaule PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty. Surgical technique. J Bone Joint Surg Am. 2006;88(Suppl 1 Pt 2):234–249. doi: 10.2106/JBJS.F.00273. [DOI] [PubMed] [Google Scholar]
- 6.Callaghan JJ, Heekin RD, Savory CG, Dysart SH, Hopkinson WJ. Evaluation of the learning curve associated with uncemented primary porous-coated anatomic total hip arthroplasty. Clin Ortho Relat Res. 1992;282:132–44. [PubMed] [Google Scholar]
- 7.Callaghan JJ, Bracha P, Liu SS, Piyaworakhun S, Goetz DD, Johnston RC. Survivorship of a Charnley total hip arthroplasty. A concise follow-up, at a minimum of thirty-five years, of previous reports. J Bone Joint Surg Am. 2009;91:2617–2621. doi: 10.2106/JBJS.H.01201. [DOI] [PubMed] [Google Scholar]
- 8.Campbell P, Mirra J, Amstutz HC. Viability of femoral heads treated with resurfacing arthroplasty. J Arthroplast. 2000;15:120–122. doi: 10.1016/S0883-5403(00)91415-3. [DOI] [PubMed] [Google Scholar]
- 9.Chan FW, Bobyn JD, Medley JB, Krygier JJ, Yue S, Tanzer M. Engineering issues and wear performance of metal on metal hip implants. Clinical Ortho Relat Res. 1996;333:96–107. [PubMed] [Google Scholar]
- 10.Chan FW, Bobyn JD, Medley JB, Krygier JJ, The TM, Otto Aufranc Award Wear and lubrication of metal-on-metal hip implants. Clin Ortho Relat Res. 1999;369:10–24. doi: 10.1097/00003086-199912000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Charnley J. Arthroplasty of the hip. A new operation. Lancet. 1961;1:1129–1132. doi: 10.1016/S0140-6736(61)92063-3. [DOI] [PubMed] [Google Scholar]
- 12.Crawford JRPS, Wimhurst JA, Villar RN. Bone loss at hip resurfacing: a comparison with total hip arthroplasty. Hep Int. 2005;15:195–198. doi: 10.1177/112070000501500411. [DOI] [PubMed] [Google Scholar]
- 13.Della Valle CJ, Nunley RM, Raterman SJ, Barrack RL. Initial American experience with hip resurfacing following FDA approval. Clin Orthop Relat Res. 2009;467:72–78. doi: 10.1007/s11999-008-0563-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dorr LD, Kane TJ, 3rd, Conaty JP. Long-term results of cemented total hip arthroplasty in patients 45 years old or younger. A 16-year follow-up study. J Arthroplast. 1994;9:453–456. doi: 10.1016/0883-5403(94)90090-6. [DOI] [PubMed] [Google Scholar]
- 15.Dowson D, Hardaker C, Flett M, Isaac GH. A hip joint simulator study of the performance of metal-on-metal joints: Part I: the role of materials. J Arthroplast. 2004;19:118–123. doi: 10.1016/j.arth.2004.09.015. [DOI] [PubMed] [Google Scholar]
- 16.Girard J, Lavigne M, Vendittoli PA, Roy AG. Biomechanical reconstruction of the hip: a randomised study comparing total hip resurfacing and total hip arthroplasty. J Bone Joint Surg Br. 2006;88:721–726. doi: 10.2106/JBJS.E.00550. [DOI] [PubMed] [Google Scholar]
- 17.Gore DR, Murray MP, Gardner GM, Sepic SB. Hip function after total vs. surface replacement. Acta Orthop Scand. 1985;56:386–390. doi: 10.3109/17453678508994353. [DOI] [PubMed] [Google Scholar]
- 18.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 19.Head WC. Wagner surface replacement arthroplasty of the hip. Analysis of fourteen failures in forty-one hips. J Bone Joint Surg Am. 1981;63:420–427. [PubMed] [Google Scholar]
- 20.Iorio R, Robb WJ, Healy WL, et al. Orthopaedic surgeon workforce and volume assessment for total hip and knee replacement in the United States: preparing for an epidemic. J Bone Joint Surg Am. 2008;90:1598–1605. doi: 10.2106/JBJS.H.00067. [DOI] [PubMed] [Google Scholar]
- 21.Jacobs JJ, Skipor AK, Doorn PF, et al. Cobalt and chromium concentrations in patients with metal on metal total hip replacements. Clin Ortho Relat Res. 1996;329:S256–263. doi: 10.1097/00003086-199608001-00022. [DOI] [PubMed] [Google Scholar]
- 22.Johanson PE, Fenstad AM, Furnes O, et al. Inferior outcome after hip resurfacing arthroplasty than after conventional arthroplasty. Evidence from the Nordic Arthroplasty Register Association (NARA) database, 1995 to 2007. Acta Orthop. 2010;81:535–541. doi: 10.3109/17453674.2010.525193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Klein GR, Levine HB, Nafash SC, Lamothe HC, Hartzband MA. Total hip arthroplasty with a collarless, tapered, fiber metal proximally coated femoral stem: minimum 5-year follow-up. J Arthroplast. 2009;24:579–585. doi: 10.1016/j.arth.2008.04.010. [DOI] [PubMed] [Google Scholar]
- 24.McLaughlin JR, Lee KR. Total hip arthroplasty with an uncemented tapered femoral component. J Bone Joint Surg Am. 2008;90:1290–1296. doi: 10.2106/JBJS.G.00771. [DOI] [PubMed] [Google Scholar]
- 25.McMinn D, Treacy R, Lin K, Pynsent P. Metal on metal surface replacement of the hip. Experience of the McMinn prothesis. Clin Ortho Related Res. 1996;329:S89–98. doi: 10.1097/00003086-199608001-00009. [DOI] [PubMed] [Google Scholar]
- 26.Nunley RM, Zhu J, Brooks PJ, et al. The learning curve for adopting hip resurfacing among hip specialists. Clin Orthop Relat Res. 2010;468:382–391. doi: 10.1007/s11999-009-1106-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vail TP, Mina CA, Yergler JD, Pietrobon R. Metal-on-metal hip resurfacing compares favorably with THA at 2 years followup. Clin Orthop Relat Res. 2006;453:123–131. doi: 10.1097/01.blo.0000238852.08497.92. [DOI] [PubMed] [Google Scholar]
- 28.Vendittoli PA, Lavigne M, Girard J, Roy AG. A randomised study comparing resection of acetabular bone at resurfacing and total hip replacement. J Bone Joint Surg Br. 2006;88:997–1002. doi: 10.2106/JBJS.E.00173. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 510 kb)
(PDF 510 kb)
(PDF 510 kb)