Abstract
Context
Interpersonal psychotherapy (IPT) is an effective specialty treatment for binge eating disorder (BED). Behavioral weight loss treatment (BWL) and guided self-help based on cognitive behavior therapy (CBTgsh) have both resulted in short-term reductions in binge eating in obese patients with BED.
Objective
To test whether patients with BED require specialty therapy beyond BWL and whether IPT is more effective than either BWL or CBTgsh in patients with a high negative affect during a 2-year follow-up.
Design
Randomized, active control efficacy trial.
Setting
University outpatient clinics.
Participants
Two hundred five women and men with a body mass index between 27 and 45 who met DSM-IV criteria for BED.
Intervention
Twenty sessions of IPT or BWL or 10 sessions of CBTgsh during 6 months.
Main Outcome Measures
Binge eating assessed by the Eating Disorder Examination.
Results
At 2-year follow-up, both IPT and CBTgsh resulted in greater remission from binge eating than BWL (P < .05; odds ratios: BWL vs CBTgsh, 2.3; BWL vs IPT, 2.6; and CBTgsh vs IPT, 1.2). Self-esteem (P < .05) and global Eating Disorder Examination (P < .05) scores were moderators of treatment outcome. The odds ratios for low and high global Eating Disorder Examination scores were 2.8 for BWL, 2.9 for CBTgsh, and 0.73 for IPT; for self-esteem, they were 2.4 for BWL, 1.9 for CBTgsh, and 0.9 for IPT.
Conclusions
Interpersonal psychotherapy and CBTgsh are significantly more effective than BWL in eliminating binge eating after 2 years. Guided self-help based on cognitive behavior therapy is a first-line treatment option for most patients with BED, with IPT (or full cognitive behavior therapy) used for patients with low self-esteem and high eating disorder psychopathology.
Trial Registration
clinicaltrials.gov Identifier: NCT00060762
In 1994, binge eating disorder (BED) was included in DSM-IV1 as a provisional eating disorder. Extensive research has since demonstrated its clinical significance and validity.2–3 Binge eating disorder is characterized by frequent and persistent episodes of binge eating accompanied by feelings of loss of control and marked distress in the absence of regular compensatory behaviors. The disorder is associated with specific eating disorder psychopathology (eg, dysfunctional body shape and weight concerns),4 psychiatric comorbidity, and significant health and psychosocial impairments.5 Binge eating disorder is also linked with overweight and obesity.6
Cognitive behavior therapy (CBT) and interpersonal psychotherapy (IPT) are specialty therapies for BED that directly target the eating disorder. Well-controlled studies have demonstrated that these therapies are reliably effective in eliminating binge eating and reducing associated psychopathology in the short- and longer-term, but do not on average produce clinically significant weight loss.7–8 Behavioral weight loss treatment (BWL) is widely used to treat obesity, including binge eating, via moderate caloric restriction, improved nutrition, and increased physical activity.9
Early studies comparing BWL with specialty CBT in the treatment of BED indicated comparable effects on binge eating in the short-term,10–11 but long-term evaluations were lacking. Obesity researchers who included measures of binge eating in studies on obesity treatment concluded that BWL was effective and that there was no need for specialty therapies.12–13 Limitations of these studies included small sample sizes, lack of longer-term follow-up, and self-report measures of binge eating rather than the Eating Disorder Examination (EDE) semi-structured interview.14 Potential advantages of BWL are that it results in clinically significant short-term weight loss and can be implemented by a wider range of health professionals than a specialty psychological therapy.
Guided self-help based on cognitive behavior therapy (CBTgsh) is designed to eliminate binge eating. The promising results of early research15–16 have been supported by more recent studies17–18 showing that CBTgsh is effective in the short-term in reducing binge eating. As a brief intervention that can be used by nonspecialist health providers,19 CBTgsh is cost-effective, an appealing option when specialty treatment is unavailable, and suitable as a first treatment in a stepped-care program.20
It is a research priority to identify predictors and moderators of treatment outcome.21 Cluster analyses of patients with BED have revealed 2 subtypes characterized by low and high negative affect.22 The high negative affect subtype has more severe eating disorder psychopathology and greater psychiatric comorbidity.22–23 This subtyping has proved superior to categorical diagnoses of depression23 and has been shown to predict treatment outcome.22
The current study compared the short- and longer-term outcomes of 3 treatments for BED: IPT, BWL, and CBTgsh. The primary aim was to test whether a specialty therapy (IPT) was more effective than BWL or CBTgsh. Interpersonal psychotherapy was selected as the specialty treatment because it is theoretically and procedurally distinct from both BWL and CBTgsh and because it has a well-documented efficacy in treating BED, depression, and negative affect.24 Our specific moderator hypothesis was that IPT would be the optimal treatment in patients with high negative affect, with no difference between IPT, BWL, or CBTgsh in patients with low negative affect. As a brief and less costly treatment, CBTgsh is well suited as a condition against which to evaluate the effectiveness of both a professionally administered specialty therapy (IPT) and nonspecialty treatment (BWL).
METHODS
There were 2 intervention sites for this study, Rutgers University and Washington University in St Louis, and a separate data and coordinating center at Stanford University, where data were collected and analyzed. The study was approved by each of the 3 sites’ institutional review boards. Two hundred five individuals meeting DSM-IV criteria for BED were entered into the study at the 2 treatment sites (100 at Rutgers and 105 at Washington University).
PARTICIPANTS
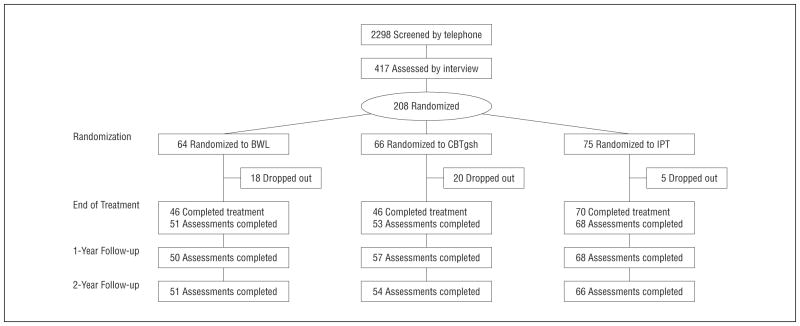
Study participants were identified through advertising and clinic referrals. They were first screened by telephone to ensure that they met preliminary criteria for age, binge eating, and weight (Figure 1). Eligible participants were then invited to an interview and questionnaire assessment, at which time they provided written informed consent to participate. Participants were aged 18 years and older with a body mass index (calculated as weight in kilograms divided by height in meters squared) between 27 and 45 (indicating an overweight/obese sample) and met DSM-IV criteria for BED. Exclusion criteria included current psychosis, bipolar disorder, a current suicidal state, alcohol or drug dependence within the past 6 months, medical disorders that would affect weight and ability to participate, insufficient fluency with English to participate in therapy, current participation in a weight-control program, taking medication that would affect weight, and pregnancy. Participants currently taking antidepressant medication were entered into the study provided that they had been taking a stable dosage for at least 2 months.
Figure 1.
Participant flow across all phases of the study. BWL indicates behavioral weight loss treatment; CBTgsh, guided self-help based on cognitive behavior therapy; and IPT, interpersonal psychotherapy.
Individuals who remained eligible following screening and were willing to participate were entered into the study. Participants were randomly assigned to 1 of the 3 treatment conditions using a computer-generated sequence with stratification across treatments and within site based on high and low negative affect assessed by the Beck Depression Inventory (BDI)25 with a cutoff point of 18. Analysis of a previous data set indicated that this BDI cutoff provides an efficient means of identifying high and low negative affect subtypes revealed by earlier cluster analytic studies (Eric Stice, PhD; oral communication; February 2000).
TREATMENTS
The 3 treatments were conducted during a 24-week interval. Participants were followed up at 6-month intervals for 2 years after the end of treatment.
Interpersonal Psychotherapy
Interpersonal psychotherapy for BED was formulated by Wilfley.7,26 It was based on the treatment developed by Klerman et al27 for depression, and Fairburn28 later adapted it for the treatment of bulimia nervosa. The treatment is manualized. The first phase is composed of 4 sessions and is devoted to a detailed analysis of the interpersonal context within which the eating disorder developed and was maintained. This leads to a formulation of the current interpersonal problem areas, which then form the focus of the second stage of therapy aimed at helping the patient make interpersonal changes in the specific area or areas identified. The last 3 sessions are devoted to a review of the patient’s progress and an exploration of ways to handle future interpersonal difficulties. Although links are made throughout treatment between interpersonal events and binge eating, the therapy does not contain any of the specific behavioral or cognitive procedures that characterize CBT. In the current study, all sessions were individual and 50 to 60 minutes long except for the first, which was 2 hours long. The first 3 sessions were scheduled during the first 2 weeks and were followed by 12 weekly sessions and the final 4 sessions at 2-week intervals, for a total of 19 sessions during 24 weeks. The total therapy time was the same as that for BWL.
The treatment was delivered by doctoral-level (PhD and PsyD) therapists, 3 at Rutgers University and 2 at Washington University. Dr Wilfley conducted training in IPT before the study began. Therapists received weekly supervision at their respective sites by Drs Wilfley and Wilson. In addition, joint supervision meetings twice a year and quarterly conference calls were held for both treatment sites throughout the study.
Behavioral Weight Loss Treatment
The National Institutes of Diabetes and Digestive and Kidney Diseases’s Diabetes Prevention Program’s manual29 was adapted for this study. The program includes both moderate caloric restriction and exercise. The treatment initially focused on dietary change toward a weight loss goal of 7% of one’s starting weight. Participants were first asked to reduce fat intake to 25% of calories from fat. If satisfactory progress in terms of weight loss was not being made, a calorie goal was set based on initial weight. Self-monitoring of exercise, fat intake, and (if necessary) caloric intake is an essential aspect of the program. The exercise goal was 2.5 hours of moderate exercise each week. The core curriculum consists of 16 individual weekly sessions each lasting 50 minutes and followed by 4 sessions at 2-week intervals aimed at continuing weight loss and enhancing maintenance of such losses based on the National Institutes of Diabetes and Digestive and Kidney Diseases manual for contacts after the initial core 16 sessions. The treatment was delivered by master’s-level therapists in clinical psychology or nutrition, 2 at Rutgers University and 3 at Washington University. Bonnie Gillis, MS, RD, conducted the initial training workshop and served as a consultant. The therapists received supervision every other week. As with IPT, quarterly joint supervisory meetings across sites were held throughout the study.
Guided Self-help Based on CBT
This manualized treatment is based on Fairburn’s book Overcoming Binge Eating30 and is performed under the guidance of a therapist. The book provides education about binge eating and a step-by-step self-help program. This intervention is derived from manual-based CBT. The primary focus is developing a regular pattern of moderate eating using self-monitoring, self-control strategies, and problem-solving. Relapse prevention is emphasized to promote maintenance of behavioral change. The principal role of the therapist is to explain the rationale for the use of the self-help manual, generate a reasonable expectancy for a successful outcome, and to motivate the patient to focus on using the manual. There were 10 treatment sessions, each lasting approximately 25 minutes, except for the first session, which was 60 minutes long. The first 4 sessions were weekly, the next 2 occurred at 2-week intervals, and the last 4 occurred at 4-week intervals. The therapists were first- or second-year graduate students with no experience in CBTgsh or treating BED, 4 at Rutgers University and 4 at Washington University. Dr Fairburn conducted initial training in CBTgsh in a 3-hour workshop. The therapists did not receive regularly scheduled supervision. As with the other 2 treatments, quarterly meetings across sites were held throughout the study.
All therapists were required to complete treatment of 2 pilot patients and be approved before participating in the study proper. Treatment fidelity was assessed at the data and coordinating center by auditing a 15% random sample of participants in each condition with 3 sessions from each participant sampled. The tapes were audited by one of us (W.S.A.) and were rated for adherence to the therapy protocol and quality of therapist-patient interaction on a 7-point scale. Mean ratings were as follows: IPT, 6.3 (SD, 0.7); BWL, 6.1 (SD, 0.8); and CBTgsh, 6.2 (SD, 0.7). (The scale is available on request.)
ASSESSMENTS
Assessments were conducted pretreatment, at the end of treatment, and at 6-, 12-, 18-, and 24-month follow-ups. Participants were assessed for general psychopathology with the Structured Clinical Interview for DSM-IV (SCID-I) and personality disorders with SCID-II only at the pretreatment assessment during the collection of demographic information. They were assessed for eating disorder psychopathology with the EDE,31 revised to cover a 6-month period, which documents episodes and days of binge eating as well as subscale scores for dietary restraint and concerns about eating, weight, and shape that can be summed as a global scale. Assessors were blinded to treatment condition. Reliability of EDE ratings of binge eating was determined by having a randomly selected sample of 15% of the EDEs that were conducted at each treatment site rated by assessors at the other site. Interrater reliability coefficients were 0.97 for both episodes and days of binge eating.
Questionnaires administered included the BDI, the Rosenberg Self-Esteem Scale,32 and the Social Adjustment Self-report Scale.33 Patients rated suitability of the treatment and their expectancy that it would prove effective on visual analog scales (1, lowest; 10, highest) at the end of the first and fourth therapy sessions.
STATISTICAL ANALYSIS
Sample size calculations were made using data from the Wilfley et al7 study comparing group IPT and CBT for binge eating disorder. Assuming the use of a 2 (sites) × 2 (negative affect subtypes) × 3 (treatment groups) design with a repeated-measures analysis of variance, a power of 80%, and a 5% 2-tailed test, a medium effect size of 0.5 for binge eating can be detected with a sample size of 205 (assuming a 15% attrition rate). The primary outcome variable was days of binge eating assessed during a 28-day period and weight. Analyses were by intent-to-treat and conducted separately for the treatment and follow-up periods. For the treatment period, the primary analysis for continuous measures was an analysis of variance using the slope of change in the primary variables as the outcome measures and center, treatment, negative affect subtype, and all interactions as the independent measures. When appropriate, Scheffe post hoc tests were used to determine pairwise differences between treatments. Effect sizes were calculated using Cohen d34 and applying his guidelines of 0.2, 0.5, and 0.8 as cutoffs for small, medium, and large effect sizes, respectively. For categorical outcomes, a logistic regression was used with the same independent variables and the odds ratio (OR) was used as an effect size.35 To evaluate maintenance of treatment effects, we focused on 1- and 2-year follow-ups. Change from posttreatment was used to examine maintenance. Analyses used an analysis of covariance (continuous measure) or logistic regression (categorical measure) with the posttreatment measure as a covariate. The independent measures remained the same as for the treatment period. When data were missing at posttreatment, the baseline value was carried forward. During follow-up, if 2-year data were missing, 18-month scores were used; if 1-year data were missing, 6-month scores were used. If no measures were available for a particular time, then the baseline value was used.
Exploratory analyses of nonspecific predictors and moderators included using all baseline measures as potential predictors and moderators of remission from binge eating. As defined by Kraemer et al,21 the linear model to examine moderators had the potential moderator, treatment, and treatment × moderator interaction as independent variables. Logistic regression was used, and center, negative affect status, and all interactions were also included in the model. Moderation occurred when a significant moderator × treatment interaction was found, indicating that the treatment worked differently for various levels of the moderator.
RESULTS
Figure 1 summarizes the flow of participants through the study. Baseline measures and race/ethnicity as reported by the participants, by treatment condition, are summarized in Table 1. Patients reported both BWL and IPT to be more suitable than CBTgsh at session 1 (mean [SD] suitability score: BWL, 8.6 [1.7]; CBTgsh, 7.8 [2.1]; IPT, 8.9 [1.6]; F2,186 = 7.6; P < .001) and IPT to be more suitable than CBTgsh at session 4 (BWL, 8.3 [1.8]; CBTgsh, 7.6 [2.1]; IPT, 8.7 [1.7]; F2,197 = 5.2; P < .01). Patients expected IPT to be significantly more effective than CBTgsh both at the end of session 1 (IPT, 8.4 [1.6]; CBTgsh, 7.5 [2.1]; F2,185 = 5.0; P < .01) and session 4 (IPT, 8.4 [1.7]; CBTgsh, 7.5 [2.2]; F2,187 = 4.3; P < .05).
Table 1.
Baseline Measures Across Centers and Treatments
| Characteristic | Mean (SD) by Center and Treatment
|
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Rutgers University
|
Washington University–St Louis IPT
|
Total
|
|||||||
| BWL (n=32) | CBTgsh (n=31) | IPT (n=37) | BWL (n=32) | CBTgsh(n=35) | IPT (n=38) | BWL (n=64) | CBTgsh (n=66) | IPT (n=75) | |
| Age, y | 43.9 (11.2) | 50.0 (14.8) | 47.9 (12.0) | 48.5 (10.3) | 50.7 (12.6) | 49.5 (10.3) | 46.2 (10.9) | 50.3 (13.6) | 48.7 (11.2) |
| Age range, y | 19–64 | 19–77 | 23–66 | 26–69 | 26–76 | 30–68 | 19–69 | 19–77 | 23–68 |
| BMI | 35.5 (5.9) | 36.6 (4.6) | 35.4 (5.2) | 38.1 (4.9) | 35.8 (4.1) | 37.2 (5.0) | 36.8 (5.5) | 36.2 (4.3) | 36.3 (5.1) |
| Binge days, median (IQR) | 20 (13–30) | 20 (12–31) | 15 (10–25) | 16 (13–22) | 16 (10–22) | 18 (12–23) | 20 (13–27) | 18 (11–27) | 16 (11–24) |
| Global EDE score | 3.0 (0.8) | 2.9 (0.9) | 2.8 (0.7) | 2.7 (0.8) | 2.6 (0.7) | 2.8 (0.8) | 2.8 (0.8) | 2.7 (0.8) | 2.8 (0.7) |
| BDI score >18, % | 47 | 42 | 46 | 41 | 46 | 42 | 44 | 44 | 44 |
| Rosenberg Self-Esteem Scale score | 24.3 (6.5) | 22.1 (5.9) | 23.9 (5.4) | 22.4 (5.7) | 23.4 (5.6) | 23.5 (5.5) | 23.4 (6.2) | 22.8 (5.3) | 23.7 (5.4) |
| Quality of life score | 0.64 (0.12) | 0.66 (0.09) | 0.64 (0.13) | 0.68 (0.15) | 0.68 (0.12) | 0.67 (0.12) | 0.66 (0.13) | 0.67 (0.11) | 0.66 (0.12) |
| Personality disorder, % | 31 | 12 | 24 | 22 | 26 | 21 | 27 | 20 | 23 |
| Current depression, % | 6 | 6 | 19 | 19 | 23 | 13 | 13 | 15 | 16 |
| History of depression, % | 37 | 27 | 42 | 56 | 46 | 53 | 47 | 37 | 47 |
| Substance abuse, % | 19 | 10 | 8 | 3 | 11 | 3 | 11 | 11 | 5 |
| Ethnicity, % | |||||||||
| American Indian | 0 | 0 | 3 | 0 | 0 | 0 | 0 | 0 | 1 |
| Black | 9 | 6 | 5 | 12 | 14 | 29 | 11 | 11 | 17 |
| White | 91 | 77 | 84 | 84 | 86 | 71 | 88 | 82 | 77 |
| Hispanic | 0 | 16 | 8 | 3 | 0 | 0 | 2 | 8 | 4 |
| College degree, % | 31 | 39 | 24 | 37 | 34 | 37 | 34 | 38 | 30 |
| Male sex, % | 13 | 19 | 16 | 9 | 17 | 13 | 11 | 18 | 15 |
Abbreviations: BDI, Beck Depression Inventory; BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); BWL, behavioral weight loss treatment; CBTgsh, guided self-help based on cognitive behavior therapy; EDE, Eating Disorder Examination; IPT, interpersonal psychotherapy; IQR, interquartile range.
Patients were considered dropouts if they missed 3 consecutive sessions for nonemergency reasons or wished to terminate treatment at any point. Of the latter, some were willing to participate in subsequent assessments, whereas others were not. At posttreatment, dropout rates were 7%, 28%, and 30% for the IPT, BWL, and CBTgsh groups, respectively. Interpersonal psychotherapy had a significantly lower attrition rate than either BWL or CBTgsh (F1,193 = 8.3; P < .001). Racial and ethnic minorities had a higher dropout rate (33% vs 14%; F1,182 = 8.8; P < .005) and dropouts reported higher scores on the EDE subscales at baseline (mean [SD], 3.0 [0.9]) compared with nondropouts (2.7 [0.8]; F1,182 = 4.0; P < .05). There was a significant treatment × negative affect interaction (F1,193 = 5.7; P < .005). Patients with high negative affect dropped out of BWL (46%) more often than patients in CBTgsh did (24%), whereas the pattern was reversed among the patients with low negative affect (BWL, 14%; CBTgsh, 35%). Interpersonal psychotherapy was unaffected by negative affect. The ORs for the treatment × negative affect interactions were 2.6 for BWL, 0.59 for CBTgsh, and 0.84 for IPT, for which a ratio greater than 1 favors low negative affect.
Posttreatment assessment rates were 91%, 80%, and 80% for IPT, BWL, and CBTgsh, respectively. The comparable 2-year assessment rates were 88%, 82%, and 80%. There were no site differences for dropout rate or assessment completion at posttreatment. At 2-year follow-up, however, the Washington University site had a significantly higher overall assessment completion rate than Rutgers University (F1,193 = 5.9; P < .05). There were no significant site differences on baseline patient characteristics.
TREATMENT OUTCOME
Posttreatment
Intent-to-treat analyses revealed no differences among the 3 treatments on remission from binge eating (Figure 2), reduction in days of binge eating, or no longer meeting DSM-IV criteria for BED (mean: IPT, 87%; BWL, 81%; and CBTgsh, 82%). Similarly, no differences were found on the EDE subscales of eating, weight, or shape concerns nor for BDI or the self-esteem scale. The hypothesized moderator effect of negative affect did not reach statistical significance (Table 2). Behavioral weight loss treatment was significantly more effective in reducing body mass index than IPT and CBTgsh (F2,193 = 6.6; P < .005; BWL vs CBTgsh, d = 0.741; BWL vs IPT, d = 0.48; IPT vs CBTgsh, d = 0.15) and more effective than CBTgsh in increasing dietary restraint (F2,193 = 5.3; P < .01). Behavioral weight loss treatment similarly produced a greater number of patients with a 5% reduction in body weight (41%) than IPT (15%) or CBTgsh (15%) (F2,193 = 8.3; P < .001; ORs for BWL vs CBTgsh, 3.9; for BWL vs IPT, 3.9). Table 3 summarizes the weight and global EDE outcomes at each assessment for all treatments. Remission from binge eating was associated with a significantly greater percent change in weight. Remitted patients had a mean percent change in weight of −2.4% (SD, 6.1%) compared with −0.61% (SD, 4.2%) for nonremitted patients (F1,181 = 5.8; P < .05).
Figure 2.
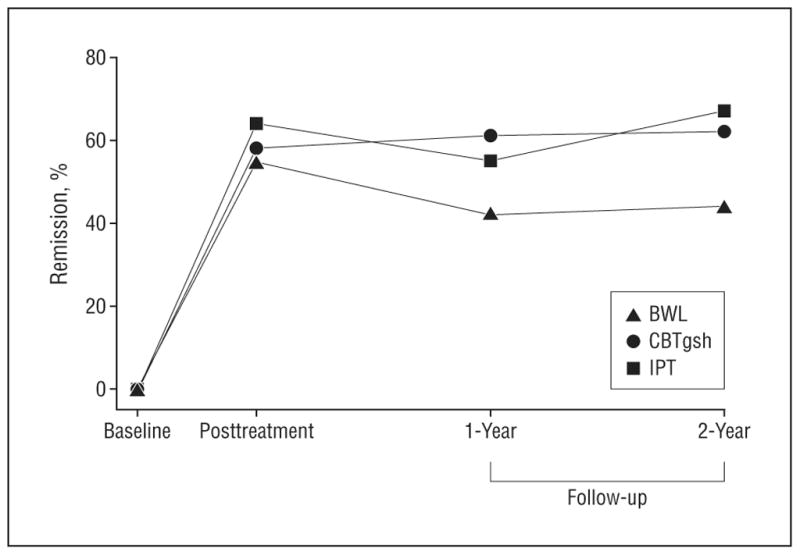
Remission rates at posttreatment and 1- and 2-year follow-up. BWL indicates behavioral weight loss treatment; CBTgsh, guided self-help based on cognitive behavior therapy; and IPT, interpersonal psychotherapy.
Table 2.
Remission Rates and ORs of Treatment × Negative Affect at Posttreatment and Follow-up
| Characteristic | Posttreatment | Follow-up
|
|
|---|---|---|---|
| 1-Year | 2-Year | ||
| Remission Rate, % | |||
| Low negative affect | |||
| 64 | 50 | 47 | |
| CBTgsh | 62 | 59 | 62 |
| IPT | 67 | 55 | 64 |
| High negative affect | |||
| BWL | 43 | 32 | 39 |
| CBTgsh | 52 | 62 | 62 |
| IPT | 61 | 55 | 70 |
| OR, Low Negative Affect vs High Negative Affecta | |||
| BWL | 2.4 | 2.1 | 1.4 |
| CBTgsh | 1.5 | 0.9 | 1.0 |
| IPT | 1.3 | 1.0 | 0.8 |
Abbreviations: BWL, behavioral weight loss treatment; CBTgsh, guided self-help based on cognitive behavior therapy; IPT, interpersonal psychotherapy; OR, odds ratio.
An OR greater than 1 indicates better results in the low negative affect category. An OR less than 1 indicates better results in the high negative affect category.
Table 3.
Weight and Global EDE Outcomes at Posttreatment and Follow-up
| Characteristic | Mean (SD)
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BWL
|
CBTgsh
|
IPT
|
||||||||||
| Baseline | Post-treatment | Follow-up
|
Baseline | Post-treatment | Follow-up
|
Baseline | Post-treatment | Follow-up
|
||||
| 1-Year | 2-Year | 1-Year | 2-Year | 1-Year | 2-Year | |||||||
| No. of binge days | 16.3 (5.9) | 4.3 (7.9) | 6.5 (8.7) | 5.8 (8.5) | 16.6 (7.3) | 3.8 (7.2) | 4.3 (7.8) | 3.7 (7.3) | 16.1 6.6 |
3.7 (7.2) | 4.8 (7.6) | 4.3 (7.8) |
| BMI | 36.8 (5.5) | 35.4 (5.7) | 36.0 (6.2) | 36.3 (6.2) | 36.2 (4.3) | 36.1 (4.4) | 35.7 (4.9) | 35.7 (5.0) | 36.3 (5.1) | 35.9 (5.3) | 35.9 (5.4) | 36.1 (5.5) |
| Weight, kg | 103.5 (22.6) | 99.8 (23.2) | 101.7 (25.2) | 102.1 (24.6) | 100.3 (14.0) | 100.0 (14.1) | 98.8 (15.1) | 99.3 (15.6) | 100.4 (18.6) | 99.1 (18.3) | 99.3 (19.0) | 99.5 (18.7) |
| 5% Reduction in weight, % | 0 | 41 | 27 | 27 | 0 | 15 | 26 | 23 | 0 | 15 | 21 | 21 |
| Global EDE score | 2.8 (0.8) | 2.1 (1.0) | 2.2 (1.0) | 2.0 (1.2) | 2.7 (0.8) | 1.7 (1.0) | 1.7 (0.9) | 1.7 (1.0) | 2.8 (0.7) | 1.8 (0.9) | 1.9 (1.0) | 1.7 (1.1) |
Abbreviations: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared); BWL, behavioral weight loss treatment; EDE, Eating Disorder Examination; CBTgsh, guided self-help based on cognitive behavior therapy; IPT, interpersonal psychotherapy.
A main effect of negative affect was found on both change in days of binge eating (F1,193 = 5.4; P < .05; d = 0.33) and not meeting DSM-IV criteria for BED (F1, 192 = 7.7; P < .01; OR, 2.8). In both instances, high negative affect resulted in less improvement. There were no significant treatment × negative affect interactions.
Follow-up
At 1 year, no significant differences among treatments on any measure of binge eating were found. Those in the BWL group showed significantly more body mass index gain than those in the CBTgsh group (F2,192 = 3.1; P < .05; BWL vs CBTgsh, d = 0.52; BWL vs IPT, d = 0 0.29; and IPT vs CBTgsh, d = 0 0.20). There was no relationship between sustained remission from binge eating and percent change in weight at 1 year. Baseline high negative affect resulted in less reduction in body mass index (F1,192 = 4.3; P < .05; weight [in kilograms], F1.192 = 4.1; P < .05) and the BDI score (F1,192 = 4.5; P < .05) than low negative affect. At 2-year follow-up, both IPT and CBTgsh were significantly more effective than BWL in terms of remission from binge eating (F2,192 = 3.6; P < .05; ORs: BWL vs CBTgsh, 2.3; BWL vs IPT, 2.6; and CBTgsh vs IPT, 1.2) (Figure 2). No significant moderator effect of negative affect subtype on remission from binge eating was found (Table 2). Behavioral weight loss was no longer significantly different from the other treatments in terms of weight loss. There were no site differences on measures of binge eating or weight. There was no significant association between sustained remission from binge eating and percent change in weight. A significantly greater proportion (31%) of patients with sustained remission from binge eating during follow-up lost a minimum of 5% of their baseline weight compared with patients who were never in remission (10%) (F1,171 = 5.3; P < .01; OR, 4.0).
NONSPECIFIC PREDICTORS AND MODERATORS
Posttreatment
Several significant exploratory baseline, nonspecific predictors of outcome (defined as remission from binge eating) were found: education, Wald1 = 7.4, P < .01; global EDE score, Wald1 = 6.2, P < .01; BDI score, Wald1 = 8.4, P < .005; and self-esteem score, Wald1 = 8.5, P < .005. Exploratory analyses showed that frequency of days of binge eating emerged as a moderator (Wald1 = 7.1, P < .01). For example, analysis using a median split of baseline frequency showed that patients who binged more than 14 days during the past 28 days responded worse to BWL (46% remission rate) and CBTgsh (50% remission rate) than to IPT (66% remission rate).
Follow-up
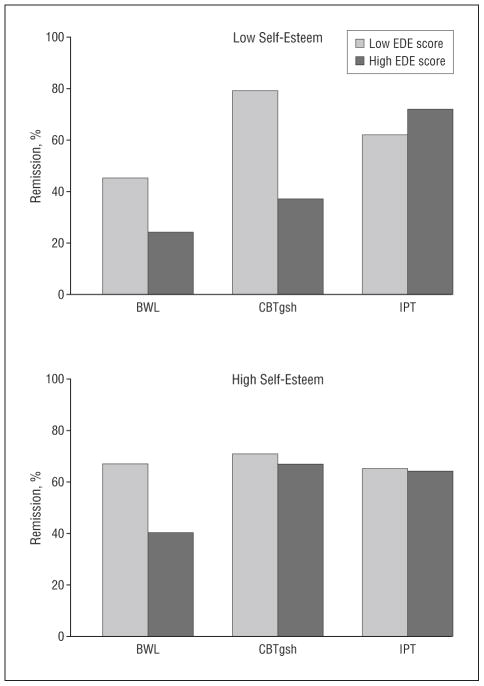
Lifetime history of depression predicted less remission from binge eating (38%) than absence of the disorder (62%) (Wald1 = 4.5, P < .05). In exploratory analyses, 2 moderators were identified at the 2-year follow-up (global EDE score, Wald1 = 4.0, P < .05, and self-esteem, Wald1 = 3.8, P < .05). For global EDE score, the ORs between low and high levels of the EDE (median split of 2.675) were as follows: BWL, 2.8; CBTgsh, 2.9; and IPT, 0.7. For self-esteem, the ORs between low and high levels (median split of 23) were BWL, 2.4; CBTgsh, 1.9; and IPT, 0.9. Whereas IPT is comparably effective across both low and high self-esteem in interaction with global EDE score, the pattern differs for BWL and CBTgsh. Patients with low self-esteem who underwent BWL fared much worse than those with high self-esteem in the context of both high and low global EDE score (Figure 3). Patients with both low self-esteem and high EDE score did worse. In CBTgsh, there is little difference between high and low self-esteem provided that global EDE score is low (71% and 79%, respectively). For those with high global EDE scores, however, patients with low self-esteem (37%) did significantly worse than those with high self-esteem (67%).
Figure 3.
Remission rates at 2-year follow-up for participants with high and low self-esteem by high and low global Eating Disorder Examination (EDE) scores. BWL indicates behavioral weight loss treatment; CBTgsh, guided self-help based on cognitive behavior therapy; and IPT, interpersonal psychotherapy.
COMMENT
Prior studies comparing BWL with a specialty treatment for BED have been limited by small sample sizes, inadequate measurement of BED, and the absence of longer-term follow-up. The current study has the largest sample size and longest follow-up of any controlled outcome study of carefully assessed BED to date. Consistent with some previous studies,11,13 ours found no difference among the 3 interventions at posttreatment on binge eating; specific eating disorder psychopathology of body weight, shape, and eating concern; or general psychopathology. At the 2-year follow-up, however, both IPT and CBTgsh were significantly more effective than BWL in eliminating binge eating. This superiority of a specialty therapy over BWL for BED is supported by 2 recent short-term studies. Munsch et al36 found that CBT was significantly superior to BWL, and Grilo and Masheb17 showed that a self-help version of CBT was significantly more effective than self-help BWL. Devlin et al,37–38 in a randomized double-blind placebo-controlled study, found that the addition of CBT—but not antidepressant medication—to BWL treatment significantly enhanced outcomes at posttreatment and 24-month follow-up. Interpersonal psychotherapy was also more successful in retaining patients in the trial than BWL or CBTgsh. Our dropout rate for BWL was consistent with previous research.36,39 The CBTgsh attrition in our study was greater than in others (eg, Grilo and Masheb17) possibly because it was contrasted with longer, more “face valid” treatments. This might also explain the difference in suitability ratings.
Additional evidence of the specificity of treatment effects with BED derive from our moderator analyses. A high frequency of binge eating at baseline negatively impacted remission rates at posttreatment in BWL and CBTgsh, but had no effect on the efficacy of IPT. At the 2-year follow-up, low self-esteem undermined the effects of BWL in eliminating binge eating, but had no influence on IPT. Guided self-help based on CBT was unaffected by low self-esteem in patients with low global EDE scores, but was substantially less effective in interaction with high EDE scores. Although self-esteem emerged as a moderator, we did not find, as hypothesized, that negative affect defined by the BDI moderated outcome. Prior studies showing that negative affect predicted treatment outcome defined the construct in terms of both BDI and Rosenberg Self-Esteem Scale scores derived from cluster analyses.22–23 In the current study, the pattern of BDI and EDE score interactions was similar to that of self-esteem and global EDE; the BDI and self-esteem measure were highly correlated (r = 0.73).
The novel finding that global EDE score moderated treatment outcome is consistent with a latent class analysis of the patients with BED described here, in which Sysko et al40 found 4 different latent classes within the sample. The one characterized by the most specific eating disorder psychopathology (ie, most severe objective and subjective bulimic episodes and highest body shape and weight concerns), which would be reflected in high global EDE scores, responded the most to IPT.
Overall CBTgsh did not differ in outcome from the intensive specialty treatment (IPT), though its attrition rate was higher. Moreover, overall CBTgsh fared as well as IPT despite patients’ significantly lower initial suitability ratings and expectations about its effectiveness as a treatment for BED. Guided self-help based on CBT was significantly superior to BWL at follow-up and comparable in terms of weight loss. Given its brevity and advantages in disseminability to a wider range of health providers than a specialty therapy, CBTgsh is a cost-effective treatment of BED.8 Although the CBTgsh therapists in this study were inexperienced beginning graduate students in clinical psychology, they were highly selected and working in a specialty eating disorder clinic setting. Other research has shown that nonspecialists can effectively deliver CBTgsh for binge eating, though specific competencies of therapists in particular service settings remain unclear.19,41 Our findings suggest that comorbid general psychopathology in BED does not contraindicate CBTgsh. Unlike BWL, it was unaffected by low self-esteem unless this was combined with a high level of specific eating disorder psychopathology.
Behavioral weight loss treatment produced significantly increased dietary restraint and reduction in body weight at posttreatment. The latter (3.8%) was substantially less than our target of a mean reduction of 7%; however, Devlin et al,37 Grilo et al,39 and Munsch et al36 all reported minimal weight loss with BWL in obese patients with BED. This finding is consistent with other evidence that obese individuals with BED lose less weight than comparably obese patients without BED undergoing BWL.42–43 Earlier studies of binge eating in obese patients produced mixed results. Whereas some showed no effect of binge eating status on BWL treatment,44–45 others indicated either a negative6,46 or even positive effect12 on weight loss. Collectively, these studies pose problems of interpretation owing to small sample sizes, self-report measures of binge eating, and a focus on binge eating rather than on the formal BED diagnosis. Despite high rates of improvement in patients with BED in terms of binge eating, specific eating disorder characteristics, and more general psychopathology, effective methods for producing longer-term weight loss remain elusive.8
Consistent with previous research,4 patients who had ceased binge eating lost more mean percent weight than those who continued to binge at posttreatment. At follow-up, the difference disappeared. Patients with sustained remission from binge eating did not show greater mean percent weight loss than those never in remission during the 2 years of follow-up. However, remission from binge eating was significantly associated with a higher number of patients losing at least 5% of their weight at the 2-year follow-up.
The study had limitations. Only 18% of the sample were minority group members and they showed a significantly higher attrition rate. Only 21% were men. Treatment at both sites was delivered within the context of specialty eating disorder clinics. Accordingly, the generalizability of our results to other populations and treatment in nonspecialist settings is limited. Strengths of the study include its large sample size, rigorous assessment of BED, and absence of any treatment differences across sites despite the different degrees of experience with the treatments at the Rutgers University and Washington University clinics.
Our findings show that all 3 treatments had similar outcomes on binge eating at posttreatment, with IPT showing the lowest attrition. At the 2-year follow-up, both those undergoing IPT and CBTgsh not only successfully maintained their improvement but had significantly superior improvement compared with those in the BWL group, who had substantial relapse, with no differences in body mass index across treatments. The findings suggest that CBTgsh be considered a first-line treatment for most patients with BED. Interpersonal psychotherapy (or perhaps another specialty therapy such as CBT) should be recommended as the treatment of choice for that subset of individuals with BED (30% of the sample in this study) with low self-esteem and a high level of specific eating disorder psychopathology.
Acknowledgments
Funding/Support: This study was funded by grants R01063863 (Dr Agras), R01064153 (Dr Wilfley), K24070446 (Dr Wilfley), and R01063862 (Dr Wilson) from the National Institutes of Health.
Footnotes
Financial Disclosure: None reported.
Previous Presentation: Portions of this paper were presented at the Eating Disorders Research Society Annual Meeting; Montreal, Quebec, Canada; September 26, 2008.
Additional Contributions: Christopher G. Fairburn, MD, Oxford University, and Bonnie Gillis, MS, RD, University of Pittsburgh, helped train therapists in CBTgsh and BWL, and R. Robinson Welch, PhD, Washington University–St Louis, assisted in conducting the study.
References
- 1.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 2.Striegel-Moore RH, Franko D. Should binge eating disorder be included in the DSM-V? a critical review of the state of the evidence. Annu Rev Clin Psychol. 2008:4305–324. doi: 10.1146/annurev.clinpsy.4.022007.141149. [DOI] [PubMed] [Google Scholar]
- 3.Wilfley DE, Bishop M, Wilson GT, Agras WS. Classification of eating disorders: toward DSM-V. Int J Eat Disord. 2007;40(suppl):S123–S129. doi: 10.1002/eat.20436. [DOI] [PubMed] [Google Scholar]
- 4.Wilfley DE, Schwartz M, Spurrell E, Fairburn C. Using the eating disorder examination to identify the specific psychopathology of binge eating disorder. Int J Eat Disord. 2000;27 (3):259–269. doi: 10.1002/(sici)1098-108x(200004)27:3<259::aid-eat2>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 5.Hudson JI, Hiripi E, Pope HJ, Kessler R., Jr The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol Psychiatry. 2007;61 (3):348–358. doi: 10.1016/j.biopsych.2006.03.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yanovski SZ. Binge eating disorder and obesity in 2003: could treating an eating disorder have a positive effect on the obesity epidemic? Int J Eat Disord. 2003;34(suppl):S117–S120. doi: 10.1002/eat.10211. [DOI] [PubMed] [Google Scholar]
- 7.Wilfley DE, Welch RR, Stein RI, Spurrell EB, Cohen LR, Saelens BE, Dounchis JZ, Frank MA, Wiseman CV. Matt GE A randomized comparison of group cognitive-behavioral therapy and group interpersonal psychotherapy for the treatment of overweight individuals with binge eating disorder. Arch Gen Psychiatry. 2002;59 (8):713–721. doi: 10.1001/archpsyc.59.8.713. [DOI] [PubMed] [Google Scholar]
- 8.Wilson GT, Grilo C, Vitousek K. Psychological treatment of eating disorders. Am Psychol. 2007;62 (3):199–216. doi: 10.1037/0003-066X.62.3.199. [DOI] [PubMed] [Google Scholar]
- 9.Wadden TA, Butryn ML, Byrne KJ. Efficacy of lifestyle modification for long-term weight control. Obes Res. 2004;12(suppl):151S–162S. doi: 10.1038/oby.2004.282. [DOI] [PubMed] [Google Scholar]
- 10.Agras WS, Telch CF, Arnow B, Eldredge K, Wilfley DE, Raeburn SD, Henderson J, Marnell M. Weight loss, cognitive-behavioral, and desipramine treatments in binge eating disorder: an additive design. Behav Ther. 1994;25 (2):225–238. [Google Scholar]
- 11.Marcus MD, Wing RR, Fairburn CG. Cognitive behavioral treatment of binge eating vs. behavioral weight control on the treatment of binge eating disorder. Ann Behav Med. 1995;17(suppl):S090. [Google Scholar]
- 12.Gladis MM, Wadden TA, Vogt R, Foster G, Kuehnel RH, Bartlett SJ. Behavioral treatment of obese binge eaters: do they need different care? J Psychosom Res. 1998;44 (3–4):375–384. doi: 10.1016/s0022-3999(97)00262-6. [DOI] [PubMed] [Google Scholar]
- 13.Stunkard AJ, Allison KC. Binge eating disorder: disorder or marker? Int J Eat Disord. 2003;34(suppl):S107–S116. doi: 10.1002/eat.10210. [DOI] [PubMed] [Google Scholar]
- 14.Wilfley DE, Wilson GT, Agras WS. The clinical significance of binge eating disorder. Int J Eat Disord. 2003;34(suppl):S96–S106. doi: 10.1002/eat.10209. [DOI] [PubMed] [Google Scholar]
- 15.Carter JC, Fairburn CG. Cognitive-behavioral self-help for binge eating disorder: a controlled effectiveness study. J Consult Clin Psychol. 1998;66 (4):616–623. doi: 10.1037//0022-006x.66.4.616. [DOI] [PubMed] [Google Scholar]
- 16.Loeb KL, Wilson GT, Gilbert JS, Labouvie E. Guided and unguided self-help for binge eating. Behav Res Ther. 2000;38 (3):259–272. doi: 10.1016/s0005-7967(99)00041-8. [DOI] [PubMed] [Google Scholar]
- 17.Grilo CM, Masheb RM. A randomized controlled comparison of guided self-help cognitive behavioral therapy and behavioral weight loss for binge-eating disorder. Behav Res Ther. 2005;43(11):1509–1525. doi: 10.1016/j.brat.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 18.Grilo CM, Masheb RM, Salant SL. Cognitive behavioral therapy guided self-help and orlistat for the treatment of binge eating disorder: a randomized, double-blind, placebo-controlled trial. Biol Psychiatry. 2005;57 (10):1193–1201. doi: 10.1016/j.biopsych.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 19.Grilo CM. Guided self-help for binge-eating disorder. In: Latner JD, Wilson GT, editors. Self-Help Approaches for Obesity and Eating Disorders. New York, NY: Guilford Press; 2007. pp. 73–91. [Google Scholar]
- 20.Wilson GT, Vitousek K, Loeb KL. Stepped-care treatment for eating disorders. J Consult Clin Psychol. 2000;68 (4):564–572. [PubMed] [Google Scholar]
- 21.Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Arch Gen Psychiatry. 2002;59 (10):877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 22.Stice E, Agras WS, Telch C, Halmi K, Mitchell J, Wilson GT. Subtyping binge eating-disordered women along dieting and negative affect dimensions. Int J Eat Disord. 2001;30 (1):11–27. doi: 10.1002/eat.1050. [DOI] [PubMed] [Google Scholar]
- 23.Grilo CM, Masheb RM, Wilson GT. Subtyping binge eating disorder. J Consult Clin Psychol. 2001;69 (6):1066–1072. doi: 10.1037//0022-006x.69.6.1066. [DOI] [PubMed] [Google Scholar]
- 24.Klerman GL, Weissman MM, editors. New Applications of Interpersonal Psychotherapy. New York, NY: American Psychiatric Press; 1993. [Google Scholar]
- 25.Beck AT, Steer RM, Garbin M. Psychometric properties of the Beck Depression Inventory: 25 years of evaluation. Clin Psychol Rev. 1988;8 (1):77–100. [Google Scholar]
- 26.Wilfley DE, Frank E, Welch R, Spurrell EB, Rounsaville B. Adapting Interpersonal Psychotherapy to a group format (IPT-G) for binge eating disorder: toward a model for adapting empirically-supported treatments. Psychother Res. 1998;8 (4):379–391. [Google Scholar]
- 27.Klerman GL, Weissman MM, Rounsaville B, Chevron E. Interpersonal Psychotherapy of Depression. New York, NY: Basic Books; 1984. [Google Scholar]
- 28.Fairburn CG. Interpersonal psychotherapy for bulimia nervosa. In: Garner DM, Garfinkel PE, editors. Handbook of Treatment for Eating Disorders. New York, NY: Guilford Press; 1997. pp. 278–294. [Google Scholar]
- 29.Diabetes Prevention Program (DPP) Research Group. The diabetes prevention program (DPP): description of lifestyle intervention. Diabetes Care. 2002;25 (12):2165–2171. doi: 10.2337/diacare.25.12.2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fairburn CG. Overcoming Binge Eating. New York, NY: Guilford Press; 1995. [Google Scholar]
- 31.Fairburn CG, Cooper Z. The eating disorder examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment, and Treatment. New York, NY: Guilford Press; 1993. pp. 361–404. [Google Scholar]
- 32.Rosenberg M. Conceiving of the Self. New York, NY: Basic Books; 1979. [Google Scholar]
- 33.Weissman MM, Bothwell S. Assessment of social adjustment by patient self-report. Arch Gen Psychiatry. 1976;33 (9):1111–1115. doi: 10.1001/archpsyc.1976.01770090101010. [DOI] [PubMed] [Google Scholar]
- 34.Cohen J. Statistical Power Analysis or the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum Associates; 1988. [Google Scholar]
- 35.Grissum HR, Kim JJ. Effect Sizes for Research. Mahwah, NJ: Lawrence Erlbaum Associates; 2005. [Google Scholar]
- 36.Munsch S, Biedert E, Meyer A, Michael T, Schlup B, Tuch A, Margraf J. A randomized comparison of cognitive behavioral therapy and behavioral weight loss treatment for overweight individuals with binge eating disorder. Int J Eat Disord. 2007;40(2):102–113. doi: 10.1002/eat.20350. [DOI] [PubMed] [Google Scholar]
- 37.Devlin MJ, Goldfein JA, Petkova E, Jiang H, Raizman PS, Wolk S, Mayer L, Carino J, Bellace D, Kamenetz C, Dobrow I, Walsh BT. Cognitive behavioral therapy and fluoxetine as adjuncts to group behavioral therapy for binge eating disorder. Obes Res. 2005;13(6):1077–1088. doi: 10.1038/oby.2005.126. [DOI] [PubMed] [Google Scholar]
- 38.Devlin MJ, Goldfein JA, Petkova E, Liu L, Walsh BT. Cognitive behavioral therapy and fluoxetine for binge eating disorder: two-year follow-up. Obes Res. 2007;15 (7):1702–1709. doi: 10.1038/oby.2007.203. [DOI] [PubMed] [Google Scholar]
- 39.Grilo CM, Masheb RM, Brownell KD, Wilson GT, White MA. Randomized comparison of cognitive behavioral weight loss treatments for obese patients with binge eating disorder: 12-month outcomes. Paper presented at: World Congress of Behavioral and Cognitive Therapy; July 11, 2007; Barcelona, Spain. [Google Scholar]
- 40.Sysko R, Hildebrandt T, Wilson GT, Wilfley DE, Agras WS. An examination of the diagnostic classification and short-term course of binge eating disorder using latent class analysis. Paper presented at the International Conference on Eating Disorders; Seattle, WA. May 16, 2008. [Google Scholar]
- 41.Sysko R, Walsh BT. A critical evaluation of the efficacy of self-help interventions for the treatment of bulimia nervosa and binge-eating disorder. Int J Eat Disord. 2008;41(2):97–112. doi: 10.1002/eat.20475. [DOI] [PubMed] [Google Scholar]
- 42.Blaine B, Rodman J. Responses to weight loss treatment among obese individuals with and without BED: a matched-study meta-analysis. Eat Weight Disord. 2007;12 (2):54–60. doi: 10.1007/BF03327579. [DOI] [PubMed] [Google Scholar]
- 43.Pagoto S, Bodenlos JS, Kantor L, Gitkind M, Curtin C, Ma Y. Association of major depression and binge eating disorder with weight loss in a clinical setting. Obesity (Silver Spring) 2007;15 (11):2557–2559. doi: 10.1038/oby.2007.307. [DOI] [PubMed] [Google Scholar]
- 44.Delinsky SS, Latner JD, Wilson GT. Binge eating and weight loss in a self-help behavior modification program. Obes Res. 2006;14 (7):1244–1249. doi: 10.1038/oby.2006.141. [DOI] [PubMed] [Google Scholar]
- 45.Sherwood NE, Jeffrey RW, Wing RR. Binge status as a predictor of weight loss treatment outcome. Int J Obes. 1999;23 (5):485–493. doi: 10.1038/sj.ijo.0800846. [DOI] [PubMed] [Google Scholar]
- 46.Marcus MD, Wing RR, Hopkins J. Obese binge eaters: affect, cognitions and response to behavioral weight control. J Consult Clin Psychol. 1988;56 (3):433–439. doi: 10.1037//0022-006x.56.3.433. [DOI] [PubMed] [Google Scholar]