Abstract
Study design
A subanalysis study.
Objective
To compare surgical outcomes and complications of multi level decompression and single level fusion to multi level decompression and multi level fusion for patients with multilevel lumbar stenosis and single level degenerative spondylolisthesis.
Summary of Background Data
In patients with degenerative spondylolisthesis who are treated surgically, decompression and fusion provides a better clinical outcome than decompression alone. Surgical treatment for multilevel lumbar stenosis and degenerative spondylolisthesis typically includes decompression and fusion of the spondylolisthesis segment and decompression with or without fusion for the other stenotic segments. To date, no study has compared the results of these two surgical options for single level degenerative spondylolisthesis with multilevel stenosis.
Methods
The results from a multicenter randomized and observational study, the Spine Patient Outcomes Research Trial (SPORT) comparing multilevel decompression and single level fusion and multi level decompression and multi level fusion for spinal stenosis with spondylolisthesis, were analyzed. The primary outcomes measures were the Bodily Pain and Physical Function scales of the Medical Outcomes Study 36-item Short-Form General Health Survey (SF-36) and the modified Oswestry Disability Index at 1,2, 3 and 4 years postoperatively. Secondary analysis consisted of stenosis bothersomeness index, low back pain bothersomeness, leg pain, patient satisfaction, and self-rated progress.
Results
Overall 207 patients were enrolled to the study, 130 had multlilevel decompression with one level fusion and 77 patients had multi level decompression and multi-level fusion. For all primary and secondary outcome measures, there were no statistically significant differences in surgical outcomes between the two surgical techniques. However, operative time and intraoperative blood loss were significantly higher in the multilevel fusion group.
Conclusion
Decompression and single level fusion and decompression and multi level fusion provide similar outcomes in patients with multilevel lumbar stenosis and single level degenerative spondylolisthesis.
Keywords: degenerative spondylolisthesis, multilevel spinal stenosis, lumbar decompression, fusion
Introduction
Degenerative spondylolisthesis (DS) is defined as a forward slipping of a vertebra with an intact neural arch on another vertebra. Most lumbar DS affects the L4–L5 level. (1,2) It commonly occurs in patients over the age of 50 and affects females 6:1.(3) DS is generally asymptomatic but can be associated with symptomatic spinal stenosis and radiculopathy.(2)
A multicenter randomized and observational trial, the Spine Patient Outcomes Research Trial (SPORT) compared surgical versus nonoperative treatment for patients with DS and spinal stenosis.(4) Although there was a high level of nonadherence in the randomized groups, this study demonstrated significantly more improvement with operative treatment in all primary outcomes compared to nonoperative treatment when an as-treated analysis was performed. This benefit appeared at 3 months and remained significant up to 4 years.(4,5)
Previously, Herkowitz and Kurz (6) prospectively compared decompressions alone with decompression and uninstrumented fusion on patients with symptomatic single-level DS. The fusion group had a significantly better outcomes and lesser progression of slip at a mean 3 years follow-up. While fusion of single-level DS demonstrated superior results over decompression alone (1,6), there are currently no studies that evaluate the different treatment methods for multiple-level spinal stenosis associated with single level DS (single level fusion vs. multiple level fusion).
The extent of this pathology is revealed in the SPORT study. In the study arm which was designed to compare the effectiveness of surgical and nonsurgical treatment among participants with degenerative spondylolisthesis (4), 35% of patients had more than one level of moderate to severe stenosis and 57% of patients who underwent surgery had more than a one level of decompression (4).
Some surgeons surgically treat these patients with a fusion at only the level of current instability and only decompress the other levels. On the other hand, some clinicians elect to incorporate multi-level fusions as a prophylaxis to adjacent level instability in this clinical scenario. Multiple prior studies have shown that laminectomy alone increases segmental instability, unless fusion is performed, (7-11). Therefore, performing a decompression only (no fusion) above a fused segment may cause additional stress on the less stable segment, which may result in an early adjacent segment disease/failure and the need for further surgical intervention.
The addition of fusion levels, however, is not without risks. Fusion of multiple levels is a longer operation with the potential for increased morbidity. It can also promote additional adjacent segment disease, due to the longer lever arm produced with poly-segmental fusions and increased stress at the remaining mobile segments (12-15).
To answer which surgical approach provides the best outcome, a sub-analysis of the SPORT DS study was performed. The purpose of the study was to determine the impact of multilevel decompression with single level fusion compared to multilevel decompression and fusion on patients' outcomes over time. This analysis represents the first clinical study comparing the different treatment methods for multi-level lumbar spinal stenosis and a single level DS.
Materials and Methods
Patient population
The SPORT study was conducted at thirteen medical centers with multidisciplinary spine practices in eleven states in the United States. Six hundred and seven DS patients, out of a total of 892 patients eligible for enrollment, were enrolled in a randomized or observational cohort. Overall, of the 372 patients that underwent surgery, 207 patients had lumbar decompression at more than a one level, with either single or multi-level fusion. Out of these 207 patients, 130 had multi-level decompression and a single level fusion and 77 patients had multi-level decompression and multi-level fusion.
All patients had neurogenic claudication or radicular leg pain with associated neurologic signs, spinal stenosis shown on cross-sectional imaging, and DS shown on lateral radiographs obtained with the patient in a standing position. Patients with isthmic spondylolisthesis were excluded. Only patients with single level of DS were included.
All patients had had persistent symptoms for at least 12 weeks and had been confirmed as surgical candidates by their physicians. Treatment was either decompressive laminectomy with a single level fusion, or decompression with concomitant multi-level fusion.
Outcome Measures
The primary outcomes measures were the Bodily Pain and Physical Function scales of the Medical Outcomes Study 36-item Short-Form General Health Survey (SF-36) and the modified Oswestry Disability Index at 1, 2, 3 and 4 years. Secondary outcome measures included the spinal stenosis bothersomeness index, leg pain bothersomeness, low back pain bothersomeness, and patient satisfaction.
Statistical Analysis
Patients receiving single versus multi-level fusion were compared with respect to demographic, health and clinical characteristics at baseline using proportions or means with chi-squared or t-tests. Reoperation rates were compared using Kaplan Meir estimates and log-rank tests.
The effects on the primary quality of life longitudinal outcomes were assessed using linear mixed models with adjustments for the time of surgery and baseline factors related to treatment choice and missing outcomes (5). The estimated response at designated follow-up times were plotted and compared between the two types of fusion using confidence intervals generated from the mixed models. Area-under-the-curve (AUC) calculations were used for overall comparisons through 48 months.
Results
Overall, 207 patients were eligible for the present study. Of these patients, 130 had multi-level decompression with single level fusion, and 77 patients had multi-level decompression and single level fusion. The proportion of enrollees who supplied data at each follow-up interval ranged from 68% to 90%, with losses due to dropouts, missed visits, and deaths.
Patients Characteristics
When comparing patient demographics between multi-level fusion and single level fusion, no differences were noticed except for more Caucasians in the multi-level fusion group (95% [73] of 77 in the multi-level fusion group compared with 85% [110] of the 130 patients in the single level fusion group) (P=0.047) (Table 1). No differences were discovered when comparing medical comorbidities.
Table 1.
Patient baseline demographic characteristics, comorbidities, health status measures and medications for DS multilevel decompression and fusion patients, according to levels of fusion.
| Two+ Levels Fusion | One Level Fusion | p-value | |
|---|---|---|---|
| (n=77) | (n=130) | ||
| Mean Age (SD) | 66.5 (9) | 66.7 (10.3) | 0.89 |
| Female - no. (%) | 51 (66%) | 81 (62%) | 0.68 |
| Non-Hispanic ethnicity - no. (%)† | 77 (100%) | 124 (95%) | 0.14 |
| White race - no. (%) | 73 (95%) | 110 (85%) | 0.047 |
| Education - At least some college - no. (%) | 51 (66%) | 90 (69%) | 0.77 |
| Work Status - no. (%) | 0.77 | ||
| Full or part time | 28 (36%) | 38 (29%) | |
| Disabled | 5 (6%) | 10 (8%) | |
| Retired | 35 (45%) | 65 (50%) | |
| Other | 9 (12%) | 17 (13%) | |
| Disability compensation - no. (%)‡ | 8 (10%) | 10 (8%) | 0.68 |
| Mean Body Mass Index (BMI), (SD)§ | 28.6 (5.7) | 29.1 (7.2) | 0.64 |
| Smoker - no. (%) | 6 (8%) | 10 (8%) | 0.81 |
| Comorbidities - no. (%) | |||
| Hypertension | 33 (43%) | 49 (38%) | 0.56 |
| Diabetes | 9 (12%) | 17 (13%) | 0.94 |
| Osteoporosis | 8 (10%) | 10 (8%) | 0.68 |
| Heart Problem | 21 (27%) | 23 (18%) | 0.15 |
| Stomach Problem | 15 (19%) | 25 (19%) | 0.89 |
| Bowel or Intestinal Problem | 4 (5%) | 9 (7%) | 0.84 |
| Depression | 6 (8%) | 22 (17%) | 0.10 |
| Joint Problem | 40 (52%) | 75 (58%) | 0.51 |
| Other¶ | 27 (35%) | 48 (37%) | 0.91 |
| Symptom duration > 6 months - no. (%) | 47 (61%) | 78 (60%) | 1 |
| SF-36 scores, mean (SD) ‖ | |||
| Bodily Pain (BP) | 33.1 (19.7) | 31.6 (20.1) | 0.59 |
| Physical Functioning (PF) | 30.2 (21.3) | 33.2 (21.8) | 0.34 |
| Physical Component Summary (PCS) | 28.4 (8.5) | 28.6 (8.2) | 0.83 |
| Mental Component Summary (MCS) | 52 (11.7) | 50.2 (10.9) | 0.25 |
| Oswestry Disability Index (ODI), mean (SD)** | 45.7 (17) | 43.3 (16.6) | 0.32 |
| Stenosis Frequency Index (0-24)†† | 14.2 (5.7) | 14.7 (5.5) | 0.59 |
| Stenosis Bothersome Index (0-24)‡‡ | 15 (5.8) | 15.4 (5.4) | 0.60 |
| Back Pain Bothersomeness§§ | 4.2 (2.1) | 4.4 (1.7) | 0.51 |
| Leg Pain Bothersomeness¶¶ | 4.5 (1.9) | 4.6 (1.7) | 0.65 |
| Patient very dissatisfied with symptoms - no. (%) | 54 (70%) | 100 (77%) | 0.36 |
| Patient's self-assessed health trend - no. (%) | 0.27 | ||
| Problem getting better | 2 (3%) | 4 (3%) | |
| Problem staying about the same | 28 (36%) | 34 (26%) | |
| Problem getting worse | 46 (60%) | 92 (71%) | |
| Insurance | 0.96 | ||
| None | 1 (1%) | 2 (2%) | |
| Employer | 27 (35%) | 45 (35%) | |
| Medicare | 26 (34%) | 44 (34%) | |
| Medicaid | 2 (3%) | 6 (5%) | |
| Private | 21 (27%) | 33 (25%) | |
| Neurogenic claudication - no. (%) | 65 (84%) | 113 (87%) | 0.77 |
| Any neurological deficit - no. (%) | 46 (60%) | 71 (55%) | 0.57 |
| Asymmetric depressed reflexes | 29 (38%) | 30 (23%) | 0.037 |
| Asymmetric decrease in sensory | 18 (23%) | 41 (32%) | 0.27 |
| Asymmetric motor weakness | 23 (30%) | 34 (26%) | 0.68 |
| Olisthesis Level - no. (%) | 0.80 | ||
| L3-L4 | 10 (13%) | 14 (11%) | |
| L4-L5 | 67 (87%) | 116 (89%) | |
| Stenosis Levels - no. (%) | |||
| L2-L3 | 9 (12%) | 19 (15%) | 0.70 |
| L3-L4 | 42 (55%) | 76 (58%) | 0.69 |
| L4-L5 | 77 (100%) | 125 (96%) | 0.20 |
| L5-S1 | 9 (12%) | 12 (9%) | 0.74 |
| Spinal instability - no. (%)* | 6 (8%) | 13 (10%) | 0.78 |
Race or ethnic group was self-assessed. Whites and blacks could be either Hispanic or non-Hispanic.
This category includes patients who were receiving or had applications pending for workers compensation, Social Security compensation, or other compensation.
Body-mass index is the weight in kilograms divided by the square of the height in meters.
Other = problems related to stroke, cancer, fibromyalgia, chronic fatigue syndrome (CFS), post traumatic stress disorder (PTSD), alcohol, drug dependency, lung, liver, kidney, blood vessel, nervous system, migraine or anxiety.
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms.
The Stenosis Frequency Index ranges from 0 to 24, with lower scores indicating less severe symptoms.
The Stenosis Bothersomeness Index ranges from 0 to 24, with lower scores indicating less severe symptoms.
The Low Back Pain Bothersomness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms.
The Leg Pain Bothersomeness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms.
Spinal instability is defined as a change of more than 10 degrees of angulation or more than 4 mm of translation of the vertebrae between flexion and extension of the spine.
Baseline Symptoms
Patients did not demonstrate any statistical difference in baseline pain or disability scores (Table 1). All primary and secondary outcome measures were not statistically different at baseline. When comparing clinical presentations, those who eventually underwent multi-level decompression and multi-level fusion were more likely to present with asymmetric depressed reflexes (38% [29] of 77 in the multi-level fusion group compared with 23% [30] of the 130 patients in the single level fusion group) (P=0.037). In the multi-level fusion group, patients were more likely to have lateral recess stenosis (97% [75] of 77 in the multi-level fusion group compared with 86% [112] of the 130 patients in the single level fusion group) (P=0.016). (Table 1)
Surgical Procedure
Operative time and intraoperative blood loss were significantly higher in the multi-level fusion group (P<0.001, P=0.034, respectively) (Table 2). The average surgical time for the multi-level fusion group was 250 minutes, with a mean blood loss of 784 mL. The average surgical time for the single fusion group was 187 minutes, with a mean blood loss of 623 mL. Interestingly, there was no significant difference between the two groups with regard to the rates of intraoperative and postoperative blood replacement (P=0.062, P=0.36, respectively),
Table 2.
Operative treatments, complications and events.
| Two+ Levels Fusion (n=77) | One Level Fusion (n=130) | p-value | |
|---|---|---|---|
| Specific procedures† | 0.078 | ||
| Non-instrumented fusion | 14 (18%) | 39 (31%) | |
| Instrumented fusion | 62 (82%) | 88 (69%) | |
| Multi-level fusion | 77 (100%) | 0 (0%) | <0.001 |
| Two-level fusion | 60 (78%) | 0 (0%) | |
| Three-level fusion | 17 (22%) | 0 (0%) | |
| Decompression level - no. (%) | |||
| L2-L3 | 19 (26%) | 22 (17%) | 0.19 |
| L3-L4 | 58 (77%) | 107 (82%) | 0.49 |
| L4-L5 | 76 (99%) | 127 (98%) | 0.99 |
| L5-S1 | 46 (60%) | 59 (45%) | 0.064 |
| No. of levels decompresssed - no. (%) | 0.27 | ||
| 2 | 43 (56%) | 84 (65%) | |
| 3+ | 34 (44%) | 46 (35%) | |
| Fusion level - no. (%) | |||
| L3-L4 | 55 (71%) | 12 (9%) | <0.001 |
| L4-L5 | 76 (99%) | 118 (91%) | 0.048 |
| L5-S1 | 40 (52%) | 0 (0%) | <0.001 |
| Fusion type - no. (%) † * | <0.001 | ||
| PLF | 14 (18%) | 39 (31%) | |
| PPS | 45 (59%) | 84 (66%) | |
| 360° | 17 (22%) | 4 (3%) | |
| Operation time, minutes (SD) | 250.4 (94.3) | 186.9 (69.2) | <0.001 |
| Blood loss, cc (SD) | 784.1 (553.2) | 622.9 (505.4) | 0.034 |
| Blood replacement - no. (%) | |||
| Intraoperative replacement | 38 (50%) | 46 (36%) | 0.062 |
| Post-operative transfusion | 14 (18%) | 32 (25%) | 0.36 |
| No. of days in hospital (SD) | 5.2 (3.5) | 4.6 (2.9) | 0.17 |
| Intraoperative complications - no. (%)§ | |||
| Dural tear/spinal fluid leak | 12 (16%) | 11 (8%) | 0.18 |
| Vascular injury | 1 (1%) | 0 (0%) | 0.79 |
| Other | 2 (3%) | 1 (1%) | 0.64 |
| None | 63 (82%) | 118 (91%) | 0.097 |
| Postoperative complications/events - no. (%)¶ | |||
| Nerve root injury | 1 (1%) | 0 (0%) | 0.79 |
| Wound infection | 0 (0%) | 6 (5%) | 0.14 |
| Other | 12 (16%) | 13 (10%) | 0.33 |
| None | 54 (71%) | 81 (63%) | 0.33 |
| Postoperative mortality - no. (%) | |||
| Within 6 weeks of surgery | 0 (0%) | 0 (0%) | |
| Within 3 months of surgery | 0 (0%) | 1 (0.3%) | 0.93 |
| Additional surgeries (1-year rate) - no. (%)‖ | 8 (10%) | 8 (6%) | 0.29 |
| Additional surgeries (2-year rate) | 12 (16%) | 16 (12%) | 0.51 |
| Additional surgeries (3-year rate) | 13 (17%) | 17 (13%) | 0.46 |
| Additional surgeries (4-year rate) | 13 (17%) | 19 (15%) | 0.65 |
| Recurrent stenosis/progressive olysthesis | 5 (7%) | 5 (4%), | |
| Pseudarthrosis/fusion exploration | 0 | 3 (2.4%) | |
| Complication or other | 8 (10.4%) | 9 (7.1%) | |
| New condition | 2 (2.6%) | 1 (NE) |
No cases were reported of aspiration into the respiratory tract, nerve-root injury, or operation at wrong level.
Complications or events occurring up to 8 weeks after surgery are listed. There were no reported cases of bone-graft complication, cerebrospinal fluid leak, paralysis, caudaequina injury, pseudarthrosis, wound dehiscence, or wound hematoma.
One-, two-, three- and four-year post-surgical re-operation rates are Kaplan Meier estimates and p-values are based on the log-rank test. Numbers and percentages are based on the first additional surgery if more than one additional surgery. Surgeries include any additional spine surgery not just re-operation at the same level.
Specific procedure data were available for 76 two+ levels fusion and 127 one level fusion patients.
Fusion type: Posterolateral in situ fusion (PLF), Posterolateral instrumented fusion with pedical screws (PPS), or PPS plus interbody fusion (360°)
Patient died 9 days after surgery of a myocardial infarction. The death was judged as probably related to treatment by the DHMC review and not related to treatment by the external review.
Note: The patient who died at 9 days after surgery would have a missing reoperation variable so that we can't track this information of death after surgery
There was also no significant difference between the two groups with regard to intra operative and post operative complications nor to the re operation rate at 1, 2, 3, and 4 years. At 1 year, 8 patients in both groups underwent additional surgery; 12 and 16 at 2 years; 13 and 17 at 3 years; 13 and 19 patients at 4 years when comparing multi-level to single level fusion patients. Recurrent stenosis and progressive lithesis was noted in 5 patients in each group (7% versus 4%). The rate of pseudarthrosis and fusion exploration was higher in the single level fusion group at 2.4% to 0%. Mortality did not differ between the two groups.
Outcomes
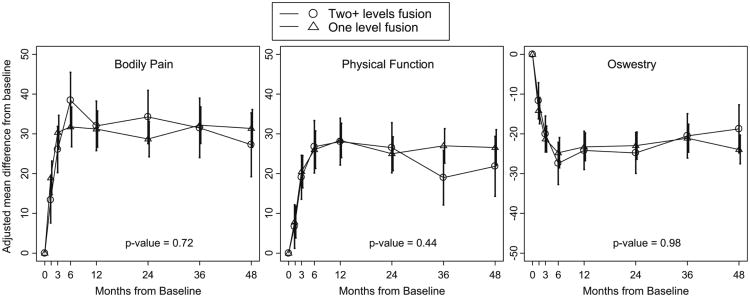
For all primary and secondary outcome measures, there were no differences in surgical outcomes when comparing single level and multi-level fusion in patients with DS and multi-level stenosis at 1, 2, 3, and 4 years follow up (Table 3). There was a trend towards more improvement in in SF-36 physical function score at 3 years for one level fusion than multi-level fusion. This change became insignificant at 4 years (Figure 1).
Table 3.
Change in scores and treatment effects for primary and secondary outcomes in the randomized and observational cohorts combined DS multilevel decompression and fusion patients, according to levels of fusion.
| Overall Mean (SE)(before surgery) | 1-Year | 2-Year | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean Change (SE)or percent | Mean Change (SE)or percent | ||||||||
| Two+ Levels Fusion | One Level Fusion | Treatment Effect (95% CI)† | p-value | Two+ Levels Fusion | One Level Fusion | Treatment Effect (95% CI)† | p-value | ||
| Primary Outcomes | (n = 58) | (n = 102) | (n = 67) | (n = 119) | |||||
| SF-36 Bodily Pain (BP) (0-100) (SE)‡ | 29.9 (1.3) | 32 (3.2) | 31.2 (2.3) | 0.8 (-7.2, 8.8) | 0.84 | 34.2 (3.4) | 28.7 (2.3) | 5.5 (-2.7, 13.8) | 0.19 |
| SF-36 Physical Function (PF) (0-100) (SE)‡ | 31.2 (1.5) | 28 (3) | 28.3 (2.2) | -0.3 (-7.8, 7.2) | 0.94 | 26.5 (3.2) | 25 (2.2) | 1.5 (-6.3, 9.3) | 0.70 |
| SF-36 Physical Component Summary (PCS) (0-100) (SE)‡ | 27.7 (0.6) | 12.3 (1.3) | 12 (0.94) | 0.4 (-2.9, 3.6) | 0.83 | 12.2 (1.4) | 10.9 (0.93) | 1.4 (-2, 4.7) | 0.42 |
| SF-36 Mental Component Summary (MCS) (0-100) (SE)‡ | 50.5 (0.8) | 2.8 (1.2) | 2 (0.9) | 0.7 (-2.3, 3.8) | 0.64 | 3.4 (1.3) | 2.5 (0.88) | 0.9 (-2.3, 4.1) | 0.57 |
| Oswestry Disability Index (ODI) (0-100) (SE)§ | 45.8 (1.2) | -24.2 (2.5) | -23.3 (1.8) | -0.9 (-7, 5.3) | 0.78 | -24.8 (2.6) | -23 (1.7) | -1.8 (-8.2, 4.6) | 0.58 |
| Secondary Outcomes | |||||||||
| Stenosis Bothersomeness Index (0-24) (SE)¶ | 15.5 (0.4) | -9 (0.83) | -9.2 (0.61) | 0.2 (-1.9, 2.3) | 0.84 | -9.5 (0.9) | -8.3 (0.6) | -1.2 (-3.5, 1) | 0.27 |
| Low back pain bothersomeness (0-6) (SE)** | 4.3 (0.1) | -2.2 (0.2) | -2.4 (0.2) | 0.2 (-0.3, 0.8) | 0.41 | -2.1 (0.3) | -2.1 (0.2) | 0 (-0.6, 0.6) | 0.98 |
| Leg pain (0-6) (SE) ‖ | 4.6 (0.1) | -2.9 (0.2) | -2.8 (0.2) | -0.1 (-0.8, 0.5) | 0.63 | -3 (0.3) | -2.6 (0.2) | -0.4 (-1, 0.3) | 0.25 |
| Very/somewhat satisfied w/symptoms (%) | 2.9 (1.7) | 63.7 | 67.5 | -3.9 (-21.2, 13.5) | 0.73 | 68.6 | 60.5 | 8.1 (-10, 26.2) | 0.39 |
| Self-rated progress: major improvement (%) | 72.1 | 68.1 | 4.1 (-12, 20.1) | 0.57 | 73.7 | 64.7 | 9 (-8, 26.1) | 0.43 | |
| Overall Mean (SE)(before surgery) | 3-Year | 4-Year | |||||||
| Mean Change (SE)or percent | Mean Change (SE)or percent | ||||||||
| Two+ Levels Fusion | One Level Fusion | Treatment Effect (95% CI)† | p-value | Two+ Levels Fusion | One Level Fusion | Treatment Effect (95% CI)† | p-value | ||
| Primary Outcomes | (n = 60) | (n = 109) | (n = 47) | (n = 93) | |||||
| SF-36 Bodily Pain (BP) (0-100) (SE)‡ | 29.9 (1.3) | 31.5 (3.8) | 32.2 (2.3) | -0.7 (-9.6, 8.3) | 0.88 | 27.3 (4.1) | 31.4 (2.4) | -4.1 (-13.6, 5.4) | 0.40 |
| SF-36 Physical Function (PF) (0-100) (SE)‡ | 31.2 (1.5) | 19 (3.5) | 27 (2.2) | -8 (-16.3, 0.3) | 0.06 | 21.8 (3.8) | 26.5 (2.3) | -4.7 (-13.7, 4.2) | 0.30 |
| SF-36 Physical Component Summary (PCS) (0-100) (SE)‡ | 27.7 (0.6) | 9.8 (1.5) | 11.9 (0.95) | -2.1 (-5.7, 1.5) | 0.26 | 10.3 (1.7) | 11 (0.99) | -0.7 (-4.6, 3.3) | 0.73 |
| SF-36 Mental Component Summary (MCS) (0-100) (SE)‡ | 50.5 (0.8) | 3.1 (1.5) | 2 (0.91) | 1.1 (-2.4, 4.6) | 0.52 | 3.5 (1.7) | 1.7 (0.96) | 1.8 (-2.1, 5.7) | 0.37 |
| Oswestry Disability Index (ODI) (0-100) (SE)§ | 45.8 (1.2) | -20.5 (2.8) | -21.1 (1.8) | 0.6 (-6.2, 7.3) | 0.87 | -18.8 (3.1) | -23.9 (1.8) | 5.2 (-2, 12.4) | 0.16 |
| Secondary Outcomes | |||||||||
| Stenosis Bothersomeness Index (0-24) (SE)¶ | 15.5 (0.4) | -8 (0.98) | -9.1 (0.62) | 1.1 (-1.3, 3.4) | 0.36 | -8.2 (1.1) | -9.2 (0.63) | 1 (-1.5, 3.5) | 0.44 |
| Low back pain bothersomeness (0-6) (SE)** | 4.3 (0.1) | -1.8 (0.3) | -2.1 (0.2) | 0.3 (-0.4, 0.9) | 0.44 | -1.7 (0.3) | -2.2 (0.2) | 0.6 (-0.2, 1.3) | 0.13 |
| Leg pain (0-6) (SE)‖ | 4.6 (0.1) | -2.9 (0.3) | -2.9 (0.2) | 0 (-0.7, 0.7) | 0.93 | -3.2 (0.3) | -3 (0.2) | -0.2 (-1, 0.5) | 0.54 |
| Very/somewhat satisfied w/symptoms (%) | 2.9 (1.7) | 51.9 | 63.7 | -11.8(-32.9, 9.3) | 0.20 | 50.6 | 59 | -8.4 (-32.6, 15.8) | 0.54 |
| Self-rated progress: major improvement (%) | 68.9 | 67.7 | 1.2 (-17.4, 19.7) | 1 | 60.1 | 63 | -3 (-25.1, 19.2) | 0.73 | |
Adjusted for age, gender, work status, BMI, any neurofroamen L or R, hypertension, depression, osteoporosis, joint problems, current symptom duration, reflex deficit, number of moderate/severe stenotic levels, treatment preference, other*** comorbidity, baseline score (for SF-36, ODI), baseline stenosis bothersomeness, and center.
Treatment effect is the difference in mean change from baseline between two+ levels fusion and one level fusion.
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms
The Stenosis Bothersomeness Index ranges from 0 to 24, with lower scores indicating less severe symptoms
The Leg Pain Bothersomeness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms
The Low Back Pain Bothersomeness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms
The sample sizes for the as-treated analyses reflect the number of patients contributing to the estimate in a given time-period using the longitudinal modeling strategy explained in the methods section.
Other = problems related to stroke, cancer, fibromyalgia, chronic fatigue syndrome (CFS), post traumatic stress disorder (PTSD), alcohol, drug dependency, lung, liver, kidney, blood vessel, nervous system, migraine or anxiety.
Figure 1.
Primary outcomes over time according to levels of fusion, along with time weighted average 4 years area under curve p-value that compares two+ levels fusion to one level fusion.
Discussion
DS with multi-level stenosis is a common problem (4). Treatment choices are either conservative care or operative intervention. When treating operatively, decompression and fusion of the spondylolisthesis segment provides better clinical outcome than decompression alone (1,6).
Different fusion techniques for treating DS did not show consistent differences in clinical outcome over 4 years (16). The other stenotic segments can be decompressed only, or decompressed and fused. To date, no study has compared the results of these two surgical options. In this sub-analysis study, no clinical differences were found when comparing multi-level fusion to single level fusion in this patient cohort. Multi-level fusion, however, came at the expense of higher intraoperative blood loss and longer operative time.
Many surgeons elect to limit fusion to only the level demonstrating instability in this patient cohort. Others have performed longer fusion as prophylaxis to future adjacent segment instability. When performing a central decompression above a fused segment, the integrity of posterior complex (spinous process-supraspinous ligament-spinous process), which acts as a tension band in flexion and helps stabilize the spine, is frequently excised. The caudal segment that is fused may cause additional stress on the adjacent unstable segment, and the patient may develop segmental instability (7-11, 17). The patient is also exposed to the risk of bone regrowth at the decompressed level, if fusion is not performed (18). On the other hand, fusion of multiple segments may impose an increased stress on adjacent levels and increase the risk of adjacent segment disease (12-15).
While these theories may make intellectual sense, no clinical studies have examined if patients with multi-level stenosis and single level DS would benefit from multi-level or single level fusion. In this study, no clinical outcomes measures were found statistically significant, but more importantly, there was no difference in recurrent stenosis and additional surgeries at four-year follow-up. Interestingly, there were more patients requiring pseudarthrosis or fusion exploration during the 4 year period for single level fusion than multi-level fusions. This surprising finding is partially explained by the higher rate of non-instrumented fusion in the single level fusion compared to the multi-level fusion, 39 patients versus 14 patients respectively (19) (Two out of the 3 patients that had pseudoarthrosis). Although clinical outcome measures did not differ substantially between the two groups, the main difference found was in operative time and intraoperative blood loss. Time and blood loss increased in the multi fusion group although intra- and post-operative blood transfusion rate did not differ.
In another subanalysis of the SPORT trial, Park et al studied the impact of multi-level lumbar stenosis without or with DS compared to single level disease on patients' clinical outcomes. Unlike in spinal stenosis patients and no DS, where the number of levels treated did not predict outcome, patients with DS and multiple level spinal stenosis had worse outcomes for all primary and secondary outcome measurements at 2 years follow-up when compared to patients with single level disease (20).
While both spinal stenosis and DS patients usually undergo decompression of the involved segments, patients with DS will also typically undergo fusion at the DS level or at all of the decompressed levels. Our study shows similar clinical outcomes for the single and multi-level fusion groups. It demonstrates that the relatively worse clinical outcome in DS with multi-level spinal stenosis found in the Park et al study is not due to one specific surgical technique. Furthermore, in an older patient population with more medical co-morbidities and frail medical conditions, the added operative time and increased blood loss for multi-level patients may not be warranted, especially if 4 year clinical follow does not demonstrate added clinical benefit.
As a part of the SPORT study, our study has similar advantages of the prior Sport studies (4,5,20). Limitations of this study include the lack of randomization and subgroup analysis of original data. Third, some surgeon may elect to perform multi-level fusion due to pre-existing adjacent level disc or facet degeneration (21). Data regarding the level of non-DS level disc and facet degeneration that was incorporated into the fusion is not available for those patients who had multi-level fusion. Fourth, surgeons may interpret the MRI differently from the enrolling physician and stenosis may have worsened between enrollment and surgery. Fifth, this study is a short-term follow up. Clinical differences may be evident at longer follow-up so future studies at longer time points may be warranted. Despite these points, this is the first study we are aware of, that systematically compared independently outcomes for two different methods of treating DS and multi-level spinal stenosis.
Conclusion
In summary, this study demonstrates that in patients with DS and multiple level stenosis in addition to decompression and fusion of the spondylolisthesis segment, decompression alone or decompression and fusion at the other stenotic segments results in similar outcomes. However, operative time and intraoperative blood loss are increased in the group of patients who undergo multiple level fusions.
Key points.
Patients who underwent multilevel decompression and multilevel fusion were noticed to have longer operative time and increased blood loss compared to patients who underwent multilevel decompression and a single level fusion.
There was no significant difference between the two groups of patients with regard to the rates of intraoperative and postoperative blood replacement.
Decompression and single level fusion and decompression and multilevel fusion provide similar outcomes in patients with multilevel lumbar stenosis and single level degenerative spondylolisthesis.
Acknowledgments
The manuscript submitted does not contain information about medical device(s)/drug(s). NIH and NIAMS grant funds were received in support of this work. Relevant financial activities outside the submitted work: Stocks, Travel/Accommodations, Grants, Consultancy, Royalties, Expert Testimony, Board Membership.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Cauchoix J, Benoist M, Chassaing V. Degenerative spondylolisthesis. Clin Orthop Relat Res. 1976;115:112–29. [PubMed] [Google Scholar]
- 2.Jacobsen S, Sonne-Holm S, Rovsing H, et al. Degenerative lumbar spondylolisthesis: an epidemiological perspective: the Copenhagen Osteoarthritis Study. Spine. 2007;32:120–25. doi: 10.1097/01.brs.0000250979.12398.96. [DOI] [PubMed] [Google Scholar]
- 3.Rosenberg N. Degenerative spondylolisthesis: predisposing factors. J Bone Joint Surg Am. 1975;57:467–74. [PubMed] [Google Scholar]
- 4.Weinstein J, Lurie JD, Tosteson TD, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med. 2007;356:2257–70. doi: 10.1056/NEJMoa070302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009;91:1295–304. doi: 10.2106/JBJS.H.00913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991;73:802–8. [PubMed] [Google Scholar]
- 7.Hopp E, Tsou PM. Postdecompression lumbar instability. Clin Orthop. 1988;227:143–151. [PubMed] [Google Scholar]
- 8.Johnsson KE, Willner S, Johnsson K. Postoperative instability after decompression for lumbar spinal stenosis. Spine. 1986;11:107–110. doi: 10.1097/00007632-198603000-00001. [DOI] [PubMed] [Google Scholar]
- 9.Katz JN, Lipson SJ, Larson MG. The outcome of decompressive laminectomy for degenerative lumbar stenosis. J Bone Joint Surg Am. 1991;73:809–816. [PubMed] [Google Scholar]
- 10.Lu WW, Luk KD, Ruan DK, Fei ZQ, Leong JC. Stability of the whole lumbar spine after multilevel fenestration and discectomy. Spine. 1999;24:1277–1282. doi: 10.1097/00007632-199907010-00002. [DOI] [PubMed] [Google Scholar]
- 11.Subramaniam V, Chamberlain RH, Theodore N, Baek S, Safavi-Abbasi S, Senođlu M, Sonntag VK, Crawford NR. Biomechanical effects of laminoplasty versus laminectomy: stenosis and stability. Spine. 2009;34:E573–8. doi: 10.1097/BRS.0b013e3181aa0214. [DOI] [PubMed] [Google Scholar]
- 12.Hsu K, Zucherman J, White A. The long-term effect of lumbar spine fusion:deterioration of adjacent motion segments. In: Yonenobu K, Ono K, Takemitsu Y, editors. Lumbar Fusion and Stabilization. Tokyo: Springer; 1993. pp. 54–64. [Google Scholar]
- 13.Chow DH, Luk KD, Evans JH, et al. Effects of short anterior lumbar interbody fusion on biomechanics of neighboring unfused segments. Spine. 1996;21:549–55. doi: 10.1097/00007632-199603010-00004. [DOI] [PubMed] [Google Scholar]
- 14.Nagata H, Schendel MJ, Transfeldt EE, et al. The effects of immobilization of long segments of the spine on the adjacent and distal facet force and lumbosacral motion. Spine. 1993;18:2471–9. doi: 10.1097/00007632-199312000-00017. [DOI] [PubMed] [Google Scholar]
- 15.Chen CS, Cheng CK, Liu CL, et al. Stress analysis of the disc adjacent to interbody fusion in lumbar spine. Med Eng Phys. 2001;23:483–91. doi: 10.1016/s1350-4533(01)00076-5. [DOI] [PubMed] [Google Scholar]
- 16.Abdu WA, Lurie JD, Spratt KF, Tosteson AN, Zhao W, Tosteson TD, Herkowitz H, Longely M, Boden SD, Emery S, Weinstein JN. Degenerative spondylolisthesis: does fusion method influence outcome? Four-year results of the spine patient outcomes research trial. Spine. 2009;34:2351–60. doi: 10.1097/BRS.0b013e3181b8a829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tai CL, Hsieh PH, Chen WP, Chen LH, Chen WJ, Lai PL. Biomechanical comparison of lumbar spine instability between laminectomy and bilateral laminotomy for spinal stenosis syndrome - an experimental study in porcine model. BMC Musculoskelet Disord. 2008;9:84. doi: 10.1186/1471-2474-9-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Postacchini F, Cinotti G. Bone regrowth after surgical decompression for lumbar spinal stenosis. J Bone Joint Surg Br. 1992;74:862–9. doi: 10.1302/0301-620X.74B6.1447247. [DOI] [PubMed] [Google Scholar]
- 19.Fischgrund JS, Mackay M, Herkowitz HN, Brower R, Montgomery DM, Kurz LT. 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine. 1997;22:2807–2812. doi: 10.1097/00007632-199712150-00003. [DOI] [PubMed] [Google Scholar]
- 20.Park DK, An HS, Lurie JD, Zhao W, Tosteson A, Tosteson TD, Herkowitz H, Errico T, Weinstein JN. Does multilevel lumbar stenosis lead to poorer outcomes?: a subanalysis of the Spine Patient Outcomes Research Trial (SPORT) lumbar stenosis study. Spine. 2010;35:439–46. doi: 10.1097/BRS.0b013e3181bdafb9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Herkowitz HN, Abraham DJ, Albert TJ. Management of degenerative disc disease above an L522–S1 segment requiring arthrodesis. Spine. 1999;24:1268–70. doi: 10.1097/00007632-199906150-00018. [DOI] [PubMed] [Google Scholar]