Abstract
Study Design
Retrospective subgroup analysis of prospectively collected data according to treatment received.
Objective
The purpose of this study is to determine if obesity affects treatment outcomes for lumbar stenosis (SpS) and degenerative spondylolisthesis (DS).
Summary of Background Data
Obesity is thought to be associated with increased complications and potentially less favorable outcomes following the treatment of degenerative conditions of the lumbar spine. This, however, remains a matter of debate in the existing literature.
Methods
An as-treated analysis was performed on patients enrolled in the Spine Patient Outcomes Research Trial (SPORT) for the treatment of SpS or DS. A comparison was made between patients with a body mass index (BMI) <30 (“non-obese”, n=373 SpS, 376 DS) and those with a BMI ≥ 30 (“obese”, n=261 SpS, 225 DS). Baseline patient characteristics, intraoperative data, and complications were documented. Primary and secondary outcomes were measured at baseline and regular follow-up time intervals up to 4 years. The difference in improvement over baseline between surgical and nonsurgical treatment (i.e. treatment effect) was determined at each follow-up interval for the obese and nonobese groups.
Results
At 4-years follow-up, operative and nonoperative treatment provided improvement in all primary outcome measures over baseline in patients with BMI of < 30 and ≥ 30. For SpS patients, there were no differences in the surgical complication or reoperation rates between groups. DS patients with BMI ≥ 30 had a higher postoperative infection rate (5% vs. 1%, p=0.05) and twice the reoperation rate at 4-years follow-up (20% vs. 11%, p=0.01) than those with BMI < 30. At 4-years, surgical treatment of SpS and DS was equally effective in both BMI groups in terms of the primary outcome measures, with the exception that obese DS patients had less improvement from baseline in the SF36 physical function score compared to nonobese patients (22.6 vs. 27.9, p=0.022). With nonoperative treatment, SpS patients with BMI ≥ 30 did worse in regards to all three primary outcome measures, and DS patients with BMI ≥ 30 had similar SF-36 bodily pain scores but less improvement over baseline in the SF-36 physical function and ODI scores. Treatment effects for SpS and DS were significant within each BMI group for all primary outcome measures, in favor of surgery. Obese patients had a significantly greater treatment effect compared to nonobese patients with SpS (ODI, p=0.037) and DS (SF36 PF, p=0.004), largely due to the relatively poor outcome of nonoperative treatment in obese patients.
Conclusion
Obesity does not affect the clinical outcome of operative treatment for SpS. There are higher rates of infection and reoperation and less improvement from baseline in the SF-36 physical function score in obese patients following surgery for DS. Nonoperative treatment may not be as effective in obese patients with SpS or DS.
Keywords: surgery, lumbar, spinal stenosis, degenerative spondylolisthesis, outcomes, body mass index (BMI)
Introduction
The obesity epidemic in the United States has come to the forefront of medical debate over the last decade. Based on 2005-2006 epidemiological data, 32.7 percent of U.S. adults 20 years and older are overweight, 34.3 percent are obese and 5.9 percent are extremely obese [1]. Body mass index (BMI), expressed as a weight to height ratio (kg/m2), is used to characterize an individual's body fat. A BMI greater than 30 defines obesity. Obesity has been shown to be a significant risk factor for and contributor to increased morbidity and mortality, cardiovascular disease, diabetes, osteoarthritis, sleep apnea, and depression, and reduced quality of life [2,3]. Additionally, obesity has been shown to be an independent predictor of back pain and its severity [5], and may also play a role in the chronicity and recurrence of low back pain [4]. More specifically, obesity has been associated with lumbar disc degeneration leading to low back pain, sciatica, and lumbar spinal stenosis [6].
The mechanism by which obesity causes lumbar disc degeneration is not well understood, but is likely the result of a combination of factors. Both static compressive loading and increased pressures with particular postures may result in damage to the integrity of the disc, followed by mechanical compression or chemical damage to the nerve roots [7]. In addition, the acute response of the spine to loading may represent a risk factor for low back pain in the obese. A greater period of recovery is necessary for obese individuals to re-establish intervertebral disc height after such a load [8]. Recent studies indicate a genetic component in disc degeneration in the obese. A collagen IX polymorphism (Trp3 allele) seems to act synergistically with persistent obesity in the development posterior disc bulge, decreased disc height, and dark nucleus pulposis [9]. The systemic effects of a common inflammatory mechanism have also been implicated in the development of disc degeneration [10].
Several studies have shown a clear link between obesity and increased complication rates after spine surgery [11]. Complications include wound infection, cerebrospinal fluid leak, deep vein thrombosis, cardiac events, pneumonia, prolonged intubation, pseudoarthrosis, urological issues, and position-related palsies. Obesity was found to be an independent risk factor for surgical site infection, both superficial and deep [34]. Obese spine patients also have increased transfusion requirements and utilize more resources [12]. The increased complication rate may be related to more difficult exposure, dissection, retraction and longer operating times [22].
There remains much controversy as to whether obesity influences the outcome of surgical treatment of spinal disease [23]. Most recent studies conclude that obese patients can achieve similar benefits to non-obese patients provided the indications for surgical intervention are based on sound clinical judgment [24,25,26,27]. There is equivocal evidence on the influence of obesity on the outcome of treatment of patients with lumbar spinal stenosis and degenerative spondylolisthesis. The purpose of this study is to use the SPORT database to determine whether or not obesity affects the clinical outcome of the treatment of stenosis and degenerative spondylolisthesis. We hypothesize that obesity will be associated with a worse outcome after treatment of lumbar spinal stenosis and degenerative spondylolisthesis.
Materials and Methods
Study Design
SPORT was conducted at thirteen multidisciplinary spine practices in eleven states across the United States. The details of methods have been reported previously. [13] [14] [15]
Patient Population
All patients had neurogenic claudication or radicular leg pain with associated neurological signs, spinal stenosis seen on cross-sectional imaging, symptoms that had persisted for at least twelve weeks, and physician confirmation that they were a surgical candidate. Patients with degenerative spondylolisthesis seen on standing lateral radiographs were included in a separate analysis.
Patients with adjacent levels of stenosis were eligible, but those with spondylolysis and isthmic spondylolisthesis were not. Pre-enrollment nonoperative care was not specified but included physical therapy (68%), epidural injections (55%), chiropractic care (25%), anti-inflammatory medications (63%), and opioid analgesics (30%). Enrollment began in March 2000 and ended in February 2005.
Study Interventions
Stenosis and degenerative spondylolisthesis patients were offered participation in either a randomized or observational cohort. Participants in the randomized cohort received computer-generated random treatment assignments blocked by center; those in the observational cohort chose their treatment with their physician. The protocol surgery consisted of a standard posterior decompressive laminectomy with or without bilateral single-level fusion (autogenous iliac crest bone-grafting with or without posterior pedicle screw instrumentation)
The non- operative protocol was “usual recommended care,” which includes, at least, active physical therapy, education and counseling with instructions regarding home exercise, and nonsteroidal anti-inflammatory drugs if the patient can tolerate them.
Because of extensive crossover in the randomized cohort (that is, some patients randomized to nonoperative care received operative care and vice versa) and similar baseline characteristics and outcomes between randomized and observational patients when analyzed by treatment, the two groups were combined in this “as-treated” analysis.
Study Measures
Data used in this study were obtained from patient questionnaires completed at baseline, six weeks, three months, six months, one year, two years, and four years after enrollment or surgery. Primary outcome measures included the bodily pain and physical function domains of the SF-36 [16] and the American Academy of Orthopaedic Surgeons MODEMS (Musculoskeletal Outcomes Data Evaluation and Management System) version of the Oswestry Disability Index. [17] Secondary measures included patient self-reported improvement, work status, and satisfaction with current symptoms and with care, and the mental component score of the SF-36. [18] Symptom severity was measured by the low back pain bothersomeness scale (Ranges from 0 to 6, with lower scores indicating less severe symptoms), the sciatica bothersomeness index (SBI, Range from 0 to 24, with lower scores indicating less severe symptoms), and leg pain bothersomeness index. [19] [20] [21] The SF-36 scales and the ODI range from 0 to 100, the SBI from 0 to 24, and the low back pain bothersomeness scale from 0 to 6. Higher scores indicated more severe symptoms on the ODI, SBI, and low back pain bothersomeness scale, whereas higher scores indicated less severe symptoms on the SF-36.
Statistical Analysis
Baseline characteristics between nonobese (BMI≤30) and obese groups (BMI>30) were compared using a chi-square test for categorical variables and t-tests for continuous variables. Primary analyses compared surgical and non-operative treatments using changes from baseline at each follow-up, with a mixed effects longitudinal regression model including a random individual effect to account for correlation between repeated measurements within individuals. Because of the crossover, analyses were based on treatments actually received in the combined randomized and observational cohorts. In these as-treated analyses, the treatment indicator was a time-varying covariate, allowing for variable times of surgery. Times are measured from the beginning of treatment, i.e. the time of surgery for the surgical group and the time of enrollment for the non-operative group. Therefore, all changes from baseline prior to surgery were included in the estimates of the non-operative treatment effect. After surgery, changes were assigned to the surgical group with follow-up measured from the date of surgery. Repeated measures of outcomes were used as the dependent variables, and treatment received was included as a time-varying covariate. To adjust for potential confounding, baseline variables associated with missing data or treatment received were included as adjusting covariates in longitudinal regression models. In addition, age, gender, race, smoking status, compensation, comorbidities, diagnosis, center, treatment preference, self-assessed health trend, and baseline outcome scores (for SF36 and ODI) were included in longitudinal regression models. Secondary and binary outcomes were analyzed using generalized estimating equations (GEE) that assumed a compound symmetry working correlation structure. The outcomes were stratified by obesity and outcomes between these sub-groups at each time-point were compared using a multiple degrees of freedom Wald test. Across the four- year follow-up, overall comparisons of area-under-curve between these sub-groups were made by using a Wald test. Computations were done using SAS procedures PROC MIXED for continuous data and PROC GENMOD for binary and non-normal secondary outcomes (SAS version 9.1 Windows XP Pro, Cary, NC). Statistical significance was defined as p < 0.05 based on a two-sided hypothesis test with no adjustments made for multiple comparisons.
Results
Spinal Stenosis
There were 373 patients in the spinal stenosis group with a BMI < 30 and 261with a BMI ≥ 30. Differences between the groups at baseline are noted in Table 1. Significant demographic differences were noted between the groups in mean age, education, income under 50,000, work status, and compensation claim. The mean BMI in the nonobese and obese groups for the stenosis cohort was 25.9 ± 2.9 and 34.6 ± 4.5, respectively (p<0.001). Comorbidities differed significantly between the groups at baseline (Table 1). The obese patient group was noted to contain a higher percentage of hypertension, diabetes, depression, heart problems, stomach problems, bowel problems, and other problems. The obese patients were noted to have worse baseline self reported scores on the SF36 physical functioning, vitality, and physical component summary domains. At baseline, a larger percentage of the obese patients had an asymmetric sensory decrease (Table 1).
Table 1.
Patient Baseline Demographic Characteristics, Comorbid Conditions, Clinical Findings, and Health Status Measures.
| Characteristics | Spinal Stenosis | Degenerative Spondylolisthesis | ||||
|---|---|---|---|---|---|---|
| Normal or overweight (BMI<30) | Obese (BMI≥30) | p-value | Normal or overweight (BMI<30) | Obese (BMI≥30) | p-value | |
| (n=373) | (n=261) | (n=376) | (n=225) | |||
| Mean Age (SD) | 66.2 (12.2) | 62.3 (10.5) | <0.001 | 67.4 (10.5) | 63.7 (9.5) | <0.001 |
| Female - no.(%) | 139 (37%) | 110 (42%) | 0.25 | 241 (64%) | 171 (76%) | 0.003 |
| Ethnicity: Not Hispanic† | 356 (95%) | 249 (95%) | 0.87 | 366 (97%) | 221 (98%) | 0.68 |
| Race - White† | 319 (86%) | 214 (82%) | 0.28 | 326 (87%) | 180 (80%) | 0.039 |
| Education - At least some college | 249 (67%) | 152 (58%) | 0.035 | 263 (70%) | 137 (61%) | 0.029 |
| Income - Under $50,000 | 58 (16%) | 64 (25%) | 0.007 | 67 (18%) | 70 (31%) | <0.001 |
| Marital Status - Married | 261 (70%) | 185 (71%) | 0.87 | 260 (69%) | 136 (60%) | 0.037 |
| Work Status | <0.001 | 0.043 | ||||
| Full or part time | 109 (29%) | 89 (34%) | 115 (31%) | 77 (34%) | ||
| Disabled | 24 (6%) | 36 (14%) | 25 (7%) | 26 (12%) | ||
| Other | 240 (64%) | 136 (52%) | 236 (63%) | 122 (54%) | ||
| Compensation - no. (%)‡ | 14 (4%) | 34 (13%) | <0.001 | 23 (6%) | 18 (8%) | 0.47 |
| Mean Body Mass Index (BMI), (SD)§ | 25.9 (2.9) | 34.6 (4.5) | <0.001 | 25.5 (2.9) | 35.3 (5.4) | <0.001 |
| Smoker | 41 (11%) | 21 (8%) | 0.27 | 35 (9%) | 16 (7%) | 0.43 |
| Comorbidities - no.(%) | ||||||
| Hypertension | 151 (40%) | 137 (52%) | 0.004 | 144 (38%) | 131 (58%) | <0.001 |
| Diabetes | 32 (9%) | 64 (25%) | <0.001 | 30 (8%) | 50 (22%) | <0.001 |
| Depression | 29 (8%) | 41 (16%) | 0.003 | 50 (13%) | 48 (21%) | 0.014 |
| Heart Problem | 110 (29%) | 55 (21%) | 0.022 | 71 (19%) | 51 (23%) | 0.31 |
| Lung Problem | 28 (8%) | 20 (8%) | 0.94 | 25 (7%) | 20 (9%) | 0.40 |
| Stomach Problem | 76 (20%) | 63 (24%) | 0.30 | 66 (18%) | 67 (30%) | <0.001 |
| Bowel or Intestinal Problem | 39 (10%) | 47 (18%) | 0.009 | 26 (7%) | 17 (8%) | 0.90 |
| Liver Problem | 6 (2%) | 4 (2%) | 0.80 | 3 (1%) | 5 (2%) | 0.27 |
| Kidney Problem | 16 (4%) | 13 (5%) | 0.83 | 13 (3%) | 14 (6%) | 0.17 |
| Blood Vessel Problem | 19 (5%) | 19 (7%) | 0.33 | 26 (7%) | 12 (5%) | 0.55 |
| Nervous System Problem | 5 (1%) | 8 (3%) | 0.22 | 13 (3%) | 9 (4%) | 0.91 |
| Joint Problem | 197 (53%) | 149 (57%) | 0.33 | 207 (55%) | 137 (61%) | 0.19 |
| Other¶ | 289 (77%) | 209 (80%) | 0.49 | 278 (74%) | 198 (88%) | <0.001 |
| SF-36 scores, mean(SD)†† | ||||||
| Bodily Pain (BP) | 34.5 (20.2) | 32 (18.9) | 0.12 | 34.6 (19) | 31.2 (19.3) | 0.033 |
| Physical Functioning (PF) | 36.7 (23.9) | 32.1 (22.2) | 0.013 | 38.2 (22.9) | 27.9 (20) | <0.001 |
| Vitality (VT) | 45.3 (22.1) | 38.5 (20.6) | <0.001 | 46.8 (21.6) | 37.8 (22.2) | <0.001 |
| Physical Component Summary (PCS) | 30.4 (8.8) | 28.7 (8.3) | 0.018 | 30.7 (8.3) | 27.6 (8.2) | <0.001 |
| Mental Component Summary (MCS) | 49.8 (12.2) | 48.6 (11.4) | 0.20 | 50.6 (11.2) | 49.2 (12) | 0.13 |
| Oswestry Disability Index (ODI)(SD)‡‡ | 41.3 (19.2) | 44 (17.4) | 0.067 | 39.7 (17.8) | 44.7 (17.6) | 0.001 |
| Sciatica Frequency Index (0-24)(SD)§§ | 13.9 (5.6) | 13.8 (6) | 0.84 | 13.9 (5.6) | 14 (5.5) | 0.77 |
| Sciatica Bothersome Index (0-24)(SD)§§ | 14.4 (5.4) | 14.3 (6.2) | 0.83 | 14.5 (5.7) | 15.1 (5.4) | 0.22 |
| Back Pain Bothersomeness (0-6)(SD)¶¶ | 4 (1.8) | 4.2 (1.9) | 0.31 | 4.1 (1.9) | 4.5 (1.6) | 0.005 |
| Satisfaction with symptoms - very dissatisfied | 259 (69%) | 174 (67%) | 0.52 | 253 (67%) | 163 (72%) | 0.22 |
| Patient self-assessed health trend - no.(%) | 0.79 | 0.044 | ||||
| Getting better | 26 (7%) | 20 (8%) | 29 (8%) | 9 (4%) | ||
| Staying about the same | 123 (33%) | 80 (31%) | 128 (34%) | 66 (29%) | ||
| Getting worse | 219 (59%) | 159 (61%) | 212 (56%) | 149 (66%) | ||
| Treatment preference at baseline - no.(%) | 0.66 | 0.10 | ||||
| Preference for non-surg | 140 (38%) | 89 (34%) | 158 (42%) | 77 (34%) | ||
| Not sure | 70 (19%) | 51 (20%) | 77 (20%) | 60 (27%) | ||
| Preference for surgery | 162 (43%) | 121 (46%) | 141 (38%) | 87 (39%) | ||
| Pseudoclaudication - Any | 303 (81%) | 205 (79%) | 0.46 | 319 (85%) | 192 (85%) | 0.96 |
| SLR or Femoral Tension | 71 (19%) | 61 (23%) | 0.22 | 60 (16%) | 25 (11%) | 0.13 |
| Pain radiation - any | 299 (80%) | 200 (77%) | 0.33 | 293 (78%) | 175 (78%) | 0.95 |
| Any Neurological Deficit | 204 (55%) | 145 (56%) | 0.89 | 203 (54%) | 124 (55%) | 0.86 |
| Reflexes - Asymmetric Depressed | 101 (27%) | 67 (26%) | 0.76 | 90 (24%) | 60 (27%) | 0.51 |
| Sensory - Asymmetric Decrease | 95 (25%) | 87 (33%) | 0.039 | 105 (28%) | 64 (28%) | 0.97 |
| Motor - Asymmetric Weakness | 113 (30%) | 64 (25%) | 0.13 | 91 (24%) | 55 (24%) | 0.98 |
| Listhesis Level | 0.27 | |||||
| L3-L4 | 0 (0%) | 0 (0%) | 40 (11%) | 17 (8%) | ||
| L4-L5 | 0 (0%) | 0 (0%) | 336 (89%) | 208 (92%) | ||
| Stenosis Levels | ||||||
| L2-L3 | 101 (27%) | 78 (30%) | 0.49 | 31 (8%) | 22 (10%) | 0.62 |
| L3-L4 | 250 (67%) | 170 (65%) | 0.68 | 144 (38%) | 92 (41%) | 0.59 |
| L4-L5 | 340 (91%) | 239 (92%) | 0.97 | 363 (97%) | 217 (96%) | 0.87 |
| L5-S1 | 101 (27%) | 72 (28%) | 0.96 | 40 (11%) | 17 (8%) | 0.27 |
| Number of Moderate/Severe Stenotic Levels | 0.36 | 0.006 | ||||
| None | 8 (2%) | 7 (3%) | 8 (2%) | 15 (7%) | ||
| One | 141 (38%) | 93 (36%) | 238 (63%) | 132 (59%) | ||
| Two | 148 (40%) | 93 (36%) | 102 (27%) | 70 (31%) | ||
| Three+ | 76 (20%) | 68 (26%) | 28 (7%) | 8 (4%) | ||
| Stenosis Locations | ||||||
| Central | 316 (85%) | 227 (87%) | 0.50 | 351 (93%) | 198 (88%) | 0.035 |
| Lateral Recess | 293 (79%) | 210 (80%) | 0.63 | 348 (93%) | 198 (88%) | 0.084 |
| Neuroforamen | 120 (32%) | 87 (33%) | 0.83 | 149 (40%) | 94 (42%) | 0.66 |
| Stenosis Severity | 0.62 | 0.009 | ||||
| Mild | 8 (2%) | 7 (3%) | 8 (2%) | 15 (7%) | ||
| Moderate | 161 (43%) | 121 (46%) | 130 (35%) | 85 (38%) | ||
| Severe | 204 (55%) | 133 (51%) | 238 (63%) | 125 (56%) | ||
| Instability | 0 (0%) | 0 (0%) | 28 (7%) | 19 (8%) | 0.78 | |
| Received surgery* | 250 (67%) | 163 (62%) | 0.27 | 235 (62%) | 156 (69%) | 0.11 |
Race or ethnic group was self-assessed. Whites and blacks could be either Hispanic or non-Hispanic.
This category includes patients who were receiving or had applications pending for workers compensation, Social Security compensation, or other compensation.
The body-mass index is the weight in kilograms divided by the square of the height in meters.
Other indicates problems related to stroke, cancer, lung, fibromyalgia, chronic fatigue syndrome, post traumatic stress disorder, alcohol, drug dependency, liver, kidney, blood vessel, nervous system, migraine, anxiety.
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms.
The Sciatica Bothersomeness index range from 0 to 24, with lower scores indicating less severe symptoms.
The Low Back Pain Bothersomness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms
Patients received surgery were classified according to whether they received surgical treatment during the first 4 years of enrollment.
Operative details of the spinal stenosis patients are presented in Table 2. Obese patients were more likely to have the L2-3 level included in the decompression compared to the nonobese patients (43% versus 32%, p=0.029). There were no significant differences in operation time, blood loss, and length of hospital stay between the groups. There were no significant differences between the groups in the incidence of nerve root injury, wound hematoma, wound infection, perioperative mortality, recurrence, or need for additional surgeries.
Table 2.
Operative treatments, complications and events.
| Characteristics | Spinal Stenosis | Degenerative Spondylolisthesis | ||||
|---|---|---|---|---|---|---|
| Normal or overweight (BMI<30) | Obese (BMI³30) | p-value | Normal or overweight (BMI<30) | Obese (BMI³30) | p-value | |
| (n=249) | (n=162) | (n=233) | (n=156) | |||
| Specific procedures† | 0.73 | 0.044 | ||||
| Decompression only | 15 (87%) | 141 (90%) | 20 (9%) | 4 (3%) | ||
| Non-instrumented fusion | 15 (6%) | 7 (4%) | 45 (20%) | 36 (23%) | ||
| Instrumented fusion | 16 (7%) | 9 (6%) | 163 (71%) | 114 (74%) | ||
| Multi-level fusion | 10 (4%) | 6 (4%) | 0.92 | 51 (22%) | 40 (26%) | 0.46 |
| Decompression level | ||||||
| L2-L3 | 78 (32%) | 69 (43%) | 0.026 | 26 (11%) | 19 (13%) | 0.82 |
| L3-L4 | 173 (71%) | 109 (69%) | 0.70 | 119 (52%) | 70 (46%) | 0.33 |
| L4-L5 | 225 (92%) | 148 (93%) | 0.90 | 225 (97%) | 149 (97%) | 0.94 |
| L5-S1 | 96 (39%) | 57 (36%) | 0.55 | 71 (31%) | 42 (27%) | 0.53 |
| Levels decompressed | 0.69 | 0.37 | ||||
| None | 5 (2%) | 3 (2%) | - | 1 (0%) | 3 (2%) | |
| 1 | 54 (22%) | 39 (24%) | - | 91 (39%) | 68 (44%) | |
| 2 | 83 (33%) | 45 (28%) | - | 85 (36%) | 53 (34%) | |
| 3+ | 107 (43%) | 75 (46%) | - | 56 (24%) | 32 (21%) | |
| Operation time, minutes (SD) | 126.2 (66.5) | 132.8 (64.7) | 0.33 | 197.2 (78.5) | 220.2 (88.9) | 0.008 |
| Blood loss, cc (SD) | 286.3 (327.4) | 350.1 (499.1) | 0.12 | 545.4 (474.6) | 636.2 (457) | 0.062 |
| Blood Replacement | ||||||
| Intraoperative replacement | 25 (10%) | 14 (9%) | 0.75 | 70 (30%) | 62 (40%) | 0.063 |
| Post-operative transfusion | 14 (6%) | 6 (4%) | 0.52 | 52 (23%) | 29 (19%) | 0.48 |
| Length of hospital stay, days (SD) | 3.3 (2.3) | 3.1 (2.6) | 0.54 | 6 (24.3) | 5.1 (3.6) | 0.66 |
| Intraoperative complications§ | ||||||
| Dural tear/spinal fluid leak | 23 (9%) | 15 (9%) | 0.88 | 33 (14%) | 8 (5%) | 0.007 |
| Vascular injury | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0%) | 0 (0%) | 0.84 |
| Other | 3 (1%) | 0 (0%) | 0.41 | 7 (3%) | 2 (1%) | 0.45 |
| None | 221 (89%) | 147 (91%) | 0.80 | 194 (83%) | 146 (94%) | 0.004 |
| Postoperative complications/events¶ | ||||||
| Nerve root injury | 0 (0%) | 0 (0%) | (0%) | 1 (0%) | 0 (0%) | 0.84 |
| Wound dehiscence | 0 (0%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (1%) | 0.84 |
| Wound hematoma | 3 (1%) | 1 (1%) | 0.94 | 0 (0%) | 1 (1%) | 0.84 |
| Wound infection | 6 (2%) | 3 (2%) | 0.97 | 3 (1%) | 8 (5%) | 0.051 |
| Other | 17 (7%) | 7 (4%) | 0.40 | 20 (9%) | 17 (11%) | 0.53 |
| None | 209 (85%) | 145 (91%) | 0.13 | 165 (71%) | 102 (67%) | 0.38 |
| Post-operative mortality (death within 6 weeks of surgery) | 1 (0.4%) | 0 (0%) | 0.82 | 1 (0.4%) | 0 (0%) | 0.83 |
| Post-operative mortality (death within 3 months of surgery) | 1 (0.4%) | 0 (0%) | 0.82 | 1 (0.4%) | 1 (0.6%) | 0.67 |
| Additional surgeries (1-year rate) ‖ | 15 (6%) | 7 (4%) | 0.486 | 10 (4%) | 15 (10%) | 0.029 |
| Additional surgeries (2-year rate) ‖ | 20 (8%) | 12 (7%) | 0.845 | 23 (10%) | 25 (16%) | 0.054 |
| Additional surgeries (3-year rate) ‖ | 30 (12%) | 16 (10%) | 0.535 | 24 (10%) | 30 (19%) | 0.01 |
| Additional surgeries (4-year rate) ‖ | 35 (14%) | 19 (12%) | 0.541 | 27 (11%) | 32 (20%) | 0.013 |
| Recurrent stenosis/progressive listhesis | 14 (6%) | 10 (6%) | 14 (6%) | 6 (4%) | ||
| Pseudarthrosis/fusion exploration | 0 | 0 | 0 | 4 (2.6%) | ||
| Complication or Other | 11 (4.5%) | 7 (4.3%) | 9 (3.9%) | 16 (10.5%) | ||
| New condition | 4 (1.6%) | 4 (2.4%) | 4 (1.7%) | 5 (3.3%) | ||
Surgical information was available for 82 normal, 167 overweight, and 162 obese patients.
Specific procedure data was available for 81 normal, 165 overweight, and 157 obese patients.
No cases were reported of aspiration into the respiratory tract or operation at wrong level.
Complications or events occurring up to 8 weeks after surgery are listed. There were no reported cases of bone-graft complication, cerebrospinal fluid leak, paralysis, caudaequina injury or pseudarthrosis.
Rates of repeated surgery at 1, 2,3,and 4 years are Kaplan-Meier estimates. P values were calculated with the use of the log-rank test. Numbers and percentages are based on the first additional surgery if more than one additional surgery.
The change in primary outcome measures of the surgically treated spinal stenosis patients can be seen in Supplemental Digital Content Appendix Table A. At 4-years follow-up, there were no statistically significant differences between surgically treated obese and nonobese patients in all three of the primary outcome measures. Furthermore, at 4-years follow-up, there were no statistically significant differences noted between the two groups in the secondary outcome measures (Supplemental Digital Content Appendix Table C)).
Of the nonoperatively treated spinal stenosis patients, the obese patients had significantly less improvement from baseline in the ODI (-3.7 versus -12.7, p<0.001), SF36 bodily pain (8.2 versus 16.6, p=0.017), and SF36 physical function scores (5.4 versus 15.1, p=0.004) at 4-years follow-up (Supplemental Digital Content Appendix Table B). There were no significant differences between obese and nonobese patients in the SF36 mental component scores. Obese patients had significantly less improvement over baseline than the nonobese patients in low back pain bothersomeness (-0.3 versus -1.1, p=0.014) and a significantly worse self rated assessment of progress (13% versus 30.2%, p=0.017) at 4-years follow-up (Supplemental Digital Content Appendix Table D).
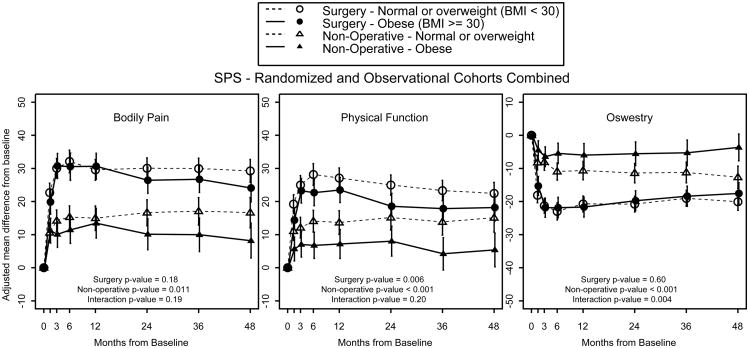
The treatment effect of surgery is the change in outcome of the surgically treated patients minus the change in outcome of the nonsurgically treated patients, i.e. the differential benefit in improvement of surgically treated patients and the nonsurgically treated patients. There was a statistically significant difference in treatment effect of surgery between obese and nonobese patients in the Oswestry Disability Index at four years (Table 3), with a greater treatment effect observed in the obese patients. This suggests that surgery has a significantly greater benefit over nonsurgical treatment in obese patients, largely due to the relatively poor outcome observed with nonsurgical treatment in obese patients (Figure 1). However, the treatment effects were not significantly different for the other primary and secondary outcome measures between obese and nonobese patients (Table 3 and Table 4).
Table 3. Treatment Effect of Surgery By Primary Outcome Measures of Spinal Stenosis and Degenerative Spondylolisthesis Patients According to Body Mass Index*.
| Outcome | Obesity (2 groups) | 1 Year | 2 Years | 3 Years | 4 Years |
|---|---|---|---|---|---|
|
| |||||
| SPS (RCT & OBS) | Treatment Effect (95% CI) | Treatment Effect (95% CI) | Treatment Effect (95% CI) | Treatment Effect (95% CI) | |
|
| |||||
| SF-36 Bodily Pain (BP) (0-100) (SE)†† | Normal or overweight (BMI < 30) | 14.6 (10.1,19.1) | 13.4 (8.7,18.1) | 12.9 (7.9,17.8) | 12.6 (7.2,18.1) |
| Obese (BMI ≥ 30) | 17.2 (11.6,22.8) | 16.3 (10.5,22.1) | 16.7 (10.6,22.9) | 15.9 (9.4,22.4) | |
|
| |||||
| pvalue | 0.47 | 0.44 | 0.32 | 0.44 | |
|
| |||||
| SF-36 Physical Function(PF) (0-100) (SE)†† | Normal or overweight | 13.5 (9.3,17.6) | 9.8 (5.5,14.2) | 9.5 (4.9,14.1) | 7.4 (2.3,12.4) |
| Obese | 16.3 (11,21.6) | 10.6 (5.1,16) | 13.6 (7.8,19.4) | 12.8 (6.7,18.9) | |
|
| |||||
| pvalue | 0.40 | 0.84 | 0.26 | 0.17 | |
|
| |||||
| Oswestry Disability Index (ODI) (0-100) (SE)‡‡ | Normal or overweight | -10.1 (-13.4,-6.8) | -9.3 (-12.8,-5.9) | -7.8 (-11.5,-4.1) | -7.4 (-11.4,-3.3) |
| Obese | -15.7 (-19.9,-11.5) | -14.2 (-18.5,-9.9) | -13.1 (-17.7,-8.5) | -13.9 (-18.8,-9) | |
|
| |||||
| pvalue | 0.036 | 0.076 | 0.07 | 0.037 | |
|
| |||||
| DS (RCT & OBS) | |||||
|
| |||||
| SF-36 Bodily Pain (BP) (0-100) (SE)†† | Normal or overweight (BMI < 30) | 16.7 (12.4,21) | 17.6 (13,22.1) | 15.6 (10.8,20.4) | 13.8 (8.7,19) |
| Obese (BMI ≥ 30) | 20.7 (15,26.4) | 20 (14,26.1) | 19.6 (13,26.1) | 17.2 (10.4,24) | |
|
| |||||
| pvalue | 0.26 | 0.51 | 0.32 | 0.43 | |
|
| |||||
| SF-36 Physical Function(PF) (0-100) (SE)†† | Normal or overweight | 16 (11.9,20.1) | 15.9 (11.6,20.2) | 14.4 (9.9,19) | 14 (9,18.9) |
| Obese | 20.7 (15.3,26.1) | 17.9 (12.2,23.6) | 19.9 (13.6,26.1) | 25.6 (19.1,32.1) | |
|
| |||||
| pvalue | 0.17 | 0.58 | 0.16 | 0.004 | |
|
| |||||
| Oswestry Disability Index (ODI) (0-100) (SE)‡‡ | Normal or overweight | -15.4 (-18.5,-12.2) | -14.5 (-17.8,-11.1) | -11.7 (-15.3,-8.2) | -12.6 (-16.4,-8.8) |
| Obese | -19.6 (-23.8,-15.4) | -18.4 (-22.8,-14) | -14.4 (-19.2,-9.6) | -17.5 (-22.5,-12.5) | |
|
| |||||
| pvalue | 0.11 | 0.15 | 0.37 | 0.12 | |
Adjusted for age, gender, race, smoking status, compensation, joint, stomach, bowel, osteoporosis, number of moderate/severe stenotic levels, self-assessed health trend at baseline, treatment preference, baseline stenosis bothersomeness, other ** comorbiditiy, baseline score and center.
Treatment effect is the difference between the surgical and non-operative mean change from baseline. Analysis is done using a mixed model with a random subject intercept term. Treatment is a time-varying covariate where a patients' experience prior to surgery is attributed to the non-operative arm and time is measured from enrollment and his/her post-surgery outcomes are attributed to the surgical arm and time is measured from time of surgery.
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
The Oswestry Disability Index ranges from 0 to 100, with lower scores indicating less severe symptoms.
Other comorbidities include: stroke, cancer, fibromyalgia, chronic fatigue syndrome, post traumatic stress disorder, alcohol, drug dependency, lung, liver, kidney, blood vessel, nervous system, migraine, anxiety.
Figure 1.
Comparison of primary outcome measures for patients with stenosis treated surgically versus nonoperatively at baseline and at follow-up time periods out to 4-years.
Table 4. Treatment Effect of Surgery By Secondary Outcome Measures of Spinal Stenosis and Degenerative Spondylolisthesis Patients According to Body Mass Index*.
| Outcome | Obesity (2 groups) | 1 Year | 2 Years | 3 Years | 4 Years |
|---|---|---|---|---|---|
|
| |||||
| SPS (RCT & OBS) | Treatment Effect (95% CI) | Treatment Effect (95% CI) | Treatment Effect (95% CI) | Treatment Effect (95% CI) | |
|
| |||||
| Stenosis Bothersomeness Index (0-24) (SE)§§ | Normal or overweight (BMI < 30) | -4.4 (-5.6,-3.2) | -3 (-4.3,-1.8) | -3.5 (-4.9,-2.2) | -3.5 (-5,-2) |
| Obese (BMI ≥ 30) | -5.3 (-6.8,-3.7) | -5.3 (-6.9,-3.7) | -3.3 (-5,-1.6) | -4 (-5.8,-2.2) | |
|
| |||||
| pvalue | 0.36 | 0.021 | 0.83 | 0.67 | |
|
| |||||
| Low Back Pain Bothersomeness (0-6) (SE)¶¶ | Normal or overweight | -1.3 (-1.7,-0.9) | -1.3 (-1.7,-0.9) | -1.3 (-1.7,-0.9) | -1 (-1.5,-0.5) |
| Obese | -1.8 (-2.3,-1.3) | -1.6 (-2.1,-1.1) | -1.3 (-1.9,-0.7) | -1.4 (-2,-0.8) | |
|
| |||||
| pvalue | 0.15 | 0.33 | 0.98 | 0.26 | |
|
| |||||
| Very/somewhat satisfied with symptoms (%) | Normal or overweight | 34.5 (24.3,44.8) | 36.7 (26.1,47.4) | 29.8 (18.2,41.5) | 33.6 (21,46.1) |
| Obese | 50.7 (39.5,61.9) | 51 (39.3,62.7) | 33 (19,47) | 31.2 (16.4,46) | |
|
| |||||
| pvalue | 0.044 | 0.08 | 0.73 | 0.85 | |
|
| |||||
| Self-rated progress: major improvement (%) | Normal or overweight | 37.9 (28,47.7) | 29.3 (18.6,40) | 28.6 (17.2,39.9) | 26.7 (14.3,39) |
| Obese | 53.3 (42.5,64) | 49 (37.5,60.5) | 42 (29.7,54.4) | 36.2 (23.9,48.5) | |
|
| |||||
| pvalue | 0.042 | 0.02 | 0.11 | 0.15 | |
|
| |||||
| Mental Component Summary (MCS)(0-100) (SE) †† | Normal or overweight | 1.5 (-0.4,3.4) | 1.4 (-0.6,3.3) | 0.9 (-1.2,3) | 1.9 (-0.5,4.2) |
| Obese | 0.6 (-1.8,2.9) | 3.9 (1.5,6.4) | 3.4 (0.8,6) | 3.1 (0.3,5.9) | |
|
| |||||
| pvalue | 0.53 | 0.099 | 0.13 | 0.49 | |
|
| |||||
| DS (RCT & OBS) | |||||
|
| |||||
| Stenosis Bothersomeness Index (0-24) (SE)§§ | Normal or overweight (BMI < 30) | -5.2 (-6.4,-4) | -5.1 (-6.3,-3.8) | -4.7 (-6,-3.3) | -5.1 (-6.5,-3.6) |
| Obese (BMI ≥ 30) | -6.6 (-8.1,-5) | -5.6 (-7.2,-3.9) | -5.5 (-7.3,-3.6) | -6.6 (-8.5,-4.8) | |
|
| |||||
| pvalue | 0.16 | 0.63 | 0.48 | 0.18 | |
|
| |||||
| Low Back Pain Bothersomeness (0-6) (SE)¶¶ | Normal or overweight | -1.2 (-1.6,-0.8) | -0.8 (-1.2,-0.4) | -0.7 (-1.1,-0.3) | -0.9 (-1.4,-0.4) |
| Obese | -1.5 (-2,-1) | -1.2 (-1.7,-0.7) | -0.8 (-1.4,-0.2) | -1.3 (-1.9,-0.7) | |
|
| |||||
| pvalue | 0.35 | 0.28 | 0.69 | 0.31 | |
|
| |||||
| Very/somewhat satisfied with symptoms (%) | Normal or overweight | 42.7 (33.3,52.2) | 39.4 (29.3,49.5) | 26.5 (15.1,37.9) | 30.3 (18.3,42.4) |
| Obese | 50.8 (39.5,62.1) | 31.5 (17.3,45.7) | 36.1 (21.2,50.9) | 43 (28.5,57.5) | |
|
| |||||
| pvalue | 0.26 | 0.38 | 0.34 | 0.24 | |
|
| |||||
| Self-rated progress: major improvement (%) | Normal or overweight | 44.4 (35,53.8) | 47.9 (38.3,57.6) | 48.4 (38.3,58.4) | 43.7 (32.6,54.7) |
| Obese | 59.4 (48.4,70.3) | 52.4 (40.2,64.6) | 40.3 (25.6,54.9) | 49.7 (35.6,63.8) | |
|
| |||||
| pvalue | 0.071 | 0.58 | 0.46 | 0.56 | |
|
| |||||
| Mental Component Summary (MCS)(0-100) (SE) †† | Normal or overweight | 0.3 (-1.5,2.2) | 1.2 (-0.7,3.2) | 1.8 (-0.2,3.9) | 2.7 (0.5,5) |
| Obese | 3.5 (1.1,5.9) | 2.5 (0,5.1) | 3.7 (0.9,6.5) | 1.6 (-1.4,4.6) | |
|
| |||||
| pvalue | 0.038 | 0.41 | 0.29 | 0.56 | |
Adjusted for age, gender, race, smoking status, compensation, joint, stomach, bowel, osteoporosis, number of moderate/severe stenotic levels, self-assessed health trend at baseline, treatment preference, baseline stenosis bothersomeness, other ** comorbiditiy, baseline score and center.
Treatment effect is the difference between the surgical and non-operative mean change from baseline. Analysis is done using a mixed model with a random subject intercept term. Treatment is a time-varying covariate where a patients' experience prior to surgery is attributed to the non-operative arm and time is measured from enrollment and his/her post-surgery outcomes are attributed to the surgical arm and time is measured from time of surgery.
The Sciatica Bothersomeness index ranges from 0 to 24, with lower scores indicating less severe symptoms.
The Low Back Pain Bothersomeness Scale ranges from 0 to 6, with lower scores indicating less severe symptoms
The SF-36 scores range from 0 to 100, with higher score indicating less severe symptoms.
Other comorbidities include: stroke, cancer, fibromyalgia, chronic fatigue syndrome, post traumatic stress disorder, alcohol, drug dependency, lung, liver, kidney, blood vessel, nervous system, migraine, anxiety.
Degenerative Spondylolisthesis
In the DS study, there were 376 patients with a BMI of <30 (“nonobese”) and 225 patients with a BMI of ≥ 30 (“obese”). Differences between the groups at baseline are noted in Table 1. Significant baseline differences between the DS patient subgroups were present in the mean age, gender, race, education, income, marital status, and work status. The mean BMI in the nonobese and obese groups for the degenerative spondylolisthesis cohort was 25.5 ± 2.9 and 35.3 ± 5.4, respectively (p<0.001). The obese patients group had a higher incidence of medical comorbidities, including hypertension, diabetes, depression, stomach problem, and other comorbidities. Baseline SF36 scores, ODI scores, back pain bothersomeness index, and self-perceived health trend were significantly worse in the obese patient group. There was a significant difference in the number of stenotic levels. There was a higher incidence of central stenosis. There was a lower incidence of severe stenosis in the obese group compared to the nonobese patient group.
Operative details of the DS patient group are described in Table 2. A higher proportion of obese patients underwent instrumented fusion and a lower percentage underwent decompression alone. Operative time was significantly higher in the obese patient group (mean 220.2 minutes versus 197.2 minutes, p=0.008). The incidence of intraoperative complications was significantly lower in the obese patient group; in particular the incidence of dural tear, which occurred in 5% of the obese patients and 14 % of the nonobese patients (p=0.007). There was a trend towards an increased rate of wound infection in the obese patients compared to the nonobese patients (5% versus 1%, p=0.051). There was a significantly higher rate of additional surgeries at 4-year follow-up (20% versus 11%, p=0.013) in the obese patient group compared to the nonobese patient group.
The change in primary outcome measures in the surgically treated DS patients demonstrated that obese patients had significantly less improvement from baseline compared to the nonobese patients in regards to the SF36 physical function scores (22.1 versus 27.9, 4-yr follow-up, p=0.022) (Supplemental Digital Content Appendix Table A). The other primary outcome measures did not display significant differences between the obese and nonobese patients (Supplemental Digital Content Appendix Table A). There were no significant differences in the secondary outcome measures between the obese and nonobese patients who were treated surgically for DS, with the exception of a significantly less improvement over baseline in obese patients compared to nonobese patients (-6.8 vs. -8.1, p value=0.04) in the stenosis bothersomeness index at the 3-year follow-up time point (Supplemental Digital Content Appendix Table C).
Obese nonsurgically treated DS patients demonstrated significantly worse in SF36 physical function and ODI scores compared to nonobese patients (Supplemental Digital Content Appendix Table B). At 4-years follow-up, obese patients treated nonoperatively had SF-36 physical function scores that worsened from baseline by a mean of mean 3.5. This is in comparison to a mean improvement of 13.9 points in the SF36 physical function score over baseline in nonoperatively treated nonobese patients at same follow-up time period (p<0.001). Obese nonsurgically treated patients also had significantly less improvement from baseline in the stenosis bothersomeness index compared to nonobese patients at 4-years follow-up (-8.2 versus -9.7, p=0.039) (Supplemental Digital Content Appendix Table D).
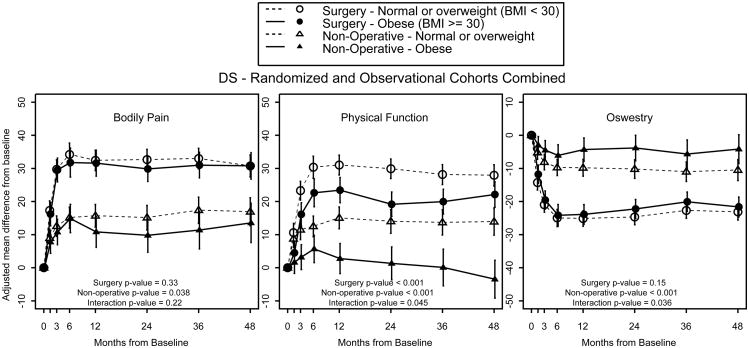
The treatment effect for the SF36 Physical Function score was significantly higher for the obese group at 4-years follow-up (25.6 versus 14.0, p=0.004, Table 3). This suggests that surgery has a significantly greater benefit over nonsurgical treatment of degenerative spondylolisthesis in obese patients, largely due to the relatively poor outcome observed with nonsurgical treatment in obese patients (Figure 2). There was no significant difference in the treatment effects for other primary outcome measures or secondary outcome measures between obese and nonobese patients (Table 3 and Table 4).
Figure 2.
Comparison of primary outcome measures for patients with degenerative spondylolisthesis treated surgically versus nonoperatively at baseline and at follow-up time periods out to 4-years.
Discussion
In the original SPORT publications dealing with spinal stenosis and degenerative spondylolisthesis, an as-treated analysis combining the randomized and observational cohorts demonstrated that the clinically relevant advantages of surgery that had been previously reported through two years were maintained at four years [28]. This finding is also supported by findings of the Maine Lumbar Spine Study, in which 8- to 10-year follow-up favored those patients initially receiving surgical treatment [29]. Amundsen, Weber et al., in another long-term follow-up study comparing surgical and conservative treatment of lumbar spinal stenosis, found favorable outcomes in those treated surgically [30]. Despite similar findings favoring surgery in these long-term prospective studies, they did not take into account the effects of obesity on outcomes.
The results of the current study support the hypothesis that obesity is associated with worse outcome after nonoperative treatment of both lumbar spinal stenosis and degenerative spondylolisthesis. However, obesity does not seem to be associated with worse outcome after surgical treatment of these conditions, with the exception of an increased reoperation rate and a lower SF-36 Physical Function score in the obese patients with degenerative spondylolisthesis. There were no differences noted at 4-years follow-up between obese and nonobese patients treated surgically for lumbar stenosis.
There was noted, in the current, study to be significant differences in treatment effect between obese and nonobese patients. This was true for the ODI treatment effect in the SpS cohort and the SF-36 Physical function treatment effect in the DS cohort, with obese patients demonstrating a significantly greater treatment effect than the nonobese patients. This significant difference in treatment effect in both instances is largely the result not of overwhelming improvement in surgical outcomes in obese patients, but rather an overwhelming lack of improvement or even a worsening of outcomes following nonoperative treatment in the obese patients. The lack of efficacy of nonoperative treatment in obese patients is an important finding, and explanation of which is not readily apparent. There is a relative lack of evidence regarding the affect of obesity on nonoperative interventions for lumbar degenerative conditions. It is possible that current nonoperative interventions are not as effective in obese patient and that alternative nonoperative treatments should be developed and further investigated for this patient population. It also suggests that currently, surgery may be a better option than the available nonsurgical options in obese patients.
Previous studies have found no influence of obesity on clinical outcome. In a prospective study of mixed lumbar diagnoses, Andreshak et al. found no significant differences between obese and control patients relative to blood loss, operative time, length of hospital stay, rate of complications, and functional outcome [25]. Gepstein et al. similarly showed similar reduction in pain, improvement of daily activities and overall satisfaction in obese and non-obese elderly patients undergoing lumbar spine surgery [31]. Djurasovic et al., in a retrospective analysis of obese and non-obese patients undergoing lumbar fusion, found no significant difference in back pain, leg pain, SF-36, or ODI scores at two-year follow up [26]. In a prospective review of patients undergoing anterior lumbar disc procedures, Peng et al. showed no significant difference in complication rates in obese patients, but did find longer duration of anterior exposure, duration of entire surgery, and longer incision. Obesity did not affect blood loss, analgesic use, length of time to ambulation, or length of hospitalization [32]. In obese and non-obese patients undergoing minimally invasive lumbar fusion, Rosen et al showed no significant difference with most self-reported outcome measures, operative time, length of hospital stay, or complications [33]. In regard to patients being treated surgically for spinal stenosis, our report supports the finding that obese patients have similar complication rates, reoperation rates, and clinical outcomes compared to nonobese patients. Obese patients with degenerative spondylolisthesis, on the other hand, were found to have an increased wound infection rate and twice the reoperation rate at 4-years follow-up. With the exception of having a lower SF-36 Physical function score, however, obese patients with DS who were treated surgically did similar to the nonobese patients at 4-years follow-up. Interestingly, obese patients with DS treated surgically had a lower intraoperative complication rate than nonobese patients, including a significantly lower dural tear rate.
There are several limitations to this subgroup analysis. The original SPORT study was designed and powered to compare the outcome of surgically and nonsurgically treated patients. There are confounding variables that are not equally distributed between treatment groups in this “as treated” analysis. For instance, there are significant differences in the demographic characteristics, outcome scores, and preference for surgery between obese and nonobese patients in both groups. Additionally, the SPORT was not specifically powered to include analysis of specific patient subgroups. However, the SPORT represents the largest study to date on SpS and DS patients and is the most likely to be powered to address questions posed in subgroup analysis.
Supplementary Material
Key Points.
Regardless of body mass index, patients treated surgically had improved outcomes at all time points relative to those treated nonoperatively
Obese patients undergoing surgery for degenerative spondylolisthesis have an increased wound infection rate and have two times the reoperation rate than nonobese patients at 4-years follow-up.
Body mass index does not have an effect on clinical outcome following the surgery treatment of lumbar stenosis.
Obese patients treated nonoperatively had worse clinical outcomes than nonobese patients treated nonoperatively for both the lumbar stenosis and degenerative spondylolisthesis cohorts.
Acknowledgments
The authors would like to acknowledge funding from the following sources: The National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444) and the Office of Research on Women's Health, the National Institutes of Health, and the National Institute of Occupational Safety and Health, the Centers for Disease Control and Prevention. The Multidisciplinary Clinical Research Center in Musculoskeletal Diseases is funded by NIAMS (P60-AR048094).
The manuscript submitted does not contain information about medical device(s)/drug(s). National Institute of Arthritis and Musculoskeletal and Skin Diseases (U01-AR45444) and the Office of Research on Women's Health; the National Institutes of Health, and the National Institute of Occupational Safety and Health; the Centers for Disease Control and Prevention; and the Multidisciplinary Clinical Research Center in Musculoskeletal Diseases (supported by the NIAMS [P60-AR048094]) funds were received to support this work. One or more of the author(s) has/have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this manuscript: e.g., honoraria, gifts, consultancies, royalties, stocks, stock options, decision making position.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.National Health and Nutrition Examination Survey (NHANES) Prevalence of overweight, obesity and extreme obesity among adults: United States, trends 1960-62 through 2005-2006. http://www.cdc.gov/nchs/data/hestat/overweight/overweight_adult.htm.
- 2.Pi-Sunyer X. The Medical Risks of Obesity. Postgrad Med. 2009 Nov;121(6):21–33. doi: 10.3810/pgm.2009.11.2074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marcus DA. Obesity and the impact of chronic pain. Clin J Pain. 2004 May-Jun;20(3):186–91. doi: 10.1097/00002508-200405000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Leboeuf-Yde C, Kyvik KO, Bruun NH. Low back pain and lifestyle. Part II--Obesity. Information from a population-based sample of 29,424 twin subjects. Spine (Phila Pa 1976) 1999 Apr 15;24(8):779–83. doi: 10.1097/00007632-199904150-00009. discussion 783-4. [DOI] [PubMed] [Google Scholar]
- 5.Webb R, Brammah T, Lunt M, Urwin M, Allison T, Symmons D. Prevalence and predictors of intense, chronic, and disabling neck and back pain in the UK general population. Spine (Phila Pa 1976) 2003 Jun 1;28(11):1195–202. doi: 10.1097/01.BRS.0000067430.49169.01. [DOI] [PubMed] [Google Scholar]
- 6.Liuke M, Solovieva S, Lamminen A, Luoma K, Leino-Arjas P, Luukkonen R, Riihimäki H. Disc degeneration of the lumbar spine in relation to overweight. Int J Obes (Lond) 2005 Aug;29(8):903–8. doi: 10.1038/sj.ijo.0802974. [DOI] [PubMed] [Google Scholar]
- 7.Flamme CH. Obesity and low back pain--biology, biomechanics and epidemiology. Orthopade. 2005 Jul;34(7):652–7. doi: 10.1007/s00132-005-0817-6. [DOI] [PubMed] [Google Scholar]
- 8.Rodacki AL, Fowler NE, Provensi CL, Rodacki Cde L, Dezan VH. Body mass as a factor in stature change. Clin Biomech (Bristol, Avon) 2005 Oct;20(8):799–805. doi: 10.1016/j.clinbiomech.2005.04.005. [DOI] [PubMed] [Google Scholar]
- 9.Solovieva S, Lohiniva J, Leino-Arjas P, Raininko R, Luoma K, Ala-Kokko L, Riihimäki H. COL9A3 gene polymorphism and obesity in intervertebral disc degeneration of the lumbar spine: evidence of gene-environment interaction. Spine (Phila Pa 1976) 2002 Dec 1;27(23):2691–6. doi: 10.1097/00007632-200212010-00008. [DOI] [PubMed] [Google Scholar]
- 10.Kauppila LI, McAlindon T, Evans S, Wilson PW, Kiel D, Felson DT. Disc degeneration/back pain and calcification of the abdominal aorta. A 25-year follow-up study in Framingham. Spine (Phila Pa 1976) 1997 Jul 15;22(14):1642–7. doi: 10.1097/00007632-199707150-00023. discussion 1648-9. [DOI] [PubMed] [Google Scholar]
- 11.Patel N, Bagan B, Vadera S, Maltenfort MG, Deutsch H, Vaccaro AR, Harrop J, Sharan A, Ratliff JK. Obesity and spine surgery: relation to perioperative complications. J Neurosurg Spine. 2007 Apr;6(4):291–7. doi: 10.3171/spi.2007.6.4.1. [DOI] [PubMed] [Google Scholar]
- 12.Shamji MF, Parker S, Cook C, Pietrobon R, Brown C, Isaacs RE. Impact of body habitus on perioperative morbidity associated with fusion of the thoracolumbar and lumbar spine. Neurosurgery. 2009 Sep;65(3):490–8. doi: 10.1227/01.NEU.0000350863.69524.8E. discussion 498. [DOI] [PubMed] [Google Scholar]
- 13.Weinstein JN, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. JAMA. 2006;296(20):2451–9. doi: 10.1001/jama.296.20.2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weinstein JN, et al. Surgical versus nonoperative treatment for lumbar disc herniation: four-year results for the Spine Patient Outcomes Research Trial (SPORT) Spine (Phila Pa 1976) 2008;33(25):2789–800. doi: 10.1097/BRS.0b013e31818ed8f4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lurie JD, et al. Lumbar discectomy outcomes vary by herniation level in the Spine Patient Outcomes Research Trial. J Bone Joint Surg Am. 2008;90(9):1811–9. doi: 10.2106/JBJS.G.00913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ware JE, Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30(6):473–83. [PubMed] [Google Scholar]
- 17.Daltroy LH, et al. The North American spine society lumbar spine outcome assessment Instrument: reliability and validity tests. Spine (Phila Pa 1976) 1996;21(6):741–9. doi: 10.1097/00007632-199603150-00017. [DOI] [PubMed] [Google Scholar]
- 18.Deyo RA, Tsui-Wu YJ. Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine (Phila Pa 1976) 1987;12(3):264–8. doi: 10.1097/00007632-198704000-00013. [DOI] [PubMed] [Google Scholar]
- 19.Atlas SJ, et al. The Maine Lumbar Spine Study, Part II. 1-year outcomes of surgical and nonsurgical management of sciatica. Spine (Phila Pa 1976) 1996;21(15):1777–86. doi: 10.1097/00007632-199608010-00011. [DOI] [PubMed] [Google Scholar]
- 20.Atlas SJ, et al. The Maine Lumbar Spine Study, Part III. 1-year outcomes of surgical and nonsurgical management of lumbar spinal stenosis. Spine (Phila Pa 1976) 1996;21(15):1787–94. doi: 10.1097/00007632-199608010-00012. discussion 1794-5. [DOI] [PubMed] [Google Scholar]
- 21.Patrick DL, et al. Assessing health-related quality of life in patients with sciatica. Spine (Phila Pa 1976) 1995;20(17):1899–908. doi: 10.1097/00007632-199509000-00011. discussion 1909. [DOI] [PubMed] [Google Scholar]
- 22.Tomasino A, Parikh K, Steinberger J, Knopman J, Boockvar J, Härtl R. Tubular microsurgery for lumbar discectomies and laminectomies in obese patients: operative results and outcome. Spine (Phila Pa 1976) 2009 Aug 15;34(18):E664–72. doi: 10.1097/BRS.0b013e3181b0b63d. [DOI] [PubMed] [Google Scholar]
- 23.Mayer T, Aceska A, Gatchel RJ. Is obesity overrated as a “risk factor” for poor outcomes in chronic occupational spinal disorders? Spine (Phila Pa 1976) 2006 Dec 1;31(25):2967–72. doi: 10.1097/01.brs.0000248432.84423.65. [DOI] [PubMed] [Google Scholar]
- 24.Vaidya R, Carp J, Bartol S, Ouellette N, Lee S, Sethi A. Lumbar spine fusion in obese and morbidly obese patients. Spine (Phila Pa 1976) 2009 Mar 1;34(5):495–500. doi: 10.1097/BRS.0b013e318198c5f2. [DOI] [PubMed] [Google Scholar]
- 25.Andreshak TG, An HS, Hall J, Stein B. Lumbar spine surgery in the obese patient. J Spinal Disord. 1997 Oct;10(5):376–9. [PubMed] [Google Scholar]
- 26.Djurasovic M, Bratcher KR, Glassman SD, Dimar JR, Carreon LY. The effect of obesity on clinical outcomes after lumbar fusion. Spine (Phila Pa 1976) 2008 Jul 15;33(16):1789–92. doi: 10.1097/BRS.0b013e31817b8f6f. [DOI] [PubMed] [Google Scholar]
- 27.Telfeian AE, Reiter GT, Durham SR, Marcotte P. Spine surgery in morbidly obese patients. J Neurosurg. 2002 Jul;97(1 Suppl):20–4. doi: 10.3171/spi.2002.97.1.0020. [DOI] [PubMed] [Google Scholar]
- 28.Weinstein JN, Lurie JD, Tosteson TD, Zhao W, Blood EA, Tosteson AN, Birkmeyer N, Herkowitz H, Longley M, Lenke L, Emery S, Hu SS. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009 Jun;91(6):1295–304. doi: 10.2106/JBJS.H.00913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results from the maine lumbar spine study. Spine (Phila Pa 1976) 2005 Apr 15;30(8):936–43. doi: 10.1097/01.brs.0000158953.57966.c0. [DOI] [PubMed] [Google Scholar]
- 30.Amundsen T, Weber H, Nordal HJ, Magnaes B, Abdelnoor M, Lilleâs F. Lumbar spinal stenosis: conservative or surgical management?: A prospective 10-year study. Spine (Phila Pa 1976) 2000 Jun 1;25(11):1424–35. doi: 10.1097/00007632-200006010-00016. discussion 1435-6. [DOI] [PubMed] [Google Scholar]
- 31.Gepstein R, Shabat S, Arinzon ZH, Berner Y, Catz A, Folman Y. Does obesity affect the results of lumbar decompressive spinal surgery in the elderly? Clin Orthop Relat Res. 2004 Sep;(426):138–44. doi: 10.1097/01.blo.0000141901.23322.98. [DOI] [PubMed] [Google Scholar]
- 32.Peng CW, Bendo JA, Goldstein JA, Nalbandian MM. Perioperative outcomes of anterior lumbar surgery in obese versus non-obese patients. Spine J. 2009 Sep;9(9):715–20. doi: 10.1016/j.spinee.2009.04.023. Epub 2009 Jun 13. [DOI] [PubMed] [Google Scholar]
- 33.Rosen DS, Ferguson SD, Ogden AT, Huo D, Fessler RG. Obesity and self-reported outcome after minimally invasive lumbar spinal fusion surgery. Neurosurgery. 2008 Nov;63(5):956–60. doi: 10.1227/01.NEU.0000313626.23194.3F. discussion 960. [DOI] [PubMed] [Google Scholar]
- 34.Pull ter Gunne AF, Cohen DB. Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine (Phila Pa 1976) 2009 Jun 1;34(13):1422–8. doi: 10.1097/BRS.0b013e3181a03013. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.