Abstract
Purpose:
The purpose of this study was to compare keratometry and anterior chamber depth (ACD) measurements from the Lenstar LS 900 (Haag-Streit AG, Switzerland) and the Pentacam (Oculus, Weltzar, Germany), and compare the keratometry readings of these two systems to a manual keratometer (MK), (Haag-Streit, Switzerland).
Materials and Methods:
In this prospective study, keratometry and ACD measurements were obtained in 50 eyes of 50 normal subjects with the Lenstar and the Pentacam. Keratometry was also measured using a MK. Correlation, comparison, and interdevice agreement was evaluated using intraclass correlation analysis, Wilcoxon test, and Bland-Altman plots.
Results:
The keratometry and ACD measurements obtained from the Lenstar and the Pentacam showed excellent correlation. The mean interdevice differences in mean keratometry (Km) for the Lenstar and the Pentacam, the Lenstar and the MK, and the Pentacam and the MK were 0.39 D, 0.10 D, and 0.30 D respectively; and the 95% limits of agreement (LoA) for Km were 0.04-0.82 D; −1.90-2.10 D; and −2.30-1.70 D, respectively. The mean interdevice difference in ACD for the Lenstar versus the Pentacam was 0.09 mm, with 95% LoA of 0.23-0.05 mm.
Conclusions:
The ACD measurements obtained using the Lenstar and the Pentacam seem to be interchangeable, whereas, the keratometry measurements obtained using the Lenstar, Pentacam, and MK differ considerably, and are not interchangeable.
Keywords: Anterior Chamber, Biometry, Cornea, Interferometry, Lenstar, Optical Low-coherence Reflectometry, Pentacam Scheimpflug
INTRODUCTION
The corneal curvature and anterior chamber depth (ACD) measurements are important in aphakic and phakic intraocular lens (IOL) surgery. Furthermore, the corneal curvature measurements are crucial in refractive surgery, and contact lens fitting. ACD measurements are required for implantation of phakic IOLs. Currently, several instruments are available for measuring corneal curvature and ACD, such as; slit-scanning topography systems, Scheimpflug topography, optical coherence tomography (OCT), partial coherence interferometry (PCI), and optical low-coherence reflectometry (OLCR).
The Pentacam (Oculus, Weltzar, Germany) uses a rotating Scheimpflug camera to image the anterior segment of the eye including the lens. The system can generate elevation topography and aberration maps of the anterior and posterior corneal surfaces, pachymetry maps, and can perform chamber angle, ACD, and lens density measurements. The central corneal thickness (CCT) and ACD measurements provided by the Pentacam have been reported to have excellent repeatability.1,2
The Lenstar LS 900 (Hagg-Streit AG, Koeniz, Switzerland) is a relatively new non-contact biometry device that can measure the corneal curvature, diameter, CCT, ACD, lens thickness, axial length, and retinal thickness. The system is based on OLCR using a broad-band light source (20-30 nm), with a central wavelength of 820 μm. The repeatability of the Lenstar for keratometry, CCT, and ACD measurements is reported to be excellent.3
The purpose of this study was to compare the corneal curvature and ACD measurements from the Lenstar LS 900 and the Pentacam. We also compared the keratometry readings from these two instruments to those from a manual keratometer (MK).
MATERIALS AND METHODS
A total of 50 healthy volunteers were prospectively recruited from the staff of our hospital. Any eye with previous ocular surgery or disease was excluded. Keratometry and ACD measurements were obtained with the Lenstar, followed by the Pentacam on the same day, consecutively. The study adhered to the tenets of the Declaration of Helsinki. The Pentacam system (software version 1.12, Oculus) was used in the automatic release mode. The Lenstar and the Pentacam measurements were performed as previously reported in detail elsewhere1,3 by the same examiner (VA). The keratometry readings were then measured using a MK (Haag-Streit, Switzerland). Three consecutive measurements were performed with each device by the same examiner (VA), and the average of the measurements obtained from the right eye of each individual was used for statistical analysis.
The Pentacam uses a hypothetical refractive index of n = 1.3775, similar to conventional keratometers, and the Lenstar uses a refractive index of n = 1.3320, the Lenstar keratometry measurements were obtained by converting the measured radius into diopters using the standard 1.3375 refractive index.
Both the Lenstar and the Pentacam measure the ACD from the endothelium to the anterior lens capsule. Therefore, in this study, the ACD was defined as the distance from the endothelium to the lens.
All data were collected in an Excel database and transferred to SPSS (SPSS for Windows, version 15.0; IBM Corp., New York, USA). Interdevice correlation was evaluated by the intraclass correlation coefficient (r). Statistical significance of interdevice differences for particular parameters was evaluated with the Wilcoxon signed-rank test, and the significance was determined as P < 0.05. Finally, interdevice aggreement and interchangeability were evaluated by the method described by Bland-Altman.4 With this method, intermeasurement differences were plotted against their means and the 95% limits of agreement (LoA) were determined (95% LoA = mean interdevice difference ± 1.96 standard deviation).
RESULTS
The mean age of the patients was 29.9 ± 6.9 years (range; 19 years to 41 years). Table 1 present the average flat keratometry (Kf), steep keratometry (Ks), and mean keratometry (Km) measurements of the 50 subject eyes. There were statistically significant differences between the keratometry readings obtained with the Lenstar and the Pentacam (Wilcoxon signed-rank test, P < 0.001 for all comparisons). Keratometry measurements from the Lenstar did not differ significantly from MK values. The mean ACD was 2.99 ± 0.33 mm with the Lenstar, and 3.08 ± 0.35 mm with the Pentacam. The difference was statistically significant (Wilcoxon signed-rank test, P < 0.001).
Table 1.
The mean Kf, Ks, and Km measurements of the 50 subject eyes (displayed as mean ± standard deviation)
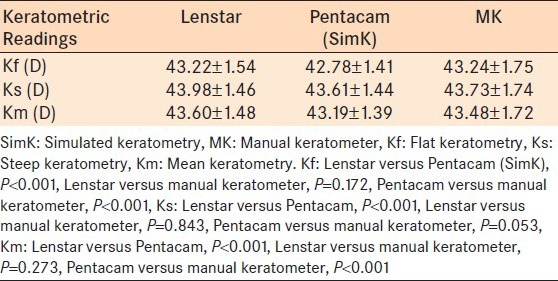
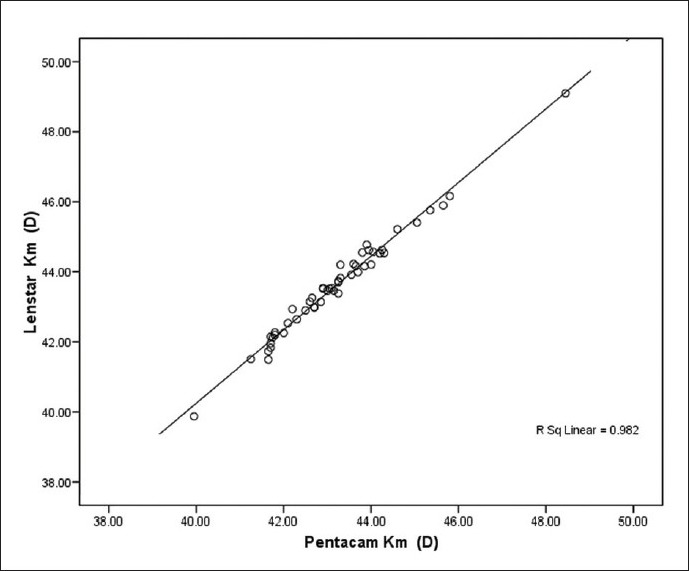
Table 2 presents the intraclass correlation coefficients for the Kf, Ks, and Km measurements. There were excellent correlations between the Lenstar and Pentacam and the Kf, Ks, and Km values [Figure 1]. The keratometry readings with the MK showed only moderate correlation to those of the Lenstar and the Pentacam [Table 1, Figures 2 and 3]. Excellent correlations were also observed between the Lenstar and the Pentacam ACD measurements (r = 0.978) [Figure 4].
Table 2.
Intraclass correlation coefficents for the keratometry measurements between each pair of the three devices (displayed as r)
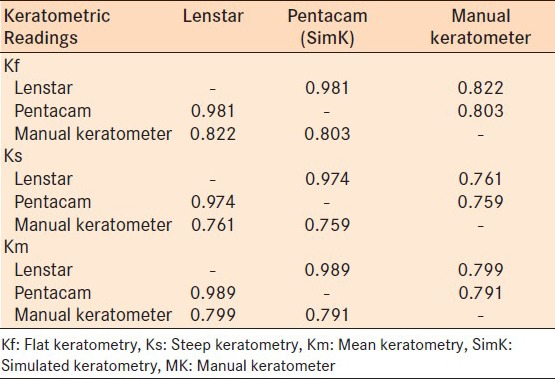
Figure 1.
Scatterplot comparing mean keratometry readings of Lenstar and Pentacam (r = 0.989)
Figure 2.
Scatterplot comparing mean keratometry readings of the Lenstar and the manual keratometer (r = 0.799)
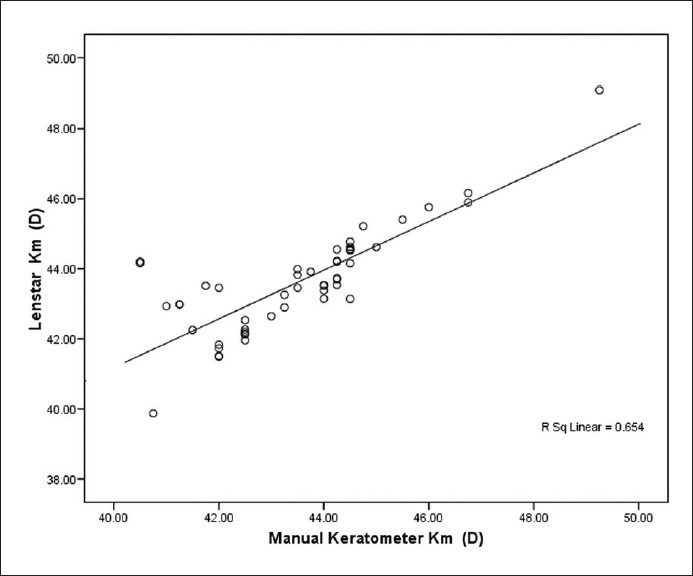
Figure 3.
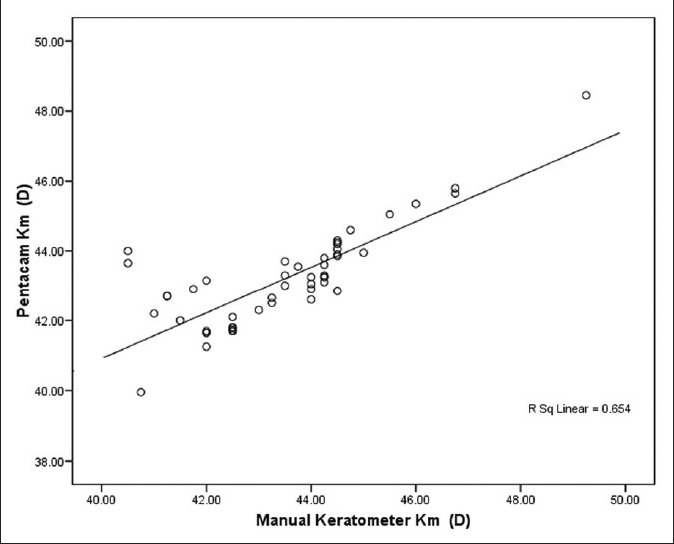
Scatterplot comparing mean keratometry readings of the Pentacam and the manual keratometer (r = 0.791)
Figure 4.
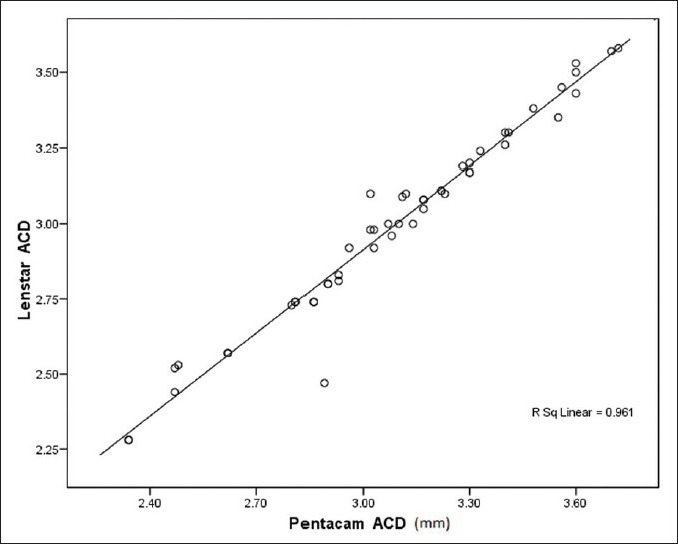
Scatterplot comparing anterior chamber depth readings of the Lenstar and the Pentacam (r = 0.978)
Figures 5-8 are Bland-Altman plots for the keratometry and ACD measurements with the three devices investigated in this study. The mean interdevice differences in Kf, Ks, and Km, and the 95% LoA for the Lenstar and the Pentacam, the Lenstar and the MK, the Pentacam and the MK, and the Lenstar and the Pentacam EquivK readings are presented in Table 3. The mean interdevice difference in ACD for Lenstar versus Pentacam was 0.09 mm, and 95% LoA were 0.23-0.05 mm.
Figure 5.
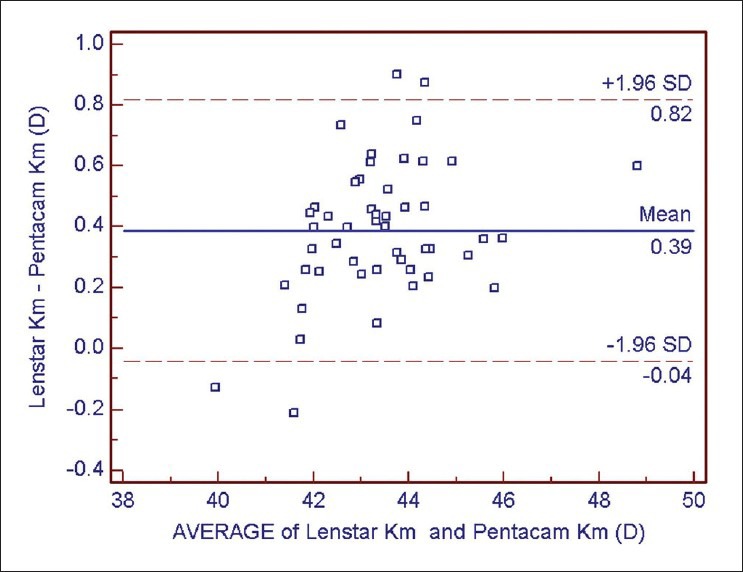
Bland-Altman plot of mean keratometry readings of the Lenstar compared to the Pentacam
Figure 8.
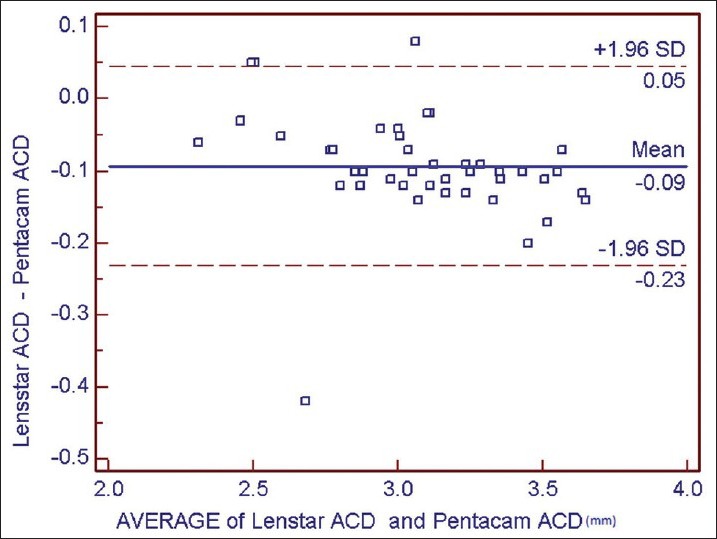
Bland-Altman plot of anterior chamber depth readings of the Lenstar compared to the Pentacam
Table 3.
The interdevice differences in Kf, Ks, and Km measurements for the three devices (displayed as 95% limits of agreement [mean interdevice difference, spans of limits of agreement])
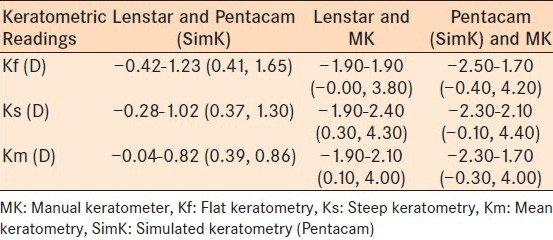
Figure 6.
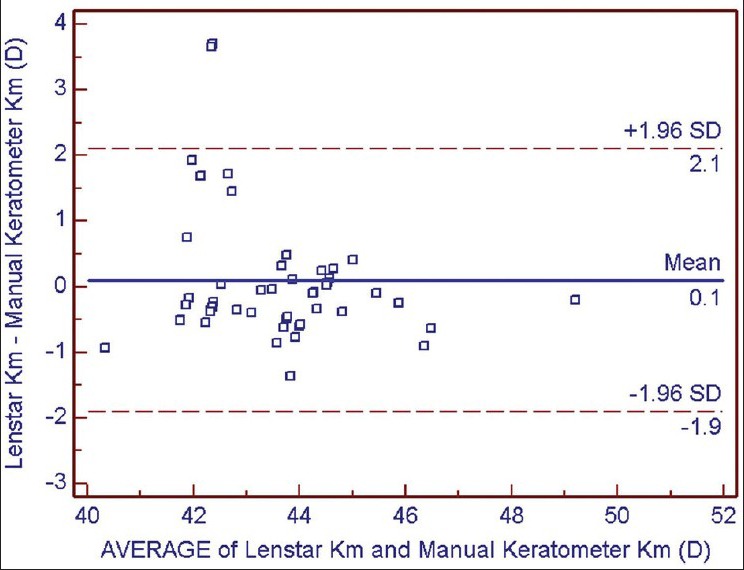
Bland-Altman plot of mean keratometry readings of the Lenstar compared to the manual keratometer
Figure 7.
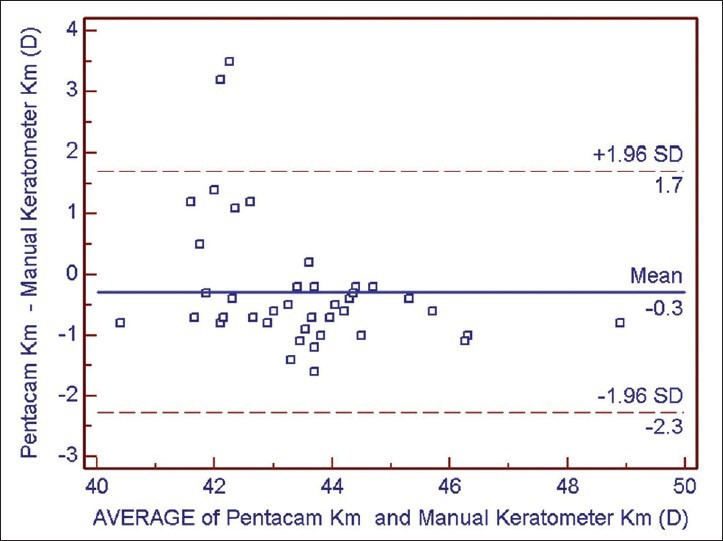
Bland-Altman plot of mean keratometry readings of the Pentacam compared to the manual keratometer
DISCUSSION
In this study, the keratometry measurements from the Lenstar were statistically significantly steeper than those from the Pentacam (P < 0.05). The Bland-Altman plots clearly demonstrated relatively large range of interdevice differences in Kf, Ks, and Km measurements. Although the difference in ACD between the Lenstar and the Pentacam was statistically significant, clinically, it was negligible, with 95% LoA and Bland-Altman plots showing a narrow range of interdevice differences. However, the differences in Kf, Ks, and Km measurements of the Lenstar and the MK were not statistically significantly different, the Bland-Altman plots showed a wide range of interdevice differences. Therefore, according to this study, the ACD measurements from the Lenstar and the Pentacam seem to be interchangeable, the keratometry measurements using the Lenstar, the Pentacam or the MK are not interchangeable for the clinical setting.
Keratometry and ACD are important biometric parameters in aphakic and refractive phakic IOL implantation. Inaccurate estimation of corneal power and ACD contribute 22% and 42% of the error in predicted refraction of an IOL using optical biometry.5 Measurement of keratometry can be performed with a variety of methods including, manual or automated keratometry, slit-scanning or scheimpflug topography, OCT, PCI, and OLCR. Among these, PCI (IOLMaster, Carl Zeiss, Germany) and OLCR (Lenstar LS 900, Hagg-Streit AG, Switzerland) systems are capable of measuring both the corneal curvature and the axial length of the eye, and therefore, provide relatively easy assessment of IOL power calculation. Very good repeatability and reproducibility of the Pentacam for keratometry6,7 and ACD2,6 measurements have been reported. Cruysberg et al.3 have reported better than 0.9% reproducibility for the keratometry and ACD for the Lenstar.
Recently, Huang et al.8 compared the keratometry, CCT and ACD measurements of the Lenstar to the Pentacam high resolution system in healthy eyes. Pentacam high resolution system is slightly different from the original system used in our study, with an optical design using a higher-resolution camera capturing a greater number of data points. Similar to our study, the authors8 reported excellent correlation between the two devices for keratometry and ACD measurements, and the Lenstar measured the Kf and Ks steeper than the Pentacam. The mean interdevice differences and the spans in LoA were 0.11 D and 0.86 D for the flat, 0.09 D and 1.08 D for the steep, and 0.10 D, and 0.86 D for the Km readings. All differences were statistically significant (P > 0.001). Similar to our study, the authors8 reported the Pentacam had deeper ACD values compared to the Lenstar. The mean interdevice difference was 0.02 mm with 95% LoA between 0.11 mm and 0.15 mm (P = 0.011). The authors8 concluded that the keratometry readings of the two devices should not be used interchangeably, whereas, the ACD measurements were interchangeable.
In this study, the Lenstar measured the flat, steep and Km readings were significantly steeper than the Pentacam (P < 0.001). The Lenstar measures 32 reflective light spots arranged in 2 rings, inner with 1.65 mm and outer with 2.30 mm diameter, whereas, with the Pentacam, the simulated keratometry (SimK) values are generated using points from around the 3 mm pupil perimeter on the sagittal curvature map. As the prolate cornea is steeper centrally compared to peripherally the finding that the Lenstar produces steeper keratometry readings may be anticipated.
To our knowledge, no previous study has compared the Lenstar keratometry readings to those of the MK. The MK assumes the cornea to be spherical, uses the refractive index of n = 1.3775, and measures the keratometry from the flattest and steepest corneal meridians along an average of a 3.0 mm diameter ring. In our study, the differences between the keratometry measurements of the Lenstar and the MK were not statistically significant (P > 0.05). However, when compared to the MK, the Pentacam measured the corneal power readings flatter along the flattest meridian as were the Km readings, and the steep keratometry readings were comparable to the MK. However, for all keratometry measurements, the spans in the LoA were very wide; 3.80 D to 4.30 D for both the Lenstar versus the MK and for the Pentacam versus the MK [Table 3]. Therefore, the keratometry measurements of neither the Lenstar, nor the Pentacam seem to be comparable to the MK. Elbaz et al.9 compared the Km readings produced by the Pentacam to those measured by an automated keratometer (ARK-700 A; Nidek Co. Ltd., Gamagori, Japan). The authors9 reported that the Pentacam produced lower Km readings with a mean interdevice difference of 0.046 D, but with spans in the LoA of 2.55 D. Similar to our study, the authors9 concluded that the interdevice variability was too high to enable these two devices to be used interchangeably in the clinical setting. Modis et al.,10 also compared the keratometry readings generated from the pentacam high resolution (HR) to those from an automated keratometer (Topcon Corp., Tokyo, Japan) and reported that the Pentacam measured both Kf, Ks and Km values flatter than the automated keratometer, with statistically significant differences. Recently, Whang et al.11 compared the Km readings produced by the Pentacam to those from a MK (Topcon Corp., Tokyo, Japan). In contrast to our and the aforementioned studies, the authors11 reported that Pentacam produced higher Km readings compared to the MK. The reason for this difference awaits further studies.
For the measurement of the ACD, ultrasound biometry or optical methods can be used. Ultrasound biometry requires placing an ultrasound probe on the central cornea. It has been speculated that this contact may also cause indentation of the cornea leading to shorter axial length measurements.12 Both the Lenstar and the IOLMaster are optical devices based mainly on the noncontact laser interferometry to assess axial ocular dimensions. For the axial length (AL) and ACD measurements, the Lenstar uses OLCR powered by a superluminescent diode (SLD).13
Previous studies compared ACD measurements of the IOLMaster to Pentacam, and reported the IOLMaster to produce significantly lower ACD readings.9,14,15 Whereas, two studies concluded that the 2 devices were not interchangeable,9,14 Reuland et al.15 suggested that the difference was small and therefore, the devices could be assumed comparable. The mean interdevice differences reported in the aforementioned studies were 0.03 mm to 0.09 mm, with spans of 95% LoA of 0.33-0.54 mm. In our study, the Lenstar measured ACD significantly shallower than Pentacam with a mean interdevice difference of 0.09 (P < 0.05). However, the Bland-Altman plots and 95% LoA indicated a narrow range of interdevice variability, and therefore, we propose that the ACD readings produced by the two systems can be used interchangeably in the clinical setting.
In conclusion, this comparative study between Lenstar and Pentacam showed excellent correlation and good agreement of the two devices for measuring the corneal curvature and ACD in healthy eyes. One limitation of our study is the small sample size, which might be the reason for the non-significant findings. However, the interdevice variability warrants caution against the use of the keratometry readings produced by the two devices interchangeably. On the Pentacam, moving the cursor at the 2 mm ring and taking the average of the measurements over the ring might have been changed the results to be comparable to that of the Lenstar; however, this observation awaits further study. Our study confirms that the ACD measurements from the two instruments can be used interchangeably. Similarly, keratometry readings generated by the MK are not interchangeable with those obtained from the Lenstar or the Pentacam.
Footnotes
Source of Support: This study was supported in part by a grant from the Ankara University
Conflict of Interest: None declared.
REFERENCES
- 1.Uçakhan OO, Ozkan M, Kanpolat A. Corneal thickness measurements in normal and keratoconic eyes: Pentacam comprehensive eye scanner versus noncontact specular microscopy and ultrasound pachymetry. J Cataract Refract Surg. 2006;32:970–7. doi: 10.1016/j.jcrs.2006.02.037. [DOI] [PubMed] [Google Scholar]
- 2.Lackner B, Schmidinger G, Skorpik C. Validity and repeatability of anterior chamber depth measurements with Pentacam and Orbscan. Optom Vis Sci. 2005;82:858–61. doi: 10.1097/01.opx.0000177804.53192.15. [DOI] [PubMed] [Google Scholar]
- 3.Cruysberg LP, Doors M, Verbakel F, Berendschot TT, De Brabander J, Nuijts RM. Evaluation of the Lenstar LS 900 non-contact biometer. Br J Ophthalmol. 2010;94:106–10. doi: 10.1136/bjo.2009.161729. [DOI] [PubMed] [Google Scholar]
- 4.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10. [PubMed] [Google Scholar]
- 5.Olsen T. Calculation of intraocular lens power: A review. Acta Ophthalmol Scand. 2007;85:472–85. doi: 10.1111/j.1600-0420.2007.00879.x. [DOI] [PubMed] [Google Scholar]
- 6.Shankar H, Taranath D, Santhirathelagan CT, Pesudovs K. Anterior segment biometry with the Pentacam: Comprehensive assessment of repeatability of automated measurements. J Cataract Refract Surg. 2008;34:103–13. doi: 10.1016/j.jcrs.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 7.Chen D, Lam AK. Reliability and repeatability of the Pentacam on corneal curvatures. Clin Exp Optom. 2009;92:110–8. doi: 10.1111/j.1444-0938.2008.00336.x. [DOI] [PubMed] [Google Scholar]
- 8.Huang J, Pesudovs K, Wen D, Chen S, Wright T, Wang X, et al. Comparison of anterior segment measurements with rotating Scheimpflug photography and partial coherence reflectometry. J Cataract Refract Surg. 2011;37:341–8. doi: 10.1016/j.jcrs.2010.08.044. [DOI] [PubMed] [Google Scholar]
- 9.Elbaz U, Barkana Y, Gerber Y, Avni I, Zadok D. Comparison of different techniques of anterior chamber depth and keratometric measurements. Am J Ophthalmol. 2007;143:48–53. doi: 10.1016/j.ajo.2006.08.031. [DOI] [PubMed] [Google Scholar]
- 10.Módis L, Jr, Szalai E, Kolozsvári B, Németh G, Vajas A, Berta A. Keratometry evaluations with the Pentacam high resolution in comparison with the automated keratometry and conventional corneal topography. Cornea. 2012;31:36–41. doi: 10.1097/ICO.0b013e318204c666. [DOI] [PubMed] [Google Scholar]
- 11.Whang WJ, Byun YS, Joo CK. Comparison of refractive outcomes using five devices for the assessment of preoperative corneal power. Clin Experiment Ophthalmol. 2012;40:425–32. doi: 10.1111/j.1442-9071.2012.02777.x. [DOI] [PubMed] [Google Scholar]
- 12.Savini G, Olsen T, Carbonara C, Pazzaglia S, Barboni P, Carbonelli M, et al. Anterior chamber depth measurement in pseudophakic eyes: A comparison of Pentacam and ultrasound. J Refract Surg. 2010;26:341–7. doi: 10.3928/1081597X-20090617-02. [DOI] [PubMed] [Google Scholar]
- 13.Rohrer K, Frueh BE, Wälti R, Clemetson IA, Tappeiner C, Goldblum D. Comparison and evaluation of ocular biometry using a new noncontact optical low-coherence reflectometer. Ophthalmology. 2009;116:2087–92. doi: 10.1016/j.ophtha.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 14.Woodmass J, Rocha G. A comparison of Scheimpflug imaging simulated and Holladay equivalent keratometry values with partial coherence interferometry keratometry measurements in phakic eyes. Can J Ophthalmol. 2009;44:700–4. doi: 10.3129/i09-172. [DOI] [PubMed] [Google Scholar]
- 15.Reuland MS, Reuland AJ, Nishi Y, Auffarth GU. Corneal radii and anterior chamber depth measurements using the IOLmaster versus the Pentacam. J Refract Surg. 2007;23:368–73. doi: 10.3928/1081-597X-20070401-09. [DOI] [PubMed] [Google Scholar]


