Abstract
Purpose:
The purpose of this study was to evaluate the anterior segment measurements according to refractive status in a sample of the Iranian population.
Setting:
Rassoul Akram Hospital, Tehran University of Medical Sciences.
Material and Methods:
In this study, refractive surgery candidates were assigned according to the refractive error to one of three groups : emmetropia, myopia, and hyperopia. Myopic eyes were further divided to four subgroups : simple myopic group, simple myopic astigmatism group, high myopic group, and high myopia with astigmatism group. Anterior segment measurements with the Pentacam Scheimpflug system were performed in the right eye of all subjects.
Results:
The study sample was comprised of 283 subjects with a mean age of 29.1 ± 7.5 (standard deviation) years. Mean keratometry reading, Anterior chamber depth (ACD) and volume measurements were significantly higher in the myopic group and mean keratometry reading and anterior chamber angle measurements were significantly lower in the hyperopic group (P < 0.05, all comparisons). Maximum anterior elevation (AEmax) and maximum posterior elevation (PEmax), Q value, progression index, minimum corneal thickness, and corneal volume measurements were similar for all groups (P > 0.05, all comparisons). In the myopic subgroups, AEmax and PEmax and maximum keratometry (Kmax) were significantly higher, and ACD was lower in the astigmatic groups (P < 0.05, all comparisons). The Q value was less negative in low myopia (P < 0.05).
Conclusions:
Myopic eyes had steeper corneas than hyperopic eyes and anterior chamber measurements were significantly higher in the myopic eyes. In myopic eyes, AEmax and PEmax and Kmax measurements were higher, and ACD measurements were lower in the astigmatic groups.
Keywords: Anterior Chamber, Keratometry, Pachymetry, Pentacam Scheimpflug Camera
INTRODUCTION
The Pentacam (Oculus Optikgerδte GmbH, Wetzlar, Germany) has become a popular device for evaluating the anterior segment of the eye since its launch in 2004. Previous studies have shown excellent reproducibility of this device for the automated measurements of the anterior segment structures.1,2,3,4 The Pentacam system may be used for the diagnosis of keratoconus, monitoring post-surgical corneas, calculating the keratometric index, intraocular lens power, and assessment of intraocular lens implants.4,5,6,7,8,9,10 Despite several reports on corneal thickness (CT),5 anterior and posterior corneal curvature and elevation,1,2,4 anterior chamber depth (ACD) and anterior chamber angle (ACA),3,11,12 and corneal volume (CV) measurements,5,12 little is known about the distribution of these measurements in the normal population and its relation to the refractive status. We evaluated the distribution of the anterior segment measurements in a population of normal Iranian subjects with different types of refractive errors.
MATERIAL AND METHODS
From January 2008 to January 2010, all patients presented for corneal refractive surgery were evaluated. Exclusion criteria included a history of corneal injury, illness, previous ocular surgery, contact lens wear during the past 3 weeks, and pregnancy.
The study was performed in accordance with the Declaration of Helsinki guidelines for human research.
The right eye of each patient was selected for measurement with the Scheimpflug camera (Pentacam, software version 1.12) with the 50-image mode. The images were obtained using the automatic mode when correct alignment with the corneal apex and focus were achieved. To avoid miscalculations due to poor imaging quality, only measurements with “OK” quality statements were selected for the study. The CT, anterior elevation (AE), posterior elevation (PE), sagittal curvature, and keratoconus maps were evaluated. The maximum anterior elevation in 4 mm central circle (AEmax), maximum posterior elevation in 4 mm central circle (PEmax), minimum corneal thickness, 3, 5, and 7 mm corneal volumes (CV3, CV5, CV7), mean keratometry (Km), maximum keratometry (Kmax) in 4 mm central circle, Q value (Q), average progression index, ACD, anterior chamber volume (ACV), and ACA measurements automatically provided by the software were recorded. For Kmax, AEmax and PEmax, the cursor was moved through the screen to find the maximum number for the central 4 mm circle. From the AE and PE map options, automatic diameters were selected for the float best-fit spheres.
The patients were divided into three groups according to the manifest refractive error. Emmetropic eyes consisted of patients within ±0.5 diopters (D) of plano and uncorrected visual acuity of 20/20. The myopic group included eyes with a spherical equivalent refraction of –0.75 D or more and hyperopic group included eyes with a spherical equivalent refraction of +0.75 or more. The myopic group was further divided into 4 subgroups; the simple myopic subgroup consisted of patients with a spherical refraction of –6.0 D or less and a cylindrical refraction of 1.00 D or less; the simple myopic astigmatism subgroup consisted of patients with a spherical refraction of –6.0 D or less and a cylindrical refraction greater than 1.0 D; the high myopic subgroup consisted of patients with a spherical refraction greater than –6.0 D and a cylindrical refraction of 1.0 D or less and; the high myopia with astigmatism subgroup consisted of patients with a spherical refraction greater than –6.0 D and a cylindrical refraction greater than 1.0 D.
Data were entered using the SPSS software (version 15, SPSS Inc.). Analyses were performed with the Chi-square test, ANOVA test, t-test, and correlation test. A P value less than 0.05 was considered statistically significant.
RESULTS
A total of 283 subjects comprised the study cohort. The mean age of the participants was 29.1 ± 7.5 years (range 18-56 years). One hundred seven participants (37.5%) were men. Patient demographics are presented in Table 1. There were 21 emmetropic eyes, 20 hyperopic eyes, and 242 myopic eyes. From the myopes, there were156 eyes in the simple myopic group, 47 eyes in the simple myopic astigmatism group, 17 eyes in the highly myopic group, and 22 eyes in the highly myopic with astigmatism group.
Table 1.
Patient demographics
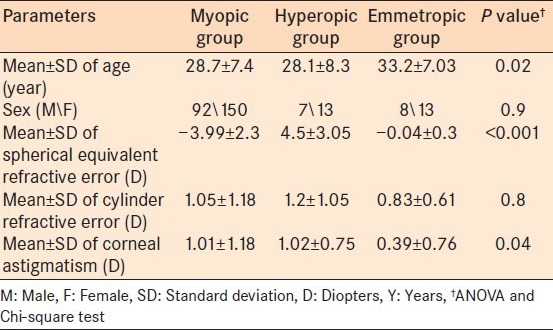
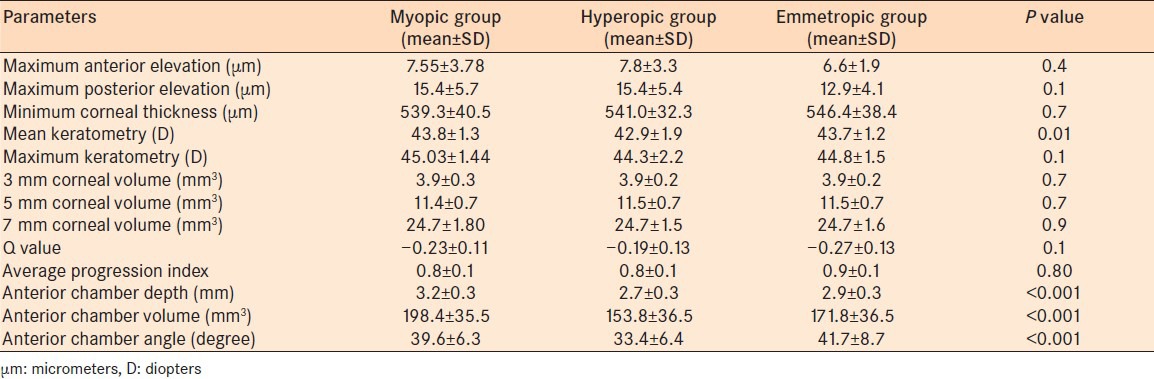
Table 2 present the different measurements between the emmetropic, myopic, and hyperopic groups. Km reading, ACD, ACV, and ACA measurements were significantly different between the three groups. Post-hoc analysis revealed higher values in the myopic group for ACD, ACV (P < 0.001 and P < 0.001, respectively) and lower values in the hyperopic group for Km and ACA (P = 0.01 and P < 0.001, respectively).
Table 2.
Measurement of structures in the anterior segment with the Pentacam Scheimpflug camera in emmetropic, myopic, and hyperopic eyes
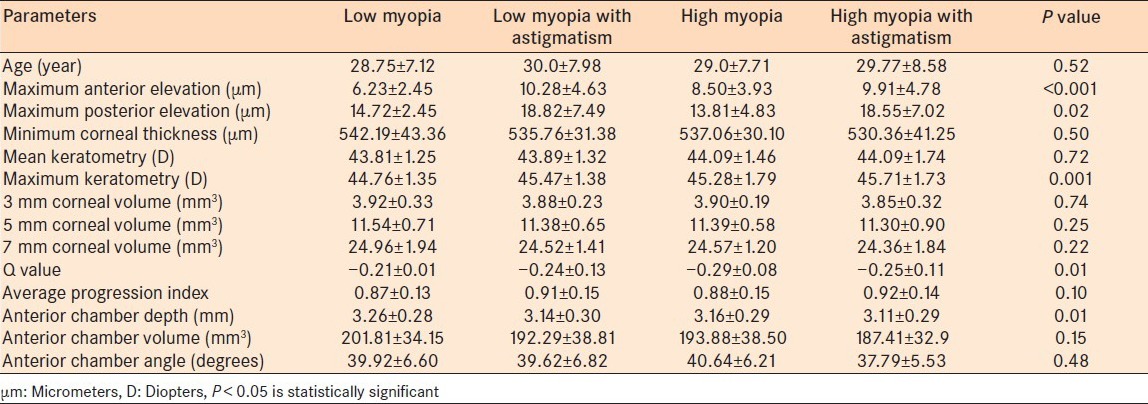
Subgroup analysis revealed a significant difference in AEmax, PEmax, Kmax, Q, and ACD between the four myopic groups [P < 0.05 all comparisons; Table 3]. AEmax, PEmax, and Kmax were significantly higher, and ACD was significantly lower in the astigmatic subgroups (P < 0.05, all comparisons). The Q value was less negative in low myopia (P > 0.05)
Table 3.
Measurement of structures in the anterior segment with the Pentacam Scheimpflug camera (mean±SD) in four myopic subgroups
In the entire study population, statistically significant correlations were found for AEmax and corneal astigmatic measurements [r = 0.67, P < 0.001; Figure 1], PEmax and corneal astigmatic measurements (r = 0.57, P < 0.001) and Kmax and corneal astigmatic measurements (r = 0.27, P = 0.01).
Figure 1.
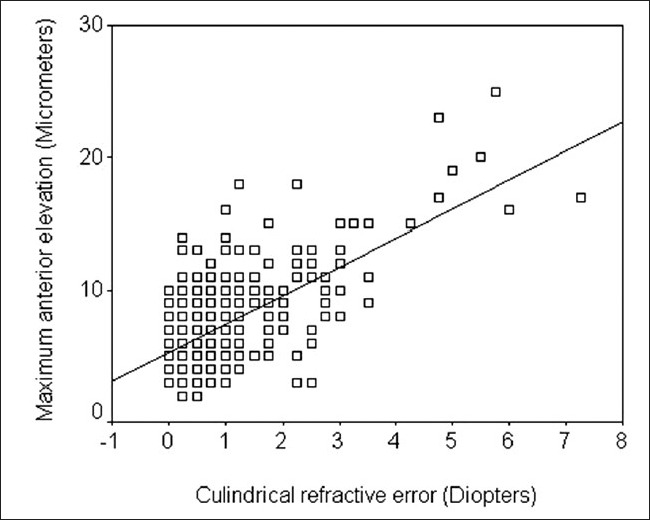
A significant correlation was found between the maximum anterior elevation and corneal astigmatic measurements
DISCUSSION
Adequate information on normal anterior segment measurements is essential for the diagnosis and treatment of abnormal ocular conditions. Obtaining and appropriately analyzing data on anterior segment structures have become more critical as various refractive surgical procedures continue to evolve and gain popularity. Different instruments are available to measure the optical and anatomical properties of the anterior segment of the eye. Among these, the Pentacam is unique in its ability to evaluate the entire anterior eye segment. The Pentacam provides clinically relevant and reproducible information from the anterior corneal surface to the posterior lens surface in a single scan without contact with the cornea.1,2,3,4 Our study evaluated the distribution of the parameters available from the Pentacam system in eyes with various refractive disorders in a sample of the Iranian population, in an attempt to better discriminate normal from abnormal values. The data from our study will aid in screening candidates for refractive surgery.
Our results show that hyperopic eyes had lower AEmax and PEmax (although not significant), and keratometry readings. The mean PEmax in our study (15.4 ± 5.7 in myopic eyes and 15.4 ± 5.4 in hyperopic eyes) are different from those reported by de Sanctis et al.,13 (19.8 ± 6.37). We used automatic diameters for the float best fitted spheres as recommended by Belin (Belin M. Proposed Screening Parameters. Pentacam Interpretation Guideline. Oculus Optikgerδte GmbH). However, de Sanctis et al.,13 used the 9 mm measurements, which may explain the difference from the data in our study. The Km readings are automatically generated by the instrument, and our findings are similar to the previous reports.3,4,14 There have been conflicting reports regarding the relationship between refractive error and corneal curvature. Parssinen,15 reported no correlation between the degree of myopia and corneal curvature. Our results; however, concur with the majority of studies that show corneal power in myopia is on average about 1.0 D greater than in hyperopia.16,17,18 Interestingly, we found higher AEmax and PEmax and Kmax readings in astigmatic eyes. When interpreting the elevation and keratometry maps in astigmatic eyes, one must consider that the high elevations and readings may represent the normal shape of the astigmatic band. To remove the effect of this astigmatic band on the elevation maps, Holladay recommends using the best-fitted toric ellipsoid option as a reference shape (Holladay J. Using the Holladay report on the Oculus Pentacam. In: The Pentacam: Precision, Confidence, Results, and Accurate “Ks!” Cataract and Refractive Surgery Today January 2007).
CT has been identified as a major determinant for measurement error of intraocular pressure and an independent risk factor for open-angle glaucoma.19 It is also important for the diagnosis of subclinical keratoconus in patients presenting for refractive surgery.20 Values outside the accepted normal range may suggest that the patient is a poor candidate for refractive surgery or that further evaluation is warranted before undergoing a refractive procedure.20,21 Studies that attempted to evaluate the effect of refractive errors, in particular degree of myopia on the central corneal thickness show conflicting results.14,22,23,24 In contrast to Murata et al.,22 and similar to those reported by Uçakhan et al.,14 we found there was no significant difference between hyperopic and myopic CT measurements (P > 0.05). Although the thinnest CT measurements were lower in high myopic eyes, the difference was not statistically significant (P > 0.05).
Recently, measurement of CV has been proposed to be useful in detecting keratoconus and planning intracorneal ring implantation.5,12 Ambrósio et al.,5 reported that the CV measurements in eyes with mild to moderate keratoconus were significantly lower than those in a group of normal eyes. Emre et al.,12 suggested that evaluating the CV within the 7.0 mm optical zone is essential to reduce the risk for implant extrusion. We found no significant difference between the myopic and hyperopic CV measurements. Although not significant, the CV of high myopic eyes was less than other myopic eyes.
The aspheric nature of the normal cornea is well-established.25,26 A negative Q-value (prolate) is defined as progressive corneal flattening from center to periphery, whereas a positive Q-value (oblate) is defined as increasing corneal curvature moving from center to periphery.27 Previous studies reported mean Q-values in normal corneas between –0.11 and –0.33, with a mean of –0.26.18,25 Our results support the findings of Sheridan and Douthwaite25 who found no significant difference in asphericity among emmetropes, myopes, and hyperopes.
The anterior chamber parameters are clinically useful for planning intraocular lens (IOL) power calculation for cataract surgery and phakic IOL placement in refractive surgery.26,27,28
Our results on the association between deeper anterior chamber, higher chamber volume, wider chamber angles, and myopia concur with previous studies on other ethnic populations.22,29,30 These data further explain why hyperopia is a predominant risk factor for a primary angle-closure glaucoma.31 Among the different subgroups of myopic eyes in the current study, higher ACD, and ACV measurements were found in low myopic eyes. These outcomes are similar to findings reported by Murata et al.,22 who reported a shallower anterior chamber in highly myopic eyes (>–9 D). However, Uçakhan et al.,14 reported significantly higher ACD and ACV measurements in the high myopic group. Different refractive definitions for the study eyes may be responsible for this discrepancy.
This study has some limitations, and the sample size is small especially in the emmetropic and hyperopic groups. This is comparable to some previous studies14,22 and actually represents the normal distribution of patients presenting for refractive surgery. The age range of patients presenting for refractive surgery is limited; some anterior segments parameters may be affected by age.
In conclusion, in this study, myopic eyes were found to have steeper corneas than hyperopic eyes and anterior chamber measurements (ACD, ACV, and ACA) were significantly higher in myopic eyes. In myopic eyes, maximum elevations and keratometry measurements were higher, and ACD measurements were lower in astigmatic groups. The information gained from this study may provide a general estimate of anterior segment parameters in the Iranian population as obtained from Pentacam.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Piñero DP, Saenz González C, Alió JL. Intraobserver and interobserver repeatability of curvature and aberrometric measurements of the posterior corneal surface in normal eyes using Scheimpflug photography. J Cataract Refract Surg. 2009;35:113–20. doi: 10.1016/j.jcrs.2008.10.010. [DOI] [PubMed] [Google Scholar]
- 2.Chen D, Lam AK. Intrasession and intersession repeatability of the Pentacam system on posterior corneal assessment in the normal human eye. J Cataract Refract Surg. 2007;33:448–54. doi: 10.1016/j.jcrs.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 3.Shankar H, Taranath D, Santhirathelagan CT, Pesudovs K. Anterior segment biometry with the Pentacam: Comprehensive assessment of repeatability of automated measurements. J Cataract Refract Surg. 2008;34:103–13. doi: 10.1016/j.jcrs.2007.09.013. [DOI] [PubMed] [Google Scholar]
- 4.Chen D, Lam AK. Reliability and repeatability of the Pentacam on corneal curvatures. Clin Exp Optom. 2009;92:110–8. doi: 10.1111/j.1444-0938.2008.00336.x. [DOI] [PubMed] [Google Scholar]
- 5.Ambrósio R, Jr, Alonso RS, Luz A, Coca Velarde LG. Corneal-thickness spatial profile and corneal-volume distribution: Tomographic indices to detect keratoconus. J Cataract Refract Surg. 2006;32:1851–9. doi: 10.1016/j.jcrs.2006.06.025. [DOI] [PubMed] [Google Scholar]
- 6.Ciolino JB, Khachikian SS, Cortese MJ, Belin MW. Long-term stability of the posterior cornea after laser in situ keratomileusis. J Cataract Refract Surg. 2007;33:1366–70. doi: 10.1016/j.jcrs.2007.04.016. [DOI] [PubMed] [Google Scholar]
- 7.Ertan A, Kamburoğlu G. Analysis of centration of Intacs segments implanted with a femtosecond laser. J Cataract Refract Surg. 2007;33:484–7. doi: 10.1016/j.jcrs.2006.11.007. [DOI] [PubMed] [Google Scholar]
- 8.Wheeldon CE, Hadden OB, Niederer RL, McGhee CN. Presumed late diffuse lamellar keratitis progressing to interface fluid syndrome. J Cataract Refract Surg. 2008;34:322–6. doi: 10.1016/j.jcrs.2007.09.025. [DOI] [PubMed] [Google Scholar]
- 9.Borasio E, Stevens J, Smith GT. Estimation of true corneal power after keratorefractive surgery in eyes requiring cataract surgery: BESSt formula. J Cataract Refract Surg. 2006;32:2004–14. doi: 10.1016/j.jcrs.2006.08.037. [DOI] [PubMed] [Google Scholar]
- 10.Turner SJ, Lee EJ, Hu V, Hollick EJ. Scheimpflug imaging to determine intraocular lens power in vivo. J Cataract Refract Surg. 2007;33:1041–4. doi: 10.1016/j.jcrs.2007.02.023. [DOI] [PubMed] [Google Scholar]
- 11.Rabsilber TM, Khoramnia R, Auffarth GU. Anterior chamber measurements using Pentacam rotating Scheimpflug camera. J Cataract Refract Surg. 2006;32:456–9. doi: 10.1016/j.jcrs.2005.12.103. [DOI] [PubMed] [Google Scholar]
- 12.Emre S, Doganay S, Yologlu S. Evaluation of anterior segment parameters in keratoconic eyes measured with the Pentacam system. J Cataract Refract Surg. 2007;33:1708–12. doi: 10.1016/j.jcrs.2007.06.020. [DOI] [PubMed] [Google Scholar]
- 13.de Sanctis U, Loiacono C, Richiardi L, Turco D, Mutani B, Grignolo FM. Sensitivity and specificity of posterior corneal elevation measured by Pentacam in discriminating keratoconus/subclinical keratoconus. Ophthalmology. 2008;115:1534–9. doi: 10.1016/j.ophtha.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 14.Uçakhan OO, Gesoğlu P, Ozkan M, Kanpolat A. Corneal elevation and thickness in relation to the refractive status measured with the Pentacam Scheimpflug system. J Cataract Refract Surg. 2008;34:1900–5. doi: 10.1016/j.jcrs.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 15.Pärssinen TO. Corneal refraction and topography in school myopia. CLAO J. 1993;19:69–72. doi: 10.1097/00140068-199301000-00013. [DOI] [PubMed] [Google Scholar]
- 16.Carney LG, Mainstone JC, Henderson BA. Corneal topography and myopia. A cross-sectional study. Invest Ophthalmol Vis Sci. 1997;38:311–20. [PubMed] [Google Scholar]
- 17.Goss DA, Cox VD, Herrin-Lawson GA, Nielsen ED, Dolton WA. Refractive error, axial length, and height as a function of age in young myopes. Optom Vis Sci. 1990;67:332–8. doi: 10.1097/00006324-199005000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Budak K, Khater TT, Friedman NJ, Holladay JT, Koch DD. Evaluation of relationships among refractive and topographic parameters. J Cataract Refract Surg. 1999;25:814–20. doi: 10.1016/s0886-3350(99)00036-x. [DOI] [PubMed] [Google Scholar]
- 19.Brandt JD. Corneal thickness in glaucoma screening, diagnosis, and management. Curr Opin Ophthalmol. 2004;15:85–9. doi: 10.1097/00055735-200404000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Khachikian SS, Belin MW, Ciolino JB. Intrasubject corneal thickness asymmetry. J Refract Surg. 2008;24:606–9. doi: 10.3928/1081597X-20080601-09. [DOI] [PubMed] [Google Scholar]
- 21.Falavarjani KG, Modarres M, Joshaghani M, Azadi P, Afshar AE, Hodjat P. Interocular differences of the Pentacam measurements in normal subjects. Clin Exp Optom. 2010;93:26–30. doi: 10.1111/j.1444-0938.2009.00446.x. [DOI] [PubMed] [Google Scholar]
- 22.Murata C, Mallmann F, Yamazaki E, Campos M. Anterior ocular segment study with the Scheimpflug rotational camera in refractive surgery candidates. Arq Bras Oftalmol. 2007;70:619–24. doi: 10.1590/s0004-27492007000400012. [DOI] [PubMed] [Google Scholar]
- 23.Pedersen L, Hjortdal J, Ehlers N. Central corneal thickness in high myopia. Acta Ophthalmol Scand. 2005;83:539–42. doi: 10.1111/j.1600-0420.2005.00498.x. [DOI] [PubMed] [Google Scholar]
- 24.Fam HB, How AC, Baskaran M, Lim KL, Chan YH, Aung T. Central corneal thickness and its relationship to myopia in Chinese adults. Br J Ophthalmol. 2006;90:1451–3. doi: 10.1136/bjo.2006.101170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sheridan M, Douthwaite WA. Corneal asphericity and refractive error. Ophthalmic Physiol Opt. 1989;9:235–8. doi: 10.1111/j.1475-1313.1989.tb00899.x. [DOI] [PubMed] [Google Scholar]
- 26.Fleming JF. Corneal asphericity and visual function after radial keratotomy. Cornea. 1993;12:233–40. [PubMed] [Google Scholar]
- 27.Olsen T, Corydon L, Gimbel H. Intraocular lens power calculation with an improved anterior chamber depth prediction algorithm. J Cataract Refract Surg. 1995;21:313–9. doi: 10.1016/s0886-3350(13)80140-x. [DOI] [PubMed] [Google Scholar]
- 28.Mimouni F, Colin J, Koffi V, Bonnet P. Damage to the corneal endothelium from anterior chamber intraocular lenses in phakic myopic eyes. Refract Corneal Surg. 1991;7:277–81. [PubMed] [Google Scholar]
- 29.Rabsilber TM, Becker KA, Frisch IB, Auffarth GU. Anterior chamber depth in relation to refractive status measured with the Orbscan II Topography System. J Cataract Refract Surg. 2003;29:2115–21. doi: 10.1016/s0886-3350(03)00409-7. [DOI] [PubMed] [Google Scholar]
- 30.Congdon NG, Youlin Q, Quigley H, Hung PT, Wang TH, Ho TC, et al. Biometry and primary angle-closure glaucoma among Chinese, white, and black populations. Ophthalmology. 1997;104:1489–95. doi: 10.1016/s0161-6420(97)30112-2. [DOI] [PubMed] [Google Scholar]
- 31.Salmon JF. Predisposing factors for chronic angle-closure glaucoma. Prog Retin Eye Res. 1999;18:121–32. doi: 10.1016/s1350-9462(98)00007-x. [DOI] [PubMed] [Google Scholar]


