Abstract
Aim:
To evaluate the effect of implantation depth of Intacs microthin prescription inserts (Addition Technology Inc, Fremont, California) on visual and topographic outcomes in patients with post- laser-assisted in situ keratomileusis (LASIK) ectasias.
Settings and Design:
Retrospective, observational case series.
Materials and Methods:
In this case series, 16 eyes of 12 patients were evaluated. All cases were post-LASIK ectasia that had undergone intrastromal corneal ring segment (ICRS) implantation. The planned insertion depth was 70% of stromal thickness using a manual dissector. At least 12 months postoperatively, all eyes underwent Visante (Carl Zeiss Meditec) AS-OCT to determine insertion depth. Cases were categorized into 3 groups based on the measured implantation depth: 40-59% thickness; 60-79% thickness; and ≥80% thickness. Visual, refractive and topographic outcomes were evaluated relative to implantation depth.
Results:
The lowest improvement in the study parameters ocurred when the implantation depth was ≥80%. In this group, uncorrected visual acuity (UCVA) and best spectacle corrected VA (BSCVA) improved less than 0.5 lines. Manifest refractive spherical equivalent (MRSE) and mean keratometry (Km) change was less than 0.5 diopters (D). The greatest improvements were observed with implantation depth of 60-79% where UCVA and BSCVA increased by 4.5 and 2.5 lines respectively, and MRSE and Km changed by approximately 2.00 D. Less improvement was found when ICRS were implanted between 40-59% of stromal thickness.
Conclusion:
Implantation of ICRS greater than 80% of stromal thickness may have no effect on visual and topographic status.
Keywords: Intacs implantation depth, Laser-assisted in situ Keratomileusis, optical coherence tomography, post–lasik Ectasia, visual Acuity
INTRODUCTION
Intacs microthin prescription inserts (Addition Technology Inc, Fermont, California) were first developed for the correction of myopia from -1.0 to -3.0 diopters (D).1,2 These intrastromal corneal ring segments (ICRS) are a 150 degree polymethyl methacrylate segment, hexagonal in cross-section, which are inserted deep into the stroma. ICRS implanation stretches the cornea peripherally resulting in central corneal flattening.3,4
Colin et al.5 were the first to implant ICRS for keratoconus. Subsequently, several authors reported on ICRS implantation for keratoconus,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23 post-LASIK ectasia24,25,26,27,28,29,30,31,32,33,34,35 and pellucid marginal degeneration.36,37,38,39,40,41,42 However, to the best of our knowledge, there are no reports on the effect of insertion or implantation depth of ICRS on the outcome. In this study we evaluate the outcome of Intacs ICRS implantation relative to the insertion depth as measured with anterior segment optical coherent tomography (AS-OCT).
MATERIALS AND METHODS
In this retrospective study, we reviewed the records of all patients who underwent Intacs ICRS implantation for post-LASIK ectasia between 2006 and 2008. To be included all patients had to have greater than 1 year postoperative follow up. The Institutional Review Board of the Eye Research Center, Farabi Eye Hospital approved this study.
All surgeries were performed by an experienced surgeon (H.H). In all cases, 0.45 mm thick segments were implanted. A single segment was implanted for decentered cones, and double segments were implanted for central cones. Surgeries were performed with tetracaine as topical anesthesic. First, the geometric center of the cornea was marked with a blunt Sinskey hook. Then, using a circular marker, the 7.0 mm optical zone and the incision position in the flat meridian were marked. A 0.9 mm vertical incision was made with a calibrated diamond knife to a depth of 70% of the corneal thickness at the insertion location as measured preoperatively using the Pentacam rotating scheimflug camera (Oculus Gmbh, Wetzlar, Germany). After inspecting whether the depth of incision was adequate, a pocketing hook was applied to the base of the incision to create a pocket on either side taking care they were made to an equal level. After placing the vacuum centering guide, the corneal separator was inserted, and the clockwise and counterclockwise dissections were made. Next, the ICRS segment was manually introduced through the incision into the tunnel and advanced until the end was approximately 1.5mm from the incision. Finally, the incision was closed with a 10-0 nylon suture. After surgery, antibiotic and steroid eye-drops four times a day were prescribed, and the suture was removed after six weeks.
Patient evaluation
The following preoperative and postoperative data were evaluated: uncorrected visual acuity (UCVA); best spectacle corrected visual acuity (BSCVA); manifest refractive spherical equivalent (MRSE); refractive cylinder (RC); steep keratometry reading (K1), flat keratometry reading (K2), mean keratometry (Km =[K1+K2]/2), topographic cylinder (TC=K1-K2) from the EyeSys Corneal Analysis System (EyeSys Technologies, Houston, Tx, USA). UCVA and BSCVA were converted to logMAR for statistical analysis. AS-OCT was performed postoperatively using the Visante (Carl Zeiss Meditec, Jena, Germany) to determine the depth at which Intacs segments were implanted into the cornea. The depth of implanted segment was measured at the middle of its length. The stromal thickness was measured over (S1) and under (S2) the segment. Intacs depth was calculated as S1/(S1+S2), and the result was multiplied by 100 to determine the percent of stromal depth at which the ICRS had been inserted. If the two segments had been implanted, then the results of superior and inferior segments were averaged. The cases were categorized into 3 groups based on the measured depth of implantation: 40-59%, 60-79%, and ≥80% thickness depths. There were no cases with less than 40% implantation depth. Visual, refractive, and topographic outcomes were compared among the three groups.
Statistical analysis
Data were analyzed with the Statistical Package for Social Sciences software for windows (version 16.0, IBM Inc., Armonk, NY, USA). The Wilcoxon rank-sum test was used to compare preoperative and postoperative values of UCVA, BSCVA, MRSE, RC, K1, K2, Km, and TC. A p value less than 0.05 were statistically significant.
RESULTS
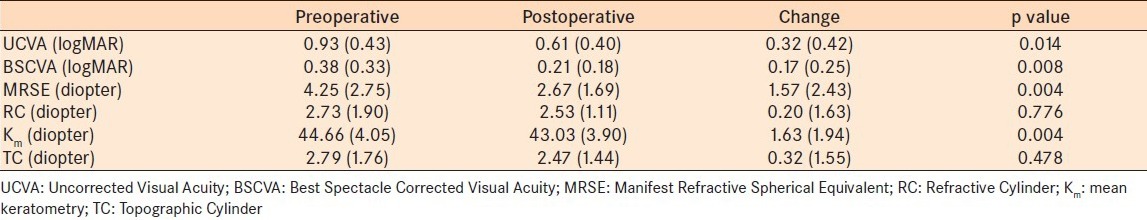
Sixteen eyes of 12 patients were evaluated. The mean age of the patients was 33.25 ± 9.2 years (range, 25 years to 54 years) and the male/female and right/left eye ratios were 1:1. Mean follow up time was 23.8 ± 9.11 m (range, 12 m to 24 m). Based on AS-OCT measurements, we had 3 cases (18.8%) in the 40-59% thickness group, 9 cases (56.2%) in the 60-79% thickness, group and 4 cases (25.0%) in the ≥80% stromal thickness group. Results of the preoperative and last postoperative visits are summarized in Table 1.
Table 1.
Mean (± standard deviation) values and changes of visual, refractive, and topographic variables before and after surgery in the entire study cohort
Visual outcome
Overall, UCVA changed by 0.32 ± 0.42 logMAR which is approximately a gain of 3 Snellen lines. BSCVA increased by 0.17 ± 0.25, which correlates a gain of 1.5 Snellen lines. Best outcomes were observed in the 60-79% thickness group. Table 2 presents the visual outcomes relative to insertion depth.
Table 2.
Mean (± standard deviation) change (preoperative versus postoperative) in visual, refractive, and topographic variables relative to the depth of Intacs insertion
Refractive and topographic outcome
Overall, MRSE and Km decreased by 1.57 ± 2.43 D and 1.6 ± 1.94 D respectively (p <0.05). The outcome was best when the ICRS were implanted to 60-79% of the stromal thickness; MRSE and Km change was 2.11 ± 3.11 D and 2.08 ± 2.40 D, respectively. When the ICRS were implanted into 80-99% of stromal depth, they had little to no effect [Table 2]. RC and TC did not show clinically or statistically significant changes as a result of surgery; overall RC and TC changes were 0.20 ±1.6 3 D and 0.32 ± 0.32 D, respectively (p >0.05, both cases). Astigmatism did not show clinically significant changes after ICRS implantation relative to depth of implantation (p >0.05; Table 2).
DISCUSSION
Several authors have demonstrated that ICRS implantation in post-Lasik ectasia can improve UCVA and BCVA by approximately 70%.16,17,18,19,20,21,22,23,24,25,26,27 However, to the best of our knowledge, there are no reports evaluating the effect of implantation depth in the corneal stroma on the postoperative outcome after ICRS.
As demonstrated in Table 2, UCVA, BSCVA, MRSE, and Km improved most significantly when the ICRS were implanted at 60-79% thickness, but there was little or no effect when the ICRS was implanted deeper than 80%. Results in the 40-59% thickness group were not as favorable as the 60-79% thickness group.
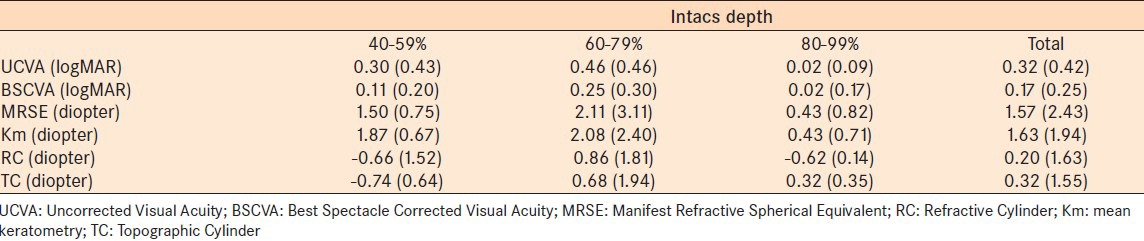
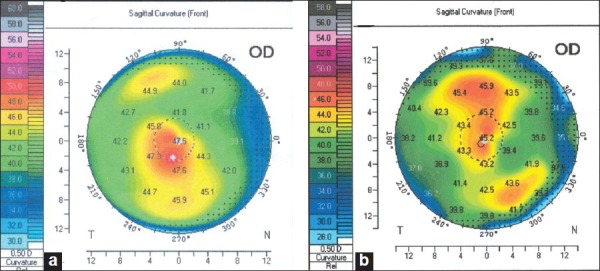
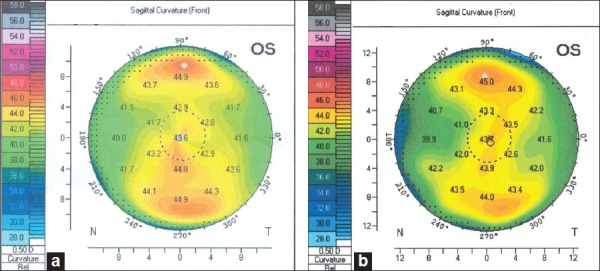
Figure 1 shows the preoperative and postoperative topography of an eye with post-LASIK ectasia treated with a single ICRS inferiorly. AS-OCT showed a depth of 61% of stromal thickness [Figure 2]. Some steepening right above the Intacs that might lead to central flattening was observed. Figure 3 shows the topography of the same patient's left eye which underwent implantation of a single ICRS inferiorly. However, this segment was inserted at 83% thickness [Figure 4]. No curvature change occurred over the ICRS and thus, no central flattening was expected. Corneal topography at 24 months postoperatively demonstrated no significant changes in keratometric power.
Figure 1.
Preoperative (a) and postoperative (b) topography of a patient right eye with post-LASIK ectasia that was implanted with a single intrastromal corneal ring segment
Figure 2.

Anterior segment optical coherence tomography of the right eye
Figure 3.
Preoperative (a) and postoperative (b) topography of the same patient left eye
Figure 4.

Anterior segment optical coherence tomography of the left eye.
CONCLUSION
The corneal stromal depth at which ICRS are implanted may be an important determinant of visual and topographic outcomes after surgery. Implanting ICRS too deep in the stroma (deeper than 80% stromal depth), may have no effect on the corneal curvature. The best stromal depth is 60-79%, and insertion in the stromal depth of 40-59% may have a lower effect.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Schanzlin DJ, Asbell PA, Burris TE, Durrie DS. The intrastromal corneal ring segments; phase II results for the correction of myopia. Ophthalmology. 1997;104:1067–78. doi: 10.1016/s0161-6420(97)30183-3. [DOI] [PubMed] [Google Scholar]
- 2.Burris TE. Intrastromal corneal ring technology: Results and indications. Curr Opin Ophthalmol. 1998;9:9–14. doi: 10.1097/00055735-199808000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Burris TE, Ayer CT, Evensen DA, Davenport JM. Effects of intrastromal corneal ring size and thickness on corneal flattening in human eyes. Refract Corneal Surg. 1991;7:46–50. [PubMed] [Google Scholar]
- 4.Burris TE, Baker PC, Ayer CT, Loomas BE, Mathis ML, Silvestrini TA. Flattening of central corneal curvature with intrastromal corneal rings of increasing thickness: An eyebank eye study. J Cataract Refract Surg. 1993;19(Suppl):182–7. doi: 10.1016/s0886-3350(13)80404-x. [DOI] [PubMed] [Google Scholar]
- 5.Colin J, Cochener B, Savary G, Malet F. Correcting keratoconus with intracorneal rings. J Cataract Refract Surg. 2000;26:1117–22. doi: 10.1016/s0886-3350(00)00451-x. [DOI] [PubMed] [Google Scholar]
- 6.Shetty R, Kurian M, Anand D, Mhaske P, Narayana KM, Shetty BK. Intacs in advanced keratoconus. Cornea. 2008;27:1022–9. doi: 10.1097/ICO.0b013e318172fc54. [DOI] [PubMed] [Google Scholar]
- 7.Ertan A, Ozkilic E. Effect of age on outcomes in patients with keratoconus treated by Intacs using a femtosecond laser. J Refract Surg. 2008;24:690–5. doi: 10.3928/1081597X-20080901-08. [DOI] [PubMed] [Google Scholar]
- 8.Ertan A, Kamburoglu G. Intacs implantation using femtosecond laser for management of keratoconus: Comparison of 306 cases in different stages. J Cataract Refract Surg. 2008;34:1521–6. doi: 10.1016/j.jcrs.2008.05.028. [DOI] [PubMed] [Google Scholar]
- 9.Shabayek MH, Alió JL. Intrastromal corneal ring segment implantation by femtosecond laser for keratoconus correction. Ophthalmology. 2007;114:1643–52. doi: 10.1016/j.ophtha.2006.11.033. [DOI] [PubMed] [Google Scholar]
- 10.Zare MA, Hashemi H, Salari MR. Intracorneal ring segment implantation for the management of keratoconus: Safety and efficacy. J Cataract Refract Surg. 2007;33:1886–91. doi: 10.1016/j.jcrs.2007.06.055. [DOI] [PubMed] [Google Scholar]
- 11.Kymionis GD, Siganos CS, Tsiklis NS, Anastasakis A, Yoo SH, Pallikaris AI, et al. Long-term follow-up of Intacs in keratoconus. Am J Ophthalmol. 2007;143:236–44. doi: 10.1016/j.ajo.2006.10.041. [DOI] [PubMed] [Google Scholar]
- 12.Alió JL, Shabayek MH, Artola A. Intracorneal ring segments for keratoconus correction: Long-term follow-up. J Cataract Refract Surg. 2006;32:978–85. doi: 10.1016/j.jcrs.2006.02.044. [DOI] [PubMed] [Google Scholar]
- 13.Alió JL, Shabayek MH, Belda JI, Correas P, Diez Feijoo E. Analysis of results related to good and bad outcomes of Intacs implantation for keratoconus correction. J Cataract Refract Surg. 2006;32:756–61. doi: 10.1016/j.jcrs.2006.02.012. [DOI] [PubMed] [Google Scholar]
- 14.Ertan A, Kamburoglu G, Bahadir M. Intacs insertion with the femtosecond laser for the management of keratoconus. One-year results. J Cataract Refract Surg. 2006;32:2039–42. doi: 10.1016/j.jcrs.2006.08.032. [DOI] [PubMed] [Google Scholar]
- 15.Colin J. European clinical evaluation: Use of Intacs for the treatment of keratoconus. J Cataract Refract Surg. 2006;32:747–55. doi: 10.1016/j.jcrs.2006.01.064. [DOI] [PubMed] [Google Scholar]
- 16.Kanellopoulos AJ, Pe LH, Perry HD, Donnenfeld ED. Modified intracorneal ring segment implantations (Intacs) for the management of moderate to advanced keratoconus. Efficacy and complications. Cornea. 2006;25:29–33. doi: 10.1097/01.ico.0000167883.63266.60. [DOI] [PubMed] [Google Scholar]
- 17.Hellstedt T, Mäkelä J, Uusitalo R, Emre S, Uusitalo R. Treating keratoconus with Intacs corneal ring segments. J Refract Surg. 2005;21:236–46. doi: 10.3928/1081-597X-20050501-06. [DOI] [PubMed] [Google Scholar]
- 18.Kwitko S, Severo NS. Ferrara intracorneal ring segments for keratoconus. J Cataract Refract Surg. 2004;30:812–20. doi: 10.1016/j.jcrs.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 19.Miranda D, Sartori M, Francesconi C, Allemann N, Ferrara P, Campos M. Ferrara intrastromal corneal ring segments for severe keratoconus. J Refract Surg. 2003;19:645–53. doi: 10.3928/1081-597X-20031101-06. [DOI] [PubMed] [Google Scholar]
- 20.Siganos CS, Kymionis GD, Kartakis N, Theodorakis MA, Astyrakakis N, Pallikaris IG. Management of keratoconus with Intacs. Am J Ophthalmol. 2003;135:64–70. doi: 10.1016/s0002-9394(02)01824-x. [DOI] [PubMed] [Google Scholar]
- 21.Boxer Wachler BS, Chandra NS, Chou B, Korn TS, Nepomuceno R, Christie JP. Intacs for keratoconus. Ophthalmology. 2003;110:1031–40. doi: 10.1016/s0161-6420(03)00094-0. [DOI] [PubMed] [Google Scholar]
- 22.Ruckhofer J, Stoiber J, Twa MD, Grabner G. Correction of astigmatism with short arc-length intrastromal corneal ring segments. Ophthalmology. 2003;110:516–24. doi: 10.1016/s0161-6420(02)01773-6. [DOI] [PubMed] [Google Scholar]
- 23.Colin J, Cochener B, Savary G, Malet F, Holmes- Higgin D. Intacs inserts for treating keratoconus. One year results. Ophthalmology. 2001;108:1409–14. doi: 10.1016/s0161-6420(01)00646-7. [DOI] [PubMed] [Google Scholar]
- 24.Carrasquillo KG, Rand J, Talamo JH. Intacs for keratoconus and post-LASIK ectasia: Mechanical versus femtosecond laser-assisted channel creation. Cornea. 2007;26:956–62. doi: 10.1097/ICO.0b013e31811dfa66. [DOI] [PubMed] [Google Scholar]
- 25.Uceda-Montanes A, Tomaás JD, Alioó JL. Correction of severe ectasia after LASIK with intracorneal ring segments. J Refract Surg. 2008;24:408–13. doi: 10.3928/1081597X-20080401-15. [DOI] [PubMed] [Google Scholar]
- 26.Kymionis GD, Tsiklis NS, Pallikaris AI, Kounis G, Diakonis VF, Astyrakakis N, et al. Long-term follow-up of Intacs for post-LASIK corneal ectasia. Ophthalmology. 2006;113:1909–17. doi: 10.1016/j.ophtha.2006.05.043. [DOI] [PubMed] [Google Scholar]
- 27.Sharma M, Boxer Wachler BS. Comparison of single-segment and double-segment Intacs for keratoconus and post-LASIK ectasia. Am J Ophthalmol. 2006;141:891–5. doi: 10.1016/j.ajo.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 28.Polkroy R, Levinger S, Hirsh A. Single Intacs segment for postlaser in situ keratomileusis keratectasia. J Cataract Refract Surg. 2004;30:1685–95. doi: 10.1016/j.jcrs.2004.02.050. [DOI] [PubMed] [Google Scholar]
- 29.Guüell JL, Velasco F, Saánchez SI, Gris O, Garcia-Rojas M. Intracorneal ring segments after laser in situ keratomileusis. J Refract Surg. 2004;20:349–55. doi: 10.3928/1081-597X-20040701-08. [DOI] [PubMed] [Google Scholar]
- 30.Kymionis GD, Siganos CS, Kounis G, Astyrakakis N, Kalyvianaki MI, Pallikaris IG. Management of post-LASIK corneal ectasia with Intacs inserts; One-year results. Arch Ophthalmol. 2003;121:322–6. doi: 10.1001/archopht.121.3.322. [DOI] [PubMed] [Google Scholar]
- 31.Siganos CS, Kymionis GD, Astyrakakis N, Pallikaris IG. Management of corneal ectasia after laser in situ keratomileusis with INTACS. J Refract Surg. 2002;18:43–6. doi: 10.3928/1081-597X-20020101-06. [DOI] [PubMed] [Google Scholar]
- 32.Lovisolo CF, Fleming JF. Intracorneal ring segments for iatrogenic keratectasia after laser in situ keratomileusis or photorefractive keratectomy. J Refract Surg. 2002;18:535–41. doi: 10.3928/1081-597X-20020901-08. [DOI] [PubMed] [Google Scholar]
- 33.Alioó JL, Salem TF, Artola A, Osman AA. Intracorneal rings to correct corneal ectasia after laser in situ keratomileusis. J Cataract Refract Surg. 2002;28:1568–74. doi: 10.1016/s0886-3350(01)01275-5. [DOI] [PubMed] [Google Scholar]
- 34.Piñero DP, Alio JL, Uceda-Montanes A, El Kady B, Pascual I. Intracorneal Ring Segment Implantation in Corneas with Post-Laser In Situ Keratomileusis Keratectasia. Ophthalmology. 2009;116:1665–74. doi: 10.1016/j.ophtha.2009.05.030. [DOI] [PubMed] [Google Scholar]
- 35.Piñero DP, Alió JL, El Kady B, Pascual I. Corneal aberrometric and refractive performance of 2 intrastromal corneal ring segment models in early and moderate ectatic disease. J Cataract Refract Surg. 2010;36:102–9. doi: 10.1016/j.jcrs.2009.07.030. [DOI] [PubMed] [Google Scholar]
- 36.Ertan A, Bahadir M. Management of superior pellucid marginal degeneration with a single intracorneal ring segment using femtosecond laser. J Refract Surg. 2007;23:205–8. doi: 10.3928/1081-597X-20070201-15. [DOI] [PubMed] [Google Scholar]
- 37.Ertan A, Bahadir M. Intrastromal ring segment insertion using a femtosecond laser to correct pellucid marginal corneal degeneration. J Cataract Refract Surg. 2006;32:1710–6. doi: 10.1016/j.jcrs.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 38.Mularoni A, Torreggiani A, Di Biase A, Laffi GL, Tassinari G. Conservative treatment of early and moderate pellucid marginal degeneration: A new refractive approach with intracorneal rings. Ophthalmology. 2005;112:660–6. doi: 10.1016/j.ophtha.2004.10.050. [DOI] [PubMed] [Google Scholar]
- 39.Barbara A, Shehadeh-Masha’our R, Zvi R, Garzozi HJ. Management of pellucid marginal degeneration with intracorneal ring segments. J Refract Surg. 2005;21:296–8. doi: 10.3928/1081-597X-20050501-15. [DOI] [PubMed] [Google Scholar]
- 40.Akaishi L, Tzelikis PF, Raber IM. Ferrara intracorneal ring implantation and cataract surgery for the correction of pellucid marginal corneal degeneration. J Cataract Refract Surg. 2004;30:2427–30. doi: 10.1016/j.jcrs.2004.04.047. [DOI] [PubMed] [Google Scholar]
- 41.Kymionis GD, Aslanides IM, Siganos CS, Pallikaris IG. Intacs for early pellucid marginal degeneration. J Cataract Refract Surg. 2004;30:230–3. doi: 10.1016/S0886-3350(03)00656-4. [DOI] [PubMed] [Google Scholar]
- 42.Rodriguez-Prats J, Galal A, Garcia-Lledo M, De la Hoz F, Alió JL. Intracorneal rings for the correction of pellucid marginal degeneration. J Cataract Refract Surg. 2003;29:1421–4. doi: 10.1016/s0886-3350(02)02038-2. [DOI] [PubMed] [Google Scholar]


