Abstract
Purpose:
To evaluate the visual and anatomic results and determine the prognostic factors after pars plana vitrectomy and posterior segment intraocular foreign body (IOFB) removal.
Materials and Methods:
This retrospective study reviews the patients’ charts of 48 consecutive patients with posterior segment IOFB who underwent pars plana vitrectomy and IOFB removal over a 4-year period, recently. Association between visual outcome and various preoperative, operative, and postoperative variables was statistically analyzed. Data were analyzed with the paired t-test and the chi square test. Statistical significance was indicated by P < 0.05.
Results:
The mean interval between the time of injury and IOFB removal was 24 ± 43.1 days and 27 (53%) eyes underwent IOFB removal within 7 days of the injury. Nine (19.1%) patients achieved a visual acuity of 20/40 or better. An improvement of visual acuity of at least three lines occurred in 21 (44.6%) eyes and the vision remained unchanged in 15 (31.9%) eyes. Postoperative retinal detachment occurred in five (10.6%) eyes. Visual improvement was more likely to occur in eyes with lower levels of presenting visual acuity (P = 0.2). Visual improvement was not associated with an entry site and IOFB location, lens injury, time to surgery, and pre- and post-operative retinal detachment. At the end of follow up, anatomical success was achieved in 97.9% of eyes.
Conclusions:
High anatomical success could be achieved after the removal of posterior segment IOFBs by vitrectomy, despite a delay in surgery. Poor visual outcome may be mainly due to the initial ocular injury.
Keywords: Intraocular Foreign Body, Parsplana Vitrectomy, Trauma
INTRODUCTION
Intraocular foreign body (IOFB) injuries are a relatively common form of ocular injury especially in young men.1,2 In addition to the initial damage, infection, and mechanical and chemical reactions are known complications of IOFBs. Several studies reported the outcome of parsplana vitrectomy (PPV) for posterior segment IOFBs.1,2,3,4,5,6,7,8 Recent advances in vitreoretinal surgical techniques, has suggested to improve the outcome of PPV in the management of posterior segment IOFBs.1,7,9
In this article, we present our experience with PPV for posterior segment IOFB removal during a recent period of 4 years.
MATERIALS AND METHODS
We retrospectively reviewed the medical charts of 48 consecutive patients who underwent surgery at our institution for posterior segment IOFBs over 4 years. The institutional review board of the Eye Research Center approved this study.
The following data were collected from the medical records: age and sex, time elapsed between initial injury and surgery, pre- and post-operative best corrected visual acuity (BCVA), details of the surgical procedures, size and location of the foreign body within the eye, pre- and postoperative status of the retina and surgical complications. Postoperative retinal detachment was considered an anatomic failure.
The surgical technique was a standard three port pars plana approach with simultaneous pars plana lensectomy or phacoemulsification when considered necessary. IOFB was removed by forceps or an intraocular magnet. We used liquid perfluorocarbon intraoperatively and sulfur hexafluoride (SF6) or silicone oil, as intraocular tamponade, if required. Endolaser photocoagulation of the breaks and 360° photocoagulation of the retinal periphery were performed.
Data were entered using Statistical Product and Service Solutions (SPSS) software version 15, (IBM Corp., Armonk, NY, USA). The paired t-test and the chi square test were performed for data analysis. A P value less than 0.05 was considered statistically significant.
RESULTS
Forty-five males and three females with a mean age of 31.7 ± 14.1 years were evaluated. Mean duration of follow up was 309 days. The mean interval between the time of injury and IOFB removal was 24 ± 43.1 days (range, 1 day to 240 days).
Intraoperatively, crystalline lens removal with or without intraocular lens insertion was performed in 31 eyes (64.5%) due to significant lens opacity. Before surgery, the retina was detached in 13 eyes; retinal reattachment surgery was unsuccessful in one eye. This eye underwent enucleation 2 weeks later; hence, the preoperative and postoperative comparison is limited to 47 eyes. Two of 13 eyes with retinal detachment developed postoperative detachment subsequently, and the presence of preoperative retinal detachment was not associated with postoperative retinal detachment (P = 0.2). Overall, 10 eyes required additional vitrectomy surgery: Five eyes for postoperative retinal detachment, four eyes for epiretinal membrane removal, and one eye for postoperative endophthalmitis. The retina was attached in all eyes at final visit. Penetrating keratoplasty was performed for two other eyes for corneal scar.
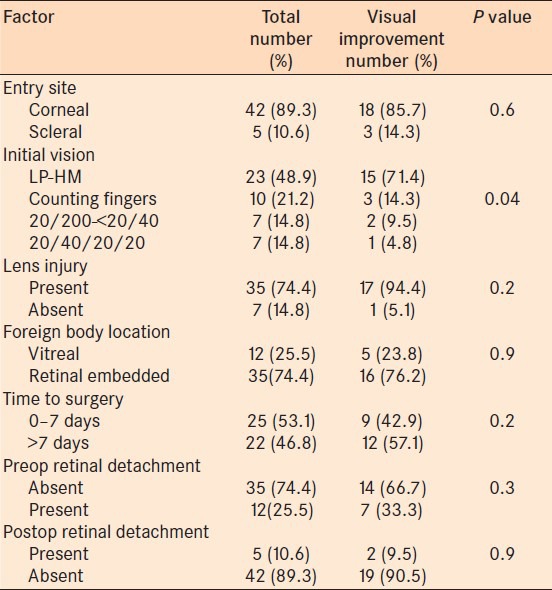
Presenting visual acuity of 2.01 ± 1.1 LogMAR improved to 1.7 ± 1.03 LogMAR at final visit (P = 0.1). Table 1 presents the initial and final visual acuities of the patients. Visual acuity improvement of at least three lines occurred in 21 (44.6%) eyes and the vision remained unchanged in 15 (31.9%) eyes. The variables studied, their frequency and the effect on visual outcome are summarized in Table 2. Preoperative visual acuity was the only variable, which was statistically significantly, associated with greater visual improvement; eyes with lower levels of preoperative visual acuity were more likely to improve postoperatively (P = 0.04). The reason for poor visual acuity was corneal scar secondary to the primary injury in the majority of eyes (42 eyes) with or without retinal injury from IOFB.
Table 1.
Preoperative and final visual acuity of patients who underwent surgery for intraocular foreign bodies
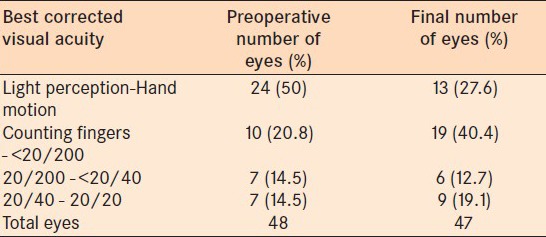
Table 2.
Effect of the study variables on postoperative visual improvement of at least 3 lines in patients who underwent surgery for intraocular foreign bodies
DISCUSSION
Microsurgical and vitreoretinal instrumentation and techniques, allows managing the posterior segment injuries associated with IOFBs successfully. It has been shown that vitreoretinal surgery is able to reduce the rate of visual loss.3,10 Many factors may affect the anatomic and functional success in PPV for IOFB. The properties and localization of the foreign body, interval between the injury and PPV, and primary ocular injuries associated with IOFB are the important prognostic factors.1,2,3,4,5,6,7,8,9,10
The incidence of infectious endophthalmitis after retaining an IOFB has been reported to be 0–13.5%.2 We had one case of endophthalmitis associated with IOFB in our series (2%). Several studies has shown that delayed removal of IOFB may end with poor visual and anatomical outcomes including the development of infectious endophthalmitis and retinal detachment.7,11,12 More recent studies have suggested that delayed IOFB removal may result in good visual outcome without an apparent increased risk of endophthalmitis or other complications.9,13,14,15,16 In our patients, the mean interval between trauma and PPV was 24 days, and the early surgery was not significantly associated with greater visual improvement. We usually perform pars plana vitrectomy soon after referral of the patients to our centre, and the mean interval of 24 days was due to the delay in patients’ presentation.
We found the preoperative level of visual acuity, as the only factor significantly related to the visual improvement. The majority of eyes (74.4%) had lens injury leading to lens removal in 64.5% of eyes. Also, preoperative retinal detachment was observed in 13 eyes (27%). Cataract surgery and retinal reattachment may be the reason for significant improvement in eyes with lower levels of preoperative visual acuity. We found a final visual acuity of 20/40 or better in 19.1% of eyes, which is lower than previous reports (23–71%).2,5 Our final anatomical success rate was 97.9%, so poor visual outcome may be attributable to the associated ocular injuries (e.g. corneal scar, retinal scar, etc).
In our study, preoperative retinal detachment was present in 25.5% of eyes; however, it was not a significant predictor of the development of a postoperative retinal detachment. It has been suggested that in the presence of a detached retina, surgical manipulations to remove the IOFB increase the risk of causing iatrogenic retinal breaks.17 Careful attention to the retina at the time of IOFB removal and the use of perfluorocarbon liquid for retinal protection may result in improved success rate. In our series, postoperative retinal detachment occurred in 10.6% of eyes. This rate ranges in the literature 6.3–36.8%.1,18 Some studies reported that retinal detachment after posterior segment IOFB injuries is associated with a poor visual outcome.18,19 We, however, did not observe such an association in our series.
The limitations of our study include the retrospective nature and small sample size of the study, and short follow up period in some eyes may preclude definite conclusion. Despite these limitations, our results show that the anatomical outcome of PPV for eyes with posterior segment IOFB in terms of retinal attachment is adequate; however, associated ocular injuries may limit visual improvement.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Yeha S, Colyerb MH, Weichel ED. Current trends in the management of intraocular foreign bodies. Curr Opin Ophthalmol. 2008;19:225–33. doi: 10.1097/ICU.0b013e3282fa75f1. [DOI] [PubMed] [Google Scholar]
- 2.Mester V, Kuhn F. Intraocular foreign bodies. Ophthalmol Clin North Am. 2002;15:235–42. doi: 10.1016/s0896-1549(02)00013-5. [DOI] [PubMed] [Google Scholar]
- 3.Williams DF, Mieler WF, Abrams GW, Lewis H. Results and prognostic factors in penetrating ocular injuries with retained intraocular foreign bodies. Ophthalmology. 1988;95:911–6. doi: 10.1016/s0161-6420(88)33069-1. [DOI] [PubMed] [Google Scholar]
- 4.Ahmadieh H, Sajjadi H, Azarmina M, Soheilian M, Mahavrivand N. Surgical management of intraretinal foreign bodies. Retina. 1994;14:397–403. doi: 10.1097/00006982-199414050-00002. [DOI] [PubMed] [Google Scholar]
- 5.El-Asrar AM, Al-Amro SA, Khan NM, Kangave D. Visual outcome and prognostic factors after vitrectomy for posterior segment foreign bodies. Eur J Ophthalmol. 2000;10:304–11. doi: 10.1177/112067210001000406. [DOI] [PubMed] [Google Scholar]
- 6.Lam SR, Devenyi RG, Berger AR, Dunn W. Visual outcome following penetrating globe injuries with retained intraocular foreign bodies. Can J Ophthalmol. 1999;34:389–93. [PubMed] [Google Scholar]
- 7.Jonas JB, Knorr HL, Budde WM. Prognostic factors in ocular injuries caused by intraocular or retrobulbar foreign bodies. Ophthalmology. 2000;107:823–8. doi: 10.1016/s0161-6420(00)00079-8. [DOI] [PubMed] [Google Scholar]
- 8.Tomic Z, Pavlovic S, Latinovic S. Surgical treatment of penetrating ocular injuries with retained intraocular foreign bodies. Eur J Ophthalmol. 1996;6:322–6. doi: 10.1177/112067219600600317. [DOI] [PubMed] [Google Scholar]
- 9.Wani VB, Al-ajmi M, Thalib L. Vitrectomy for posterior segment intraocular foreign bodies, visual results and prognostic factors. Retina. 2003;23:654–60. doi: 10.1097/00006982-200310000-00008. [DOI] [PubMed] [Google Scholar]
- 10.Chow DR, Garretson BR, Kuczynski B, Williams GA, Margherio R, Cox MS, et al. External versus internal approach to the removal of metallic intraocular foreign bodies. Retina. 2000;20:364–69. doi: 10.1097/00006982-200007000-00007. [DOI] [PubMed] [Google Scholar]
- 11.Thompson JT, Parver LM, Enger CL, Mieler WF, Liggett PE. Infectious endophthalmitis after penetrating injuries with retained intraocular foreign bodies. National Eye Trauma System. Ophthalmology. 1993;100:1468–74. doi: 10.1016/s0161-6420(93)31454-5. [DOI] [PubMed] [Google Scholar]
- 12.Chaudhry IA, Shamsi FA, Al-Harthi E, Al-Theeb A, Elzaridi E, Riley FC. Incidence and visual outcome of endophthalmitis associated with intraocular foreign bodies. Graefe's Arch Clin Exp Ophthalmol. 2008;246:181–6. doi: 10.1007/s00417-007-0586-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Woodcock MG, Scott RA, Huntbach J, Kirkby GR. Mass and shape as factors in intraocular foreign body injuries. Ophthalmology. 2006;113:2262–9. doi: 10.1016/j.ophtha.2006.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Colyer MH, Weber ED, Weichel ED, Dick JS, Bower KS, Ward TP, et al. Delayed intraocular foreign body removal without endophthalmitis during operations Iraqi freedom and enduring freedom. Ophthalmology. 2007;114:1439–47. doi: 10.1016/j.ophtha.2006.10.052. [DOI] [PubMed] [Google Scholar]
- 15.Bai H, Yao L, Meng X, Wang YX, Wang DB. Visual outcome following intraocular foreign bodies: A retrospective review of 5-year clinical experience. Eur J Ophthalmol. 2011;21:98–103. doi: 10.5301/ejo.2010.2210. [DOI] [PubMed] [Google Scholar]
- 16.Ferrari TM, Cardascia N, Di Gesu I, Catella N, Recchimurzo N, Boscia F. Early versus late removal of foreign bodies. Retina. 2001;21:92–3. doi: 10.1097/00006982-200102000-00026. [DOI] [PubMed] [Google Scholar]
- 17.Erakgun T, Egrilmez S. Prognostic factors in vitrectomy for posterior segment intraocular foreign bodies. J Trauma. 2008;64:1034–7. doi: 10.1097/TA.0b013e318047dff4. [DOI] [PubMed] [Google Scholar]
- 18.Wickham L, Xing W, Bunce C, Sullivan P. Outcomes of surgery for posterior segment intraocular foreign bodies-a retrospective review of 17 years of clinical experience. Graefes Arch Clin Exp Ophthalmol. 2006;244:1620–6. doi: 10.1007/s00417-006-0359-6. [DOI] [PubMed] [Google Scholar]
- 19.El-Asrar AMA, Al-Amro SA, Khan NM, Kangave D. Retinal detachment after posterior segment intraocular foreign body injuries. Int Ophthalmol. 1998;22:369–75. doi: 10.1023/a:1006469705126. [DOI] [PubMed] [Google Scholar]


