Abstract
Background:
Hyperbaric ropivacaine produce more reliable sensory and motor block, with faster onset, better quality of muscles relaxation than isobaric ropivacaine. So, this study was designed to compare the efficacy of hyperbaric ropivacaine with isobaric ropivacaine in patients undergoing lower abdominal surgery.
Methods:
A randomized controlled double blind study in two groups of patients. group A (n=35) received 3 ml of isobaric ropivacaine 6 mg/ml (18 mg). Group B (n=35) received 3 ml of hyperbaric ropivacaine 6 mg/ml (18 mg). The onset and duration of sensory block at dermatome level T10, maximum upper and lower spread of sensory block, intensity, and duration of motor block were recorded.
Statistical Analysis:
Block characteristics were compared using the two-tailed Mann – Whitney U-test. The proportion of side effects was compared using the Chi-square test.
Results:
The median time of onset of sensory block at the T10 dermatome was 4.4±1.3 min in group B and 6.0±1.03 min in group A. The median time to maximum block height was 16.7±3.7 min in group A and 12.03±1.96 min in group B. The median duration of complete motor recovery (B0) was significantly shorter in the heavy ropivacaine group (166.5±11.7 min) compared with the isobaric ropivacaine group (192.9±9.6 min).
Conclusions:
Intrathecal hyperbaric ropivacaine provides more rapid, adequate, and good quality of sensory and motor block with rapid post-operative recovery as compare to isobaric ropivacaine.
Keywords: Hyperbaric ropivacaine, intrathecal injection, isobaric ropivacaine, lower abdominal surgery
INTRODUCTION
Spinal anesthesia is a common safe, economical, easy to perform and effective technique which provides rapid and reliable anesthesia with muscle relaxation for patients undergoing lower abdominal surgery.[1,2] Various local anesthetic commonly used for spinal anesthesia are lignocaine, bupivacaine, levobupivacaine, and ropivacaine.[3,4] Nowadays, ropivacaine is gaining increasing popularity because of reduced risk of central nervous system and cardiac toxicity, early ambulation and discharge with good quality of post-operative analgesia.[5] Ropivacaine is the pure S(−) enantiomer of ropivacaine, new long-acting amino amide with lower lipid solubility, produces variable sensory and motor block when it is given in isobaric form while hypothetically, hyperbaric ropivacaine produced more reliable sensory and motor block, with faster onset, better quality of muscles relaxation than isobaric ropivacaine. Therefore, this prospective, randomized, double-blind study was designed to compare isobaric with hyperbaric ropivacaine for spinal anesthesia in patients undergoing lower abdominal surgery. Our primary outcomes of the study are the onset of the sensory and motor blockade and hemodynamic, secondary outcome are regression of sensory and motor blockade, duration of analgesia, visual analog scale (VAS), side effects, patients, and surgeon satisfaction.
METHODS
A randomized controlled double-blind study was performed after obtaining the approval of the Ethical Committee of the institution, 70 ASA Grade I-II patients who were to undergo elective lower abdominal surgery under spinal anesthesia gave written informed consent to take part in the study. Patients were randomized into two groups (n=35 in each group) using a computer generated random number tables. These groups were further classified, based on the intrathecal drug combination used.
Group A: 18 mg 0.6% isobaric ropivacaine.
Group B: 18 mg 0.6% hyperbaric ropivacaine.
The patients were explained about the intrathecal use of drug, and written informed consent was taken. Patients and anesthetist who recorded the data were not aware of the drug combination, nor the doctors who prepared the drug knew which group of drug they received for spinal anesthesia. Exclusion criteria were patient refusal, any contraindication for spinal anesthesia, patients with previous abdominal surgeries, known drug allergy, patients having a body weight >70 kg. All Patients were nil per orally for 6 h, pre-medicated with oral ranitidine 150 mg, alprax 0.25 mg, and metoclopramide 10 mg the night before and on the morning of surgery, patients were preloaded with 10-15 ml/kg body of ringer lactate via 18 gauge venous catheters. Baseline standard monitoring included continuous electrocardiogram, pulse oximetry, non-invasive blood pressures and urine output. Sensory and motor assessment methods were described in all patients before the start of anesthesia. The solution was prepared aseptically by the anesthetist, by mixing ropivacaine 7.5 mg/ml (4 ml) with 25% dextrose (1 ml) to obtain a total volume of 5 ml, each ml contained ropivacaine 6 mg and glucose 50 mg to give solutions a density of 1.01949 g at 37°C.[6] Spinal anesthesia was given in left lateral position between L3 and L4 vertebrae using 25 gauge Whitacre needle taking complete aseptic precautions. In group A, intrathecal isobaric ropivacaine (18 mg) and in group B, intrathecal hyperbaric ropivacaine (18 mg) was given over 10-15 s. Noninvasive blood pressure pulse and oxygen saturation were measured every 5 min for first 30 min and thereafter every 10 min. Patients were given supplementary O2 with the help of venturi mask if oxygen saturation dropped ≤92%. Sensory block was tested by cold, touch, and pinprick along the midclavicular line till the block reached T6 level and then the surgical incision was allowed.[7] Motor block using a modified Bromage Scale (0=no block, 1=inability to raise extended leg, 2=inability to flex knee, and 3=inability to flex ankle and foot) was also recorded at the 5, 10, 15, 20, 25, and 30 min.[8] The following variables were recorded: time to an initial onset of analgesia, highest level of sensory analgesia, the time to complete motor block, time to two-segment regression of analgesic level, regression of analgesic level to S1 dermatome, motor recovery (ability to move lower limbs), and first request for analgesic. The total duration of analgesia was considered from the time of injection of spinal anesthetic, until the first request for analgesic by the patient. The surgical anesthesia was graded by anesthetist as “excellent” – if there were no complaints from patient or surgeon, “good” – if there was a complaint of pain, which was relieved by IV opioid analgesics and “poor” – if more than one dose of analgesic or rescue general analthesia (GA) was required.[9] Hypotension (defined as systolic arterial pressure falling more than 20%) was treated with injection ephedrine 6 mg in bolus doses and heart rate <55 beats/min was treated with 0.4 mg of injection atropine. Intravenous fluids were given as per operative loss with blood transfusion if required. During the surgical procedure, side effects like sedation, nausea, vomiting, shivering, bradycardia or hypotension was recorded. Nausea and vomiting were treated with 4-6 mg of i.v. ondansetron. Urinary bladder was catheterized in all patients before the start of surgery, until 24 h post-operatively. VAS score between 0 and 10 (0=no pain, 10=the most severe pain) was used for post-operative pain analysis at every 4 h until 24 h.[10] Injection paracetamol 15 mg/kg intravenous was given as rescue analgesia when VAS ≥4. Follow-up was carried out for 1 week post-operatively by the blinded anesthetist who asked about post-operative headache as well as post-operative pain and dysesthesia in the buttock, thighs, or lower limbs. Supplementation of some analgesia and sedation was given such as ketamine, midazolam, and fentanyl during the perioperative period if required.
Statistical analysis
The collected data were analyzed by using statistical software namely statistical product and service solutions (SPSS) 15.0. The sample size determination was based on α risk of 0.05 and β risk of 0.10 which showed that 30 patients per study groups were needed. Data are presented as median (range), mean (SD), or frequencies as appropriate.[11,12] Block characteristics were compared using the two-tailed Mann – Whitney U-test. A P value of<0.05 was considered statistically significant. The proportion of side effects was compared using the Chi-square test (χ2 =57.24, 10) and statistical significance was observed at P<0.001.
Power analysis
Statistical power was calculated to be 99.9% for motor and sensory block period as α=0.05 and β=0.001.
RESULTS
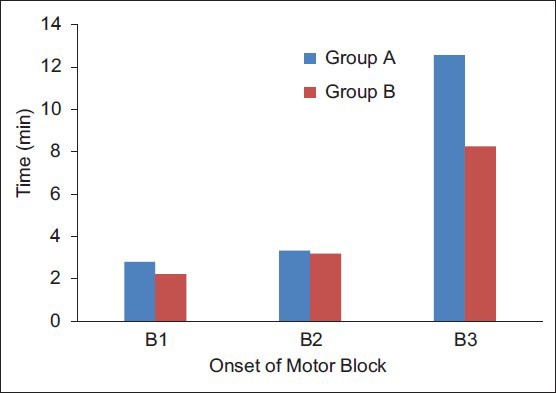
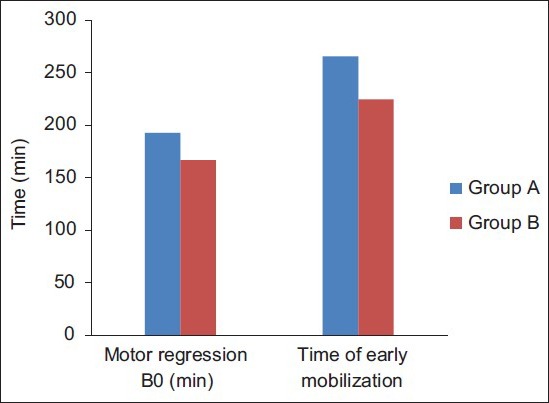
The groups were comparable with respect to age, height, weight, sex, and ASA status [Table 1]. After randomization and a lumbar puncture, five patients from group A and two patients from group B were withdrawn because of total block failure (no muscle weakness or loss of sensation) and given a general anesthetic, so leaving 30 patients in group A and 33 patients in group B. There was no difference in the type of surgery, although its duration was somewhat longer in the group A (50.8±10.2) as compared to group B (45.5±15.5) [Table 1]. Hyperbaric ropivacaine produced a more rapid onset of sensory block, which, ultimately regressed more quickly. The onset of analgesia to pinprick at T10 was more rapid in group B (4.43±1.33) as compared to group A (6.0±1.03), and the maximum block height T4 (T3-T6) was greater in group B, as compared to group A with T5 (T4-T6) [Table 2]. Median time to maximum block height was the earliest in group B (10.03±1.22), as compared to group A (14.2±1.51) [Table 2]. The onset of motor block B1, B2, and B3 was slightly faster in the hyperbaric group, as compared with the isobaric solution [Table 2 and Figure 1]. Median time to two segment regression of sensory block to T10 was longer in the hyperbaric group (66.54±10.25) as compared to isobaric group (48.14±5.26), but median times to complete regression of both sensory and motor block (B0) were longer in the isobaric group (192.49±9.60) as compared to hyperbaric group (166.57±11.71) [Table 2 and Figure 2]. Patients mobilized sooner in the group B (224.26±11.41) as compared to group A (265.26±12.86) [Table 2 and Figure 2]. Patients of hyperbaric blocks were adequate for surgery while two patients required general anesthesia due to surgical complication, five patients (two patients blocks were not extensive enough and in three patients became inadequate 20 min after the start of surgery) who received isobaric ropivacaine required general anesthesia. Patients of both groups were hemodynamically stable throughout the surgery, group B showed a mean heart rate (72.11±5.75) and a mean blood pressure (82.17±4.98) as compared to group A showed a heart rate (78.2±5.29) [Figure 3] and a mean blood pressure (85.14±5.32) [Figure 4]. Doses of ephedrine administered were more in group B (14±6) as compared to group A (8±4). Supplementation of midazolam (1.8±0.6) mg, ketamine (30.8±8.6) mg, and fentanyl (50.5±10.8) mcg were required in the isobaric group for completion of surgery, while patients of hyperbaric group did not require any analgesic and/or sedative for completion of surgery. The surgical anesthesia was graded by anesthetist as “excellent” in hyperbaric group and “Good” in isobaric group. There were no major sequelae in both the groups.
Table 1.
Patient characteristics
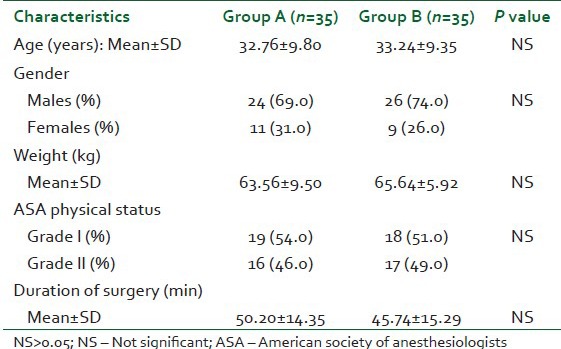
Table 2.
Block characteristics
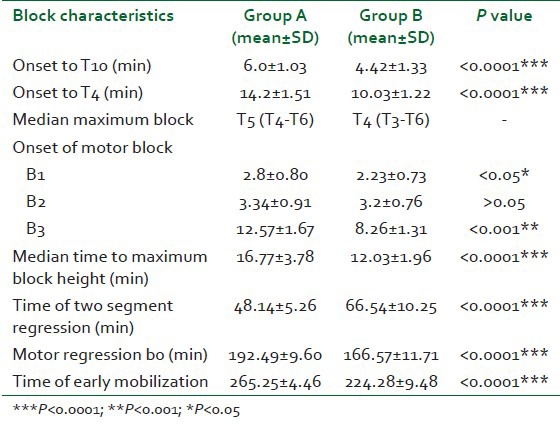
Figure 1.
Onset of motor block
Figure 2.
Motor regression and mobilization
Figure 3.
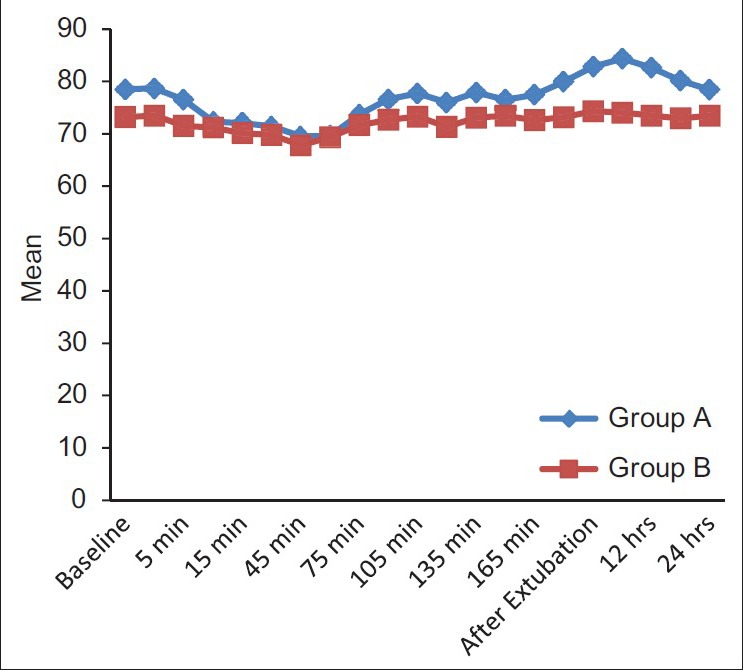
Heart rate summary
Figure 4.
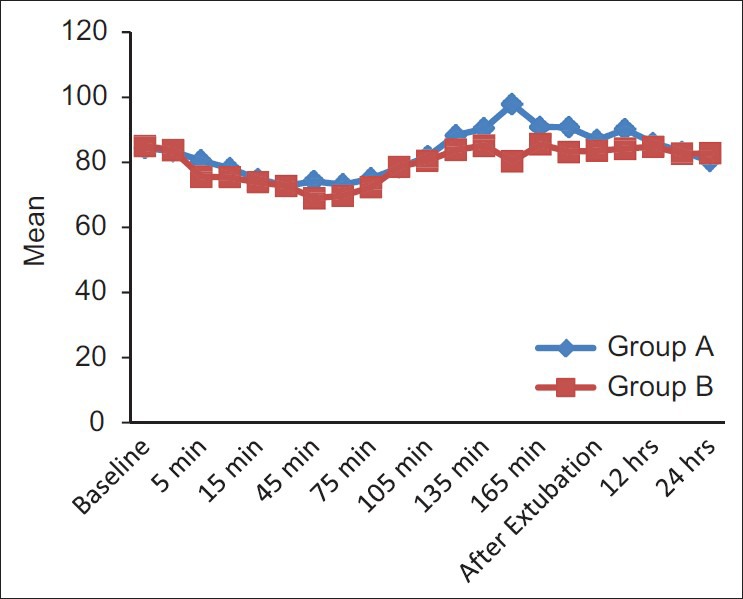
Mean blood pressure summary
DISCUSSION
This prospective randomized, double blind comparative study was conducted between hyperbaric ropivacaine and isobaric ropivacaine for lower abdominal surgeries. Our study showed that hyperbaric solution of ropivacaine produces a more reliable block than an isobaric one. Addition of glucose to isobaric ropivacaine led to a more rapid onset, more dense motor blockade, increase the level of block with early post-operative mobilization and rehabilitation as compared to isobaric ropivacaine. The addition of glucose 50 mg/ml to ropivacaine causes earlier onset of the block, good quality with adequate duration, and increase the recovery. Isobaric solutions was not reliable for abdominal surgery.[13]
Addition of glucose to isobaric ropivacaine increases its density that result in an equal distribution of the drug and increase height of the block while isobaric ropivacaine produces less intense, unpredictable, and variable height of block, therefore, patient of isobaric group felt some discomfort during surgery so supplementation of analgesia and sedation were required such as ketamine, midazolam, and fentanyl in a few patients in our study. Kallio et al.[14] also found analgesic effect in 64% (18/28) patients in the isobaric group while good quality of anaesthesia was found in all patients of hyperbaric group.
This study shows that hyperbaric ropivacaine, in a dose of 18 mg, produces predictable and reliable spinal anaesthesia for lower abdominal surgeries of relatively longer duration as compared to isobaric ropivacaine. Yegin et al.[15] studied effect of hyperbaric ropivacaine in a dose of 18 mg and compared with hyperbaric ropivacaine 18 mg and fentanyl 25 μg in trans urethral resection prostate (TURP) surgery and found similar effect in onset and duration of sensory and motor effect except for prolonged analgesic effect in fentanyl group. In the comparison of the isobaric solutions of ropivacaine, the hyperbaric preparation produced a higher, more consistent block with faster onset and recovery, whereas there was a failure rate with the isobaric solution,[13] similar result was noted by Hocking and Wildsmith.[16] While variability in a spread can be minimized by adding glucose, the variable response of isobaric ropivacaine should always consider. The spread of isobaric ropivacaine is dependent on the current produced by injection and simple diffusion. So that the drug, which we inject through intrathecal route stays locally at the point of injection, so quality of the block is not reliable for abdominal surgery but prolong effect was observed in lower limbs due to dense effects on lumber and sacral nerve.[13] Our study also shows variable response during lower abdominal surgery with isobaric ropivacaine and required some supplementation of analgesic and sedative agent for good quality of surgical relaxation. In our previous study in which we studied isobaric ropivacaine for lower limb surgery and found the best quality of prolonged analgesic effects which justified dense effect of isobaric ropivacaine on lumber and sacral plexus.[12] In the earlier time lidocaine was the standard agent for a short duration of surgery, but this drug is now not used because of the high incidence of transient neurological symptoms.[16,17] So the currently ropivacaine is of great choice for short duration of surgery.
CONCLUSION
Hyperbaric ropivacaine produced more consistent, reliable and good quality of sensory and motor block, with faster onset, early mobilization and rehabilitation than an isobaric ropivacaine, which is required for day-case surgery in which prolong immobilization is undesirable. Isobaric ropivacaine did not provide good quality of motor blockade it required some additional analgesic and sedative agent for completion of the surgery. We, therefore, conclude that isobaric ropivacaine are very good for lower limb surgery. However, further studies are necessary to evaluate the role of hyperbaric ropivacaine in comparison to isobaric ropivacaine for surgical procedures of short-duration, particularly in the day case surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.O’Connor PJ, Hanson J, Finucane BT. Induced hypotension with epidural/general anesthesia reduces transfusion in radical prostate surgery. Can J Anaesth. 2006;53:873–80. doi: 10.1007/BF03022829. [DOI] [PubMed] [Google Scholar]
- 2.van Kleef JW, Veering BT, Burm AG. Spinal anesthesia with ropivacaine: A double-blind study on the efficacy and safety of 0.5% and 0.75% solutions in patients undergoing minor lower limb surgery. Anesth Analg. 1994;78:1125–30. [PubMed] [Google Scholar]
- 3.Lim Y, Ocampo CE, Sia AT. A comparison of duration of analgesia of intrathecal 2.5 mg of bupivacaine, ropivacaine, and levobupivacaine in combined spinal epidural analgesia for patients in labor. Anesth Analg. 2004;98:235–9. doi: 10.1213/01.ANE.0000094338.80430.C5. [DOI] [PubMed] [Google Scholar]
- 4.Casati A, Moizo E, Marchetti C, Vinciguerra F. A prospective, randomized, double-blind comparison of unilateral spinal anesthesia with hyperbaric bupivacaine, ropivacaine, or levobupivacaine for inguinal herniorrhaphy. Anesth Analg. 2004;99:1387–92. doi: 10.1213/01.ANE.0000132972.61498.F1. [DOI] [PubMed] [Google Scholar]
- 5.Sultan MA, Ali Shams TM, Mageed NA, El-ebidy MG. Intrathecal hyperbaric ropivacaine versus hyperbaric bupivacaine in geriatric hypertensive patients. Benha M. J. 2005;22:479. [Google Scholar]
- 6.Hocking G, Wildsmith JA. Intrathecal drug spread. Br J Anaesth. 2004;93:568–78. doi: 10.1093/bja/aeh204. [DOI] [PubMed] [Google Scholar]
- 7.Chung CJ, Choi SR, Yeo KH, Park HS, Lee SI, Chin YJ. Hyperbaric spinal ropivacaine for cesarean delivery: A comparison to hyperbaric bupivacaine. Anesth Analg. 2001;93:157–61. doi: 10.1097/00000539-200107000-00031. [DOI] [PubMed] [Google Scholar]
- 8.Bromage PR. Philadelphia: WB Saunders; 1978. Epidural analgesia; p. 144. [Google Scholar]
- 9.Gupta R, Bogra J, Verma R, Kohli M, Kushwaha JK, Kumar S. Dexmedetomidine as an intrathecal adjuvant for postoperative analgesia. Indian J Anaesth. 2011;55:347–51. doi: 10.4103/0019-5049.84841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gould D. Visual analogue scale. J Clin Nurs. 2001;10:697–706. doi: 10.1046/j.1365-2702.2001.00525.x. [DOI] [PubMed] [Google Scholar]
- 11.Murphy KR, Myors B. 2nd ed. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. The power of statistical tests. Statistical Power Analysis: A Simple and General Model for Traditional and Modern Hypothesis Tests; pp. 1–21. [Google Scholar]
- 12.Gupta R, Verma R, Bogra J, Kohli M, Raman R, Kushwaha JK. A comparative study of intrathecal dexmedetomidine and fentanyl as adjuvants to bupivacaine. J Anaesthesiol Clin Pharmacol. 2011;27:339–43. doi: 10.4103/0970-9185.83678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fettes PD, Hocking G, Peterson MK, Luck JF, Wildsmith JA. Comparison of plain and hyperbaric solutions of ropivacaine for spinal anaesthesia. Br J Anaesth. 2005;94:107–11. doi: 10.1093/bja/aei008. [DOI] [PubMed] [Google Scholar]
- 14.Kallio H, Snäll EV, Tuomas CA, Rosenberg PH. Comparison of hyperbaric and plain ropivacaine 15 mg in spinal anaesthesia for lower limb surgery. Br J Anaesth. 2004;93:664–9. doi: 10.1093/bja/aeh257. [DOI] [PubMed] [Google Scholar]
- 15.Yegin A, Sanli S, Hadimioglu N, Akbas M, Karsli B. Intrathecal fentanyl added to hyperbaric ropivacaine for transurethral resection of the prostate. Acta Anaesthesiol Scand. 2005;49:401–5. doi: 10.1111/j.1399-6576.2005.00607.x. [DOI] [PubMed] [Google Scholar]
- 16.Hocking G, Wildsmith JA. Intrathecal drug spread. Br J Anaesth. 2004;93:568–78. doi: 10.1093/bja/aeh204. [DOI] [PubMed] [Google Scholar]
- 17.Schneider M, Ettlin T, Kaufmann M, Schumacher P, Urwyler A, Hampl K, et al. Transient neurologic toxicity after hyperbaric subarachnoid anesthesia with 5% lidocaine. Anesth Analg. 1993;76:1154–7. doi: 10.1213/00000539-199305000-00044. [DOI] [PubMed] [Google Scholar]


