Abstract
Background:
Endoscopic retrograde cholangiopancreatography (ERCP) is a unique diagnostic and therapeutic procedure performed in high risk patients in prone/semi-prone position. Propofol based deep sedation has emerged as the method of choice however, the ability to predict possible complications is yet un-explored.
Aims:
The present study aimed to evaluate known high risk-factors for general anesthesia (American Society of Anesthesiologists (ASA) status, body mass index (BMI), and Mallampati class) for their ability to affect outcomes in ERCP patients.
Study Design:
Retrospective data of 653 patients who underwent ERCP during a period of 26 months at university hospital of Pennsylvania was reviewed. Patient-specific and procedure specific data was extracted. Desaturation was defined by fall of pulse oximeter saturation below 95% and its relation to patient specific high risk-factors was analyzed.
Results:
Only 45 patients had transient de-saturation below 95% without any residual sequlae. No statistically significant relation between desaturation episodes and patients higher ASA status or BMI or modified Mallampati (MMP) class was found. Despite 60% patients being ASA III/IV none required emergency intubation or procedural interruption. Optimal oxygenation and airway patency was maintained with high degree of success using simple airway maneuvers or conduit devices (nasal/oral trumpet) with oxygen supplementation in all patients.
Conclusions:
Unlike general anesthesia, pre-operative patient ASA status, higher MMP or increasing BMI does not bear relation with likelihood of patients desaturating during ERCP. In presence of vigilant apnea monitoring and careful dose titration of maintenance anesthetics with airway conduits, general anesthesia, emergency intubations, and procedure interruptions can be avoided.
Keywords: Airway in endoscopic retrograde cholangiopancreatography, endoscopic retrograde cholangiopancreatography anesthesia, endoscopic retrograde cholangiopancreatography desaturation, risk predictors endoscopic retrograde cholangiopancreatography
INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) is a common diagnostic and therapeutic procedure differing from other gastrointestinal endoscopic procedures in terms of anesthetic requirements. ERCP procedures, when compared to open surgical procedures are significantly less painful and despite being performed in prone/semi-prone position, do not need paralysis or endotracheal intubation. Patients planned for ERCP often have additional comorbidities that make them high-risk candidates for general anesthesia. Additional airway interventions, apart from slowing the turn over time, can also add to poorer outcome. In the absence of sufficient literature on the anesthesia techniques for ERCP, patients are often subject to endotracheal intubation. Apart from requiring higher anesthetic doses that raise direct costs, this approach also increases risks and duration of the procedure with no apparent change in patient outcome or procedural safety. Theoretically, unlike other procedures done under sedation or general anesthesia, carbon dioxide insufflation of the stomach and intestines during ERCP in prone position can predispose to higher risk of aspiration[1] and vagally mediated hypotension.[2] Previous literature on monitored anesthesia care under sedation advocates the use of endotracheal intubation with general anesthesia in high risk (higher American Society of Anesthesiologists (ASA) grade and obese) patients, however, our experience of maintaining natural open airway over the years has proved to be safe and efficient both for procedural success and safety. There is no conclusive data to support or refute the need for endotracheal intubation during ERCP. Having known that our practice of not intubating these patients, yet maintaining airway patency without any apparent complications, we decided to retrospectively study the anesthesia records to analyze the safety and efficiency of our anesthetic practice.
METHODS
Study design
After approval by the Institutional Review Board of the University of Pennsylvania, we used a retrospective explorative study design. In our gastroenterology suite an anesthesiologist (physician) supervises up to three anesthetizing locations at a time including ERCPs. All cases are anesthetized by a certified registered nurse anesthetist (CRNA) regularly involved in procedures under sedation. The anesthetic charting is carried out on a paper and the vitals are also printed from the computerized monitoring system at the end of the case. Anesthesia and perioperative records of all patients who underwent ERCP from 13-7-2009 to 23-9-2011 were reviewed to obtain the following patient-specific and procedure specific data: Demographic profile and comorbidities (ASA grade) airway evaluation, indication of ERCP, method of airway management, minimal oxygen saturation during the procedure, cardiovascular complications, unexpected endoscope withdrawal to facilitate patients’ oxygenation, duration of procedure, and any procedure cancellation after start of the procedure due to anesthesia issues. Special attention was paid to record the need for emergency airway management and any anesthesia related immediate complications during the ERCP.
As a routine protocol, all patients prior to ERCP underwent a detailed pre-anesthetic assessment as per ASA guidelines. Prior to induction, all patients received 100% oxygen by breathing into a tightly held inflatable face mask of appropriate size. High flow oxygen (12-15 l/min) was administered through a Mapelson C breathing system. The administration of high-flow oxygen not only helped to increase oxygen saturation to 100% irrespective of baseline room air saturation, but also allowed to tide over 1-2 min of apnea soon after induction without any desaturation. This period was used for insertion of both nasal trumpet and endoscope insertion (which also allowed restoration of sufficient spontaneous ventilation). ERCP was performed in semi-prone position and besides routine hemodynamic monitoring (continuous Electrocardiogram, intermittent 5 min interval-automated non-invasive blood pressure), possible apnea during the procedure was monitored using end tidal CO2, impedance pneumogram, and (or) acoustic respiratory monitor along with a vigilant visual assessment of chest excursion.
Anesthesia was induced using titrated doses of propofol (0.5 mg-1.5 mg/kg) and fentanyl (25-50 μg initially for an adult) to carefully maintain spontaneous breathing yet allowing maneuvers (airway insertion etc.) to maintain airway patency. Once, adequate jaw relaxation was achieved the endoscopy probe was inserted. Maintenance of anesthesia was carried out using propofol infusion usually between 80-120 mcg/kg/min along with combination of fentanyl (supplements of 25-50 μg) or remifentanyl (as a mixture with propofol at 5 μg/cc of propofol). For patients receiving propofol, remifentanyl mixture, fentanyl was not administered. Furthermore, this mixture was never used as a bolus due to higher incidence of apnea. The duration of the procedure was varied, with some procedures (like stent change or stent removal) being very short. On completion of the procedure, patients were transferred to a dedicated recovery room and monitored till they were ready to be discharged.
Data analysis
The data obtained was analyzed using SPSS Version 20 (IBM Inc. Chicago, USA) for Macintosh. Descriptive statistics were used for variables involving patient demography, surgery indication, airway device, and duration. Desaturation was defined as pulse oximeter saturation ≤95%. The level of statistical significance was set at P<0.05 and association between desaturation and ASA grade, body mass index (BMI), and modified Mallampati (MMP) class was derived using non-parametric Pearson's Chi-square test.
RESULTS
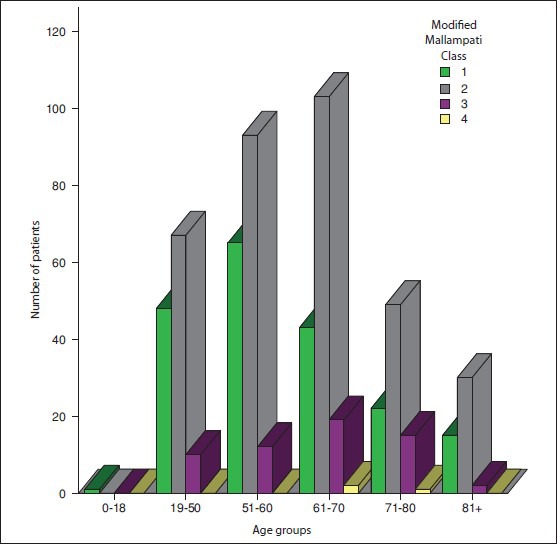
A total of 653 patients underwent ERCP under sedation during the selected span of 26 months. The mean age of patients was 60.5±14.18 years (range 18-97) with 420 (64.3%) males and 233 (35.6%) females. The commonest indications for ERCP in our out-patient facility were post-hepatic transplant, carcinoma of pancreas, chronic pancreatitis and primary sclerosing cholangitis (in decreasing order) [Table 1]. Patient specific demographic parameters and pre-anesthetic evaluation (age distribution, BMI, MMP classification (airway) and ASA stratification) are shown in Table 2, ASA stratification, MMP, and BMI data based on age distribution is represented in Table 2, Figures 1-3. Multiple patients had systemic comorbidities involving cardio-respiratory system; the frequency and ailments are represented in Table 3. All patients were induced using propofol and the frequency of patients maintained on propofol infusion in combination with remifentanyl, fentanyl or ketamine is shown in Table 4a. No patient required emergency intubation during the procedure and airway was maintained using nasal/oral trumpet with oxygen supplementation and sometimes aided by simple airway maneuvers [Table 4b]. The nurse anesthetist guided the method of airway maintenance on patient-to-patient basis in consultation with the supervising anesthesiologist. Minimum documented pulse oximeter saturation data was available for 651 patients and 45 (6.9%) patients showed transient desaturation as per above defined cut off. No specific time or procedure phase was found related to desaturation episode. Mean pulse oximetry oxygen saturation was 99.01±2.152 (range 60-100%) with only three patients transiently desaturating below 90%. The mean duration of procedure as defined by induction to final shifting of patient to recovery room was 54.89±24.30 (range 10-208) min.
Table 1.
Indications of endoscopic retrograde cholangiopancreatography
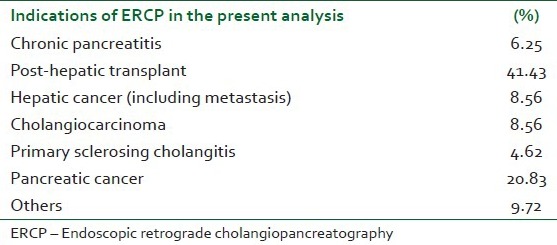
Table 2.
Patient specific data (body mass index, airway and anesthesia classification)
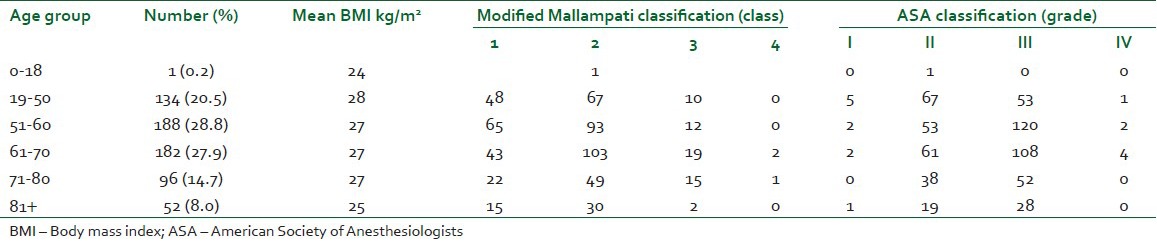
Figure 1.
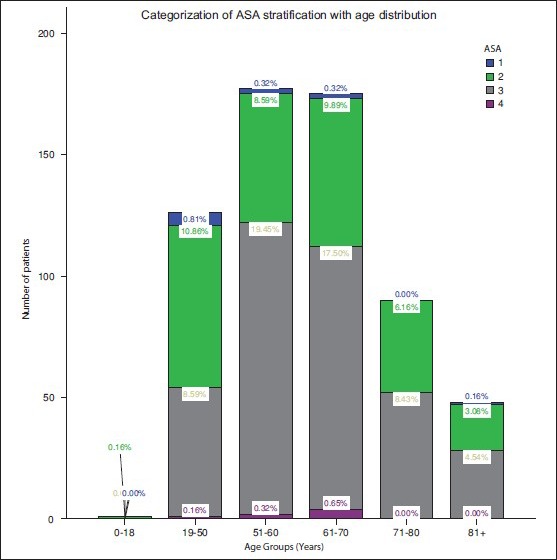
Age distribution and American Society of Anesthesiologists status of patients
Figure 3.
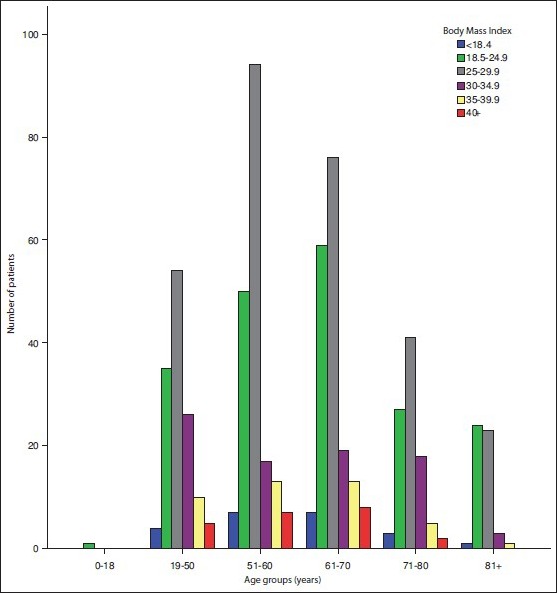
Distribution of body mass index of patients
Table 3.
Specific systemic comorbidities
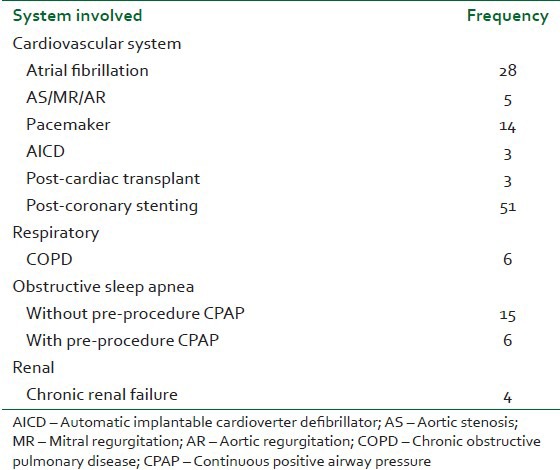
Table 4a.
Number of patients and anesthetics used
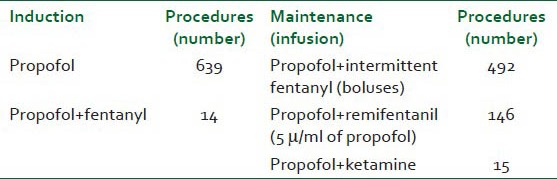
Table 4b.
Number of patients and anesthetics used
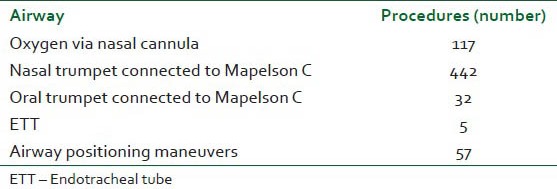
Figure 2.
Modified Mallampati score and age distribution of patients
No statistically significant association was found by Pearson's Chi-square test between number of patients desaturating and – increasing ASA status (P=0.782) [Figure 4], MMP score (P=0.255) [Figure 5] and BMI (P=0.378) [Figure 6]. The commonest post-procedure complications were abdominal pain and nausea.
Figure 4.
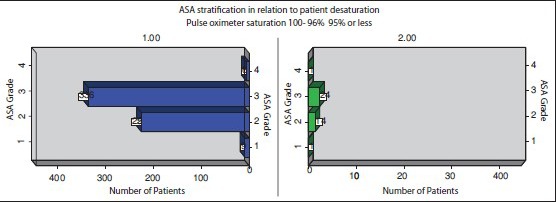
Relation of American Society of Anesthesiologists status and patient desaturation
Figure 5.
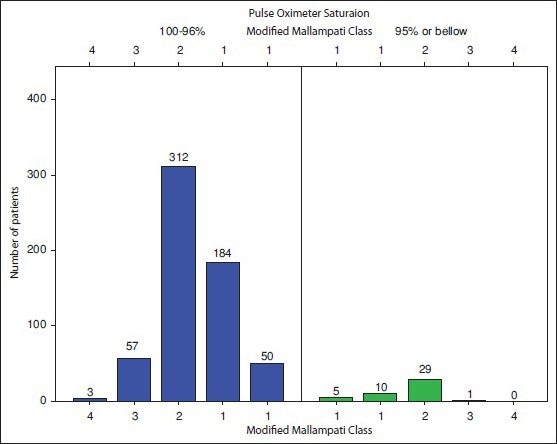
Relation between patient desaturation and Modified Mallampati score
Figure 6.
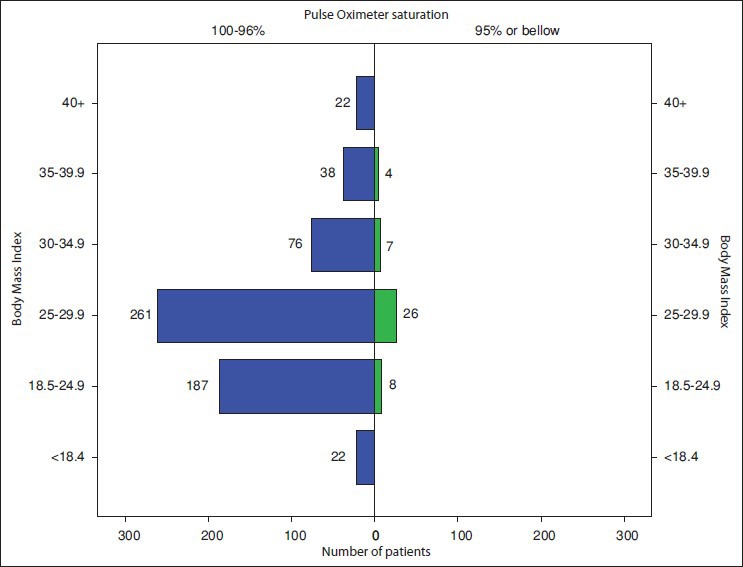
Relation between body mass index and patient desaturation
DISCUSSION
ERCP is a diagnostic/therapeutic gastrointestinal endoscopic procedure performed in prone/semi-prone position under deep sedation and sometimes-general anesthesia. ASA has recently redefined anesthesia and sedation, which has greatly cleared the confusion between the patients’ expectation (conscious sedation/Monitored Aanesthesia Care (MAC)) and providers’ perception of the state (usually general anesthesia). What we deliver in ERCP may be more appropriately defined as deep sedation in view of this document.[3] Propofol has emerged as a safe drug of choice for induction and maintenance of these patients.[4] with carefully titrated infusion, one can attain optimal sedation levels and the procedure can be safely performed avoiding general anesthesia and endotracheal intubation.[5,6,7] Although, multiple recent studies have advocated the use of sedation alone, the ability to predict possible complications is yet un-explored. The procedure often involves high-risk patients with multiple comorbidities in prone position. Unsecured airway, high-risk of aspiration and endoscope introduced orally (shared airway) make it difficult to appropriately treat any airway obstruction/apnea, while the patient is in an “anesthetist unfamiliar” position. The problems are compounded by the fact that commonly used respiratory monitoring (capnography) is not as reliable during this procedure. Additionally, ERCP also faces same limitations like other anesthesia procedures performed in remote locations.
In order to make ERCP under sedation safer, relation of desaturation episodes to possible patient related predictors was analyzed. To increase the sensitivity of detection of desaturation we chose an extremely low threshold of pulse oximetry measured fall to 95% or lower. Although, this value may seem clinically not relevant but we already mentioned that management of airway complications could be relatively difficult in ERCP, thus, statistically such a small value chosen allowed us to improve the sensitivity of detection of early desaturation which could later progress to become clinically significant. The present study found no correlation between desaturation with ASA status or BMI. ASA stratification data was available for 616 patients and 367 (60%) patients were either ASA III or IV. Most of these patients were ones with severe hepatic compromise, patients graded ASA III or IV due to cardiorespiratory compromise are not usually scheduled for ERCP as their lowered reserves prioritizes them to undergo cardiac/respiratory interventions first. As a result ASA III/IV patients in the study group on adequate pre-oxygenation had 100% baseline saturation and only 45% of total desaturation episodes were seen in this subgroup. This is in contrast to previous study by Berzin et al. where the authors concluded that anesthetist administered sedation had direct association with both higher ASA status and increasing BMI.[2] Unlike our study where we used airway devices (nasal trumpet/nasal cannula, etc.) with oxygen supplementation to prevent airway obstruction and desaturation, they relied primarily upon patient's natural airway tone to prevent obstruction under deep sedation. Sicker and obese patients are more likely to obstruct as a result of loss of upper airway tone due to the effects of anesthetic medications,[8] thus, our use of airway conduits probably eliminated these factors. The degree of success of these simple airway devices during ERCP is highlighted by the fact that 21 (3.2%) of our patients had obstructive sleep apnea with 29% of these receiving continuous positive airway pressure therapy. None required intubation or emergency airway interventions during or after the procedure. Only four of these showed transient desaturation, which was managed easily by ventilating using the bag mask attached to the nasal trumpet. Although, ventilation in this manner is not very effective, it was sufficient to supplement patient's poor respiratory efforts due to deep sedation. Readjustment of infusion rate helped to re-establish adequate spontaneous ventilation.
Another significant finding in our analysis was that no patient required emergency intubation during the procedure and no procedural interruptions were noted due to airway complications. Previous study by Raymondos et al. reported premature termination rate of around 14% either due to inadequate sedation or airway related complications.[9] At our center, use of airway conduits with oxygen supplementation allows us to titrate sedation to deeper levels without either desaturation or airway obstruction thus eliminating the possibility of inadequate sedation or airway obstruction. In view of higher incidence of complications, preference of general anesthesia over sedation for ERCP was advocated, however our present results favor the use of propofol based sedation over general anesthesia with almost no complication rates.[10] Another reason advocated for using general anesthesia by Ramondos et al., was that they had higher percentage of patients undergoing painful duct dilatations (61%). Use of shorter acting opioids like remifentanyl/fentanyl used in combination of propofol infusion provide satisfactory analgesia with high degree of patient satisfaction without recourse to general anesthesia. They also concluded that gastroenterologists found increased procedural difficulty levels with general anesthesia,[9] we however, due to non-availability of records on these aspects could not compare this outcome. Another reason for contrasting results between previous and recent literature emerging in favor of deep sedation is probably because of increased use of propofol infusions/boluses in recent era compared to use of benzodiazepines in combination with pethidine previously.[11] Quality of propofol sedation is known to be much better with deeper levels attainable on reliable dose response curves compared to benzodiazepines. Another reason for such a contrasting low incidence of airway complications in our analysis could be due to the presence of supervising anesthesiologist at gastroenterology suite, unlike previous studies where sedation was often administered by gastroenterologist himself, who may not be as efficient in predicting and treating airway related complications.
Five of 653 patients (0.76%) patients were administered planned general anesthesia with endotracheal intubation before beginning of the procedure due to various reasons, mainly aspiration risk. This is consistent with available literature and was carried out prophylactically as ERCP is known to increase the possibility of aspiration mainly due to prone/semi-prone positioning and associated gastric insufflation.[12] Patients with higher MMP class are likely to have higher incidence of upper airway obstruction under sedation/general anesthesia.[13] However, the present analysis found no relation of airway obstruction related early desaturations with MMP class. Our study clearly, highlights the importance of using airway conduits (with oxygen supplementation). Despite a low threshold of desaturation, only 6% patients showed transient desaturation below 95%, which responded to oxygen supplementation using same conduit without procedural interruptions. The type of airway device used was based upon individual preferences of nurse anesthetist assigned for the case. They also controlled the rate of oxygen supplementation via these conduits on a case basis, Oxygen was administered via either Mapelson C breathing system [Figure 7] at a rate of 12-15 l/min or If oxygen cannula was used it was carried out at 8-10 l/min. In the majority of procedures a standard nasal trumpet attached to Mapelson breathing system with suitable modification [Figure 7] was the airway of choice. These devices used during procedures under sedation not only prevent airway obstruction but can also provide slight continuos positive pressure, when used with high oxygen flow. This is supported by the fact that one patient had documented minimum saturation of 60% which responded to bag and mask ventilation via a nasal trumpet at high oxygen flow using Mapleson circuit.
Figure 7.

Image showing patient positioning and airway conduit (nasal cannula) for ERCP. The patient is being supplemented oxygen via a Mapleson circuit connected to nasal cannula
We did not analyze hemodynamic complications in our present study as these are often documented to be transient and without long-term sequelae. Our aim was to access airway related problems as these are deemed difficult to manage. Transient hypotension is associated with propofol-based sedation; multiple patients in our study received boluses of ephedrine/phenylephrine and responded well without any long-term sequelae.
LIMITATIONS
The present analysis suffers limitations similar to ones faced by ASA grading. Patients with cardio-respiratory diseases are more likely to desaturate rapidly attributable to their primary disease when compared to patients classified as higher ASA grade due to renal or hepatic disease. With a low threshold of only 5% fall in SpO2, although, we increased the sensitivity of foreseeing possible desaturations, this however, can be associated with increased number of false positive patients in desaturation group. Furthermore, capnography (commonest apnea monitoring) when used with high-flow oxygen supplementation is less reliable during ERCP,[14] thus, having low saturation cutoff initiated early airway interventions in prone position provided additional safety. The airway devices used were not standardized and varied with the nurse anesthetist involved in perioperative care. Finally, most retrospective analysis depends upon prior documentations done without intent of specific analysis later. Our anesthesia records were limited to complications warranting immediate actions during the procedure, therefore in the present analysis we focused upon primarily airway related issues involved in ERCP patients.
CONCLUSIONS
Pre-operative patient ASA status, higher MMP or increasing BMI does not bear relation with likelihood of patients desaturating during ERCP. In presence of vigilant apnea monitoring and careful dose titration of maintenance anesthetics with airway conduits, emergency intubations and procedure interruptions can be avoided.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Chainaki IG, Manolaraki MM, Paspatis GA. Deep sedation for endoscopic retrograde cholangiopacreatography. World J Gastrointest Endosc. 2011;3:34–9. doi: 10.4253/wjge.v3.i2.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berzin TM, Sanaka S, Barnett SR, Sundar E, Sepe PS, Jakubowski M, et al. A prospective assessment of sedation-related adverse events and patient and endoscopist satisfaction in ERCP with anesthesiologist-administered sedation. Gastrointest Endosc. 2011;73:710–7. doi: 10.1016/j.gie.2010.12.011. [DOI] [PubMed] [Google Scholar]
- 3.American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non Anesthesiologists. Practice guidelines for sedation and analgesia by non anesthesiologists. Anesthesiology. 2002;96:1004–17. doi: 10.1097/00000542-200204000-00031. [DOI] [PubMed] [Google Scholar]
- 4.Krugliak P, Ziff B, Rusabrov Y, Rosenthal A, Fich A, Gurman GM. Propofol versus midazolam for conscious sedation guided by processed EEG during endoscopic retrograde cholangiopancreatography: A prospective, randomized, double-blind study. Endoscopy. 2000;32:677–82. doi: 10.1055/s-2000-9021. [DOI] [PubMed] [Google Scholar]
- 5.Lordan JT, Woods J, Keeling P, Paterson IM. A retrospective analysis of benzodiazepine sedation vs. propofol anaesthesia in 252 patients undergoing endoscopic retrograde cholangiopancreatography. HPB (Oxford) 2011;13:174–7. doi: 10.1111/j.1477-2574.2010.00266.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garewal D, Powell S, Milan SJ, Nordmeyer J, Waikar P. Sedative techniques for endoscopic retrograde cholangiopancreatography. Cochrane Database Syst Rev. 2012;6:CD007274. doi: 10.1002/14651858.CD007274.pub2. [DOI] [PubMed] [Google Scholar]
- 7.Jung M, Hofmann C, Kiesslich R, Brackertz A. Improved sedation in diagnostic and therapeutic ERCP: Propofol is an alternative to midazolam. Endoscopy. 2000;32:233–8. doi: 10.1055/s-2000-96. [DOI] [PubMed] [Google Scholar]
- 8.Schwartz AR, Patil SP, Squier S, Schneider H, Kirkness JP, Smith PL. Obesity and upper airway control during sleep. J Appl Physiol. 2010;108:430–5. doi: 10.1152/japplphysiol.00919.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Raymondos K, Panning B, Bachem I, Manns MP, Piepenbrock S, Meier PN. Evaluation of endoscopic retrograde cholangiopancreatography under conscious sedation and general anesthesia. Endoscopy. 2002;34:721–6. doi: 10.1055/s-2002-33567. [DOI] [PubMed] [Google Scholar]
- 10.Etzkorn KP, Diab F, Brown RD, Dodda G, Edelstein B, Bedford R, et al. Endoscopic retrograde cholangiopancreatography under general anesthesia: Indications and results. Gastrointest Endosc. 1998;47:363–7. doi: 10.1016/s0016-5107(98)70219-6. [DOI] [PubMed] [Google Scholar]
- 11.Rey JF. Sedation for upper gastrointestinal endoscopy: As much as possible, or without? Endoscopy. 1996;28:308–9. doi: 10.1055/s-2007-1005460. [DOI] [PubMed] [Google Scholar]
- 12.Garewal D, Waikar P. Propofol sedation for ERCP procedures: A dilemna? Observations from an anesthesia perspective. Diagn Ther Endosc 2012. 2012 doi: 10.1155/2012/639190. 639190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saghaei M, Shetabi H, Golparvar M. Predicting efficiency of post induction mask ventilation based on demographic and anatomical factors. [Available ahead of print Last cited 2013 Jan 24];Adv Biomed Res. 2012 1:10. doi: 10.4103/2277-9175.96056. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3507007 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goudra BG, Singh PM, Sinha AC. Anesthesia for ERCP: Impact of Anesthesiologist's Experience on Outcome and Cost. Anesthesiology Research and Practice. 2013;2013:5. doi: 10.1155/2013/570518. Article ID 570518. doi:10.1155/2013/570518. [DOI] [PMC free article] [PubMed] [Google Scholar]


