Abstract
Purpose:
To compare two different doses of propofol for laryngeal mask airway (LMA) insertion in children undergoing out-patient surgeries.
Background:
Insertion of LMA just after anesthesia induction is facilitated using propofol. However, the optimal dose of this drug not determined yet as heavy doses may lead to severe complications, whereas lower doses may not be quite as effective.
Methods:
In a double-blind randomized clinical trial, 120 children undergoing out-patient surgeries were recruited to receive intravenous propofol at a dose of either 2.5 mg/kg (group 1) or 3.5 mg/kg (group 2) for induction. Intravenous midazolam (0.03 mg/kg) and fentanyl (1 μg/kg) were used as pre-medication in all patients and anesthesia induction was initiated using lidocaine (1 mg/kg) prior to propofol administration. Hemodynamic changes, probable complications, quality of the established airway and number of attempts for LMA insertion were compared between two groups.
Results:
There were no differences in systolic and diastolic blood pressure, heart rate, peripheral oxygen saturation and intraoperative complications between the groups (P>0.05). LMA insertion was successful at the first attempt in 55 (93.2%) and 54 (91.5%) cases in group 1 and group 2, respectively (P>0.05). The efficiency of the established airways was adequate in all the patients of both groups.
Conclusion:
It seems that propofol doses of 2.5 and 3.5 mg/kg are equally effective for LMA insertion following intravenous midazolam, fentanyl, and lidocaine.
Keywords: Children, laryngeal mask airway, propofol
INTRODUCTION
Being a standard and widely accepted supraglottic airway device for airway management in children, laryngeal mask airway (LMA) has been commonly used in the field of pediatric anesthesia since 1990.[1] LMA insertion, however, is not always achieved easily, a gentle technique is of great importance throughout this procedure. Appropriate anesthetic depth along with sufficient muscle relaxation is required to prevent complications such as cough, struggling, laryngospasm, and patient movement.[2] At the present time, propofol is accepted as the most frequently administered medication for LMA insertion. Scanlon et al. reported better results of LMA insertion while using propofol (2.5 mg/kg) compared with thiopental (5 mg/kg).[3] On the other hand, in their study, Bahk et al. recommended not using single propofol in LMA insertion.[4] Numerous medications including lidocaine, midazolam, low-dose muscle relaxants and opioids have been added to hypnotic agents to assist LMA insertion. In general, administering several of the above mentioned medications for LMA insertion procedure increases the success rate to more than 90%.[2] Recommended induction doses for propofol are 2.9 mg/kg in an infant younger than 2 years and 2.2 mg/kg in children 6-12 years.[5] The aim of the present study was to determine the most appropriate of two propofol doses in LMA insertion while maintaining spontaneous breathing without encountering unwanted complications including hypotension and apnea in children.
METHODS
In a double-blind randomized clinical trial, which was approved by the ethics committee of University of Medical Sciences, 120 children undergoing different operations in university affiliated Children's Hospital were randomized into two groups of 60 patients from May 2009 to May 2011. Prior to the study, written informed parental consents were obtained from all patients’ parents. All children were American Society of Anesthesiologists (ASA) class 1 or II patients weighing less than 20 kg. The children underwent out-patient surgeries including inguinal herniorrhaphy, cryptorchidism surgery and etc., Children with airway anomalies and history of upper respiratory tract complication within previous 4 weeks were excluded.[6] In all patients, pre-medication was performed using midazolam (0.03 mg/kg/IV) and fentanyl (1 μg/kg/IV) (few minutes before separation from parents) and anesthesia induction was initiated using lidocaine (1 mg/kg).[7] Group 1 (n=60) was given propofol with a dose of 2.5 mg/kg and group 2 (n=60) was given propofol with a dose of 3.5 mg/kg. FiO2 100% before LMA insertion and FiO2 mixed with air 50% after LMA insertion were administered. Moreover, ventilation was managed as assisted spontaneous ventilation in both groups to keep Etco2 less than 45 mmHg. Heart rate (HR), systolic and diastolic blood pressure (BP), and peripheral oxygen saturation (SpO2) were recorded before induction (after iv pre-medication), immediately after LMA insertion, and in 10 and 20 min (by anesthesia nurse that was blind to propofol dosage). Appropriate LMA size was calculated based on the bodyweight; LMA size 1 was used for weight <5 kg, size 1.5 for 5-10 kg and size 2 for 10-20 kg. Rotational LMA insertion with partially inflated technique was administered in all patients. The success rate of LMA insertion at first attempt was evaluated based on the ventilation status; easy ventilation was defined as the presence of normal capnogram wave and lack of air leak after LMA insertion. In case of poor ventilation, LMA was removed and reinserted. A rescue propofol dose of 2 mg/kg was used whenever there was resistance to LMA insertion or the patient moved.
Ventilation via LMA was graded as adequate (rectangular capnographic wave form was obtained with no air leak at airway pressure of 20 cm H2O), possible (capnographic wave form was obtained with air leak at airway pressure less than 20 cm H2 O) and impossible (no capnographic trace detected).[8] The patient was excluded from the study in case of a failure in successful LMA insertion after second attempt. In all patients, anesthesia was maintained with isoflurane (1-2%). Demographic data, number of attempts for LMA insertion, and efficiency of established airway were listed. The incidence of complications including cough, resistance to LMA insertion and apnea was recorded as well. Finally probable complications, ease of insertion and grade of established airway ventilation were compared.
To achieve a power of 80% (insertion success first try) with a type I error rate of 0.05, the sample size was calculated as sixty patients for each group. Data were presented as mean ± standard deviation. Obtained data were analyzed using SPSS (Statistical Package for the Social Sciences) ver. 16.0. Chi-square or Fisher's exact tests were used to study the qualitative data, T-test for independent groups to compare quantitative variables and repeated measures analysis to evaluate the vital indices in both groups. A P value less than 0.05 was considered statistically significant.
RESULTS
One hundred and twenty children were included in the study; meanwhile two patients were excluded because of failure in LMA insertion (these patients intubated for surgery). Data obtained from 118 children were later analyzed: 59 individuals in each group. There were no differences in gender, age, and weight between the groups (P>0.05)]. Furthermore, no significant differences in systolic and diastolic BP, HR, and SpO2 were detected between two groups at different recorded times P>0.05, Figures 1-4 group 1 and group 2, respectively (P>0.05). LMA insertion was accomplished at the second attempt in 4 (6.8%) and 5 (8.5%) children in groups 1 and 2, respectively (P>0.05). The efficiency of the established airways was adequate in all the patients of the both groups. In addition, intraoperative complications (cough, resistance to LMA insertion and apnea) were observed in 6 (10.1%) and 1 (1.6%) patients in groups 1 and 2, respectively (P=0.11).
Figure 1.
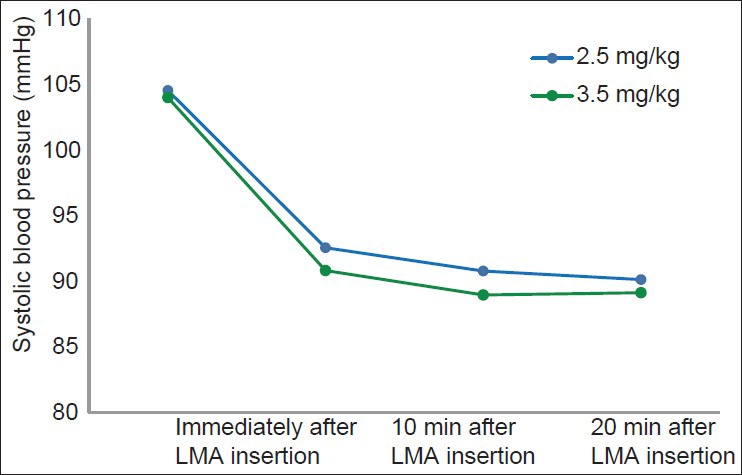
Systolic blood pressure changes at different recorded times between two groups
Figure 4.
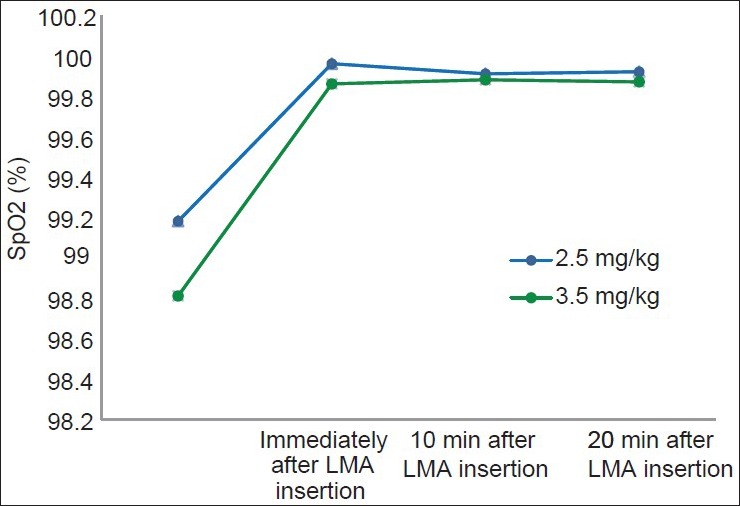
SpO2 changes at different recorded times between two groups
Figure 2.
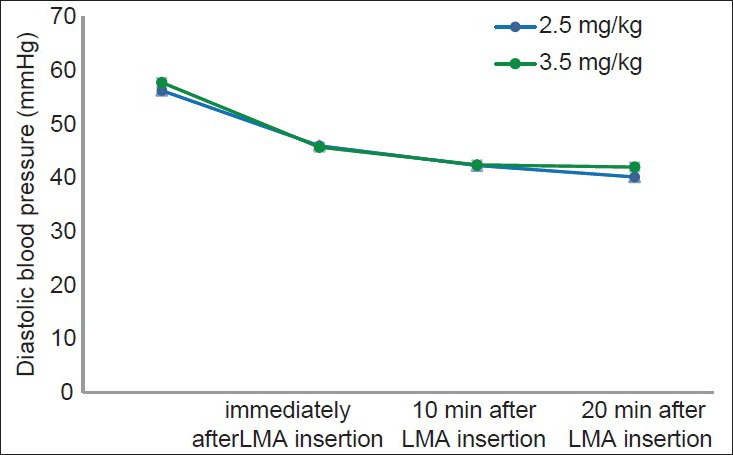
Diastolic blood pressure changes at different recorded times between two groups
Figure 3.
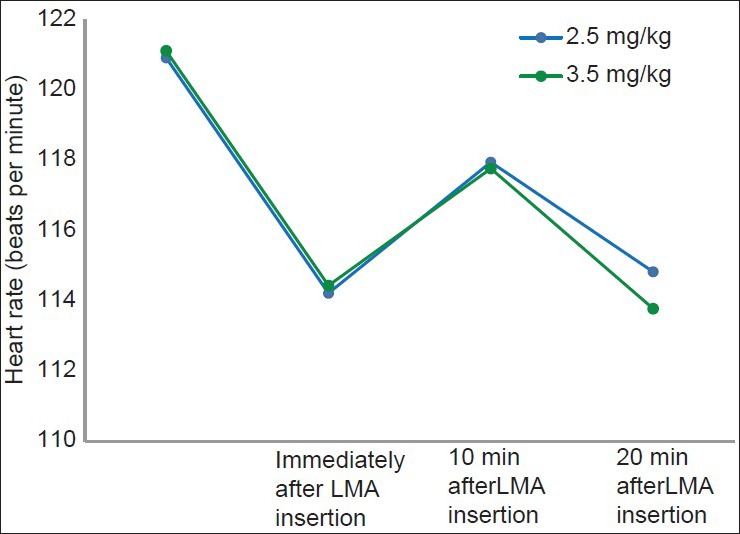
Heart rate changes at different recorded times between two groups
DISCUSSION
In the present study, comparing both groups revealed no statistically significant difference regarding the number of attempts for LMA insertion, complications and the success of insertion.
Overall more than 90% of the attempts led to successful insertion. This finding is in accordance with the study by Allsop et al. who reported successful insertion in all their patients.[9] Ti et al. studied the efficacy of intravenous propofol with the dose of 3 mg/kg versus sevoflurane for LMA insertion in adults and concluded that the advantages of this dose of medication were quick LMA insertion and fewer attempts.[10] In contrast, Bahk et al. concluded that none of the proposed doses of propofol (2.5, 3, 3.5, and 4 mg/kg), compared with ketamine plus lidocaine spray group, were associated with appropriate results, yet there was increased risk of complications (apnea and airway obstruction).[4]
With regard to the complications following propofol administration, there have been controversial results; in a study carried out by Scanlon et al. the efficacy of propofol administration with those of 2.5 mg/kg for LMA insertion was studied on 35 children and the results were compared with a group receiving thiopental.[3] The complications, in this study, were observed in 26% of the cases of propofol group, which was significantly less than the thiopental group. Consequently propofol was suggested to be utilized in children for LMA insertion.[3] In our study, the complications associated with this dose of the medication were 10% (mostly resist to LMA insertion) in group I and 3.3% in the other group. Therefore, the results obtained from our study are in better status regarding complications compared with those of the study by Scanlon et al.[3] Administering pre-medication may have contributed to this difference. It has already been proven that pre-medication using midazolam or fentanyl or a combination of both could decrease the required dose of propofol and its related complications significantly.[11,12,13,14] Martelew et al. in a study carried out on children, concluded that pre-medication could decrease complications such as hypotension and apnea significantly.[11] In the study of Park et al., a significant difference was reported in the EC50 of the propofol for LMA insertion in the patients having received remifentanyl compared with the patients having received normal saline.[15] We also used midazolam, fentanyl, and lidocaine as premedication in both groups which could explain the low complication rates in both groups. In contrast, Allsop et al. studied LMA insertion success rate in children having received propofol doses of 2.5, 3, and 3.5 mg/kg with no pre-medication. In their study, easier insertions were achieved in the latter group.[9]
In contrast, successful LMA insertion was similarly achieved using both propofol doses of 2.5 and 3.5 mg/kg in the present study. In the study of Baik et al., the efficacy of propofol based on target plasma concentration was evaluated. It was concluded that higher concentrations of the medication led to easier insertion. However, they could cause hypotension as well.[16,17] In our study, despite being statistically insignificant, hypotension and increase in HR until 10 min, which was followed by a decrease in HR were observed in both groups. These findings are all in accordance with Allsop et al. report as well.[9]
The present study has certain limitations. One of the limitations of the present study could be examining only two doses of propofol (2.5 and 3.5 mg/kg). Further studies investigating wider ranges of proposed doses are recommended. In the present study, the route of administering pre-medication was intravenous, which was due to unavailability of oral agents such as midazolamin our country. This could limit generalizing our findings. As the rate of the complications was not sufficient to be compared with the hemodynamic variables, it seems that further studies with larger number of patients and consequently higher rates of complications are required to achieve a solid relation in this regard. Nevertheless, using pre-medication could be considered as an advantageous factor over the previous similar studies.[9]
In conclusion, it seems that propofol doses of 2.5 and 3.5 mg/kg have no superiority over each other in LMA insertion in children.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Nakayama S, Osaka Y, Yamashita M. The rotational technique with a partially inflated laryngeal mask airway improves the ease of insertion in children. Paediatr Anaesth. 2002;12:416–9. doi: 10.1046/j.1460-9592.2002.00847.x. [DOI] [PubMed] [Google Scholar]
- 2.Hui JK, Critchley LA, Karmakar MK, Lam PK. Co-administration of alfentanil-propofol improves laryngeal mask airway insertion compared to fentanyl-propofol. Can J Anaesth. 2002;49:508–12. doi: 10.1007/BF03017932. [DOI] [PubMed] [Google Scholar]
- 3.Scanlon P, Carey M, Power M, Kirby F. Patient response to laryngeal mask insertion after induction of anaesthesia with propofol or thiopentone. Can J Anaesth. 1993;40:816–8. doi: 10.1007/BF03009250. [DOI] [PubMed] [Google Scholar]
- 4.Bahk JH, Sung J, Jang IJ. A comparison of ketamine and lidocaine spray with propofol for the insertion of laryngeal mask airway in children: A double-blinded randomized trial. Anesth Analg. 2002;95:1586–9. doi: 10.1097/00000539-200212000-00021. [DOI] [PubMed] [Google Scholar]
- 5.Seyedhejazi M, Abafattash G, Taheri R. Accidental 5-fold overdose of propofol for induction in a 38-days-old infant undergoing emergency bilateral inguinal hernia repair. Saudi J Anaesth. 2011;5:417–8. doi: 10.4103/1658-354X.87273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taheri R, Shayeghi S, Razavi SS, Sadeghi A, Ghabili K, Ghojazadeh M, et al. Efficacy of bupivacaine-neostigmine and bupivacaine-tramadol in caudal block in pediatric inguinal herniorrhaphy. Paediatr Anaesth. 2010;20:866–72. doi: 10.1111/j.1460-9592.2010.03374.x. [DOI] [PubMed] [Google Scholar]
- 7.Taheri R, Seyedhejazi M, Ghojazadeh M, Ghabili K, Shayeghi S. Comparison of ketamine and fentanyl for postoperative pain relief in children following adenotonsillectomy. Pak J Biol Sci. 2011;14:572–7. doi: 10.3923/pjbs.2011.572.577. [DOI] [PubMed] [Google Scholar]
- 8.Komatsu R, Nagata O, Sessler DI, Ozaki M. The intubating laryngeal mask airway facilitates tracheal intubation in the lateral position. Anesth Analg. 2004;98:858–61. doi: 10.1213/01.ane.0000100741.46539.6b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allsop E, Innes P, Jackson M, Cunliffe M. Dose of propofol required to insert the laryngeal mask airway in children. Paediatr Anaesth. 1995;5:47–51. doi: 10.1111/j.1460-9592.1995.tb00240.x. [DOI] [PubMed] [Google Scholar]
- 10.Ti LK, Chow MY, Lee TL. Comparison of sevoflurane with propofol for laryngeal mask airway insertion in adults. Anesth Analg. 1999;88:908–12. doi: 10.1097/00000539-199904000-00041. [DOI] [PubMed] [Google Scholar]
- 11.Martlew RA, Meakin G, Wadsworth R, Sharples A, Baker RD. Dose of propofol for laryngeal mask airway insertion in children: Effect of premedication with midazolam. Br J Anaesth. 1996;76:308–9. doi: 10.1093/bja/76.2.308. [DOI] [PubMed] [Google Scholar]
- 12.Driver IK, Wiltshire S, Mills P, Lillywhite N, Howard-Griffin R. Midazolam co-induction and laryngeal mask insertion. Anaesthesia. 1996;51:782–4. doi: 10.1111/j.1365-2044.1996.tb07897.x. [DOI] [PubMed] [Google Scholar]
- 13.Gill PS, Shah J, Ogilvy A. Midazolam reduces the dose of propofol required for induction of anaesthesia and laryngeal mask airway insertion. Eur J Anaesthesiol. 2001;18:166–70. doi: 10.1046/j.0265-0215.2000.00805.x. [DOI] [PubMed] [Google Scholar]
- 14.Goyagi T, Tanaka M, Nishikawa T. Fentanyl decreases propofol requirement for laryngeal mask airway insertion. Acta Anaesthesiol Scand. 2003;47:771–4. doi: 10.1034/j.1399-6576.2003.00123.x. [DOI] [PubMed] [Google Scholar]
- 15.Park HJ, Lee JR, Kim CS, Kim SD, Kim HS. Remifentanil halves the EC50 of propofol for successful insertion of the laryngeal mask airway and laryngeal tube in pediatric patients. Anesth Analg. 2007;105:57–61. doi: 10.1213/01.ane.0000266447.23037.e4. [DOI] [PubMed] [Google Scholar]
- 16.Baik HJ, Kim JH, Lee CH. Laryngeal mask insertion during target-controlled infusion of propofol. J Clin Anesth. 2001;13:175–81. doi: 10.1016/s0952-8180(01)00237-9. [DOI] [PubMed] [Google Scholar]
- 17.Seyedhejazi M, Zarrintan S. Evaluation of caudal anesthesia performed in conscious infants for lower abdominal surgeries. Neurosciences. 2008;13:46–8. [PubMed] [Google Scholar]


