Abstract
Background:
The purpose of this study was to clinically evaluate the benefits of sub gingival chlorhexidine (CHX) varnish and biodegradable CHX chip application used as an adjunct to scaling and root planning (SRP) as combined therapy and also to compare the effect of combined therapy with SRP alone.
Materials and Methods:
Fifteen patients with at least three sites with a probing pocket depth (PPD) of 5-8 mm were considered. Following baseline evaluation, all three sites were subjected for SRP. After completing SRP, each site was randomly subjected for CHX varnish, CHX chip application and the 3rd site was left without any medication as a control. Clinical parameters such as sulcus bleeding index, plaque index, bleeding on probing (BOP), PPD, and clinical attachment level (CAL) were recorded at baseline, 1 month and 3 months post-operatively.
Results:
All three groups presented with an improvement in clinical parameters compared to baseline. The mean reduction in PPD was 2.4 mm in SRP sites, 2.5 mm in SRP + CHX varnish sites and 2.8 mm in SRP + CHX chip sites. The mean gain in CAL was 2.4 mm in SRP sites, 2.3 mm in SRP + CHX varnish sites and 2.8 mm SRP + CHX chip sites.
Interpretation and Conclusion:
The present study indicated that application of CHX varnish and placement of CHX chip as an adjunct to SRP produced a clinically significant reduction in the PPD, BOP and a gain in CAL at 30th day and 90th day from baseline when compared to SRP alone. The results though were not statistically significant.
Keywords: Chlorhexidine chip and scaling and root planning, chlorhexidine varnish, local drug delivery, periodontitis
Introduction
Periodontitis is a multifactorial disease caused by the presence of periodontopathogenic species in a susceptible host and this susceptibility maybe influenced by environmental and genetic factors. The most important goal of periodontal therapy is to reduce or eliminate the sub gingival microorganisms, which cause the periodontal disease to maintain periodontal health and if possible to regenerate the lost tissues. Scaling and root planning (SRP) is considered as a gold standard to attain and maintain periodontal health by elimination of bacterial plaque. As the probing depth increases, the effectiveness of SRP decreases because of limited access to deep pockets, which leads to incomplete removal of periodontopathogens.[1]
Due to the infective nature of periodontal disease, several antimicrobial agents, which are delivered by rinsing, irrigation, systemic administration, and local devices, have been used to overcome the limited efficacy of conventional treatment of periodontitis. The inherent limitations of systemic and topical chemotherapeutics led to the development of local drug delivery systems. Targeting the antimicrobial agent directly to the infected site and maintaining effective levels for a sufficient time are necessary for successful treatment.[2] This approach also addresses the critical concerns of unnecessarily exposing the patient to large amounts of systemic antibiotics, which can result in bacterial resistance.[3]
Chlorhexidine (CHX) has long been known as an effective antimicrobial agent and has been used as a topical antiseptic for over 30 years. Its efficacy as a topical mouth rinse to inhibit dental plaque and gingivitis has been well established and demonstrated in study periods for two years without evidence of the development of any bacterial resistance.[4] It is a bisbiguanide antiseptic and antimicrobial agent, which is used as a locally applied slow release drug delivery system available in the form of gel, varnish, chip, etc.
To enhance the efficacy of non-surgical therapy a chemo-mechanical treatment concept was introduced based on sequential SRP and the adjunctive subgingival administration of 35% CHX varnish[5] and subgingival placement of a biodegradable CHX chip,[6] which biodegrades and releases CHX within the pocket over 7-10 days maintaining an average concentration in the GCF greater than 12 mg/ml for 8 days.
The objectives of this study were to clinically evaluate the use of CHX varnish and biodegradable CHX chip when used as an adjunct to SRP (combined therapy) and also to compare the combined therapy with SRP alone.
Materials and Methods
Experimental design
A total of 15 patients (7 males and 8 females) aged 35-55 years reporting to the Department of Periodontics and Implantology, Coorg Institute of Dental Sciences, Virajpet, Coorg were recruited for the study.
Inclusion criteria
Subjects diagnosed with chronic periodontitis characterized by at least three sites with a probing depth of 5-8 mm, which should bleed on probing
Presence of minimum 16 natural teeth (at least 4 teeth per quadrant)
Subjects in a good state of general health without any systemic disorder.
Exclusion criteria
Subjects with a history of allergy to CHX
Subjects who are on any medication within the last 6 months
Subjects showing endodontic-periodontic lesions
Subjects undergoing orthodontic treatment
Subjects who have undergone surgery in relation to the site within a period of 6 months
Subjects with habits such as smoking, mouth breathing, and tongue thrusting.
After an initial screening visit for recruitment and signing an informed consent, all patients were subjected for site selection by another examiner who was unaware of the study design. Then, three sites in each patient were randomly assigned for Group A, Group B, and Group C. Baseline measurements were recorded on all sites and subjected to different treatment modality accordingly. The study protocol was approved by the ethical committee of Coorg Institute of Dental Sciences, Virajpet, Karnataka.
Treatment
In each patient, the treatment sites were divided randomly into three groups: Group A (Control site): Periodontal pocket was treated by SRP alone [Figure 1].
Figure 1.
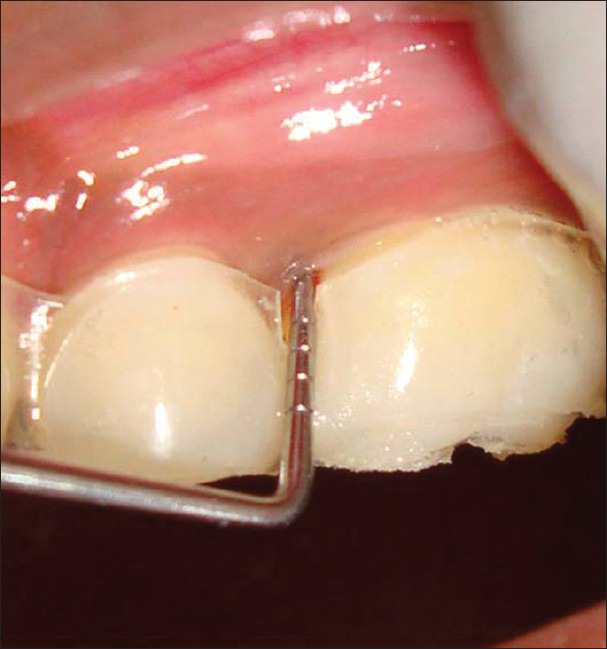
Baseline – SRP group – 5 mm probing depth
Group B (CHX varnish): Periodontal pocket was treated with SRP plus the application of CHX varnish. The varnish was applied using a blunt needle and the content was slowly released while the needle was moved in a coronal direction from the bottom of the pocket. Pockets were deliberately overfilled and left for 15 min. Then, the excess varnish was gently removed by using Gracey's curette [Figures 2, 3 and 4].
Figure 2.
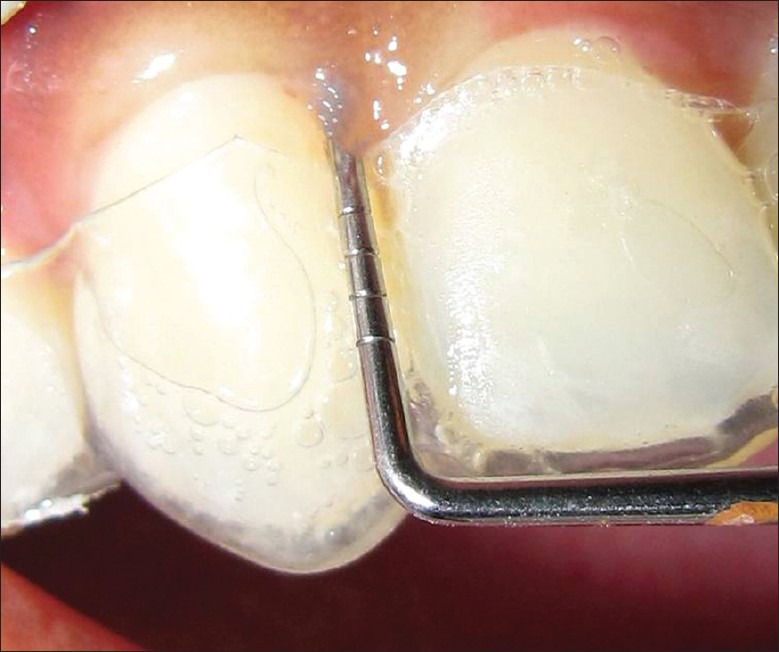
Baseline – SRP + CHX varnish group 5mm probing depth
Figure 3.
Initial CHX varnish application – SRP + CHX varnish group
Figure 4.

CHX Varnish removal after 15 minutes with a curette
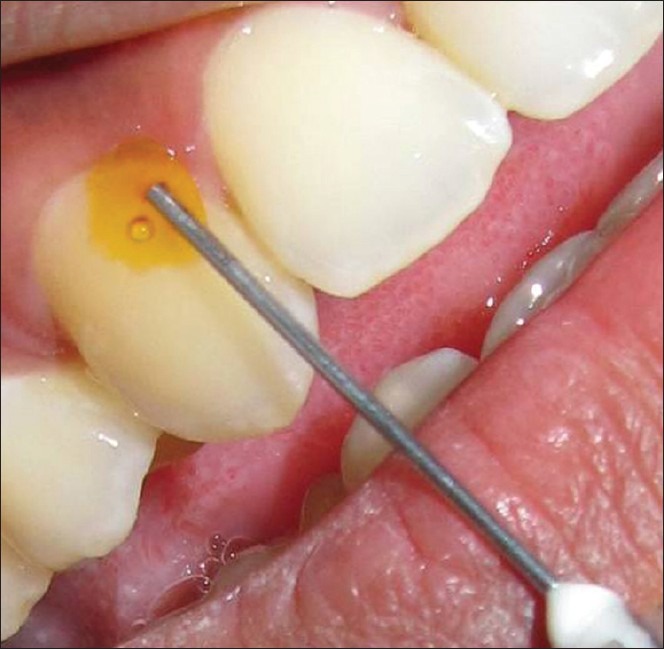
Group C (CHX chip): Periodontal pocket was treated with SRP, and then the biodegradable CHX chip was placed inside the pocket. The chip was inserted apically into the pocket with the rounded end of the chip facing towards the base of the pocket until resistance is met at the base of the pocket and the sites were covered with a periodontal dressing (Coe pack) [Figures 5 and 6].
Figure 5.

Baseline – SRP + CHX chip group – 5 mm probing depth
Figure 6.

CHX chip insertion – SRP + CHX Chip group
Examination criteria
The following parameters were recorded at baseline, 1 month and 3 months post-operatively:
Plaque index (PI) (Silness and Loe 1964)[7]
Bleeding on probing (BOP) evaluated 30 s after pocket probing
Sulcus Bleeding index (SBI) (Mühlemann and Son 1971)[8]
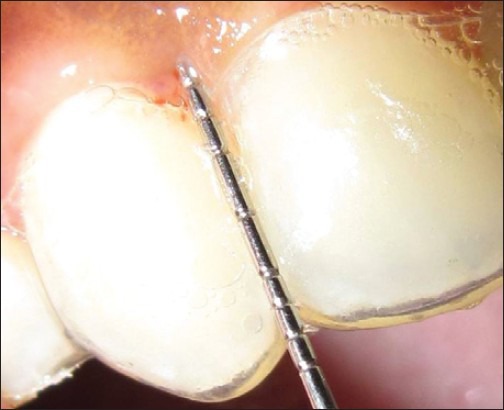
Probing Pocket depth (PPD) linear measurement taken from the gingival margin to base of the pocket using customized acrylic occlusal stent with vertical grooves.
Clinical attachment level (CAL) CAL was measured using occlusal stent with vertical grooves.
Statistical analysis
The indices values of PI and SBI were subjected for Kruskal Wallis test. The clinical changes over time within each group and the impact of the treatment modalities on BOP; PPD and CAL were statically analyzed with Mann Whitney U-test.
Results
Plaque Index (PI)
The PI determined the overall oral hygiene status of the patient. The mean PI of Group A (SRP) at baseline was 1.33, at 30 days was 0.73 and at 90 days, it was 0.8 and the difference was statistically significant. The mean PI of Group B (SRP + CHX varnish) at baseline was 1.67, at 30 days was 0.67 and at 90 days was 0.73 and the difference was statistically significant. The mean PI of Group C (SRP + CHX chip) at baseline was 1.67, at 30 days was 0.67, and at 90 days it was 0.8 and the difference was statistically significant [Table 1].
Table 1.
Kruskal Wallis test showing the comparison of plaque index between the 3 groups (SRP, SRP+CHX varnish and SRP+CHX chip) at baseline, 30th day and 90th day
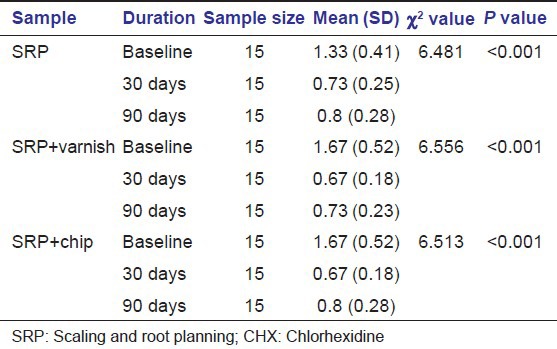
The results showed a significant reduction (P < 0.001) in PI scores between baseline and 30th and 90th day. There was a slight increase in the score from 30th to 90th day. All three selected sites demonstrated BOP at baseline, i.e., 100%.
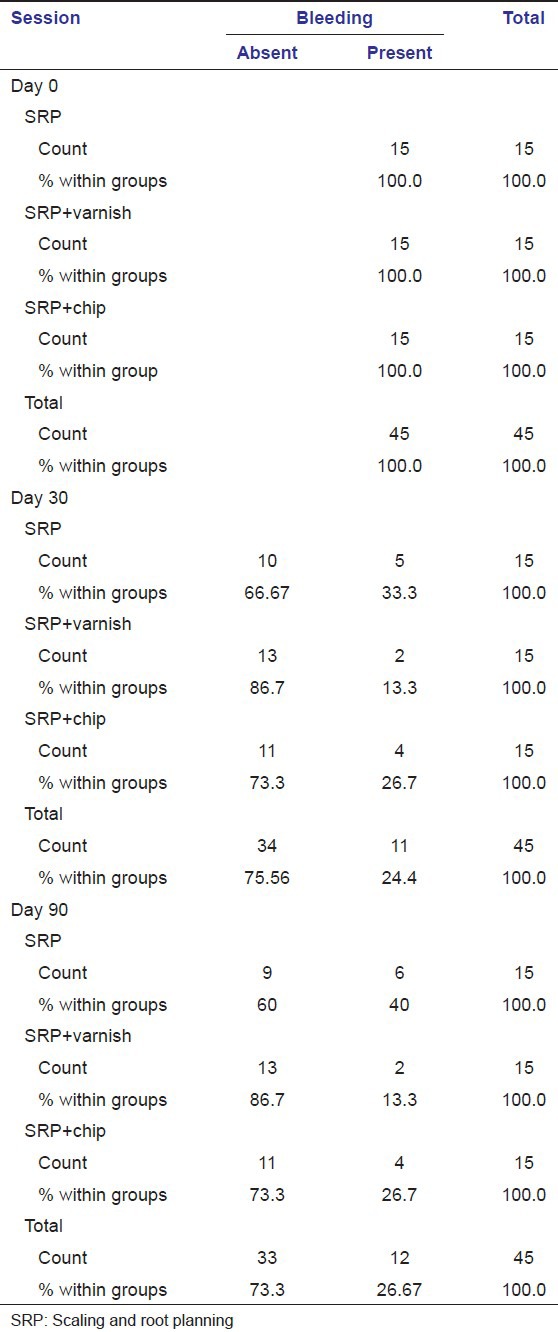
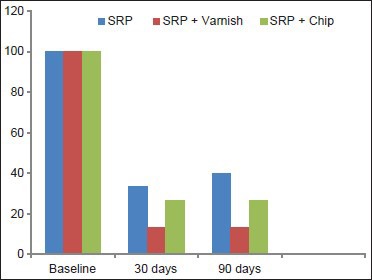
BOP
The percentage reduction in BOP on 30th day was 66.67% in Group A, 86.7% in Group B, and 73.3% in Group C. The percentage reduction in BOP on 90th day was 60% in Group A, 86.7% in Group B, and 73.3% in Group C. The differences were statistically significant [Table 2, Graph 1].
Table 2.
Percentages of bleeding on probing between the three groups at baseline, 30th day and 90th day
Graph 1.
Comparing probing pocket depth between the three groups (scaling and root planning [SRP], SRP + chlorhexidine [CHX] varnish and CHX chip) at baseline, 30th day and 90th day
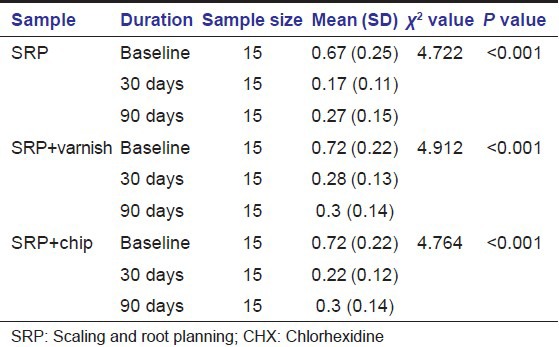
Sulcus bleeding index
The mean SBI of Group A (SRP alone) at baseline was 0.67, at 30 days was 0.17 and at 90 days was 0.27. The difference was statistically significant. The mean SBI of Group B (SRP + CHX varnish) at baseline was 0.72, at 30 days was 0.28 and at 90 days was 0.3. The difference was statistically significant. The mean SBI of Group C (SRP + CHX chip) at baseline was 0.72, at 30 days was 0.22 and at 90 days was 0.3 and the difference was statistically significant.
The results showed a significant reduction (P < 0.001) in index scores between baseline and 30th and 90th day. There was a slight increase in the score from 30th to 90th day [Table 3].
Table 3.
Kruskal Wallis test showing the comparison of sulcus bleeding index between the 3 groups (SRP, SRP+CHX varnish and SRP+CHX chip) at baseline, 30th day and 90th day
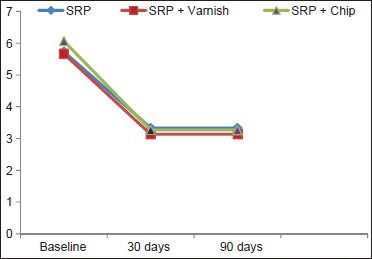
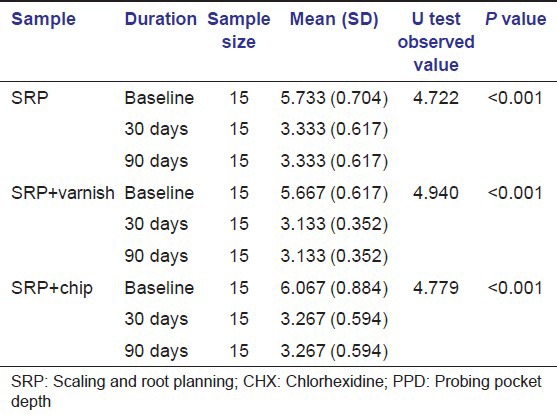
PPD
In Group A, the average values at baseline were 5.733 ± 0.704, at 30th day the average values of PPD reduced to 3.333 ± 0.617 and after that until 90th day there was no further reduction in PPD was seen. However, this difference in reduction of PPD was statistically significance (P < 0.001). In Group B, the average PPD was reduced from 5.667 ± 0.617 at baseline to 3.133 ± 0.352 at 30th day, which was statically significant. There was no further reduction in PPD was seen thereafter. Similar results were seen in Group C where PPD reduced from 6.067 ± 0.884 at baseline to 3.267 ± 0.594 at 30th day [Table 4, Graph 2, Figures 7, 8 and 9].
Table 4.
The PPD between the three groups (SRP, SRP+CHX varnish and SRP+CHX chip) at baseline, 30th day and 90th day Mann Whitney U test
Graph 2.
Comparison of Clinical Attachment Level between the three groups (scaling and root planning [SRP], SRP + chlorhexidine [CHX] varnish, SRP + CHX chip) at baseline 30th day and 90th day
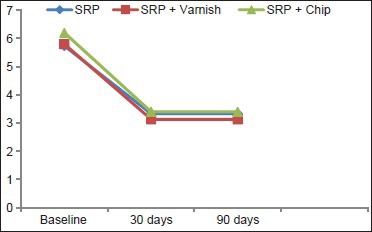
Figure 7.
90th day – SRP + CHX varnish group – 2 mm probing depth
Figure 8.

90th day – SRP + CHX Chip group –3 mm probing depth
Figure 9.

90th day – SRP group – 3 mm probing depth
CAL
In Group A, the average value of CAL at baseline was 5.733 ± 0.704, at 30th day the average value reduced to 3.333 ± 0.617 and this gain in CAL between 0th and 30th day was statistically significant. In Group B, the baseline value was 5.800 ± 0.775, at 30th day it was 3.133 ± 0.352 and the difference was statically significance. Similarly, in Group C the average value of CAL reduced from 6.200 ± 1.082 to 3.400 ± 0.632 at baseline and 30th day respectively, which was statistically significant; however in all three groups have shown no further improvement in CAL from 30th to 90th day [Table 5, Graph 3].
Table 5.
The clinical attachment levels between the three groups (SRP, SRP+CHX varnish and SRP+CHX chip) at baseline, 30th day and 90th day Mann Whitney U test
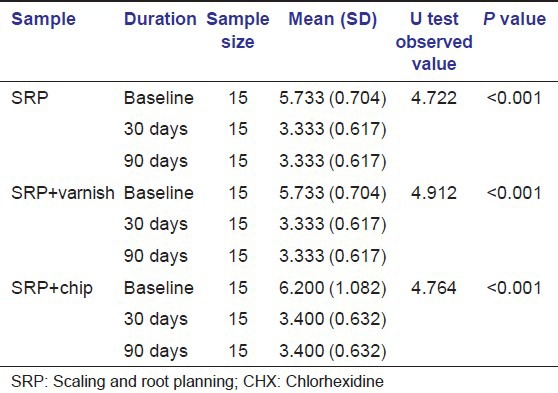
Graph 3.
The differences in percentages of Bleeding on Probing between three groups (scaling and root planning [SRP], SRP + chlorhexidine [CHX] varnish and SRP + CHX chip) at baseline, 30th day and 90th day
Discussion
The objective of the study was to evaluate the efficacy of two CHX containing local drug delivery systems (EC40 CHX varnish and Periochip) over SRP for a period of 3 months. The 3 month time frame was chosen because the effects of locally delivered CHX has been shown to be evident for 11 weeks after administration and also 3 months corresponds to the typical recall interval for patients after periodontal treatment.[2]
In the present study, the full mouth plaque scores from baseline to 30th and 90th day were taken into consideration. There was a reduction in PI scores, which was statistically significant. These findings are in accordance with the results obtained in studies conducted by Soskolne et al. (1997),[9] Jeffcoat et al. (1998),[2] and Heasman et al. (2001).[3]
The SBI scores showed a significant reduction in both groups from baseline until 90th day. The results are in accordance with the findings observed by Soskolne et al. (1997),[9] Jeffcoat et al. (1998),[2] Heasman et al. (2001).[3]
Reduction in BOP was similar in all three groups of sites. This can be attributed to the elimination of local factors with SRP in all three groups, which is in accordance with studies conducted by Carvalho et al. 2007.[10]
There was a significant reduction in PPD in the Groups A (SRP group), B (SRP + CHX varnish group) and C (SRP + CHX chip group) from baseline to 30 days. However, the reduction in probing depth from 30 days to 3 months was not as significant rather it was consistent. This is in accordance with the results of the studies conducted by Jeffcoat et al. (2000),[6] Heasman et al. (2001).[3]
The intergroup probing depth values when compared to Group A (SRP group), Group B (SRP + CHX varnish group) and Group C (SRP + CHX chip group) showed no statistical difference between the groups at 3 months from baseline. This is in accordance with the results of the studies by Jeffcoat et al. (2000)[6] Heasman et al. (2001)[3] where significant differences were noted between the groups only at 9 months from baseline. The results are also in conjunction with Grisi (2002)[11] wherein the probing depth at 3, 6, and 9 months did not show any significant differences between the control and test groups. Results obtained from another study by Rodrigues et al. (2007)[12] also demonstrated that at 6 months all three treatment groups were equally effective. This is also in accordance with Grisi et al. (2002)[11] in which the differences in probing depth and CALs between the control and test groups were not statistically significant at 3 and 6 months.
The findings of this study were not in accordance with Soskolne et al. (1997)[13] wherein statistically significant differences were found between test and control groups at 3 and 6 months. This is may be attributed to differences in study design and sample size. A point to be considered is that in both multicenter studies (Soskolne et al. 1997,[9] Jeffcoat et al. 1998[2]) the period of SRP was confined to one hour period without administration of local anesthetic, in a study carried out by Badersten et al. in which SRP was carried out with no time limit and under local anesthesia, sites showed improvements in probing depth and clinical attachment gain greater than those obtained in the controlled pockets. The results are also in conjunction with the study done by Carvalho et al. 2007[10] and it has reiterated the fact that time limitation may have affected the quality of root planning.
All three groups showed statistically significant reduction in PPD and gain in CAL from baseline to 30th day, but there was no significant difference in the scores from 30th to 90th day or rather the scores remained stable and also there was no significant difference in the scores within the groups.
In the present study, the CAL values followed a trend similar to probing depth reduction, improvement in attachment levels was observed in all the groups when compared to pre-treatment values. The mean attachment gain was 2.4 mm (SRP group), 2.3 mm (SRP + CHX varnish group) and 2.8 mm (SRP + CHX chip group). The results obtained between all the three groups were similar.
The present study indicated that application of CHX varnish and placement of CHX chip as an adjunct to SRP produced a clinically significant reduction in the PPD, BOP and a gain in CAL at 30th day and 90th day from baseline when compared to SRP alone though the results were not statistically significant. The limitations of this study could be a smaller sample size over a shorter period and single application/insertion of the varnish/chip.
Conclusion
Based on the findings of this study, CHX varnish (EC40) and CHX chip (Periochip) did provide clinically significant benefits beyond that achieved with conventional SRP after a 3 month period, but the difference was not statistically significant. Long-term studies with a larger sample size and multiple application/insertion are required to determine the potential use of these drugs as an adjunct to conventional periodontal therapy.
Footnotes
Source of Support: Nil,
Conflict of Interest: None declared
References
- 1.Buchanan SA, Robertson PB. Calculus removal by scaling/root planing with and without surgical access. J Periodontol. 1987;58:159–63. doi: 10.1902/jop.1987.58.3.159. [DOI] [PubMed] [Google Scholar]
- 2.Jeffcoat MK, Bray KS, Ciancio SG, Dentino AR, Fine DH, Gordon JM, et al. Adjunctive use of a subgingival controlled-release chlorhexidine chip reduces probing depth and improves attachment level compared with scaling and root planing alone. J Periodontol. 1998;69:989–97. doi: 10.1902/jop.1998.69.9.989. [DOI] [PubMed] [Google Scholar]
- 3.Heasman PA, Heasman L, Stacey F, Mc Cracken GI. Local delivery of chlorhexidine gluconate (PerioChip) in periodontal maintenance patients. J Clin Periodontol. 2001;28:90–5. doi: 10.1034/j.1600-051x.2001.280114.x. [DOI] [PubMed] [Google Scholar]
- 4.Seymour RA, Heasman PA. A Modern Clinical Picture. 1st ed. Ch. 3. 2009. Textbook of Drugs, Diseases and the Periodontium; p. 38. [Google Scholar]
- 5.Cosyn J, Wyn I, De Rouck T, Sabzevar MM. Subgingival chlorhexidine varnish administration as an adjunct to same-day full-mouth root planing. I. Clinical observations. J Periodontol. 2007;78:430–7. doi: 10.1902/jop.2007.060221. [DOI] [PubMed] [Google Scholar]
- 6.Jeffcoat MK, Palcanis KG, Weatherford TW, Reese M, Geurs NC, Flashner M. Use of a biodegradable chlorhexidine chip in the treatment of adult periodontitis: Clinical and radiographic findings. J Periodontol. 2000;71:256–62. doi: 10.1902/jop.2000.71.2.256. [DOI] [PubMed] [Google Scholar]
- 7.Silness J, Loe H. Periodontal disease in pregnancy. ii. Correlation between oral hygiene and periodontal condtion. Acta Odontol Scand. 1964;22:121–35. doi: 10.3109/00016356408993968. [DOI] [PubMed] [Google Scholar]
- 8.Mühlemann HR, Son S. Gingival sulcus bleeding: A leading symptom in initial gingivitis. Helv Odontol Acta. 1971;15:107–13. [PubMed] [Google Scholar]
- 9.Soskolne WA, Heasman PA, Stabholz A, Smart GJ, Palmer M, Flashner M, et al. Sustained local delivery of chlorhexidine in the treatment of periodontitis: A multi-center study. J Periodontol. 1997;68:32–8. doi: 10.1902/jop.1997.68.1.32. [DOI] [PubMed] [Google Scholar]
- 10.Carvalho J, Novak MJ, Mota LF. Evaluation of the effect of subgingival placement of chlorhexidine chips as an adjunct to scaling and root planing. J Periodontol. 2007;78:997–1001. doi: 10.1902/jop.2007.060122. [DOI] [PubMed] [Google Scholar]
- 11.Grisi DC, Salvador SL, Figueiredo LC, Souza SL, Novaes AB, Grisi MF. Effect of a controlled-release chlorhexidine chip on clinical and microbiological parameters of periodontal syndrome. J Clin Periodontol. 2002;29:875–81. doi: 10.1034/j.1600-051x.2002.291001.x. [DOI] [PubMed] [Google Scholar]
- 12.Rodrigues IF, Machion L, Casati MZ, Nociti FH, Jr, de Toledo S, Sallum AW, et al. Clinical evaluation of the use of locally delivered chlorhexidine in periodontal maintenance therapy. J Periodontol. 2007;78:624–8. doi: 10.1902/jop.2007.060317. [DOI] [PubMed] [Google Scholar]
- 13.Soskolne WA. Probing depth changes following 2 years of periodontal maintenance therapy including adjunctive controlled release of chlorhexidine. J Periodontol. 2006;77:437–43. doi: 10.1902/jop.2003.74.4.420. [DOI] [PubMed] [Google Scholar]


