Abstract
Introduction:
Oral lichen planus (OLP) is a relatively common inflammatory mucocutaneous disorder that frequently involves the oral mucosa. The clinical presentation of OLP ranges from mild painless white keratotic lesions to painful erosions and ulcerations. An important complication of OLP is the development of oral squamous cell carcinoma, which led the World Health Organization (WHO) to classify OLP as a potentially malignant disorder. The demographic and clinical characteristics of OLP have been well-described in several relatively large series from developed countries, whereas such series from developing countries are rare.
Objective:
The objective of this retrospective study was to investigate the epidemiological and clinical characteristics of 128 OLP patients in rural population of India.
Materials and Methods:
In this study, the diagnostic criteria proposed by van der Meij et al. in 2003 based on the WHO definition of OLP were used to identify cases.
Results:
In 128 patients, M:F ratio was 1.61:1. The buccal mucosa was the most common site (88.20%). White lichen was seen in 83.59% and red lichen in 16.40% cases. Reticular type of OLP was the most common form (83.5%) followed by erosive (15.6%) and atrophic OLP (0.78%). The incidence of systemic diseases included hypertension (11%), diabetes mellitus (2.4%), and hypothyroidism (0.78%). Histopathologically epithelial dysplasia was present in 4 cases.
Conclusion:
Most of the characteristics are consistent with previous studies with differences in few. Lichen planus is a chronic disease where treatment is directed to control of symptoms. Long-term follow-up is essential to monitor for symptomatic flare ups and possible malignant transformation.
Keywords: Clinical features, lichen planus, oral mucosa
Introduction
Oral lichen planus (OLP) is a relatively common inflammatory mucocutaneous disorder that frequently involves the oral mucosa. The exact etiology is uncertain, but the immunological system is believed to play a significant role in it. It has a protracted clinical course despite various available treatment modalities.[1,2] The age of onset is usually between 3rd and 6th decade of life and it is commonly seen in Asian population.[3,4] The prevalence of OLP is 1-2% in the general population while its prevalence in Indian population is 2.6%.[5] It is predominantly seen in females.[6,7,8,9]
Its clinical presentation ranges from mild painless white keratotic lesions to painful erosions and ulcerations.[10] The most commonly affected site is buccal mucosa, usually bilateral. Clinically, OLP may occur in six clinical variants as reticular, papular, plaque-like, erosive, atrophic and bullous as classified by Andreasen.[11] It was simplified by other authors[12] who consider only three types of lesions: Reticular, including white lines, plaques and papules; atrophic, and erythematous; and erosive, including ulcerations and bullae. Gandolfo et al.[13] and Carbone et al.[14] classified the clinical forms of OLP in white lichen in the presence of reticular, papular, or plaque-like lesions and as red lichen in the presence of atrophic, erosive or bullous lesions, independently of whether or not these coincide with white lichen at the periphery or in other sites. The reticular form is the most common type and presents as papules and plaques with interlacing white keratotic lines (Wickham striae) with an erythematous border. The typical location of striae are bilaterally on the buccal mucosa, mucobuccal fold, gingiva, and less commonly on the tongue, palate, and lips.[15] The reticular type has been reported to occur significantly more often in men compared to women[9] and is usually asymptomatic. Erosive, atrophic or bullous type lesions cause burning sensation and pain.
Genital and cutaneous lichen planus are associated with approximately 20% and 15% of OLP, respectively.[1,16] One of the most important complication concerning the progression and prognosis of OLP is the development of oral squamous cell carcinoma (OSCC), with a frequency of malignant transformation of 0.4-5.3%,[17] which led the World Health Organization (WHO) to classify OLP as a potentially malignant disorder.[18] Thus, evaluation of OLP patients by a multidisciplinary group of health care providers is very important due to the occasional concomitant lesion in extraoral sites involvement and oral cancer risk.
The demographic and clinical characteristics of OLP have been well-described in several relatively large series from developed countries,[6,8,11,12,13,14] whereas such series from developing countries are rare.[5,7,19] Besides, there are no universally accepted specific clinically and histopathologically diagnostic criteria to date while other disorders such as leukoplakia, erythroplakia, and discoid lupus erythematosus can present with a similar clinical appearance.
The objective of this retrospective study was to investigate the epidemiological and clinical characteristics of 128 OLP patients in rural population of India, describe similarities and differences in clinical features of these patients relative to those in previously reported series.
Materials and Methods
All case files of patients with the clinical and pathological diagnosis of OLP in the Department of Oral Medicine were retrospectively reviewed. Most of the patients were diagnosed on clinical grounds when the lesion showed Wickhams striae. The diagnostic criteria proposed by van der Meij et al.[20] in 2003 based on the WHO definition of OLP were used to identify the cases of OLP. These included clinical as well as histopathological features. The clinical criteria included the presence of bilateral, mostly symmetrical lesions, presence of lace-like network of slightly raised white lines (reticular pattern), erosive, atrophic, bullous, and plaque type lesions. Histopathological criteria included hypergranulosis, parakeratosis, acanthosis, “liquefaction degeneration” of cells within the basal layer and presence of lymphohistiocytic infiltrate in a band-like pattern at the level of papillary dermis and absence of epithelial dysplasia.
Biopsies from some of the lesions were taken, especially in suspicious cases of malignancy or in erosive type, whenever patients consented. In our clinic, periodic follow-up examinations at intervals of every 6 months (or less if required) were recommended for patients diagnosed with OLP. Based on these criteria 128 patients with OLP were selected for review. Information regarding age, gender, symptoms, sites of oral involvement, predominant clinical form (reticular, atrophic and erosive) at the time of the initial diagnosis of OLP was all documented. History of smoking, tobacco and gutakha chewing, alcohol use, systemic disease, and family history (i.e., in first-degree relatives) of OLP and oral cancer were also reviewed and analyzed. In patients with more than one clinical form of lesions, the most severe clinical form was used to classify the lesions.
Results
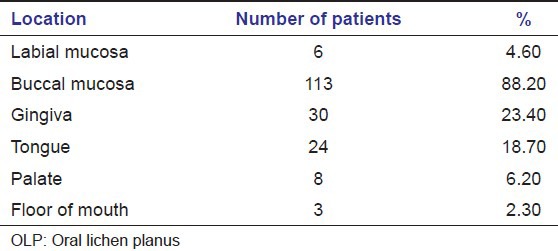
The epidemiological characteristics of OLP are presented in Table 1. There were 49 females and 79 males (ratio M:F = 1.61:1), the mean age at presentation was 35.5 years for males and 39.1 years for females. The mean age at diagnosis was 36.9 years, and the peak of age-frequency distribution was the third decade (35.2%) of life. The buccal mucosa was the most common site (88.20%). Gingiva, tongue and lip were affected in 24 (18.7%), 30 (23.40%) and 6 (4.6%) patients respectively [Figures 1 and 2].
Table 1.
Age and sex distribution of 128 patients with OLP
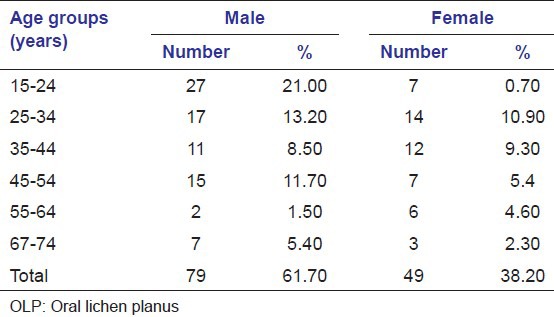
Figure 1.

Reticular oral lichen planus affecting gingivae
Figure 2.

Wickhams striae on buccal mucosa
Multiple oral sites were affected in 51 (39.84%) patients. Buccal mucosa concomitant tongue was affected in 48 (37.5%) patients. Lesions only on the lip, gingiva, palate, and in the floor of the oral cavity were uncommon. The clinical characteristics of OLP are listed in Tables 2 and 3. At initial presentation, white lichen was seen in 107 (83.59%) patients, and red lichen was observed in 21 (16.40%) patients. Reticular type of OLP was the most common form and was present in 107 (83.5%) patients. Erosive form was observed in 20 (15.6%) patients while atrophic OLP was present in only one (0.78%) patient. Reticular form was predominantly seen in males (n = 76) while erosive and atrophic types were predominantly observed in females (n = 15). History of tobacco, gutakha chewing, smoking and alcohol use were reported in 51 (39.8%), 26 (20.3%), 10 (7.81%) and 13 (10.15%) cases, respectively. Family history of OLP and oral cancer was not reported in our study. The incidence of systemic diseases included hypertension (11%), diabetes mellitus (2.4%) and hypothyroidism (0.78%).
Table 2.
Distribution of OLP lesions according to clinical type
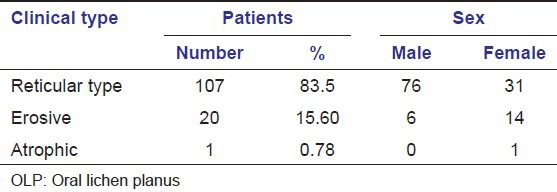
Table 3.
Distribution of OLP lesions according to site
History of skin lesions was present in 4 (3.1%) patients. Histopathologically epithelial dysplasia was present in four cases. We recorded no cases of malignant transformation in this case series [Figure 3].
Figure 3.
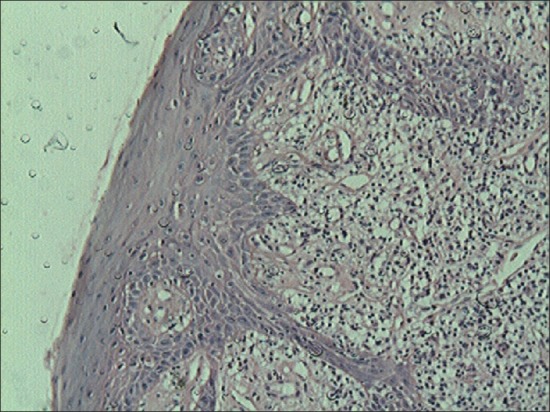
Histopathological features of oral lichen planus
Discussion
The present retrospective study attempts to elucidate the epidemiological and clinical characteristics of OLP patients in relatively small cohort from India. Retrospective studies have many limitations and cannot be compared satisfactorily to prospective studies. However, they are useful in evaluating patient populations.
The data presented in this study are consistent with data from previous OLP studies in regard to lesion location, its clinical type, disease chronicity, symptoms and medical history.
According to the clinical and histopathological criteria of the WHO, the results of this study reveal that OLP is seen in middle-aged patients, with sex predilection for males, and it usually affected the bilateral buccal mucosa, gingiva and tongue.
The clinical features of patients in our study share many similarities and some disimilarities with those reported previously. In this study, we observed that the men outnumbered the women (ratio M:F = 1.61:1), which is not in agreement with various other reports.[8,19,21] In most of the studies done in different parts of the world a female predominance is reported. OLP is more prevalent in 3rd decade of life in our study (mean age 36.9 years), which is lower than the mean age reported in central China (50.4 years), UK (52.0 years), Spain (56.4 years), and Italy (56.7 years).[6,13,15,19] This was probably due to the ethnic population and geographic difference in our cohorts compared to previous reports. OLP in minor juveniles or children is uncommon and in our study childhood form of OLP was not observed. Although childhood OLP is very rare, early recognition is very important to make appropriate treatment and relieve symptoms of little children.[3,4]
As previously mentioned, the lesions of OLP were typically bilateral, symmetrical and the buccal mucosa was the most common site of involvement, followed by the gingiva and the tongue.[6,8,13,14,15,16,17,18,19,20,21] Multiple oral sites involvement was also common. Buccal mucosa concomitant gingive were the most common multiple oral sites. Isolated lesions located on gingiva, palate, and mouth floor were rare, whereas these sites usually concomitant buccal mucosa or tongue were affected in multiple oral sites.
Reticular type of OLP was the most common form and was present in 107 (83.5%) patients. Erosive form was observed in 20 (15.6%) patients while atrophic OLP was present in only one (0.78%) patient. Reticular form was predominantly seen in males (n = 76) while erosive and atrophic types were predominantly observed in females (n = 15). These findings are consistent with various previous studies.
The associated pigmentation of the oral mucosa was a prominent feature in reticular form. It was noted in 38 patients. The higher frequency of pigmentation in this study could be related to racial factors, skin type and habit of chewing gutakha, tobacco, and betelnut and leaves by the local population. The pigmentation was diffuse or in patches, ranged from brown to black in color and seen especially on the buccal mucosa. Other less affected sites were adjacent gingivae, lateral and dorsal aspect of tongue and hard palate. The similar findings were observed in some Indian studies.[9,22]
According to two categories of clinical form classified by Gandolfo et al.[13] and Carbone et al.,[14] the prevalence of white lichen in their series were 59.7% and 58.9%, respectively. Likewise, the prevalence of white lichen in our series was 83.59% and red lichen was 16.4%. Besides, none of the patient from our series of patients had family members with a history of OLP. Bermejo-Fenoll et al.[15] reported five families with two affected members, and one family with three affected members. These did not provide definitive insight into a genetic basis; whether OLP and development of OSCC has a strong genetic etiopathogenesis was not established by this study.
The majority of the patients (67%) from this study complained of some degree of oral discomfort in the form of burning sensation, pain or soreness as reported in other studies.[6,12]
Histopathologically, epithelial dysplasia was present in four cases. The similar findings were reported in study performed by Murti et al.[5] Malignant transformation was not observed in our study. These findings are consistent with studies by Murti et al. and Andreasen.[5,11]
The incidence of the history of systemic diseases including hypertension (11.0%), diabetes mellitus (2.4%), hypothyroidism (0.78%) was not higher than expected when compared with the incidence reported in the general population. Moreover, the incidence of these systemic diseases was lower than the previous reports.[3,6,16,21] This indicates systemic diseases may not have a role in the pathogenesis of OLP. Although the correlation of OLP with diabetes mellitus has been suggested,[23] our present study did not support this observation.
The long-term behavior of OLP has rarely been reported, although data suggest that perhaps 17-20% of patients will have spontaneous resolution of signs and symptoms of this entity.[12,21] Cutaneous and genital involvement of lichen planus can precede, arise concurrently with or appear after the development of OLP. It is estimated that 20-34% of patients with OLP have cutaneous or other mucosal lesions of LP.[12] In the present study, only four patients had a history of skin lesions. Thus we, as specialists in Oral Medicine should carefully examine the skin of hands, feet and legs of patients with OLP, enquire regarding signs/symptoms of genital lesions and when relevant, referral to an appropriate specialist should be carried out.
In conclusion, the present study elucidated the epidemiological and clinical characteristics of patients with OLP in a relatively small cohort of the rural population in India. Most of the characteristics are consistent with previous studies while few are not in agreement with those studies. Since, lichen planus is a chronic disease, treatment is directed to control of symptoms. The most effective drugs have been anti-inflammatory and immunosuppressive agents. Long-term follow-up is essential to monitor for symptomatic flare ups and possible malignant transformation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Farhi D, Dupin N. Pathophysiology, etiologic factors, and clinical management of oral lichen planus, part I: Facts and controversies. Clin Dermatol. 2010;28:100–8. doi: 10.1016/j.clindermatol.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 2.Crincoli V, Di Bisceglie MB, Scivetti M, Lucchese A, Tecco S, Festa F. Oral lichen planus: Update on etiopathogenesis, diagnosis and treatment. Immunopharmacol Immunotoxicol. 2011;33:11–20. doi: 10.3109/08923973.2010.498014. [DOI] [PubMed] [Google Scholar]
- 3.Alam F, Hamburger J. Oral mucosal lichen planus in children. Int J Paediatr Dent. 2001;11:209–14. doi: 10.1046/j.1365-263x.2001.00266.x. [DOI] [PubMed] [Google Scholar]
- 4.Laeijendecker R, Van Joost T, Tank B, Oranje AP, Neumann HA. Oral lichen planus in childhood. Pediatr Dermatol. 2005;22:299–304. doi: 10.1111/j.1525-1470.2005.22403.x. [DOI] [PubMed] [Google Scholar]
- 5.Murti PR, Daftary DK, Bhonsle RB, Gupta PC, Mehta FS, Pindborg JJ. Malignant potential of oral lichen planus: Observations in 722 patients from India. J Oral Pathol. 1986;15:71–7. doi: 10.1111/j.1600-0714.1986.tb00580.x. [DOI] [PubMed] [Google Scholar]
- 6.Ingafou M, Leao JC, Porter SR, Scully C. Oral lichen planus: A retrospective study of 690 British patients. Oral Dis. 2006;12:463–8. doi: 10.1111/j.1601-0825.2005.01221.x. [DOI] [PubMed] [Google Scholar]
- 7.Pakfetrat A, Javadzadeh-Bolouri A, Basir-Shabestari S, Falaki F. Oral Lichen Planus: A retrospective study of 420 Iranian patients. Med Oral Patol Oral Cir Bucal. 2009;14:E315–8. [PubMed] [Google Scholar]
- 8.Eisen D. The clinical features, malignant potential, and systemic associations of oral lichen planus: A study of 723 patients. J Am Acad Dermatol. 2002;46:207–14. doi: 10.1067/mjd.2002.120452. [DOI] [PubMed] [Google Scholar]
- 9.Chainani-Wu N, Silverman S, Jr, Lozada-Nur F, Mayer P, Watson JJ. Oral lichen planus: Patient profile, disease progression and treatment responses. J Am Dent Assoc. 2001;132:901–9. doi: 10.14219/jada.archive.2001.0302. [DOI] [PubMed] [Google Scholar]
- 10.Scully C, Carrozzo M. Oral mucosal disease: Lichen planus. Br J Oral Maxillofac Surg. 2008;46:15–21. doi: 10.1016/j.bjoms.2007.07.199. [DOI] [PubMed] [Google Scholar]
- 11.Andreasen JO. Oral lichen planus. 1. A clinical evaluation of 115 cases. Oral Surg Oral Med Oral Pathol. 1968;25:31–42. doi: 10.1016/0030-4220(68)90194-1. [DOI] [PubMed] [Google Scholar]
- 12.Silverman S, Jr, Gorsky M, Lozada-Nur F. A prospective follow-up study of 570 patients with oral lichen planus: Persistence, remission, and malignant association. Oral Surg Oral Med Oral Pathol. 1985;60:30–4. doi: 10.1016/0030-4220(85)90210-5. [DOI] [PubMed] [Google Scholar]
- 13.Gandolfo S, Richiardi L, Carrozzo M, Broccoletti R, Carbone M, Pagano M, et al. Risk of oral squamous cell carcinoma in 402 patients with oral lichen planus: A follow-up study in an Italian population. Oral Oncol. 2004;40:77–83. doi: 10.1016/s1368-8375(03)00139-8. [DOI] [PubMed] [Google Scholar]
- 14.Carbone M, Arduino PG, Carrozzo M, Gandolfo S, Argiolas MR, Bertolusso G, et al. Course of oral lichen planus: A retrospective study of 808 northern Italian patients. Oral Dis. 2009;15:235–43. doi: 10.1111/j.1601-0825.2009.01516.x. [DOI] [PubMed] [Google Scholar]
- 15.Bermejo-Fenoll A, Sánchez-Siles M, López-Jornet P, Camacho-Alonso F, Salazar-Sánchez N. A retrospective clinicopathological study of 550 patients with oral lichen planus in south-eastern Spain. J Oral Pathol Med. 2010;39:491–6. doi: 10.1111/j.1600-0714.2010.00894.x. [DOI] [PubMed] [Google Scholar]
- 16.Edwards PC, Kelsch R. Oral lichen planus: Clinical presentation and management. J Can Dent Assoc. 2002;68:494–9. [PubMed] [Google Scholar]
- 17.Eisen D. The evaluation of cutaneous, genital, scalp, nail, esophageal, and ocular involvement in patients with oral lichen planus. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:431–6. doi: 10.1016/s1079-2104(99)70057-0. [DOI] [PubMed] [Google Scholar]
- 18.Shi P, Liu W, Zhou ZT, He QB, Jiang WW. Podoplanin and ABCG2: Malignant transformation risk markers for oral lichen planus. Cancer Epidemiol Biomarkers Prev. 2010;19:844–9. doi: 10.1158/1055-9965.EPI-09-0699. [DOI] [PubMed] [Google Scholar]
- 19.Xue JL, Fan MW, Wang SZ, Chen XM, Li Y, Wang L. A clinical study of 674 patients with oral lichen planus in China. J Oral Pathol Med. 2005;34:467–72. doi: 10.1111/j.1600-0714.2005.00341.x. [DOI] [PubMed] [Google Scholar]
- 20.van der Meij EH, Schepman KP, van der Waal I. The possible premalignant character of oral lichen planus and oral lichenoid lesions: A prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96:164–71. doi: 10.1016/s1079-2104(03)00305-6. [DOI] [PubMed] [Google Scholar]
- 21.Thorn JJ, Holmstrup P, Rindum J, Pindborg JJ. Course of various clinical forms of oral lichen planus. A prospective follow-up study of 611 patients. J Oral Pathol. 1988;17:213–8. doi: 10.1111/j.1600-0714.1988.tb01527.x. [DOI] [PubMed] [Google Scholar]
- 22.Kanwar AJ, Ghosh S, Dhar S, Kaur S. Oral lesions of lichen planus. Int J Dermatol. 1993;32:76. doi: 10.1111/j.1365-4362.1993.tb00982.x. [DOI] [PubMed] [Google Scholar]
- 23.Lowe NJ, Cudworth AG, Clough SA, Bullen MF. Carbohydrate metabolism in lichen planus. Br J Dermatol. 1976;95:9–12. doi: 10.1111/j.1365-2133.1976.tb15530.x. [DOI] [PubMed] [Google Scholar]


