Abstract
Ameloblastoma is a unique, histologically benign but aggressive neoplasm of the jaws, arising from odontogenic epithelium with potency to cause extensive destruction of jaw bones and infiltration into the surrounding tissues. Recurrences are common after incomplete treatment. Recurrences can occur at difficult sites such as temporal and infratemporal fossa, orbit, anterior cranial base, paranasal sinuses etc. Fine needle aspiration cytology or core biopsy of these recurrent lesions may be misleading. Clinical course and radiological features help immensely in these situations. Good communication between surgeon, radiologist, and pathologist is of paramount importance.
Keywords: Oral squamous cell carcinoma, recurrent ameloblastoma, temporal fossa
Introduction
Ameloblastoma is a unique neoplasm of the jaws arising from odontogenic epithelium presenting in a variety of clinico-radiological and histological forms. Although histologically benign, ameloblastoma represents a locally aggressive lesion with potency to cause extensive destruction of jaws with infiltration into the surrounding soft tissues. Recurrences after surgical treatment are common, locally.[1] Very rarely, they may present in temporal/infratemporal fossa, orbit, anterior skull base and with intracranial extensions.[2,3,4,5,6,7]
Case Report
A 32-year-old Indian female reported to our institution in October 2010 with a painless swelling in the left temporal region. She had undergone a fine needle aspiration cytology (FNAC) which was reported elsewhere as “Chondromyxoid aspirate with atypical chondrocytes-suggesting malignancy.” Slides were not available for review. An orthopantomograph showed left hemimandibulectomy with disarticulation. She gave a history of prior surgery (2005) for the lower jaw swelling. No details were available.
Clinical examination showed a ~8 cm × 7 cm × 5 cm, soft, fluctuant, non-pulsatile, and non-tender swelling in left temporal fossa along with a 6 cm scar in the submandibular region. Cranial nerve examination was normal. There were no palpable neck nodes. Oral cavity examination was normal [Figure 1a and b]. A computed tomography (CT) showed a well-defined, 8 cm × 6 cm, uniform, oval, cystic, homogenous lesion medial to the left zygomatic arch, infiltrating the pterygoid and temporalis muscles, abutting the deep lobe of the parotid gland, and causing erosion of the left zygomatic arch [Figure 2a and b].
Figure 1.

(a and b) Frontal and worm's eye views show swelling over the left side of face arising from temporal region. Furthermore, note the submandibular scar from the previous surgery and the cosmetic deformity due to surgery and the swelling
Figure 2.
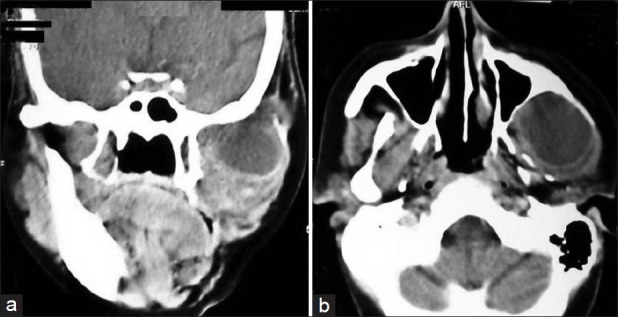
(a and b) Radiological appearance of the lesion in left temporal fossa on computed tomography (Detail description in text)
On FNAC, amber colored, non-purulent fluid showed inflammatory infiltrate of macrophages, occasional giant cells, atypical squamous cells with enlarged nuclei and keratinous cytoplasm. A core biopsy showed fibroadipose tissue with tiny focus of a tumor with squamoid differentiation infiltrating skeletal muscle. Squamous cell carcinoma was reported.
However, clinical course and radiological features of the lesion were pointing toward a benign pathology. Case was discussed in tumor board and surgical excision was planned. After thorough work-up, patient underwent excision of left temporal mass with infratemporal fossa clearance via a combined temporal and cervical approaches under general anesthesia [Figure 3a]. Reconstruction was carried out using the free anterolateral thigh flap to provide for oral cavity lining and bulk in the temporal area. Histopathological examination confirmed “ameloblastoma” [Figure 4a]. Patient is disease free for last 1½ years [Figure 3b].
Figure 3.

Intraoperative exposure of the tumor and post-operative frontal view after 1 year
Figure 4.
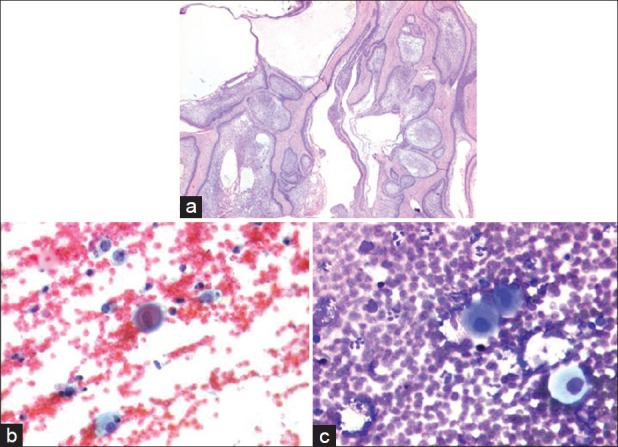
(a) H and E stained sections showing ameloblastoma with solid and cystic patterns. No squamous differentiation or nuclear atypia was seen (X40). (b and c) Fine needle aspiration cytology of the lesion. Squamous cells showing nuclear atypia admixed with foamy macrophages on a hemorrhagic background. (a) Papanicolaou stain (X400) (b) Giemsa stain (X400)
Discussion
Ameloblastoma is the second most common odontogenic tumor of the jaws. It is commonly seen in adults between 30 years and 50 years without gender predilection. Mandible is most commonly affected. Maxillary ameloblastomas are less common. It runs an indolent course and therefore remains asymptomatic for a long time and can attain massive sizes. The cosmetic deformity is commonly the presenting complaint.
Clinically, ameloblastomas are classified as (1) solid/multicystic (2) unicystic, (3) extraosseous/peripheral. Histologically, ameloblastoma shows follicular and plexiform patterns. Depending upon the differentiation, the follicular type is further divided into acanthomatous, desmoplastic, granular cell, basal cell, and clear cell and mixed variety.[1] Reichart et al., found the solid variant to be the most common (92%) while the unicystic (6%) and peripheral variants (2%) were rare. Follicular and Granular cell variants showed high recurrence rates.[8]
Various treatment modalities of “conservative” and “radical” surgery are described. Enucleation, cauterization or local curettage, are “conservative approaches” while segmental resection is referred to as “Radical.” Due to benign histology, it is likely that a conservative surgical approach may be favored. However, conservative treatment modalities have very high recurrence rates (90% for mandibular tumors, 100% for maxillary tumors).[1,8] Time for recurrence is highly variable, (Range 1-30 years, average 5 years).[1] Recurrence is attributed to inadequate removal, “seeding,” aggressive histology and spread along the muscle attachment.[1,3,4,5] Treatment of recurrence often mandates extensive ablative and reconstructive surgery with inherent morbidity, even in expert hands. It is burdensome to the patient, physically, psychologically, and financially. Use of radiotherapy for such cases has limited success.[9]
This patient had undergone segmental resection at initial surgery. We hypothesize that recurrence in the temporal region probably occurred due to retraction of temporalis muscle already infiltrated by tumor with/without a small fractured fragment of coronoid process (weakened due to existing pathology and fracturing during the surgical manipulation) [Figure 5].
Figure 5.
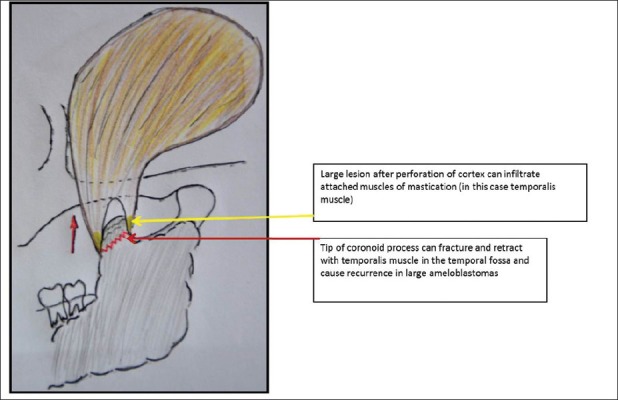
Schematic representation showing large ameloblastoma (grey shaded area) involving ramus coronoid and condyle of mandible
Histopathology is the gold standard to confirm the diagnosis of recurrences at such rare sites. In this case, the histopathological diagnosis (FNAC, biopsy) of squamous cell carcinoma was perplexing. FNAC of the lesion showed a few scattered epithelial cells resembling squamous cells with mild nuclear atypia, along with a few foamy macrophages [Figure 4 (b and c)]. Aspirates from lymph nodes harboring metastatic squamous carcinoma also shows similar features. Hence possibility of metastatic squamous carcinoma was considered. It is difficult to differentiate ameloblastic epithelial cells from squamous cells in FNAC due to overlapping morphological features. Small clusters of ameloblastic epithelial cells in core biopsy can resemble squamous cells. A scanty focus of ameloblastoma in core biopsy, hence can lead to suspicion of oral squamous cell carcinoma.
Ameloblastoma recurrences can occur at non-conventional sites such as temporal and infratemporal fossa. FNAC or core biopsy of these recurrent lesions may be inconclusive or even misleadingly suggestive of malignancy. Clinical examination and radiology are therefore of immense value. Good communication between surgeon, radiologist, and pathologist is of paramount importance.
Recurrences are due to incomplete removal at primary surgery, rather than de novo lesions. Strict adherence to the principles of ablative surgery, which include adequate surgical exposure, en bloc removal with adequate bony (1-1.5 cm) and soft-tissue margins, is mandatory. Intraoperative use of frozen section can help a thorough excision. The policy of including the next uninvolved anatomic structure for adequate clear margins must be followed.[1]
It is important to identify and define high-risk characteristics pre-operatively. Extensive bone destruction of the vertical ramus, coronoid, and condylar process are high-risk features and should be evaluated using Computerised tomography/magnetic resonance imaging (preferred) to look for infiltration of attached muscles. Similarly, maxillary ameloblastomas with erosion of bony walls are high risk tumors as they may infiltrate pterygoid muscles posteriorly or extend superiorly into orbital floor, paranasal sinuses. Clinico-radiological follow-up every year is necessary for these high-risk cases.
Acknowledgment
We thank Dr. Prabha Yadav, M.S., (Head, Plastic and Reconstructive services, Tata Memorial Hospital, Mumbai) and her team, also Dr. Prashant Pawar, Dr. Sourav Datta (Both, Fellow at Tata Memorial Hospital, Mumbai) for their invaluable contribution toward this patient's care.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Carlson ER, Marx RE. The ameloblastoma: Primary, curative surgical management. J Oral Maxillofac Surg. 2006;64:484–94. doi: 10.1016/j.joms.2005.11.032. [DOI] [PubMed] [Google Scholar]
- 2.Todd R, Gallagher GT, Kaban LB. Mass in the infratemporal fossa. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1997;84:116–8. doi: 10.1016/s1079-2104(97)90054-8. [DOI] [PubMed] [Google Scholar]
- 3.Al-Bayaty HF, Murti PR, Thomson ER, Niamat J. Soft tissue recurrence of a mandibular ameloblastoma causing facial deformity in the temporal region: Case report. J Oral Maxillofac Surg. 2002;60:204–7. doi: 10.1053/joms.2002.29826. [DOI] [PubMed] [Google Scholar]
- 4.Auluck A, Shetty S, Desai R, Mupparapu M. Recurrent ameloblastoma of the infratemporal fossa: Diagnostic implications and a review of the literature. Dentomaxillofac Radiol. 2007;36:416–9. doi: 10.1259/dmfr/45988074. [DOI] [PubMed] [Google Scholar]
- 5.To EW, Tsang WM, Pang PC. Recurrent ameloblastoma presenting in the temporal fossa. Am J Otolaryngol. 2002;23:105–7. doi: 10.1053/ajot.2002.30629. [DOI] [PubMed] [Google Scholar]
- 6.Chen WL, Li JS, Yang ZH, Wang JG, Zhang B. Recurrent ameloblastoma of the anterior skull base: Three cases treated by radical resections. J Craniomaxillofac Surg. 2006;34:412–4. doi: 10.1016/j.jcms.2006.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Oka K, Fukui M, Yamashita M, Takeshita I, Fujii K, Kitamura K, et al. Mandibular ameloblastoma with intracranial extension and distant metastasis. Clin Neurol Neurosurg. 1986;88:303–9. doi: 10.1016/s0303-8467(86)80051-8. [DOI] [PubMed] [Google Scholar]
- 8.Reichart PA, Philipsen HP, Sonner S. Ameloblastoma: Biological profile of 3677 cases. Eur J Cancer B Oral Oncol. 1995;31B:86–99. doi: 10.1016/0964-1955(94)00037-5. [DOI] [PubMed] [Google Scholar]
- 9.Gardner DG. Radiotherapy in the treatment of ameloblastoma. Int J Oral Maxillofac Surg. 1988;17:201–5. doi: 10.1016/s0901-5027(88)80033-x. [DOI] [PubMed] [Google Scholar]


