Abstract
Forced orthodontic eruption (FOE) is a non-surgical treatment option that allows modifying the osseous and gingival topography. The aim of this article is to present a clinical case of a FOE, which resulted in an improvement of the amount of available bone and soft-tissues for implant site development. Patient was referred for treatment of mobility and unesthetic appearance of their maxillary incisors. Clinical and radiographic examination revealed inflamed gingival tissue, horizontal and vertical tooth mobility and interproximal angular bone defects. It was chosen a multidisciplinary treatment approach using FOE, tooth extraction, and immediate implant placement to achieve better esthetic results. The use of FOE, in periodontally compromised teeth, promoted the formation of a new bone and soft-tissue in a coronal direction, without additional surgical procedures, enabling an esthetic, and functional implant-supported restoration.
Keywords: Bone remodeling, forced eruption, multidisciplinary treatment, orthodontic extrusion
Introduction
The presence of an unsatisfactory recipient site caused by alveolar ridge resorption in result of periodontal disease makes unfeasible the ideal 3-dimensional implant position in the anterior maxilla. In addition, the gingival contour follows the osseous crest resulting in severe esthetic problems that compromise subsequent prosthetic restoration. Thus, the replacement of a compromised anterior tooth by a dental implant remains one of the most difficult challenges for the dentists.[1]
In these situations, different surgical techniques such as guided tissue regeneration,[2] bone and connective graft procedures,[3,4] distraction osteogenesis,[5] and ridge splitting[6] have been widely used in clinical practice to increase the amount of available bone and/or gingival tissue at the potential implant site and improve implant esthetic and/or anchorage.
Instead of surgical traditional techniques, another approach to improve the 3-dimensional topography of the implant recipient site is the forced orthodontic eruption (FOE). This is a non-surgical treatment that aims to obtain hard and soft-tissue formation at potential implant sites, extruding orthodontically hopeless teeth and their periodontal apparatus.[7] Among the advantages of this technique are: Leveling of isolated infrabone defects, lengthening the clinical crown, repositioning of the gingival margin, improvement of primary anchorage of a dental implant and increased amount of attached gingiva and bone.[7] This bone and gingival augmentation improves the recipient implant site for a more esthetical restoration.
During the orthodontic extrusion, mechanical stresses exerted onto the alveolar bone led to activation of angiogenic growth factors, which would contribute to the formation of new support tissue: Gingival and periodontal fibers, and deposition of new bone via osteoblastic activity at the alveolar crest.[8] As tooth movement occurs in the coronally direction, the gingiva and the bone attached by the periodontal ligaments migrate in the same direction of the movement, resulting in a coronal shift of the bone at the base of the defect. FOE can also promote augmentation of soft- tissue volume through the increasing of the attached gingival. The only requirement for the satisfactory application of this procedure is that the apical third of the root must maintain an intact fiber apparatus and the patient should not present systemic problems such diabetes mellitus that impairs the bone healing.[7,9] The regeneration of periodontal tissue support allows the installation of implants and becomes foreseeable the results of the treatment.
According to Gkantidis et al.[10] harmonious cooperation of the general dentist, the periodontist and the orthodontist are necessary to increase the possibilities for the successfully treatment.[11] Although it is possible to find many articles in scientific dental literature about orthodontic extrusion treatment for periodontal regeneration, some authors reinforce the need to describe a case on the installation of implants after orthodontic extrusion. Therefore, the aim of this study was to report a clinical case of orthodontic extrusion of maxillary anterior incisors in a patient with periodontal disease for posterior implants rehabilitation.
Case Report
A 22-year-old woman was referred to the School of Dentistry at Araraquara, with the complaint of tooth mobility in the right maxillary lateral incisor. She was also disappointed with her prosthesis. Her medical history was non-contributory and her dental history revealed a root canal therapy and provisional restoration on the right maxillary lateral incisor. Clinical examination revealed that the tooth presented degree II of mobility, 5 mm probing depth in the interproximal surface and the gingival tissue surrounding the tooth was inflamed. The temporary acrylic resin crown presented some marginal infiltration, and after removing it, a cavity was found under the gingival tissue [Figure 1]. Periapical radiograph revealed bone resorption around the root, interproximal angular bone defects, and satisfactory canal treatment. Because it was impossible to obtain an adequate crown-root ratio after tooth treatment, it was decided with patient to extract the root orthodontically and to replace it by a dental implant.
Figure 1.

Clinical view showing of the temporary acrylic resin crown presented some marginal infiltration
It is important to note that this case report was planned with a multidisciplinary team, i.e., orthodontist, periodontist, and prosthodontist. The initial phase of treatment occurred with the reduction of control plaque accumulation and gingival inflammation. For this patient, the periodontal treatment and oral hygiene instruction were performed during 4 months, according to Gkanditis et al.[10]
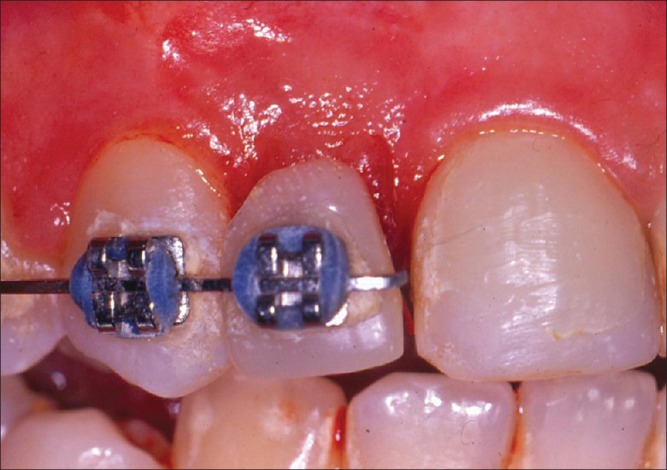
After 4 months, a careful clinical examination was made, the cavity was treated, the excess of gingival tissue was removed, and the temporary crown was replaced. The orthodontic treatment was initiated using the brackets with Roth prescription and the right lateral incisor bracket was positioned more cervically than those on the other tissues, in order to allow the tooth extrusion with a 0.016″ Ni-Ti wire. To help prevent intrusion of the anchorage teeth, a 0.019″ × 0.025″ stainless steel auxiliary arch was used [Figure 2a and f]. Patient was seen every 2 weeks for reduction of the incisal surface of the extruded tooth to prevent occlusal interferences during extrusive movement. Furthermore, the lateral incisor bracket was repositioned as close as possible to the gingival margin to allow a long extruding range. Periapical radiographs were taken monthly to monitor progress in the bone profile.
Figure 2.
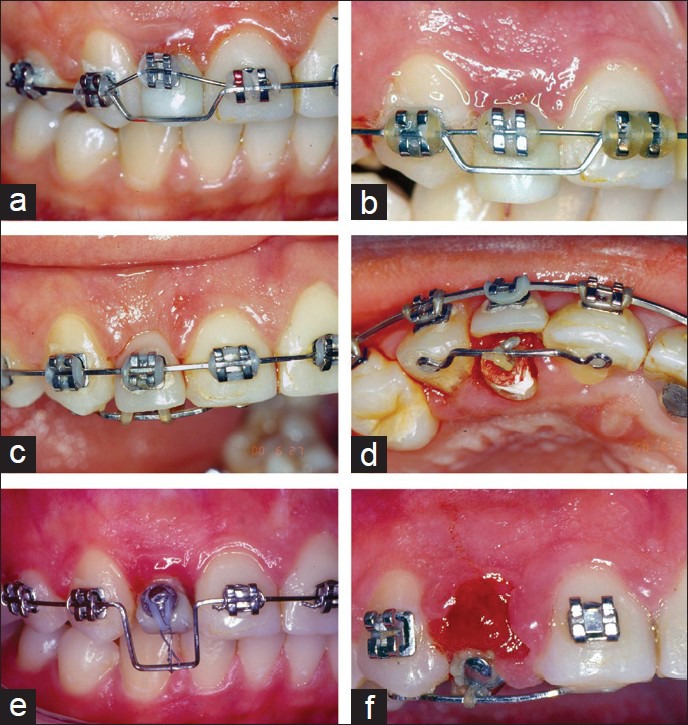
(a and f) The bracket positioned more cervically allowed the tooth extrusion with a 0.016″ Ni-Ti wire and the 0.019″ × 0.025″ wire prevented intrusion of the teeth
After 12 weeks of orthodontic extrusion, the tooth was stabilized for 4 months in order to get a proper reorganization of the soft-tissue, and bone remodeling [Figure 3a and c]. Before extraction of the maxillary right lateral incisor, it was possible to observe, clinical, and radiographically, a substantial interproximal and vertical bone formation and an increase in the amount of attached gingiva. After 15 months of orthodontic treatment, the lateral incisor was extracted [Figure 4] and an implant (3.3 mm × 11 mm implant, Neodent, Curitiba, Brazil) was placed immediately, remaining unloaded for 6 months until the osseointegration period [Figure 5]. The periapical radiographic evaluation showed osseointegration around of the implant 6 months after its installation [Figure 6]. After this time, a provisional restoration was confectioned for allowed the gingival recontouring [Figure 7].
Figure 3.
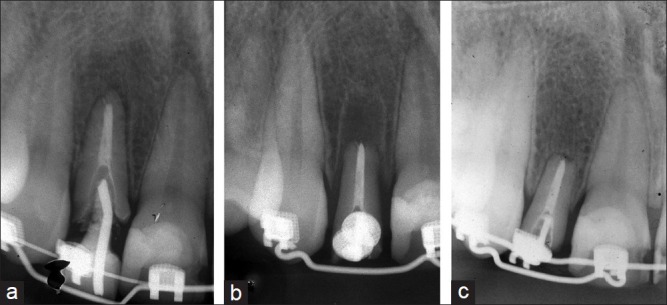
(a and c) Periapical radiographs to show bone topography on maxillary lateral incisor
Figure 4.
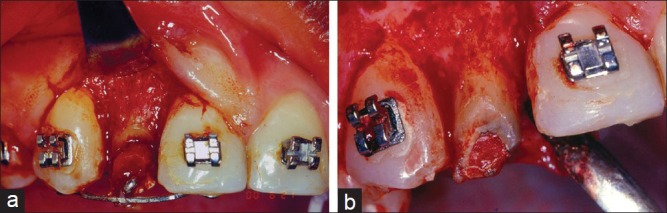
(a and b) Extrusion of the lateral incisor
Figure 5.
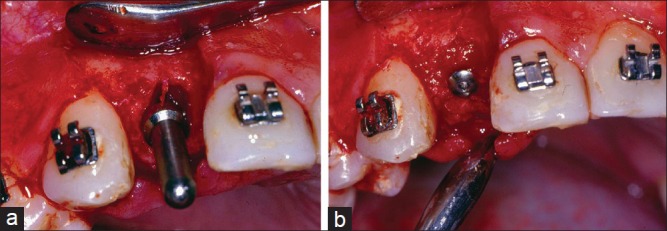
(a and b) Clinical view showing implant placement after tooth extraction (3.3 mm x 11 mm implant, Neodent, Curitiba, Brazil) placed immediately
Figure 6.
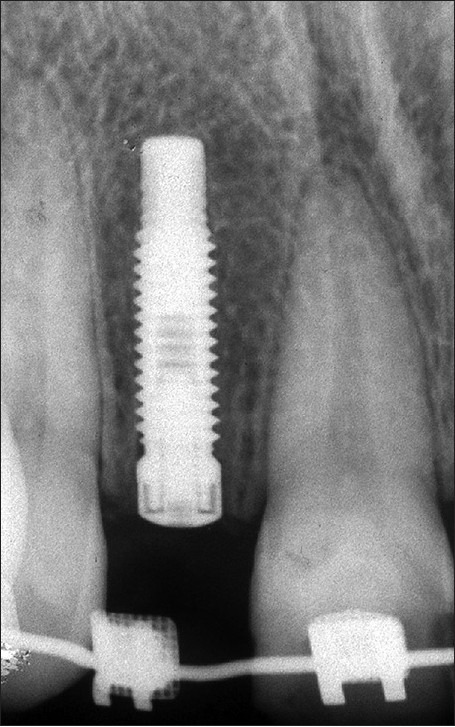
Periapical radiographs a week after implant placement
Figure 7.
Buccal view of the provisional restoration after 6 months of the implant placement
A definitive metal-ceramic crown was installed 1 year after implant placement [Figure 8]. After 5-year follow-up, the patient reported no complaints, and the dental implant was stable and healthy. Patient was very satisfied with the aesthetic result.
Figure 8.

Buccal view of the definitive metal-ceramic crown
Discussion
This case described a successful FOE procedure in hopeless teeth, for implant site development that did not have enough bone and soft-tissue to support it. The multidisciplinary treatment for these patients included: Basic periodontal therapy for adequacy of the oral environment, FOE to avoid ridge collapse after extraction and to improve the amount of bone and soft-tissues, teeth extraction, immediate implant and fixed provisional crowns placement. This treatment protocol was used with success to restore functional and esthetic in a maxillary compromised anterior teeth.
FOE is a non-invasive method to increase the amount of keratinized gingiva and bone, improving the 3-dimensional topography of the periodontal apparatus. This approach allows optimization of the implant recipient site prior to tooth extraction through a better engagement of bone during implant placement.[12,13] The increase in bone and gingival volume is resulted from the stretching of gingival and periodontal fiber bundles. When tension is applied to the periodontal ligament through orthodontic extrusion movement, periodontal fibers are elongated and osteoblastic activity induces bone formation at the alveolus base. Studies have demonstrated that when tooth is extruded by using light forces, the gingiva follows bone formation in a coronal direction.[14]
The regeneration of periodontal tissue support allows the installation of implants and becomes foreseeable the results of the treatment. However, it was recommended that in patients with periodontal disease, orthodontic treatment should start 2-6 months after periodontal therapy to allow for periodontal healing and stabilization.[10] At the same time, the light continues forces should be implemented for efficient tooth movement in a compromised periodontium, i.e., constant orthodontic forces that produce an extrusion rate of ≤2 mm/month is ideal.[15]
The use of implant for a single tooth replacement in the anterior region is one of the greatest challenges in esthetic dentistry.[1] The main objectives of such procedures include successful osseointegration of the dental implant, health of the surrounding soft and hard tissues, and balance between the final restoration and the adjacent teeth. An important factor to achieve esthetic success in an esthetic zone is the quality of the alveolar bone (height, volume, and density of the cortical plate) at the implant site, once the gingival contour follows the underlying osseous crest. The integration of orthodontics and implant dentistry provides a better option in a clinical situation comparing to invasive procedures.
Tooth extraction in the anterior maxillary area usually cause defects of the alveolar ridge. An increased interoclusal space can be expected after the extraction that results in restoration with an unfavorable crown-to-implant ratio, causing crestal bone loss around the implant or an increase in the risk of mechanical problems like screw loosening. Forced eruption is an interesting alternative to prevent ridge resorption and also, to increase the amount of bone and soft-tissues before implant placement. Furthermore, forced eruption has been effective in periodontal correction of angular bony defects, in repositioning the gingival margin, in reducing the probing depth and in clinical lengthening of the crown.[7]
Dental implants require enough amount of vertical bone. Vertical augmentation, especially of the buccal bone plate and crest, allows better implant placement. Autogenous block grafts allow the reconstruction of atrophic ridges. However, there are complications related to this autograft: Morbidity, bleeding, nerve injury, pain, swelling, graft failure, dehiscence and others.[16] Moreover, the tooth needs to be extracted and implant installation can’t be achieved because the bone remodeling takes 6-9 months before implants can be placed.
On the other hand, FOE of the compromised maxillary anterior teeth allows vertical bone augmentation and also, the immediate replacement of a tooth with a fixed-implant provisional prosthesis, without any additional surgical procedure.[11] The key factor for the success of FOE is the application of appropriate orthodontic forces and sufficient retention period after extrusion allowing the stabilization of the tissues.[17] The disadvantages of this procedure are: Longer treatment time, additional orthodontic treatment, and patient cooperation. This procedure is indicated in cases of moderate bony defects and recession of up to the middle-third of the root. However, FOE is more advantageous when minimally invasive procedures are performed.[17] Teeth with endodontic periapical lesions, gingival recession with severe buccal bone resorption, ankylosed teeth, and severe circumferential and angular defects are contraindicated for orthodontic extraction.[18]
In this case report, after the initial forced eruption therapy, the alveolar bone crest and the gingival margin were located in normal relation to the tissues of the adjacent teeth. Surgical procedures, including extraction and implant placement, were performed with minimal trauma preserving the buccal bone. This situation allowed an adequate primary stabilization, appropriate emergency profile, and crown-implant ratio. Consequently, it was possible to make an immediate provisional restoration, favoring the achievement and maintenance of the esthetic results.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
References
- 1.Solakoglu O, Cooper LF. Immediate implant placement and restoration in the anterior maxilla: A tissue-related approach. Observations at 12 months after loading. Int J Periodontics Restorative Dent. 2006;26:571–9. [PubMed] [Google Scholar]
- 2.Zitzmann NU, Schärer P, Marinello CP. Long-term results of implants treated with guided bone regeneration: A 5-year prospective study. Int J Oral Maxillofac Implants. 2001;16:355–66. [PubMed] [Google Scholar]
- 3.Winkler S. Implant site development and alveolar bone resorption patterns. J Oral Implantol. 2002;28:226–9. doi: 10.1563/1548-1336(2002)028<0226:ISDAAB>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 4.de Molon RS, de Avila ÉD, de Souza JA, Nogueira AV, Cirelli CC, Cirelli JA. Combination of orthodontic movement and periodontal therapy for full root coverage in a Miller class III recession: A case report with 12 years of follow-up. Braz Dent J. 2012;23:758–63. doi: 10.1590/s0103-64402012000600022. [DOI] [PubMed] [Google Scholar]
- 5.Aparicio C, Jensen OT. Alveolar ridge widening by distraction osteogenesis: A case report. Pract Proced Aesthet Dent. 2001;13:663–8. [PubMed] [Google Scholar]
- 6.Shimoyama T, Kaneko T, Shimizu S, Kasai D, Tojo T, Horie N. Ridge widening and immediate implant placement: A case report. Implant Dent. 2001;10:108–12. doi: 10.1097/00008505-200104000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Salama H, Salama M. The role of orthodontic extrusive remodeling in the enhancement of soft and hard tissue profiles prior to implant placement: A systematic approach to the management of extraction site defects. Int J Periodontics Restorative Dent. 1993;13:312–33. [PubMed] [Google Scholar]
- 8.Shiu YT, Weiss JA, Hoying JB, Iwamoto MN, Joung IS, Quam CT. The role of mechanical stresses in angiogenesis. Crit Rev Biomed Eng. 2005;33:431–510. doi: 10.1615/critrevbiomedeng.v33.i5.10. [DOI] [PubMed] [Google Scholar]
- 9.de Molon RS, Morais-Camilo JA, Verzola MH, Faeda RS, Pepato MT, Marcantonio E., Jr Impact of diabetes mellitus and metabolic control on bone healing around osseointegrated implants: Removal torque and histomorphometric analysis in rats. Clin Oral Implants Res. 2013;24:831–7. doi: 10.1111/j.1600-0501.2012.02467.x. [DOI] [PubMed] [Google Scholar]
- 10.Gkantidis N, Christou P, Topouzelis N. The orthodontic-periodontic interrelationship in integrated treatment challenges: A systematic review. J Oral Rehabil. 2010;37:377–90. doi: 10.1111/j.1365-2842.2010.02068.x. [DOI] [PubMed] [Google Scholar]
- 11.de Avila ED, de Molon RS, de Assis Mollo F, Jr, de Barros LA, Capelozza Filho L, de Almeida Cardoso M, et al. Multidisciplinary approach for the aesthetic treatment of maxillary lateral incisors agenesis: Thinking about implants? Oral Surg Oral Med Oral Pathol Oral Radio. 2012;114:e22–8. doi: 10.1016/j.oooo.2011.09.023. [DOI] [PubMed] [Google Scholar]
- 12.Mirmarashi B, Torbati A, Aalam A, Chee W. Orthodontically assisted vertical augmentation in the esthetic zone. J Prosthodont. 2010;19:235–9. doi: 10.1111/j.1532-849X.2009.00563.x. [DOI] [PubMed] [Google Scholar]
- 13.Holst AI, Nkenke E, Blatz MB, Geiselhöringer H, Holst S. Prosthetic considerations for orthodontic implant site development in the adult patient. J Oral Maxillofac Surg. 2009;67:82–8. doi: 10.1016/j.joms.2009.07.010. [DOI] [PubMed] [Google Scholar]
- 14.Mantzikos T, Shamus I. Forced eruption and implant site development: An osteophysiologic response. Am J Orthod Dentofacial Orthop. 1999;115:583–91. doi: 10.1016/s0889-5406(99)70284-2. [DOI] [PubMed] [Google Scholar]
- 15.Korayem M, Flores-Mir C, Nassar U, Olfert K. Implant site development by orthodontic extrusion. A systematic review. Angle Orthod. 2008;78:752–60. doi: 10.2319/0003-3219(2008)078[0752:ISDBOE]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 16.Pikos MA. Atrophic posterior mandibular reconstruction utilizing mandibular block autografts: Risk management. Int J Oral Maxillofac Implants. 2003;18:765–6. [PubMed] [Google Scholar]
- 17.Owman-Moll P, Kurol J, Lundgren D. Effects of a doubled orthodontic force magnitude on tooth movement and root resorptions. An inter-individual study in adolescents. Eur J Orthod. 1996;18:141–50. doi: 10.1093/ejo/18.2.141. [DOI] [PubMed] [Google Scholar]
- 18.Holst S, Hegenbarth EA, Schlegel KA, Holst AI. Restoration of a nonrestorable central incisor using forced orthodontic eruption, immediate implant placement, and an all-ceramic restoration: A clinical report. J Prosthet Dent. 2007;98:251–5. doi: 10.1016/S0022-3913(07)00266-1. [DOI] [PubMed] [Google Scholar]


