Abstract
Introduction:
Lacidipine (LCDP) is chemically a “1, 4-dihydropyridine derivative” Ca+2 channel blocker used as an antihypertensive. Type and extent of packaging have a strong influence on the photo-stability of the 1,4-dihydropyridine derivatives. In standard, light protection of drug substance/drug product can be obtained either by use of an opaque additive in the formulation that competitively absorbs or reflects light reaching the sample and/or by blocking the access of light to the drug through external protection by packaging.
Materials and Methods:
External protection by covering tablets with an opaque film coating involving a light-reflecting inorganic pigment such as titanium dioxide and/or by using an opaque impermeable packaging material was an appropriate suitable option for establishing photo-stability. Thus, the main objective of the present study was to optimize the % level of film coating in LCDP core tablets, and selection of a final packaging material and its respective extent, that is, primary, secondary and/or tertiary packaging, for LCDP tablets.
Results and Conclusion:
The main objective (% level of film coating) was optimized by directly exposing core tablets, 1% w/w, 2% w/w and 3% w/w film-coated tablets, to a light source as per Option-2 of ICH Q1B and its comparative analysis at the end of light exposure testing. The other objective (extent of drug product packaging) was established successfully by assessing whether or not an acceptable change has occurred at the end of the light exposure testing of the LCDP film-coated tablets in a direct exposure study or a primary immediate pack and/or secondary marketing pack.
Keywords: Alu–Alu blister, film coating, folding box board carton, immediate pack, lacidipine, marketing pack, oriented poly amide, photodegradation, photo-stability, polyvinyl chloride
INTRODUCTION
Lacidipine (LCDP) is chemically designated as E-4-{2-[3-(1,1-dimethylethoxy)-3-oxo-1-propenyl] phenyl}-1,4-dihydro-2, 6-di-methyl-3,5-pyridine-dicarboxylic acid diethyl ester, which is pharmacologically a “calcium channel blocker” used as an antihypertensive. The active trans form is used in therapy.[1] 1,4-Dihydropyridines, so-called calcium channel blockers, serve to treat hypertension and coronary diseases.[2] The drug is sensitive to light, in line with the well-known photosensitivity of the dihydro-pyridine compound class.[3,4] In principle, light protection can be obtained either by blocking the access of light to the drug with external protection or by the use of an additiv e in the finished product formulation that competitively absorbs or reflects light reaching the sample. In the case of tablets or capsules, external protection from packaging is generally suitable,[5] and can be obtained by using an opaque blister or an opaque gelatine shell for capsules or covering tablets with an opaque film. The opaqueness can be obtained by adding a pharmaceutically acceptable dye the absorption spectrum of which is the same as that of the drug principle or by adding a reflecting pigment such as titanium dioxide.[6,7]
The intrinsic photo-stability characteristics of any new drug substances and products should be evaluated to demonstrate that light exposure does not result in any unacceptable change. The ICH Q1B guideline primarily addresses the generation of photo-stability information for submission in registration applications for new molecular entities and associated drug products.[8] A systematic approach to photo-stability testing is recommended covering, as appropriate, studies such as:
-
(i)
Tests on the drug substance;
-
(ii)
Tests on the exposed drug product outside of the immediate pack, and if necessary,
-
(iii)
Tests on the drug product in the immediate pack, and if necessary,
-
(iv)
Tests on the drug product in the marketing pack.
Thus, the main objective of the present photo-stability study is to optimize the % level of film coating in the finished product formulation, and selection of packaging material and its extent, that is, primary, secondary and/or tertiary packaging for the finished product. The extent of drug product testing was established by assessing whether or not an acceptable change (mainly in terms of impurities generated by different factors[9] as represented in Figure 1) has occurred at the end of the light exposure testing as described in the proposed decision flow chart for photo-stability testing of drug products as represented in Figure 2. Acceptable change is a change within the limits of justified specifications as per current version of British Pharmacopoeia.
Figure 1.

Chemical structure of LCDP (pure dihydropyridine trans isomer), solvent impurity (A: methyl derivative), temperature impurity (B: pyridine) and light impurity (C: cis isomer and its cyclic derivative)
Figure 2.
Proposed decision flow chart for photo-stability study of LCDP film-coated tablets with respect to optimization of % film coating level, and selection of packaging material and its respective extent (immediate pack and/or marketing pack)
MATERIALS AND METHODS
LCDP was procured from Cadila Pharmaceuticals Limited (Ankleshwar, India). Polyvinyl pyrrolidone (Plasdone® K29/32) was purchased from ISP Pharmaceuticals (New Jersey, USA). Lactose monohydrate (Pharmatose® 200M and DCL® 11) purchased from DFE Pharma (Goch, Germany) used as an intra-granular diluent cum powder substrate. Absolute alcohol (ethanol 99.6% v/v) was procured from Chalthan Vibhag Khand Udyog Sahkari Mandali Limited (Surat, India). Magnesium stearate of vegetable grade was purchased from Ferro Synpro (Ohio, USA). Pre-mixed film coating material, Opadry® II White (composed of lactose (film former) and polyethylene glycol (plasticizer) in a 5:1 w/w ratio with titanium dioxide as an inorganic pigment), which can be readily dispersible in water, was purchased from Colorcon Asia Pvt Limited (Goa, India).
LCDP is a, once-a-day, orally administered, 1,4-dihydropyridine-derived “calcium channel blocker” and an antihypertensive with an intrinsically slow onset of activity ensuing in lack of reflex tachycardia with a long duration of action and a high degree of vascular selectivity.[10] But the quandary is that LCDP is a Bio-pharmaceutics (BCS) class-IV drug with low solubility and highly variable permeability, presenting a challenge to formulation scientists.[11] Thus, solvent evaporation by the fluidized bed process (FBP) was selected as a method of choice for formulation by solid dispersion; as it improves wettability with simultaneous increase in the porosity of granules. Moreover, it also decreases the crystalline structure of the drug and promotes its conversion to a more soluble amorphous form.[12] An optimized formulation having the desired disintegration and dissolution rate comprises LCDP, carrier (PVP), diluent and lubricant, wherein the weight ratio of LCDP to carrier is 1:10, with a definite intra-granular lactose (Pharmatose 200M) to extra-granular lactose ratio (DCL 11) of 80:20 and magnesium stearate as represented in Table 1a. Moreover, as LCDP is a highly variable drug product, thus the FBP parameters should be precisely controlled to produce the intended robust product as per predefined QTPP.
Table 1a.
Optimized LCDP formulation

At a pilot scale, for FBP (Pam-Glatt®-GPCP2), LCDP was first dissolved in ethanol (99.6% v/v) with stirring at slow speed until a clear solution was obtained. To this solution, PVP-K29/32 was slowly added with continuous stirring until a clear yellow solution was obtained. To carry out top spray fluidized bed granulation, 40# sifted lactose monohydrate (Pharmatose 200M) was loaded in the fluidized bed processor and granulated by spraying the drug carrier solution (LCDP-PVP K29/32) for moistening the lactose powder substrate using top spray mechanics on the fluidized bed as per Table 1a, while peristaltic pump rpm, spray rate and atomization air pressure were very slowly increased to optimum and recorded intermittently in every 10 min.
After completion of granulation, fluidized bed drying was carried out in the same FBP using the parameters declared in Table 1b, until the desired constant Loss on Drying (LOD) specifically from 1.5 to 2.5% w/w at 105°C was achieved. Dried granules were sifted through a 20# screen in a mechanical sifter. The dried sifted granules were mixed in a double-cone blender for 5 min at 10 ± 2 rpm with 40# pre-sifted spray dried lactose (Pharmatose DCL 11) and lubricated with 60# pre-sifted magnesium stearate. Finally, the lubricated granules were compressed using 12.7 × 7.1 mm oval punches using the parameters listed in Table 1c using a 16-station rotary tablet compression machine (RIMEK®). Film coating was carried out using a 24” auto coater (Ganscoater®) at an inlet temperature of 60 ± 10 °C with an Opadry II White (comprising lactose (film former) and polyethylene glycol (plasticizer) in a 5:1 w/w ratio with titanium dioxide as an inorganic pigment) suspension until the desired weight gain from 1% to 3% w/w was achieved. Appropriate quantities of samples with different weight gains, that is, 1%, 2% and 3%, were collected during film coating and packed in different packs for exposure in the photo-stability study as per ICH Q1B.
Table 1b.
FBP parameters
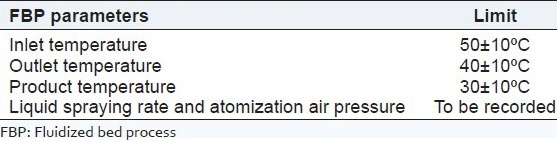
Table 1c.
Compression parameters

Usually, photo-stability studies of drug products should be carried out in a sequential manner starting with testing the directly exposed drug product then progressing as necessary to the product in the immediate pack and then if required in the marketing pack. Testing should progress until the results demonstrate that the drug product is adequately protected from exposure to light.
Light source, temperature and relative humidity in a photo-stability chamber
For photo-stability testing, a cool, white, fluorescent lamp designed to produce an output similar to that specified in ISO 10977 (1993) and a near-UV fluorescent lamp having a spectral distribution from 320 to 400 nm (with maximum energy emission between 350 and 370 nm; a significant proportion of UV in both bands of 320-360 nm and 360-400 nm) of ICH Q1B (Option-2) were used in the photo-stability chamber (Model no: TP 200S) manufactured by Thermolab Scientific Equipments (Thane, Maharashtra, India).[13] Samples were exposed to the cool white fluorescent light providing overall illumination of not less than 1.2 million lux hours and an integrated near-UV energy of not less than 200 W h/m2. The controls of temperature and relative humidity were maintained appropriately constant throughout within 25 ± 2°C and 60 ± 5% relative humidity, respectively, to minimize the effect of localized temperature and humidity changes.
Selecting locations for samples in the photo-stability chamber
Lux meter and light meters were used to read the intensity of the cool, white, fluorescent light and near-UV fluorescent light, respectively, at a particular location in the photo-stability chamber. The probe of the meter was inserted through the hole provided in the chamber, and kept at any location on the tray. The hole was closed with the cap. White fluorescent and UV lamps were switched on. The readings on the meters were recorded. Then the lamps were switched off and the chamber was opened. The probe was removed and kept at different locations on the tray in the chamber and the above procedure was repeated. It was made sure that the chosen locations had nearly similar intensity to minimize variations in exposure to the light between the test and control samples. With nearly similar intensity of light, the test and control samples were loaded at the same location on the same day and at the same time.
Calculating duration of light exposure of samples
Detailed understanding of the actual explanation of the calculation of exposure time for both the cool, white, fluorescent light and near-UV fluorescent light has been provided in sub-sections “For cool, white, fluorescent lamp designed to produce an output similar to outdoor daylight as defined in ISO 10977 (D65)” and “For cool, white, fluorescent lamp designed to produce an output similar to outdoor daylight as defined in ISO 10977 (D65)”. For explanation of the calculation steps for light exposure duration, it was assumed that the intensity of the cool, white, fluorescent light and near-UV fluorescent light at particular location in the chamber for both test and control samples was [X] lx and [U] W/m2, respectively.[14]
For the cool, white, fluorescent lamp designed to produce an output similar to outdoor daylight as defined in ISO 10977 (D65)
For the test and control samples to get exposed to 1.2 million lux hours, they have to be kept in the photo-stability chamber for the following number of days:
[X] lx × [Y] h = [1.2 × 106] lx h
[Y] = 1.2 × 106 lx h/[X] lx
Converting hours into number of days = [Y] h/24 h = [Z] day(s)
For the near-UV fluorescent lamp designed to produce an output similar to indoor indirect daylight standard (ID65)
For the test and control samples to get exposed to 200 W h/m2, they have to be kept in the photo-stability chamber for the following number of days:
[U] W/m2 × [V] hours = 200 W h/m2
[V] = 200 W h/m2/[U] W/m2
Converting hours into number of days = [V] hours/24 hours = [W] day(s)
Presentation of samples
Different sets of samples of drug substance and drug products were required to be prepared for three main objectives: (i) Optimization of % weight gain in film coating and (ii) selection of suitable packaging material for the finished product.
The extent of drug product testing was established by assessing whether or not acceptable change has occurred at the end of the light exposure testing as described in the proposed decision flow chart for photo-stability testing of drug product as represented in Figure 1. Acceptable change is considered a change within the British Pharmacopoeial limits for LCDP Tablets.
Possible interactions between the samples and any packaging material or for general protection of the sample was also considered and eliminated wherever not relevant to the test being carried out. The samples were positioned to provide maximum area of exposure to the light source, that is, if the test product is to be directly exposed to light then it should be placed in a dish in a single layer and if testing of the drug product in the immediate container or as marketed was required, the samples were placed horizontally or transversely with respect to the light source for the most uniform exposure of the samples.
Analysis of samples
At the end of the exposure period, samples were examined for any changes in physical properties (e.g., appearance, disintegration and dissolution) and analyzed for assay and Related Substances by a suitably validated analytical method.[15,16] When LCDP API was involved, sampling was ensured by a representative portion that was to be used in individual tests. For LCDP tablets, testing was conducted on an appropriately sized composite of 20 tablets. The analysis of the exposed sample was performed concomitantly with that of protected samples used as dark controls.
Sample preparations for assay and related substances procedures (by HPLC)
Standard preparations
A 20-mg weight of an LCDP working standard was accurately weighed and transferred into a 100 ml volumetric flask; 20 ml of absolute ethanol was added and sonicated to dissolve. It was diluted to 100 ml with n-hexane. For the assay procedure, 1 ml of this solution was further diluted to 100 ml with mobile phase (final concentration about 2.0 μg/ml). For the related substance (RS) procedure, 1 ml of the assay standard solution was further diluted to 100 ml with mobile phase (final concentration about 2.0 μg/ml).
Sample preparations
Solution (1): 20 tablets were taken, weighed and powdered. Tablet powder equivalent to 10.0 mg of LCDP was accurately weighed and transferred into the quantity of to a 50-ml volumetric flask. About 10 ml of absolute alcohol was added and sonicated for 10 min. Further, 30 ml of n-hexane was added and sonicated for 10 min with intermittent shaking and diluted to volume with n-hexane. A 5-ml volume of the solution was filtered through a 0.45-μm membrane filter (Millipore Millex is suitable).
Solution (2): 1 volume of Solution (2) of assay was diluted to 100 volumes with the mobile phase.
Solution (3): 1 volume of a 0.1% w/v solution of LCDP impurity standard BPCRS was diluted in absolute ethanol to five volumes with the mobile phase.
Mobile phase: 3 volumes of absolute alcohol and 97 volumes of n-hexane.
Chromatographic parameters: A liquid chromatograph is equipped with a variable-wavelength photo diode array detector, an injector and a data processor.
Column: A stainless steel column (25 cm × 4.6 mm) packed with cyanosilyl silica gel for chromatography (5 μm) (Spherisorb CN is suitable)
Flow rate: 2.0 ml/min
Detection wavelength: 240 nm
Injection volume: 20 μl
Procedure for assay
Solution (1) was injected (in duplicate) into the chromatograph. Chromatograms were recorded and the principal peak area was measured. The percentage of LCDP was calculated by using the following formula:
![]()
Where, Au = Average area of LCDP obtained with the sample preparation.
As = Average area of LCDP obtained with replicate injections of the standard preparation.
W1 = Weight of the LCDP working standard (mg).
W2 = Weight of sample (mg).
Avg. wt = Average weight of LCDP tablets.
LC = Label claim of LCDP tablet.
P = Potency of the LCDP working standard in percentage on an as-is basis.
Procedure for RS
A single injection of a blank and solution (1) was injected into the chromatograph. Any peak due to the blank was disregarded. Chromatograms were recorded and the area response of peaks was measured. The percentage of individual impurity was calculated by using the following formula: Any peak with a relative retention time of 1.5 was disregarded with respect to the peak due to LCDP impurity B:

Where, Au = Area of Impurity B obtained with the sample preparation (Solution (1)).
As = Average area of LCDP peak obtained with replicate injections of the standard preparation (Solution (2)).
W1 = Weight of the LCDP working standard (mg).
W2 = Weight of sample taken (mg).
W3 = Average weight of tablet (mg).
LC = Label claim of LCDP (mg).
P = Potency of the LCDP working standard in percentage on an as-is basis.
CF = Correction factor of impurity B (2.0)

Where, Au = Area of any other secondary impurity obtained with the sample preparation (Solution (1)).
As = Average area of LCDP peak obtained with replicate injections of the standard preparation (Solution (2)).
W1 = Weight of the LCDP working standard (mg).
W2 = Weight of sample taken (mg).
W3 = Average weight of tablet (mg).
LC = Label claim of LCDP (mg).
P = Potency of the LCDP working standard in percentage on an as-is basis.
Total impurities = Sum of % of all individual impurities (% w/w)
Procedure for dissolution
Dissolution was carried out using BP Dissolution Apparatus II. A paddle-stirring assembly was used and the following parameters were maintained:
Medium: 1% Polysorbate 20 in purified water (mi × 100 ml water with 10 ml Polysorbate 20, shaking gently and diluting to 1000 ml with water).
Volume: 500 ml
rpm: 50
Temperature: 37°C ± 0.5°C
Standard preparation
A 20.0-mg weight of the LCDP working standard was accurately weighed and transferred to a 100-ml volumetric flask. It was dissolved and diluted to volume with absolute ethanol, mixed well and used as stock solution. A 4-ml volume of the stock solution was diluted to 100 ml with dissolution medium and used as the standard preparation (final concentration: 8.0 μg/ml).
Sample preparation
The parameters of the instrument were set as mentioned in the test method and the medium was degassed prior to use. One tablet was transferred into each of six different vessels using 500 ml of medium and the apparatus was operated for exactly 45 min. At time points of 10, 15, 20, 30 and 45 min, 10 ml of the solution was withdrawn from the midway zone between the surface of the medium and the top of the rotating paddle not less than 1 cm from the vessel wall and same 10 ml was replaced with dissolution media for correction. The sampled solution was filtered through a 0.20-μm membrane filter that was first activated with 3 ml of methanol followed by 5 ml of a 1% w/v solution of Polysorbate 20, discarding the first 5 ml of the filtrate. This solution was used as the test preparation (final concentration of LCDP in the sample: 8.0 μg/ml for LCDP 4-mg tablets). Absorbance of the standard preparation (six times) and sample preparation (once) was measured with a suitable spectrophotometer at a wavelength of maximum absorbance of 284 nm against the medium as blank. Percentage of LCDP dissolved was calculated in individual tablet using the following formula:
![]()
Where, Au = Absorbance of the sample preparation.
As = Average absorbance of the standard preparation.
W1 = Weight of the LCDP working standard (mg).
P = Potency of the LCDP working standard in percentage, on an as-is basis.
RESULTS AND DISCUSSIONS
Light source and temperature in the photo-stability chamber
For conducting the photo-stability study of LCDP tablets (4 mg) the photo-stability chamber manufactured by Thermolab Scientific Equipments (instrument ID: CD/STB/007) having an operation capacity of 200 l was utilized. As per ICH Q1B Option-2, it was equipped with both cool, white fluorescent, light and near-UV-A light, with an average cool, white, fluorescent light reading of 2000 lx and an average near-UV-fluorescent light reading of 0.32 W/m2. Temperature was maintained appropriately within the very narrow range of 25 ± 2°C (23-27°C) throughout to minimize the effect of localized temperature changes within the photo-stability chamber.
Calculating the duration of light exposure of the samples
Samples were exposed to light as per the final actual decision flow chart for LCDP tablets as represented in Figure 2 providing overall illumination of not less than 1.2 million lux hours and integrated near-UV energy of not less than 200 W h/m2 to allow direct comparisons to be made between the drug products.
For the cool, white, fluorescent lamp designed to produce an output similar to outdoor daylight as defined in ISO 10977 (D65)
The average intensity of the cool, white, fluorescent light source that is designed to produce an output similar to the D65 (internationally recognized standard for outdoor daylight) in the photo-stability chamber was 2000 lx. For the test sample and for control sample to get exposed to overall illumination of not less than 1.2 million lux hours from the light source designed to produce an output similar to the D65, it has to be kept in the photo-stability chamber for the following number of days:
2000 lx × (X) = 1.2 × 106 lx h
[X] = 1.2 × 106 lx h/2000 lx = 600 h, where X is the total hours of light exposure required.
Converting hours into number of days = 600 h/24 h = 25 days. Thus actually, 25 days were required for the samples to get exposed to illumination of 1.2 million lux hours.
For the near-UV fluorescent lamp designed to produce an output similar to indoor indirect daylight standard (ID65)
Similarly, the average intensity of the near UV–fluorescent light source that was designed to produce an output similar to the ID65 (internationally recognized standard for indoor indirect daylight) in the chamber was 0.32 W/m2. For the test sample and control sample to get integrated near-UV light energy with output similar to the ID65 (ID65 is equivalent indoor indirect daylight standard) of not less than 200 W h/m2, it had to be kept in the photo-stability chamber for the following number of days:
0.32 W/m2 × UV hours = 200 W h/m2
[UV] = (200 W h/m2)/(0.32 W/m2) =625 h
(where as Y is the total hours of light exposure required).
Converting hours into number of days = 625 h/24 h = 26.04 days.
Thus actually, 26.04 days were required for the samples to get integrated near-UV light energy of not less than 200 W h/m2. From the above calculations, both the test and control samples had been exposed to a maximum of 27 days to both lights simultaneously, providing overall illumination of not less than 1.2 million lux hours and integrated near-UV energy of not less than 200 W h/m2.
Presentation of samples
For optimization of %w/w film coating level in finished product formulation
-
(i)
As a positive control: LCDP core tablets were directly exposed outside from the immediate pack in an open Petri dish spread in a single layer for uniform exposure.
-
(ii)
As a test product: LCDP core tablets were coated with three different levels of film coating, that is, 1% w/w, 2% w/w and 3% w/w, which were directly exposed outside from the immediate pack in an open Petri dish spread in a single layer for uniform exposure for comparison of the photo-stability of the finished product for optimization of film coating level in the finished product.
-
(iii)
As a negative control: 2% Film-coated tablets of LCDP were exposed in a closed Petri dish covered with aluminum foil to evaluate the contribution of thermally induced changes to the total observed change.
For selection of packaging material for optimized finished product formulation
-
(i)
As a positive control: LCDP film-coated tablets were directly exposed outside from the immediate pack in an open Petri dish spread in a single layer for uniform exposure.
-
(ii)
As a primary test pack: LCDP film-coated tablets were exposed in the immediate pack, that is, 7's count Alu–Alu blister (cold-formed foil: made up of a 25-μm OPA (Oriented Poly Amide) film/adhesive/45-μm aluminum foil/adhesive/60-μm PVC (polyvinyl chloride) film).
-
(iii)
As a marketing test pack: LCDP film-coated tablets were exposed in the marketing pack, that is, 7's count Alu–Alu blister placed in a reverse tack folding paper box board carton of 300 gsm (grammage) with UV varnish.
-
(iv)
As a negative control: LCDP film-coated tablets were exposed in a closed Petri dish covered with aluminum foil to evaluate the contribution of thermally induced changes to the total observed change.
RESULTS OF ANALYSIS OF SAMPLES WITH ACCEPTANCE CRITERIA
The extent of drug product testing was established by assessing whether or not acceptable change had occurred at the end of the light exposure testing as described in the actual decision flow chart for photo-stability testing as represented in Figure 3. Acceptable change is change within limits justified, that is, NMT (−) 5% for assay and dissolution value, and NMT (+) 0.1% for related substances (impurities). At the end of the exposure period, the samples were examined and analyzed for tests against the specified limits and results are mentioned in Tables 2 and 3.
Figure 3.

Actual decision flow chart for photo-stability study of LCDP film-coated tablets with respect to optimization of % film coating level, and selection of packaging material and its respective extent (primary immediate pack and secondary marketing pack)
Table 2.
Results for photo-stability study for optimization of % w/w film coating level in finished product formulation

Table 3.
Results for photo-stability study for selection of packaging material for optimized finished product formulation

CONCLUSION
From the results of the optimization study of % weight gain in film coating by conducting a photo-stability study, the following conclusion can be made successively:[17] (i) When LCDP core (uncoated) tablets were directly exposed to light, there was a significant change observed in Related Substances, that is, more than +0.1% profile of the finished product. When 1% w/w film-coated tablets were directly exposed to light, a significant change was observed in assay and dissolution, and the RS profile of the finished product, which failed at the borderline of the finished product specifications. When 2% w/w and 3% w/w film-coated tablets of LCDP were directly exposed to light, changes observed in assay and dissolution, and the RS profile, of the LCDP tablets were almost same and they were non-significant, that is, within the proposed acceptance criteria. Thus, depending on the comparative extent of change in assay, dissolution and RS of the finished product, 2% w/w film coating level was proposed for finished product formulation, which was adequately appropriate to protect the LCDP core tablets to mitigate exposure to light.
For selection of finished product packaging material by conducting a photo-stability study of the finished product, it can be concluded from the results mentioned in Table 2 that (i) When LCDP film-coated tablets were directly exposed to light, there was a significant change in Related Substances, that is, more than +0.1% profile of the finished product; (ii) when LCDP film-coated tablets were packed in the immediate pack, that is, 7's count Alu–Alu blister (cold-formed foil: made up of a 25-μm OPA film/adhesive/45-μm aluminum foil/adhesive/60-μm PVC film) as a primary pack and exposed to light, no significant change was observed in assay and dissolution, and the RS profile of the finished product; (iii) when LCDP film-coated tablets were packed in the proposed marketing pack, that is, 7's count Alu–Alu blister placed in a reverse tack folding paper box board carton of 300 gsm with UV varnish as a secondary pack and exposed to light, the changes observed in assay and dissolution, and the RS profile of the LCDP film-coated tablets were almost similar and non-significant. Thus, depending upon the comparative extent of change in assay, dissolution and RS of the finished product, 7's count Alu–Alu fompacked Alu–Alu blister (cold-formed foil: Made up of a 25-μm micron OPA film/adhesive/45-μm aluminum foil/adhesive/60-μm PVC film) placed in a folding paper box board carton of 300 gsm with UV varnish was proposed as the final packaging for LCDP tablets, which is sufficiently suitable to protect the finished product from exposure to light.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Lee CR, Bryson HM. Lacidipine. A review of its pharmacodynamic and pharmacokinetic properties and therapeutic potential in the treatment of hypertension. Drugs. 1994;48:274–96. doi: 10.2165/00003495-199448020-00010. [DOI] [PubMed] [Google Scholar]
- 2.Micheli D, Collodel A, Semeraro C, Gaviraghi G, Carpi C. Lacidipine: A calcium antagonist with potent and long-lasting antihypertensive effects in animal studies. J Cardiovasc Pharmacol. 1990;15:666–75. [PubMed] [Google Scholar]
- 3.Albini EF. Cambridge: The Royal Society of Chemistry; 1998. Photochemistry of drugs: An overview and practical problems, Drugs-Photochemistry and Photostability; pp. 1–65. [Google Scholar]
- 4.Greenhill JV. London: Taylor-Francis; 1996. Is the photodecomposition of drug predictable? The Photostability of drugs and drug formulations; pp. 83–110. [Google Scholar]
- 5.Thoma K, Klimek R. Photostabilization of drugs in dosage forms without protection from packaging materials. Int J Pharm. 1991;67:169–75. [Google Scholar]
- 6.Béchard SR, Quraishi O, Kwong E. Film coating: Effect of titanium dioxide concentration and film thickness on the photostability of nifedipine. Int J Pharm. 1992;87:133–9. [Google Scholar]
- 7.Matsuda Y, Itooka T, Mitsuhashi Y. Photostability of indomethacin in model gelatin capsules: Effects of film thickness and concentration of titanium dioxide on the coloration and photolytic degradation. Chem Pharm Bull (Tokyo) 1980;28:2665–71. doi: 10.1248/cpb.28.2665. [DOI] [PubMed] [Google Scholar]
- 8.ICH Harmonised Tripartite Guideline Q1B: Stability testing: Photostability testing of new drug substances and products, published by. International Conference on Harmonisation, Current Step 4, version. November. 1996. [Last accessed on 2012 Dec 01]. Available from: http://www.ich.org/products/guidelines/quality/quality-single/article/stability-testing-photostability-testing-of-new-drug-substances-and-products.html .
- 9.De Filippis P, Bovina E, Da Ros L, Fiori J, Cavrini V. Photodegradation studies on lacidipine in solution: Basic experiments with a cis–trans reversible photoequilibrium under UV-A radiation exposure. J Pharm Biomed Anal. 2002;27:803–12. doi: 10.1016/s0731-7085(01)00505-2. [DOI] [PubMed] [Google Scholar]
- 10.Pellegatti M, Grossi P, Ayrton J, Evans GL, Harker AJ. Absorption, distribution and excretion of lacidipine, a dihydropyridine calcium antagonist, in rat and dog. Xenobiotica. 1990;20:765–77. doi: 10.3109/00498259009046891. [DOI] [PubMed] [Google Scholar]
- 11.Gannu R, Palem CR, Yamsani VV, Yamsani SK, Yamsani MR. Enhanced bioavailability of lacidipine via microemulsion based transdermal gels: Formulation optimization, ex vivo and in vivo characterization. Int J Pharm. 2010;388:231–41. doi: 10.1016/j.ijpharm.2009.12.050. [DOI] [PubMed] [Google Scholar]
- 12.Martinez MN, Amidon GL. A mechanistic approach to understanding the factors affecting drug absorption: A review of fundamentals, pharmacokinetics and pharmacodynamics. J Clin Pharmacol. 2002;42:620–43. doi: 10.1177/00970002042006005. [DOI] [PubMed] [Google Scholar]
- 13.Technical Data for Photo-stability chamber manufactured by Thermolab scientific. [Last accessed on 2012 Oct 02]. Available from: http://www.thermolabscientific.com/photostability-chamber.php .
- 14.“Pre-formulation” in Online Knowledge Centre of Innvelop Pharmaceuticals Pvt. Ltd. [Last accessed on 2012 Dec 10]. Available from: http://www.innveloppharma.com/preformulation.html .
- 15.The Stationery Office Information and Publishing House; 2011. [Last accessed on 2012 Nov 11]. Lacidipine Tablets as a Monograph in British Pharmacopoeia. Available from: http://www.bp2012.infostar.com.cn/Bp2012.aspx?tab=browse and a=display and n=653 and id=5749 . [Google Scholar]
- 16.Tang J, Zhu R, Zhao R, Cheng G, Peng W. Ultra-performance liquid chromatography-tandem mass spectrometry for the determination of lacidipine in human plasma and its application in a pharmacokinetic study. J Pharm Biomed Anal. 2008;47:923–8. doi: 10.1016/j.jpba.2008.04.018. [DOI] [PubMed] [Google Scholar]
- 17.Matsuda Y. Some aspects on the evaluation of photostability of solid-state drugs and pharmaceutical preparations. Pharm Tech Japan. 1994;10:7–17. [Google Scholar]



