Abstract
Changes of various brain metabolites including γ-aminobutyric acid (GABA), measured by 1H-magnetic resonance spectroscopy (MRS), have been reported in panic disorder (PD). Deficits in GABA have been implicated in the pathophysiology of PD. Furthermore, it has been suggested that cortical metabolite changes in PD are familial. Eleven PD patients, including five with and six without a PD family history, and eight age- and gender-matched healthy controls without a family history of psychopathology were recruited. Each subject underwent MRS exams and behavioral assessments (resting visual analog anxiety level and the Panic Disorder Severity Scale). GABA was detected with a MEGA-PRESS J-editing sequence and fitted to minimize mac-romolecule contaminations. A significant decrease in GABA, expressed as the ratio of GABA over total creatine (GABA/tCr), was detected in the anterior cingulate cortex (ACC)/medial prefrontal cortex (mPFC) in PD patients (p<0.05), which tends to be pronounced in patients with a PD family history. No other patient/control differences in metabolites were noted in the ACC/mPFC or occipital cortex (OCC). Overall, our results indicate that deficits in GABA levels in PD patients vary by brain regions and possibly by family history status.
Keywords: Family history, GABA, MRS, Panic disorder
1. Introduction
Panic disorder (PD) is one of the most common psychiatric disorders with a lifetime prevalence of up to 5% in the US (Grant et al., 2006). Emerging evidence has implicated dysfunction in the main CNS inhibitory neurotransmitter system, the γ-aminobutyric acid (GABA) system, in the pathophysiology of PD. For example, abnormal reductions in GABAA-benzodiazepine receptor binding were consistently found in various brain regions by positron emission tomography (PET) and single-photon emission computed tomography (SPECT) (Cameron et al., 2007; Hasler et al., 2008; Kaschka et al., 1995; Malizia et al., 1998; Schlegel et al., 1994), consistent with abnormal inhibitory neuromodulation in PD.
Magnetic resonance spectroscopy (MRS) provides a unique opportunity to noninvasively detect and quantify in vivo brain metabolites such as GABA in humans. In the conventional short-echo-time (short-TE) 1H spectrum, a series of metabolites can be directly measured. These include N-Acetyl-aspartate (NAA, a neuronal marker), creatine and phosphocreatine (often referred to as total creatine, tCr, an energy buffer and shuttle), myo-inositol (mI, a glial cell marker), choline (Cho, involved in cell membrane synthesis and degradation), glutamate (Glu, the major excitatory neurotransmitter) and the sum of glutamate and glutamine (Glx). The GABA signal within these spectra is usually covered by other larger, overlapping peaks due to its small concentration (about 1 mM in vivo) and multiplet structure. Hence special GABA editing techniques are needed in order to achieve signal identification and separation of the relatively small GABA peak.
Both short-TE and GABA-edited MRS have been used to study metabolite changes in PD in the last decade with mixed results. Goddard et al. first showed decreased occipital GABA in unmedicated PD patients using a GABA editing sequence, a decrease which was later suggested to be associated with family history (Goddard et al., 2001, 2004). Ham et al. observed decreased GABA levels in the anterior cingulate cortex (ACC) and basal ganglia without using a GABA editing sequence. In addition, these authors found increased lactate and Cho in the ACC in medicated patients with PD (Ham et al., 2007). In contrast, no changes of prefrontal cortical GABA, Glx, Cho, and NAA were observed in unmedicated, non-depressed patients with PD by Hasler et al. (2009). Reduced tCr, NAA and Cho were found in the right medial temporal lobe of unmedicated PD patients (Massana et al., 2002). Yet another study reported reduced NAA/Cr and unchanged Cr and Cho/Cr in the left hippocampus in medicated PD patients (Trzesniak et al., 2010). Overall, the literature leads us to hypothesize that metabolite changes, especially GABA deficits, occur in certain brain regions in PD patients.
The ACC appears to regulate both cognitive processing and emotional processing relevant to anxiety (Bush et al., 2000). The occipital cortex and posterior cingulate cortex have been implicated in visual/spatial processing and response preparation to a physical threat (Vogt et al., 1992), functions which could be relevant to anticipatory anxiety in PD. We therefore studied GABA levels, both in the ACC and occipital cortex (OCC), using the MEGA-PRESS J-editing technique (Edden and Barker, 2007; Mescher et al., 1998).
PD is thought to be familial, with genetic factors accounting for 30–40% of the variation in causation (Finn and Smoller, 2001; Smoller et al., 2008; Weissman, 1993; Weissman and Merikangas, 1986). Normal subjects with a family history of anxiety disorder in their first-degree relatives have been found to be more vulnerable to lactate-induced panic attacks than those without a family history of anxiety disorder (Balon et al., 1989). Therefore, we also hypothesize that cortical metabolite changes, especially GABA deficits, depend on family history and may be more profound in PD patients with a family history of PD.
2. Material and methods
2.1. Subjects
Eleven PD patients (PDP, n=11, five females) and eight age- and gender-matched healthy controls (n=8, four females) without a family history of psychopathology were recruited for our study. Written in-formed consent was obtained from all subjects prior to participation in the study. For a preliminary estimate on the effect of family history, PD patients were further separated into two groups: patients with a PD family history (1st degree relatives) (Pw/F, n=5, three females) and patients without a PD family history (Pw/oF, n=6, two females). PD diagnoses were established by the Structured Clinical Interview of Mental Disorders (SCID) SCID interview (Diagnostic and Statistical Manual of Mental Disorders—fourth edition), and family history status ascertained with the Family Health Inventory (FHI) (Merikangas, 1993). Subjects were free of psychotropic medicines for 4 weeks prior to MRI/MRS scanning. Urine toxicology was negative in all subjects prior to scanning. The study protocol received official approvals from the Institutional Review Board at Indiana University School of Medicine.
Prescan behavioral assessments were performed with each subject including state anxiety level (visual analog anxiety level-rated on a 0–100 mm scale), Trails Making Test Part B (TMT-B), and Panic Disorder Severity Scale (PDSS) total scores (0–28) (Shear et al., 1997). The PDSS assesses the severity of seven dimensions of PD psychopathology and was performed in the same manner as described in a previous publication (Goddard et al., 2001). TMT-B provides a measure of cognitive function such as visual attention, visual scanning, and visual–motor coordination (Gaudino et al., 1995).
2.2. MRI/MRS and GABA editing
MRI scans were performed on a 3T Siemens Tim Trio scanner (Siemens Healthcare, Erlangen, Germany), equipped with a 32-channel head coil. In addition to anatomical imaging, short-TE 1H spectra (PRESS localization; TR/TE = 1500/30 ms; CHESS water suppression) and GABA-edited proton spectra were acquired in each subject from two volumes of interest (VOI): one in the ACC also containing portions of medial prefrontal cortex (mPFC) (20.8 ml), hence named ACC/mPFC, and a second in the OCC (18.8 ml). For each MRS scan, a reference spectrum was acquired without water suppression and used later for phase and frequency correction of the corresponding water-suppressed spectrum. Shimming and other preparation phases were performed fully automatically, resulting in line widths of <15 Hz for the unsuppressed water peak for all spectra.
The MEGA-PRESS J-editing sequence (Mescher et al., 1998), later adapted for GABA editing (Edden and Barker, 2007), was used for GABA detection (TR/TE = 1500/68 ms). This sequence makes use of the J-coupling between pairs of protons in the GABA molecule to isolate its small signal amidst much larger peaks. 196 averages were acquired with the editing pulse centered at 1.9 ppm and 196 averages with the pulse centered at 7.5 ppm in an interleaved fashion. The resulting difference spectrum contains a GABA peak at 3.0 ppm. However, a known problem with this version of the MEGA-PRESS technique is that the signal at 3.0 ppm also includes a contribution from co-edited macromolecules (“MM30”). Moreover, any GABA measurement also includes a small contribution from homocarnosine, a dipep-tide consisting of GABA and histidine with the same spin behavior as GABA, resulting in a resonance at 3.0 ppm.
MRS data processing and quantification were performed with LCModel (Provencher, 1993), fitting each spectrum as a weighted linear combination of basis spectra from individual metabolites. For the short-TE data, a basis set of in vitro spectra from individual metabolite solutions was used, and only those fitting results with relative standard deviations (%SD) <20% as reported by LCModel were used for further statistical analysis. To cancel out variations in signal due to coil loading or partial volume effects, we report metabolite concentrations as ratios with respect to the tCr concentration (a commonly used denominator for in vivo spectroscopy). For the MEGA-PRESS spectra, basis sets were generated from density matrix simulations of the sequence using published values for chemical shifts and J-couplings (Govindaraju et al., 2000), with an exact treatment of metabolite evolution during the two frequency-selective MEGA inversion pulses. Difference basis spectra were obtained by subtracting the simulated metabolite response to selective inversion at 7.5 ppm from that at 1.9 ppm. Because the subtraction was assumed to be perfect, only those metabolites with resonances close to 1.9 ppm were included in the difference basis sets: GABA, glutamate (Glu), glutamine, glutathione, and NAA. An extra Gaussian peak at 3.0 ppm was added to the LCModel calculation to explicitly fit MM30, and a soft constraint was applied to the ratio of MM30 and a resonance at 0.9 ppm from macromolecules (MM09) (Bhagwagar et al., 2007), in order to minimize the MM30 contribution to the GABA signal. We chose MM30/MM09 = 0.667 ± 0.1 for the ratio value based on preliminary LCModel fitting experiments. This fitting technique is suggested to give GABA levels close to those obtained with sequences that do not co-edit macromolecules (Long et al., 2011). As with the short-TE data, we report GABA/tCr, the ratio of GABA to total creatine. Here tCr levels were obtained from TE = 68 ms spectra with the MEGA-PRESS editing pulse centered at 7.5 ppm.
2.3. Statistics
All data are expressed as mean ± SD values. GABA levels of all patients and the healthy controls were tested for their normal distribution and compared with an independent sample t-test. Furthermore, GABA means of PDP, Pw/F, and Pw/oF were initially compared using analysis of variance (ANOVA). A Tukey's post hoc pair-wise comparison was used to further determine differences between groups if the ANOVA results indicated significance. For the statistical analysis of other metabolites, we used a false discovery rate with q-value = 0.10 to correct for multiple comparisons. The level of significance was set at p<0.05. Statistical tests were conducted using PASW Statistics 18.0 software (http://www-01.ibm.com/software/analytics/spss/).
3. Results
Patients showed no significant difference in age (t(17) = 0.227, p = 0.823) and Trails Making Test Part B (TMT-B) scores (t(17) = 0.980, p = 0.341), but significantly higher mean VAS anxiety level (t(11.44) = − 3.076, p<0.01) and mean Panic Disorder Severity Scale than controls (t(10) = − 9.746, p<0.0001). Mean values and standard deviations of these metrics for each group and subgroup are listed in Table 1.
Table 1.
Patients and healthy control subjects: baseline demographic and clinical information.
| Age (mean yr ± SD) | Mean ± SD VAS anxiety level (0–100 mm) | Mean ± SD Panic Disorder Severity Scale (PDSS) | Mean ± SD Trails Making Test Part B (TMT-B) test score | |
|---|---|---|---|---|
| Patients (PDP, n = 11) | 38.2 ± 12.7 | 45.8 ± 28.8** | 9.8 ± 3.3** | 10.3 ± 2.6 |
| Patients with PD family history (Pw/F, n = 5) | 32.6 ± 5.9 | 38.2 ± 36.8* | 10.6 ± 4.7** | 10.8 ± 3.8 |
| Patients without PD family history (Pw/oF, n = 6) | 42.8 ± 15.5 | 52.2 ± 21.6** | 9.2 ± 1.8** | 9.3 ± 1.0 |
| Controls (n = 8) | 39.5 ± 12.1 | 4.1 ± 8.0 | 0 | 12.3 ± 3.7 |
p<0.05 compared to controls.
p<0.01 compared to controls.
3.1. Short-TE spectra
Fig. 1 depicts the VOIs for the two brain regions – ACC/mPFC and OCC (yellow and green rectangles, respectively) – as well as representative short-TE and GABA spectra for each region. Table 1 shows the demographic and clinical information of all subjects.
Fig. 1.
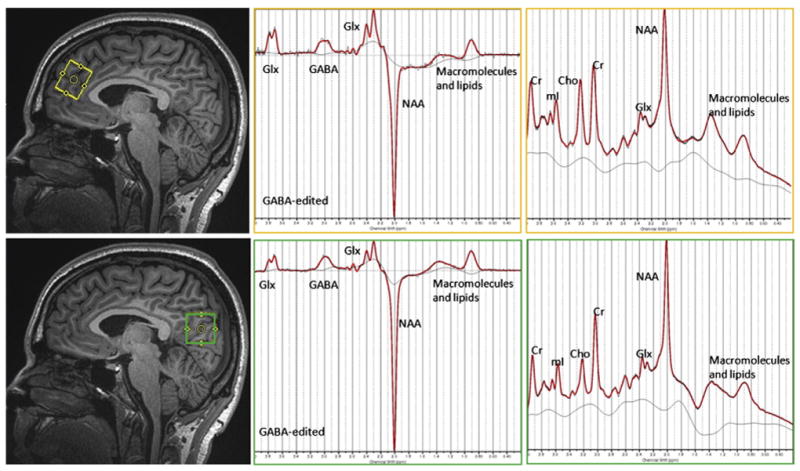
Volumes of interest (VOIs) for two brain regions and representative spectra (black) with LCModel fitting for each region: anterior cingulate cortex/medial prefrontal cortex (upper) and occipital cortex (lower) with a corresponding short-TE spectrum and a MEGA-PRESS difference spectrum (black line: raw unfiltered spectra; red line: LCModel fit; grey line: LCModel baseline).
Neither PDP nor Pw/F or Pw/oF groups showed different tCr levels relative to unsuppressed water signal in the ACC/mPFC or OCC compared to the control group. Therefore, it is reasonable to use tCr as internal reference for other metabolites. The PDP group showed no significant change in any metabolites obtained by short-TE spectra from the ACC/mPFC and OCC. In the OCC, Pw/F patients had significantly higher Glu/tCr values (mean ± SD = 0.989 ± 0.030) than Pw/oF (mean ± SD = 0.856 ± 0.090) (F(2, 16) = 4.036, p<0.05), which however did not pass the false discovery rate threshold at q-value = 0.10.
3.2. GABA-edited spectra
A significant decrease in GABA/tCr was found in the ACC/mPFC but not the OCC in PDP (mean ± SD = 0.145 ± 0.079) compared to control subjects (mean ± SD = 0.245 ± 0.105) (t(17) = 2.374, p = 0.030, Fig. 2). No correlations between GABA/tCr and resting anxiety or PDSS were found in the PDP group. The Pw/F patient subgroup tended to show lower GABA/tCr in the ACC/mPFC (mean ± SD = 0.119 ± 0.081) than controls (F(2, 16) = 3.133, p = 0.069), whereas Pw/oF (mean ± SD = 0.166 ± 0.077) showed no changes (p = 0.277). In the OCC, no changes were found among Pw/F, Pw/oF and control groups. GABA/tCr values of each subject are shown in Fig. 3.
Fig. 2.
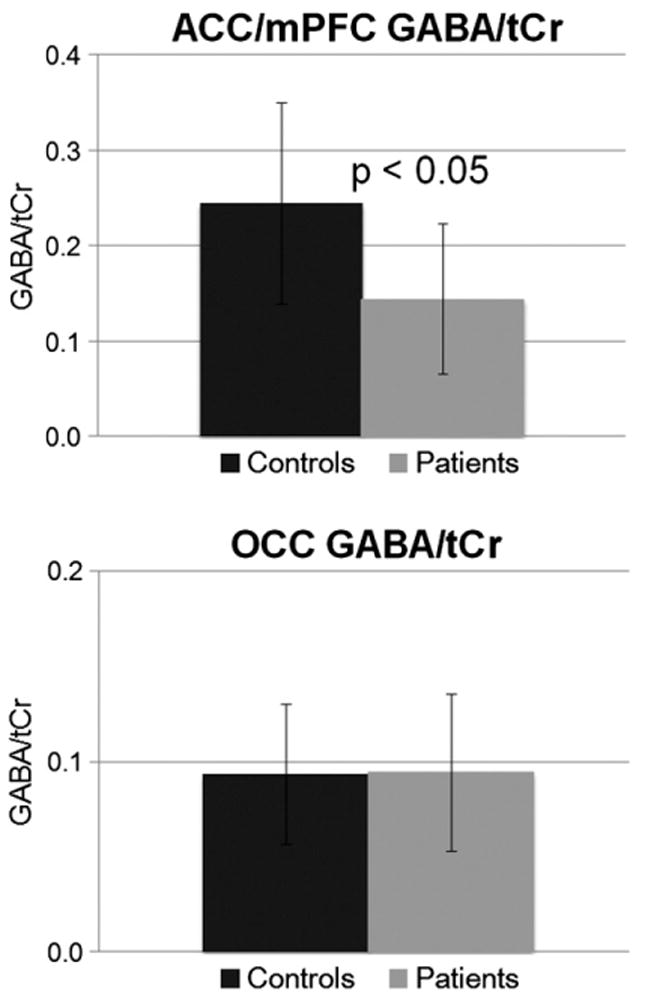
Mean and standard deviation for GABA, expressed as the ratio over total creatine, GABA/tCr, in the anterior cingulate cortex (ACC)/medial prefrontal cortex (mPFC) and occipital cortex (OCC) of panic patients and healthy controls.
Fig. 3.
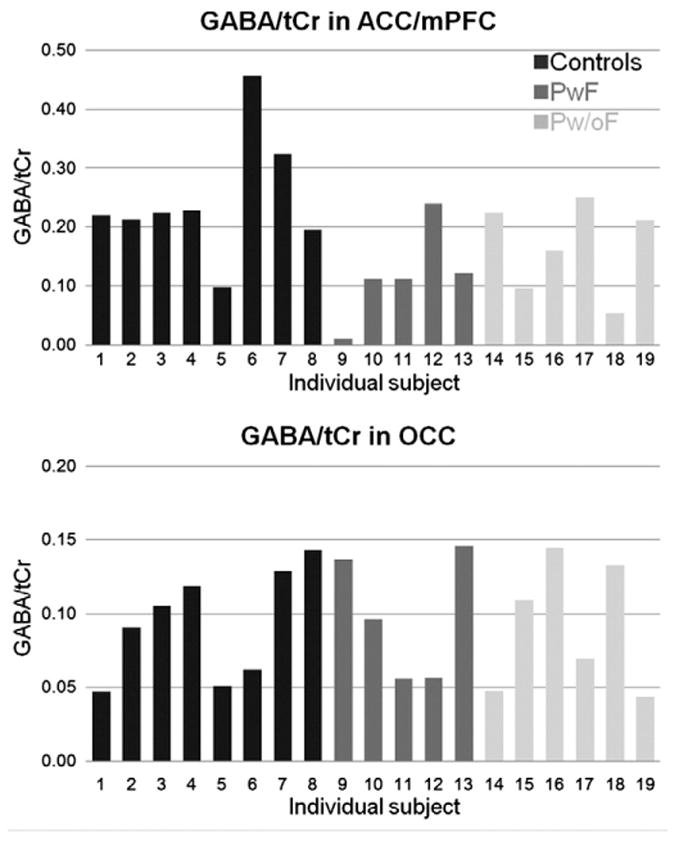
Histogram of GABA, expressed as the ratio over total creatine GABA/tCr, in the anterior cingulate cortex (ACC)/medial prefrontal cortex (mPFC) and occipital cortex (OCC) of panic patients and healthy controls.
4. Discussion
Using a GABA-edited MRS technique and a fitting method to minimize macromolecule contamination, we found that GABA deficits were present in the ACC/mPFC of PD patients, a result that supports the hypothesis that GABA neuronal dysfunction is intrinsic to PD. No other metabolite differences between patients and controls were observed in either the ACC/mPFC or the OCC. Patients and controls with a personal or family history of major depressive disorder were carefully excluded by the study design. In addition, medication effects were controlled for, and should not have significantly influenced data interpretation. Low cortical GABA may be due to dysfunctional GABA synthesis enzymes or due to dysfunction in enzymes involved in glutamate–glutamine cycling, which accounts for 10–15% of the neuronal pool of GABA (Kugler, 1993).
In healthy controls, we observed that GABA/tCr levels were higher in the ACC/mPFC than in the OCC, similar to Ongur et al. (2010). This difference could be a function of our voxel placement, which contained some medial frontal cortex as indicated in Fig. 1. GABA levels in the frontal cortex have been reported to be about two times higher than that in the OCC (Goto et al., 2010; Kakeda et al., 2011). The current study did not observe OCC GABA deficits in PD patients as reported previously (Goddard et al., 2001), which might be due to the different placement of the VOIs within the occipital cortex in the two studies. In addition, the mean PDSS of the subjects in Goddard et al. was 13, indicating a higher level of panic symptoms than the patients participating in this study (mean PDSS = 9.8 ± 3.3).
Our preliminary results from the small patient subgroups support the idea that brain metabolite changes in PD may be influenced by familial factors, as suggested by Goddard et al. (2004). The GABA deficit we observed was more pronounced in the Pw/F patient subgroup. However, since our sample size is small, a follow-up study needs to be conducted with larger subgroups of subjects to confirm these results. Furthermore, brain tissue segmentation was not performed in the present study, limiting our ability to achieve absolute quantitation of gray matter GABA and other metabolites. A potential confound of group differences in gray/white matter proportion may have affected our GABA results since GABA concentration varies in gray and white matter.
The technique of GABA editing at 3T limits the sensitivity to measure GABA in other fear circuit structures importantly implicated in panic anxiety such as medial temporal lobe, amygdala, and hypothalamus due to their small volumes. It lacks the capacity to measure intrasynaptic GABA concentrations, which may be more physiologically relevant. Confirmation of the finding of low cortical GABA in PD patients, which is especially strong in patients with a panic family history, is needed by appropriately-powered, follow-up studies.
5. Conclusion
Our results suggest that a GABA deficit exists in the ACC/mPFC of panic patients. This deficit may be more pronounced in those patients with a positive panic family history. The role of GABA in the patho-physiology of PD may also vary by brain region and needs to be studied taking into account family history status.
Acknowledgments
The authors gratefully acknowledge Michele Beal and Courtney Robbins for their professional and dedicated work in MRS data acquisition (Center for Neuroimaging, Department of Radiology and Imaging Sciences, Indiana University School of Medicine). We want to thank Dr. Anantha Shekhar and the staff of the Indiana CTSI center for their support of this project. We further thank Dr. James B. Murdoch for helpful discussions about GABA fitting methods.
This work was supported by a Collaborative Research Grant by the Indiana Clinical and Translational Sciences Institute, funded in part by grant # RR 02576 from the National Institutes of Health, National Center for Research Resources.
Abbreviations
- GABA
γ-aminobutyric acid
- MM30
macromolecule resonance at 3.0 ppm
- MRS
magnetic resonance spectroscopy
- MM09
macromolecule resonance at 0.9 ppm
- PD
panic disorder
- ACC
anterior cingulate cortex
- OCC
occipital cortex
- mPFC
medial prefrontal cortex
- Glu
glutamate
- tCr
total creatine
References
- Balon R, Jordan M, Pohl R, Yeragani VK. Family history of anxiety disorders in control subjects with lactate-induced panic attacks. Am J Psychiatry. 1989;146:1304–6. doi: 10.1176/ajp.146.10.1304. [DOI] [PubMed] [Google Scholar]
- Bhagwagar Z, Wylezinska M, Jezzard P, Evans J, Ashworth F, Sule A, et al. Reduction in occipital cortex gamma-aminobutyric acid concentrations in medication-free recovered unipolar depressed and bipolar subjects. Biol Psychiatry. 2007;61:806–12. doi: 10.1016/j.biopsych.2006.08.048. [DOI] [PubMed] [Google Scholar]
- Bush G, Luu P, Posner MI. Cognitive and emotional influences in anterior cingulate cortex. Trends Cogn Sci. 2000;4(6):215–22. doi: 10.1016/s1364-6613(00)01483-2. [DOI] [PubMed] [Google Scholar]
- Cameron OG, Huang GC, Nichols T, Koeppe RA, Minoshima S, Rose D, et al. Reduced gamma-aminobutyric acid (A)-benzodiazepine binding sites in insular cortex of individuals with panic disorder. Arch Gen Psychiatry. 2007;64:793–800. doi: 10.1001/archpsyc.64.7.793. [DOI] [PubMed] [Google Scholar]
- Edden RA, Barker PB. Spatial effects in the detection of gamma-aminobutyric acid: improved sensitivity at high fields using inner volume saturation. Magn Reson Med. 2007;58:1276–82. doi: 10.1002/mrm.21383. [DOI] [PubMed] [Google Scholar]
- Finn CT, Smoller JW. The genetics of panic disorder. Curr Psychiatry Rep. 2001;3:131–7. doi: 10.1007/s11920-001-0010-5. [DOI] [PubMed] [Google Scholar]
- Gaudino EA, Geisler MW, Squires NK. Construct validity in the Trail Making Test: what makes Part B harder? J Clin Exp Neuropsychol. 1995;17:529–35. doi: 10.1080/01688639508405143. [DOI] [PubMed] [Google Scholar]
- Goddard AW, Mason GF, Almai A, Rothman DL, Behar KL, Petroff OA, et al. Reductions in occipital cortex GABA levels in panic disorder detected with 1h-magnetic resonance spectroscopy. Arch Gen Psychiatry. 2001;58:556–61. doi: 10.1001/archpsyc.58.6.556. [DOI] [PubMed] [Google Scholar]
- Goddard AW, Mason GF, Rothman DL, Behar KL, Petroff OA, Krystal JH. Family psychopathology and magnitude of reductions in occipital cortex GABA levels in panic disorder. Neuropsychopharmacology. 2004;29:639–40. doi: 10.1038/sj.npp.1300374. [DOI] [PubMed] [Google Scholar]
- Goto N, Yoshimura R, Kakeda S, Moriya J, Hori H, Hayashi K, et al. No alterations of brain GABA after 6 months of treatment with atypical antipsychotic drugs in early-stage first-episode schizophrenia. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34(8):1480–3. doi: 10.1016/j.pnpbp.2010.08.007. [DOI] [PubMed] [Google Scholar]
- Govindaraju V, Young K, Maudsley AA. Proton NMR chemical shifts and coupling constants for brain metabolites. NMR Biomed. 2000;13:129–53. doi: 10.1002/1099-1492(200005)13:3<129::aid-nbm619>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, Goldstein RB, Smith S, et al. The epidemiology of DSM-IV panic disorder and agoraphobia in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2006;67:363–74. doi: 10.4088/jcp.v67n0305. [DOI] [PubMed] [Google Scholar]
- Ham BJ, Sung Y, Kim N, Kim SJ, Kim JE, Kim DJ, et al. Decreased GABA levels in anterior cingulate and basal ganglia in medicated subjects with panic disorder: a proton magnetic resonance spectroscopy (1H-MRS) study. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:403–11. doi: 10.1016/j.pnpbp.2006.10.011. [DOI] [PubMed] [Google Scholar]
- Hasler G, Nugent AC, Carlson PJ, Carson RE, Geraci M, Drevets WC. Altered cerebral gamma-aminobutyric acid type A-benzodiazepine receptor binding in panic disorder determined by [11C]flumazenil positron emission tomography. Arch Gen Psychiatry. 2008;65:1166–75. doi: 10.1001/archpsyc.65.10.1166. [DOI] [PubMed] [Google Scholar]
- Hasler G, van der Veen JW, Geraci M, Shen J, Pine D, Drevets WC. Prefrontal cortical gamma-aminobutyric acid levels in panic disorder determined by proton magnetic resonance spectroscopy. Biol Psychiatry. 2009;65:273–5. doi: 10.1016/j.biopsych.2008.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakeda S, Korogi Y, Moriya J, Ohnari N, Sato T, Ueno S, et al. Influence of work shift on glutamic acid and gamma-aminobutyric acid (GABA): evaluation with proton magnetic resonance spectroscopy at 3T. Psychiatry Res. 2011;192:55–9. doi: 10.1016/j.pscychresns.2010.10.011. [DOI] [PubMed] [Google Scholar]
- Kaschka W, Feistel H, Ebert D. Reduced benzodiazepine receptor binding in panic disorders measured by iomazenil SPECT. J Psychiatr Res. 1995;29:427–34. doi: 10.1016/0022-3956(95)00019-2. [DOI] [PubMed] [Google Scholar]
- Kugler P. Enzymes involved in glutamatergic and GABAergic neurotransmission. Int Rev Cytol. 1993;147:285–336. doi: 10.1016/s0074-7696(08)60771-8. [DOI] [PubMed] [Google Scholar]
- Long Z, Murdoch James, Xu J, Dydak U. Proc Intl Soc Magn Reson Med. 2011;19:1399. [Google Scholar]
- Malizia AL, Cunningham VJ, Bell CJ, Liddle PF, Jones T, Nutt DJ. Decreased brain GABA(A)-benzodiazepine receptor binding in panic disorder: preliminary results from a quantitative PET study. Arch Gen Psychiatry. 1998;55:715–20. doi: 10.1001/archpsyc.55.8.715. [DOI] [PubMed] [Google Scholar]
- Massana G, Gasto C, Junque C, Mercader JM, Gomez B, Massana J, et al. Reduced levels of creatine in the right medial temporal lobe region of panic disorder patients detected with (1)H magnetic resonance spectroscopy. Neuroimage. 2002;16:836–42. doi: 10.1006/nimg.2002.1083. [DOI] [PubMed] [Google Scholar]
- Merikangas KR. Genetic epidemiologic studies of affective disorders in childhood and adolescence. Eur Arch Psychiatry Clin Neurosci. 1993;243:121–30. doi: 10.1007/BF02190718. [DOI] [PubMed] [Google Scholar]
- Mescher M, Merkle H, Kirsch J, Garwood M, Gruetter R. Simultaneous in vivo spectral editing and water suppression. NMR Biomed. 1998;11:266–72. doi: 10.1002/(sici)1099-1492(199810)11:6<266::aid-nbm530>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- Ongur D, Prescot AP, McCarth J, Cohen BM, Renshaw PF. Elevated gamma-aminobutyric acid levels in chronic schizophrenia. Biol Psychiatry. 2010;68(7):667–70. doi: 10.1016/j.biopsych.2010.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Provencher SW. Estimation of metabolite concentrations from localized in vivo proton NMR spectra. Magn Reson Med. 1993;30:672–9. doi: 10.1002/mrm.1910300604. [DOI] [PubMed] [Google Scholar]
- Schlegel S, Steinert H, Bockisch A, Hahn K, Schloesser R, Benkert O. Decreased benzodiazepine receptor binding in panic disorder measured by IOMAZENIL-SPECT. A preliminary report. Eur Arch Psychiatry Clin Neurosci. 1994;244:49–51. doi: 10.1007/BF02279812. [DOI] [PubMed] [Google Scholar]
- Shear MK, Brown TA, Barlow DH, Money R, Sholomskas DE, Woods SW, et al. Multicenter collaborative Panic Disorder Severity Scale. Am J Psychiatry. 1997;154:1571–5. doi: 10.1176/ajp.154.11.1571. [DOI] [PubMed] [Google Scholar]
- Smoller JW, Gardner-Schuster E, Covino J. The genetic basis of panic and phobic anxiety disorders. Am J Med Genet C Semin Med Genet. 2008;148C:118–26. doi: 10.1002/ajmg.c.30174. [DOI] [PubMed] [Google Scholar]
- Trzesniak C, Uchida RR, Araujo D, Guimaraes FS, Freitas-Ferrari MC, Filho AS, et al. (1)H magnetic resonance spectroscopy imaging of the hippocampus in patients with panic disorder. Psychiatry Res. 2010;182:261–5. doi: 10.1016/j.pscychresns.2010.03.008. [DOI] [PubMed] [Google Scholar]
- Vogt BA, Finch DM, Olson CR. Functional heterogeneity in cingulate cortex: the anterior executive and posterior evaluative regions. Cereb Cortex. 1992;2(6):435–43. doi: 10.1093/cercor/2.6.435-a. [DOI] [PubMed] [Google Scholar]
- Weissman MM. Family genetic studies of panic disorder. J Psychiatr Res. 1993;27(Suppl. 1):69–78. doi: 10.1016/0022-3956(93)90018-w. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Merikangas KR. The epidemiology of anxiety and panic disorders: an update. J Clin Psychiatry. 1986;47:11–7. [Suppl.]. [PubMed] [Google Scholar]


