Abstract
Recent findings have demonstrated an indispensable role for granulocyte-emacrophage colony-stimulating factor (GM-CSF) in the pathogenesis of experimental autoimmune encephalomyelitis (EAE). However the signaling pathways and cell populations that regulate GM-CSF production in vivo remain to be elucidated. Our work demonstrates that the interleukin-1 receptor type 1 (IL-1R) is required for GM-CSF production following both TCR and cytokine induced stimulation of immune cells in vitro. Conventional αβ and γδ T cells were both identified to be potent producers of GM-CSF. Moreover secretion of GM-CSF was dependent on IL-1R under both IL-12 and IL-23 induced stimulatory conditions. Deficiency in IL-1R conferred significant protection from EAE and this correlated with reduced production of GM-CSF and attenuated infiltration of inflammatory cells into the central nervous system (CNS). We also find that GM-CSF production in vivo is not restricted to a defined CD4+ T cell lineage, but is rather heterogeneously expressed in the effector CD4+ T cell population. In addition, inflammasome derived IL-1β upstream of IL-1R is a critical regulator of GM-CSF production by T cells during priming and the adaptor protein, MYD88, promotes GM-CSF production in both αβ and γδ T cells. These findings highlight the importance of inflammasome-derived IL-1β and the IL-1R/MYD88 signaling axis in the regulation of GM-CSF production.
Keywords: NLR, Inflammasome, Caspase-1, IL-1R, IL-1β, EAE
INTRODUCTION
Multiple sclerosis (MS) is a debilitating neuroinflammatory disease that occurs when myelin-reactive CD4+ T cells gain entry into the central nervous system (CNS) and cause destruction of myelin-producing oligodendrocytes. T helper type 1 cells (TH1 cells) and interleukin 17 (IL-17) producing helper T cells (TH17) have been shown to be important mediators of autoimmune neuroinflammation in both MS patients and in EAE. Both TH1 cells and TH17 cells can induce demyelinating disease and inflammation following passive transfer into naïve hosts. Paradoxically the signature cytokines produced by each T cell lineage, IFN-γ and IL-17 respectively, are not essential for disease (1) (2). Recently, GMCSF was discovered to be the key pathogenic cytokine required for both TH1- and TH17-mediated demyelinating disease (3) (4) (5). T cell derived GM-CSF was shown to prolong CNS inflammation during the effector phase by promoting local activation of macrophages and the recruitment of myeloid cells (6) (3). Despite this major advance in the field of demyelinating disease, the signaling pathways and cells types that control GM-CSF production during disease progression still remain unknown.
IL-1 signaling is critically involved in numerous inflammatory and autoimmune diseases (7). The importance of IL-1 in disease pathogenesis is highlighted by the effectiveness of IL-1 blocking therapies in the treatment of many of these diseases. The inflammasome has recently emerged as a central regulator of IL-1β production and IL-1-mediated diseases (8) (9) (10). The inflammasome is a multiprotein complex that controls caspase-1 activation and downstream secretion of IL-1β and IL-18. Activation of intracellular NOD-like receptors (NLRs) by pathogens and endogenous danger signals promote the formation of the inflammasome complex, which is required for caspase-1 cleavage and activation. Inflammasome-derived cytokines play a crucial role in host protection to numerous infections however unchecked production of both IL-1β and IL-18 is associated with chronic inflammation and many autoimmune diseases. Studies from our lab and others have identified caspase-1 and IL-1R as important contributors to the induction and progression of demyelinating autoimmune disease (11) (12) (13) (14). For instance, IL-1R deficient mice are protected from neuroinflammatory disease (15) (16) (17). The abrogation of IL-17 production in IL-1R−/− mice was proposed to contribute to disease resistance. However the fact that EAE can still be induced in the absence of IL-17 and the recent identification of the essential role for GM-CSF in disease suggests that IL-1R-mediated control of demyelination may involve more than just regulation of IL-17 production.
We report here that IL-1R regulates the generation of GM-CSF by both CD4+ T cells andγδ T cells during EAE. Moreover we indentify that inflammasome derived IL-1β promotes the priming of GM-CSF producing CD4+ T cells upstream of IL-1R during EAE and that IL-1R induced GM-CSF production requires MYD88 signaling in bothα β andγ δ T cells.
MATERIALS AND METHODS
Mice
Caspase-1−/− and IL-1β−/− have been described (10) (11). IL-1R deficient mice on the C57BL/6 background were purchased from The Jackson Laboratory. Mice at 7–12 wk of age were used. All mice were kept in specific pathogen-free conditions within the Animal Resource Center at St. Jude Children’s Research Hospital. Animal protocols were approved by the Institutional Animal Care and Use Committee of St. Jude Children’s Research Hospital.
Cell purification and culture
Splenocytes and peripheral LNs were harvested from WT, IL-1R−/−, and MYD88−/− mice. Bulk leukocytes (2×106 cells/ml) were stimulated in the presence or absence of 1µ g/ml anti-mouse CD3 (2C11) and 10 ng/ml IL-1β, 10 ng/ml IL-23, 10 ng/ml IL-12, or a combination of these stimuli.γδ T cells (δ γ TCR+) and memory CD4+ T cells (CD4+CD44hi) were purified (purity > 98%) on a MoFlow (Beckman Coulter) or Reflection (i-Cyt) flow sorter. Sorted cells were cultured at either 2.5×105 cells/ml (memory CD4+ T cells) or 1×105 cells/ml (γ δ T cells) and stimulated with 10 ng/ml IL-1β, 10 ng/ml IL-23, 10 ng/ml IL-12, or a combination of these stimuli. To stimulate T cells in the presence of DCs, naïve CD4+ T cells (CD4+CD44loCD25−) were FACs sorted and then cultured at a ratio of 10:1 (T cells: BMDCs). T cells were stimulated with 1 µg/ml anti-mouse CD3 (2C11) and 10 ng/ml IL-1β or 10 ng/ml IL-1β plus 10 ng/ml IL-23.
EAE Model
Age (7–12 weeks of age) and sex matched mice were immunized subcutaneously with 100 µg MOG35–55 peptide (MEVGWYRSPFSRVVHLYRNGK) emulsified in CFA (Difco Laboratories) with 500 µg Mycobacterium tuberculosis on day 0. Mice also received 200 ng of pertussis toxin (List Biological Laboratories, Inc.) by intraperitoneal injection on days 0 and 2. Disease severity was assessed daily by assigning clinical scores according to the following scale: 0, no disease; 1, tail paralysis; 2, weakness of hind limbs; 3, paralysis of hind limbs; 4, paralysis of hind limbs and severe hunched posture; 5, moribund or death. To harvest CNS leukocytes, mice were perfused through the left ventricle with PBS. The spinal cord was isolated, cut into small pieces, and then passed through a 70 µm cell strainer. Leukocytes were then purified by gradient centrifugation using a 38% Percoll solution. The cells were washed once in PBS and then resuspended in media.
Bioplex assay
Splenocytes obtained from mice with EAE were cultured at 2×106 cells/ml and stimulated with 30 µg/ml MOG peptide or media alone. Supernatants were harvested after 48 hrs from these experiments. In all other assays, supernatants from cells that were stimulated with anti-CD3 or cytokine stimuli were harvested after 72 hrs. Cytokine levels in the supernatants were measured using MILLIPLEX kits for mouse cytokine/chemokine according to the manufacturer’s instruction (Millipore).
Intracellular cytokine staining
Splenocytes or LN cells were harvested from mice with EAE and restimulated with phorbol 12-myristate 13-acetate (PMA) and ionomycin or 30 µg/ml MOG peptide in the presence of monensin for 4–5 hrs. Cells were stained according to the manufacturer’s instructions (ebioscience). Flow cytometry data were acquired on an upgraded five-color FACScan or multi-color LSRII (BD) and were analyzed with FlowJo software (Tree Star)
Statistics
P-values were calculated with Student’s t test. P-values <0.05 were considered significant.
RESULTS
IL-1R is required for the induction of GM-CSF production following in vitro stimulation
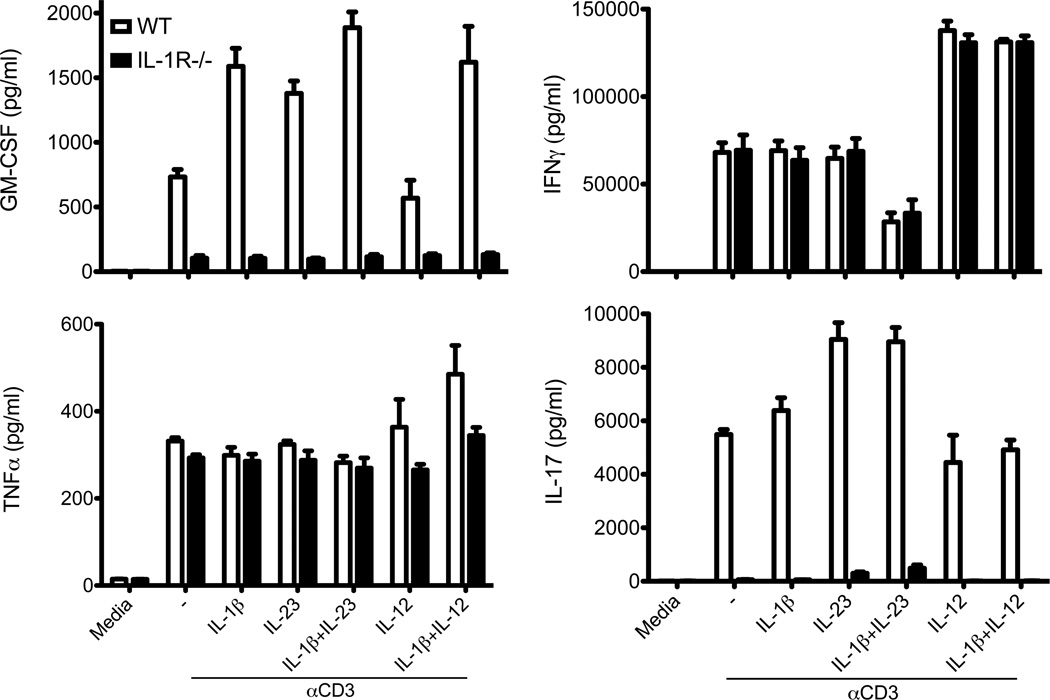
To study the contribution of IL-1 signaling to the induction of GM-CSF production, WT and IL-1R−/− splenocytes and lymph node cells were stimulated in vitro with anti-CD3 in combination with various cytokines previously reported to promote the induction of disease during EAE. Treatment with anti-CD3 alone induced GMCSF secretion, however treatment with exogenous IL-23, IL-1β, or IL-1β in combination with either IL-12 or IL-23 further enhanced GM-CSF production (Fig. 1). Interestingly, IL-1R−/− immune cells failed to secrete GM-CSF under any of the stimulatory conditions tested, suggesting that IL-1R centrally controls GM-CSF production. Consistent with published reports (11) (15) (16), absence of IL-1 signaling also completely abrogated IL-17 production. The defect in GM-CSF production was not the result of a global impairment in immune cell activation as production of TNF-α, IFN-γ, and IL-1β (Supplemental Fig. 1) was not affected by IL-1R deficiency.
Figure 1. IL-1 signaling regulates anti-CD3 induced GM-CSF production.
Splenocytes and lymph node cells were harvested from wild-type (WT) or IL-1R−/− mice. Cells were stimulated with anti-CD3 in the presence of IL-1β, IL-23, IL-1β and IL-23, IL-12, or IL-12 and IL-1β. Supernatants were collected at 72 hrs for analysis of GM-CSF, IFN-γ, TNF-α, and IL-17 production by ELISA. Data are representative of four independent experiments with 2–3 mice per group. Data represent mean ± SEM.
GM-CSF production by γ δ T cells requires IL-1R
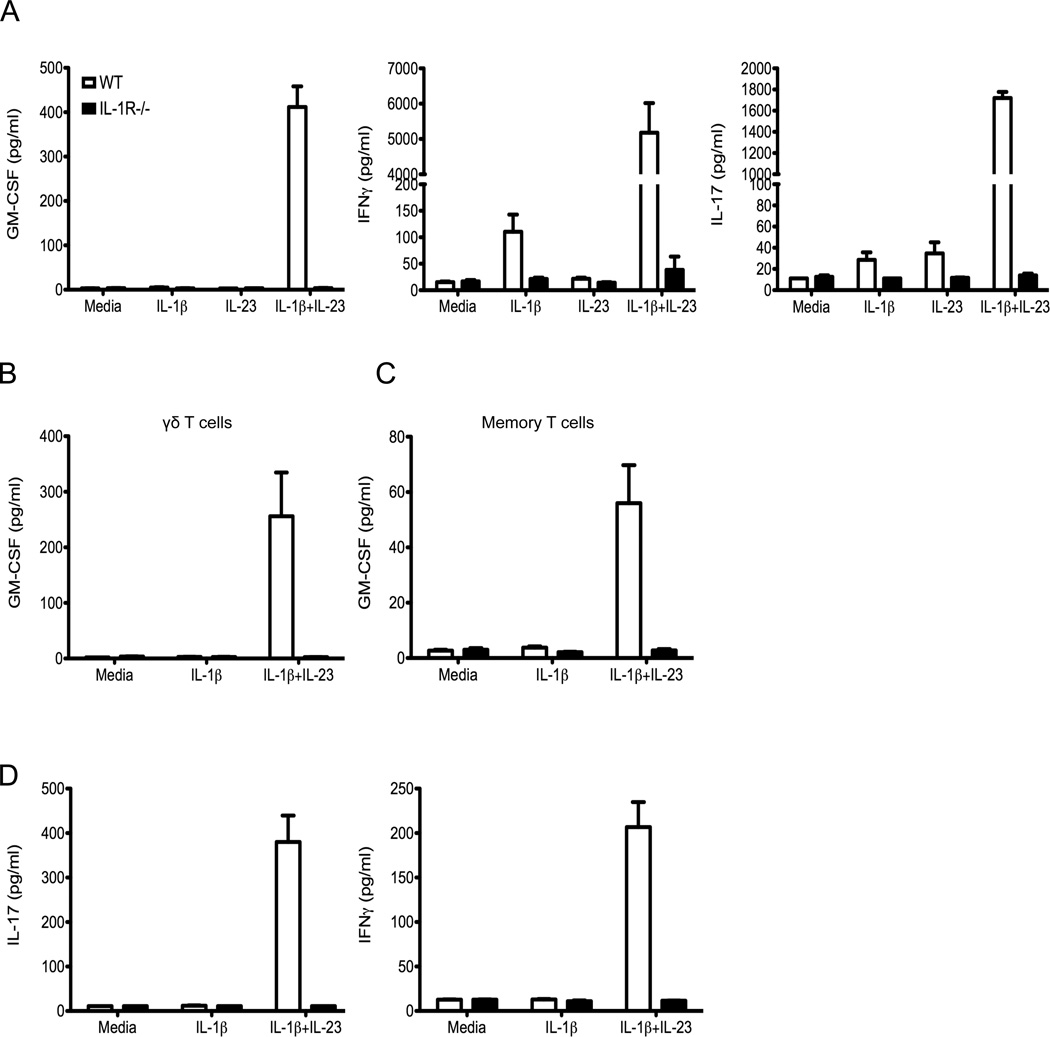
In addition to autoreactive T cells, additional immune cells can also substantially contribute to the inflammatory cytokine environment and tissue destruction in many diseases. For instance, IL-17 producing δ γ T cells have been shown to exacerbate disease progression in numerous autoimmune models (18). Furthermore, antigen-nonspecific memory T cells can also be recruited into inflamed tissues and release inflammatory mediators. Thus we were interested in studying whether immune cells can be stimulated to produce GM-CSF in the absence of TCR stimulation and also determining the potential role of IL-1 signaling in this process. Neither IL-1β nor IL-23 stimulation alone was able to induce GM-CSF production from bulk immune cells (Fig. 2A). Rather treatment with both IL-1β and IL-23 was needed to induce GM-CSF production by WT cells in the absence of anti-CD3 treatment. In contrast, IL-1R−/− cells failed to secrete GM-CSF following cytokine stimulation. This indicates that IL-1R is essential to promote GM-CSF production following stimulation with both IL-1β and IL-23. As an experimental control we also assessed the capacity of IL-1R to influence the production of IFN-γ and IL-17 following cytokine stimulation. In agreement with published reports (15), we found that IL-1β and IL-23 synergize to induce robust production of both IL-17 and IFN-γ in an IL-1R dependent fashion (Fig. 2A).
Figure 2. γδ T cells produce GM-CSF in a IL-1R dependent fashion.
Splenocytes and lymph node cells were harvested from WT or IL-1R−/− mice. Bulk leukocytes were stimulated with IL-1β, IL-23, or IL-1β and IL-23. (A) Supernatants were collected at 72 hrs for analysis of GM-CSF, IFN-γ, and IL-17 production by ELISA. (B) Sorted γδ T cells from WT or IL-1R−/− mice were stimulated with IL-1β or IL-1β and IL-23. Supernatants were collected after 72 hrs and GM-CSF was measured by ELISA. (C) Sorted memory CD4+ T cells (CD44+CD4+) were stimulated with IL-1β or IL-1β and IL-23. Supernatants were collected after 72 hrs and GM-CSF, (D) IL-17, and IFN-γ were measured by ELISA. Data are representative of three independent experiments with 2–3 mice per group. Data represent mean ± SEM.
To identify the cellular source of GM-CSF following TCR-independent stimulation, we FACS sorted γ δ T cells and memory CD4+ T cells and measured GM-CSF production following cytokine treatment. Dual IL-1β and IL-23 stimulation potently induced GM-CSF from δ γ T cells (Fig. 2B). Memory CD4+ T cells, in contrast, only produced modest amounts of GM-CSF following the same stimulation conditions (Fig. 2C). Memory CD4+ T cells can secrete substantial levels of IL-17 and IFN-γ in response to IL-1β and IL-23 (Fig. 2D), suggesting that TCR-independent secretion of GM-CSF by memory T cells may be more tightly regulated than IL-17 or IFN-γ. In agreement with our earlier findings, IL-1R is essential for IL-1β plus IL-23-induced GM-CSF production by both purified γ δ T cells and memory CD4+ T cells.
IL-1R deficiency attenuates GM-CSF production in vivo
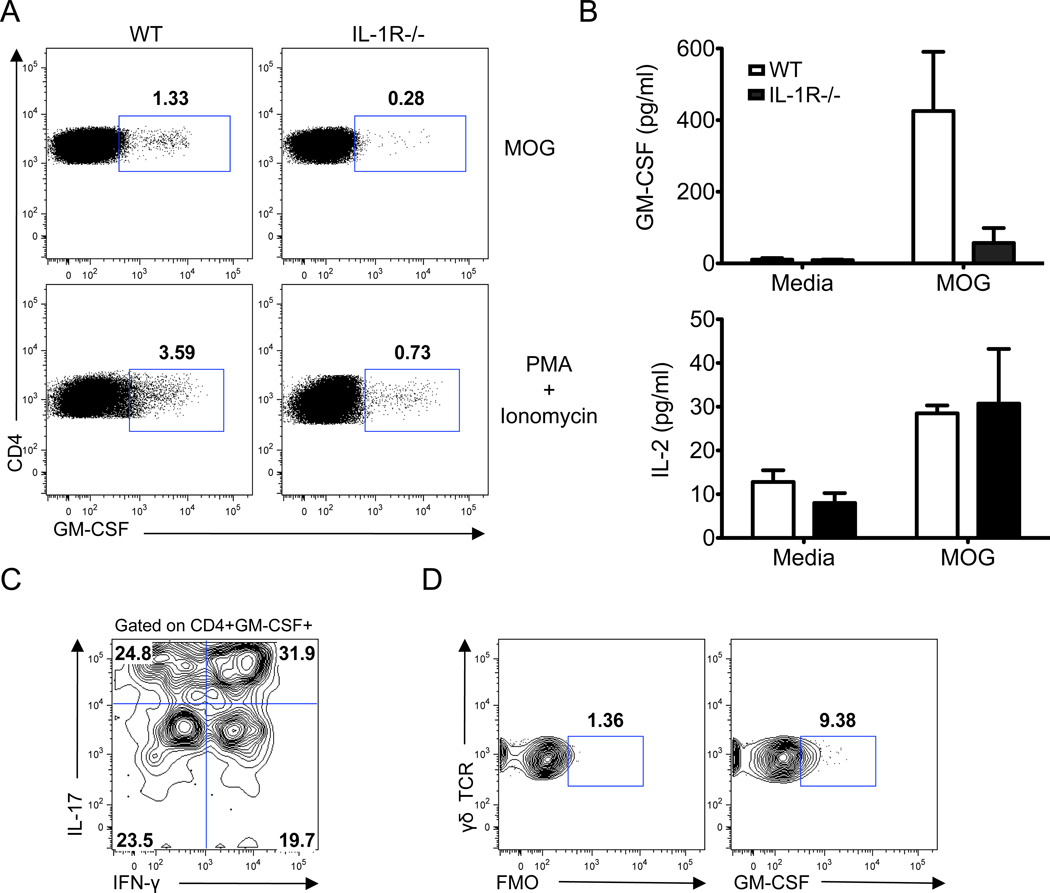
We next examined the possibility that IL-1 exacerbates neuroinflammation during EAE by promoting the generation of GM-CSF producing immune cells. To test this, EAE was induced in WT and IL-1R−/− mice and the production of GM-CSF by T cells was evaluated at day 10 in the dLNs. T cell-mediated GM-CSF production was significantly attenuated in the dLNs of IL-1R−/− mice following restimulation with either MOG peptide or PMA/ionomycin (Fig. 3A). It is possible that the impairment in MOG-specific GM-CSF production by IL-1R−/− T cells is the result of a global defect in T cell expansion and activation. Conversely it is also possible that the absence of IL-1R directly affects the acquisition of specific cytokine production by T cells. To test this, supernatants were collected from day 10 dLN cells that were restimulated with MOG peptide for 48 hours and the production of cytokines was measured. Consistent with our flow data, we observed a significant reduction in GM-CSF production in the absence of IL-1R (Fig. 3B). However, IL-1R was not found to alter the secretion of other T cell derived cytokines including IL-2, TNF-α, and IL-10 (Fig. 3B and data not shown). This data demonstrates that the impairment in GM-CSF production that occurs in IL-1R−/− mice is the direct result of altered acquisition of effector cytokine production and not the result of decreased T cell expansion.
Figure 3. IL-1R controls in vivo GM-CSF production during EAE.
WT and IL-1R−/− mice were immunized with MOG/CFA. (A) On day 10, dLN cells were stimulated with either MOG peptide (top panel) or PMA/ionomycin (bottom panel) for 5 hrs followed by intracellular staining for GM-CSF. Data are representative of four independent experiments. (B) Splenocytes were stimulated for 48 hrs with MOG peptide and cytokines were measured by ELISA. Data are representative of four independent experiments with at least 4 mice per group. (C) Intracellular staining for IL-17 and IFN-γ in CD4+GM-CSF+ T cells obtained from the dLNs of WT mice and restimulated with MOG peptide for 5hrs. Data are representative of 8 independent experiments. (D) Intracellular staining of GM-CSF in γδ T cells obtained from the dLNs of WT mice and stimulated with PMA/ionomycin for 5 hrs. Data are representative of 6 independent experiments. FMO, fluorescence-minus-one control.
Our in vitro data (Fig. 1) and recent in vitro work by other groups have shown that GM-CSF production can be induced following both TH1 (e.g. IL-12) and TH17 (e.g. IL-23) stimulation conditions. To gain further insight into the expression profile of GM-CSF producing cells in an inflammatory setting that is more physiologically relevant to human disease, we evaluated the expression of IL-17 and IFN-γ by GM-CSF producing CD4+ T cells during EAE. Our data show that approximately half of the GM-CSF+ T cells also express either IL-17 or IFN-γ(Fig. 3C). A population of autoreactive T cells that only produce GM-CSF and do not produce either prototypical TH1 or TH17 cytokines was also detected. To further characterize this population of pathogenic T cells we also stained for IL-4 and IL-9 to see if they were TH2 or TH9 cells. However the population was not found to expression either IL-4 or IL-9 (Supplemental Fig. 2). GM-CSF production was also detected in a population of CD4+ T cells that produced both IL-17 and IFN-γ. Our data demonstrates that GM-CSF production is not restricted to discrete CD4+ T cells lineages during inflammation but is rather heterogeneously expressed in the autoreactive T cell compartment. Furthermore, our findings reveal that GM-CSF can be expressed in tandem with both TH1 and TH17 signature cytokines during inflammation. This helps to explain the ability of TH1 and TH17 MOG-specific T cells to induce demyelinating disease even in the absence of IFN-γ and IL-17. To evaluate whether γδ T cells are also a source of GM-CSF production during inflammation we measured the expression of GMCSF by γδ T cells using intracellular flow staining. Indeed, γδ T cells are a major innate source of GM-CSF in EAE (Fig. 3D).
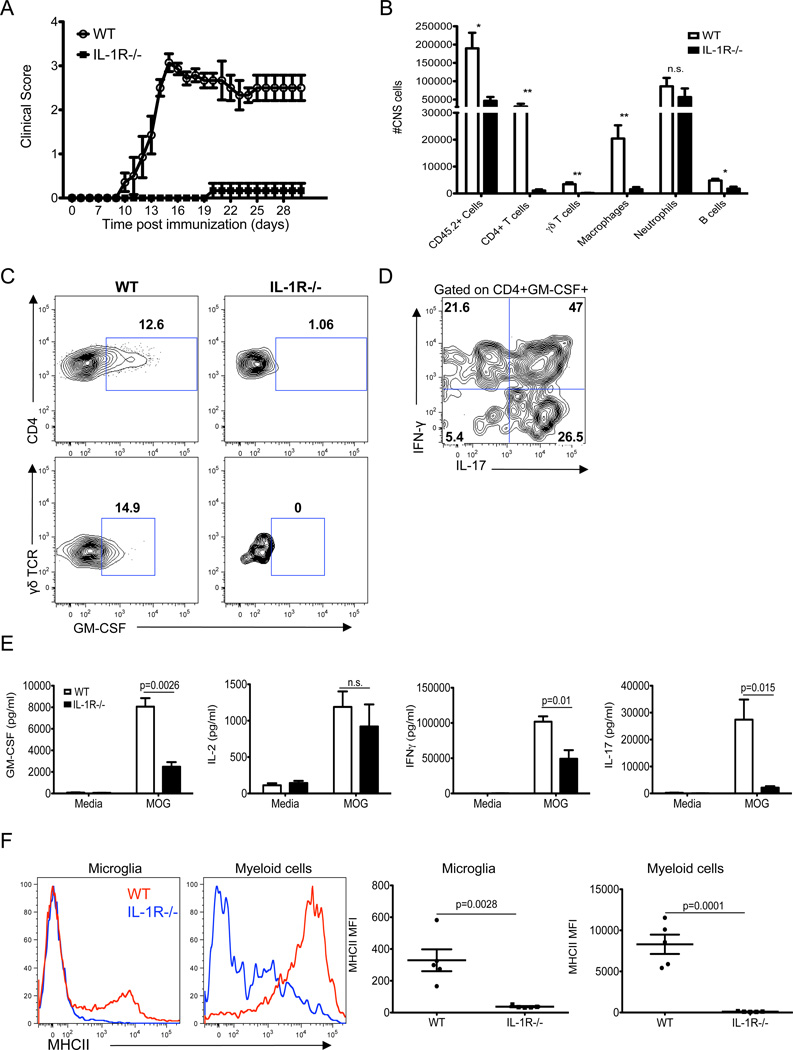
Next we evaluated the ability of IL-1 signaling to influence GM-CSF production and CNS inflammation during the effector phase of disease. Consistent with published studies (15) (16) (17), IL-1R−/− mice were protected from EAE disease symptoms (Fig. 4A) and this correlated with a significant reduction in the infiltration of inflammatory cells into the CNS (Fig. 4B). Infiltrating MOG-specific CD4+ T cells and γδ T cells produced elevated levels of GM-CSF in the CNS of WT mice (Fig. 4C). In contrast, deficiency in IL-1R resulted in complete abrogation of GM-CSF production by both CD4+ and γδ T cells in the CNS. Furthermore, when we expanded the GM-CSF+ CD4+ T cell population to assess how GM-CSF production is co-regulated with other cytokines in inflammatory environments we found that there is an enrichment of potentially highly pathogenic CD4+ T cells that co-express GM-CSF, IL-17 and IFN-γ in tandem (Fig. 4D). To further examine IL-1R mediated control of GM-CSF production during the effector phase of EAE we restimulated splenocytes with MOG peptide for 48hrs and measured the secretion of cytokines. Production of GM-CSF was compromised in IL-1R−/− mice, however production of IL-2 (Fig. 4E) and IL-1β (Supplemental Fig. 3) were unaffected. In addition, secretion of IFN-γ and IL-17 was also significantly affected by the absence of IL-1R. These findings confirm that IL-1R controls the encephalitogenicity of T cells by regulating pathogenic cytokine production including GM-CSF.
Figure 4. IL-1R regulates GM-CSF production in the CNS.
WT and IL-1R−/− mice were immunized with MOG/CFA. (A) Clinical scores were recorded daily for 30 days. (B) Absolute number of CD45+ cells, CD4+ T cells (CD45+CD4+TCRβ+), γδ T cells (CD45+γδ TCR+), macrophages (CD45hiCD11b+MHCII+), neutrophils (CD45+CD11b+Gr-1+MHCII−) and B cells (CD45+CD19+TCRβ−) in the CNS 18 days after immunization. (C) Intracellular staining of GM-CSF for CD4+ T cells (top panel) and γδ+ T cells (bottom panel) obtained from the CNS and stimulated with either MOG peptide (top panel) or PMA/ionomycin for 5 hrs. (D) Intracellular staining for IL-17 and IFN-γ in CD4+GM-CSF+ T cells obtained from the CNS of WT mice and stimulated with MOG peptide for 5hrs. (E) Splenocytes were stimulated for 48 hrs with MOG peptide and cytokines were measured by ELISA. (F) Expression of major histocompatibility complex class II (MHCII) by microglia (CD45.2intCD11b+) and myeloid cells (CD45hiCD11b+) 18 days after immunization. Data are representative of three independent experiments. Data represent mean ± SEM.
GM-CSF is believed to exacerbate neuroinflammation by promoting the activation of myeloid cells and microglia in the CNS (6) (3). Thus we next analyzed whether the diminished expression of GM-CSF that occurs in IL-1R−/− mice results in dampened antigen presenting cell (APC) activation in the CNS. Indeed, the expression of MHCII on both microglia and myeloid cells was reduced in the absence of IL-1R mediated GM-CSF production (Fig. 4F).
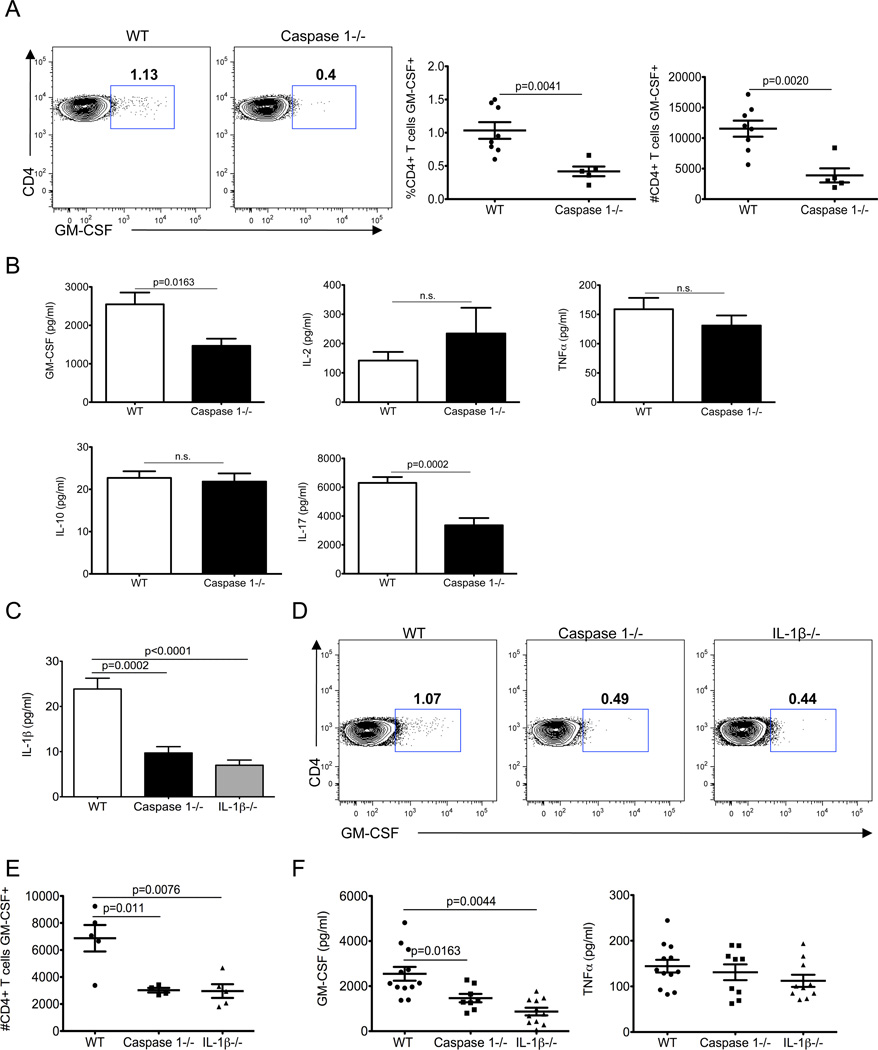
Inflammasome activation promotes the generation of GM-CSF producing T cells
Recent work by our lab and others has highlighted the importance of the inflammasome in the regulation of many IL-1 mediated inflammatory and autoimmune diseases including EAE (10) (12) (14) (13). However the role of the inflammasome in the induction of GM-CSF production remains unknown. To directly test this, EAE was induced in WT and caspase-1−/− mice and the generation of autoreactive GM-CSF producing T cells was evaluated at day 10 in the dLNs. The absence of caspase-1 resulted in a marked decrease in both the frequency and total number of autoreactive GM-CSF producing T cells (Fig. 5A). Splenocytes from these mice were restimulated with MOG peptide to measure cytokine secretion. The production of GM-CSF was significantly reduced in caspase-1−/− mice (Fig. 5B). However, the antigen-specific secretion of additional T cell derived cytokines including IL-2, TNF-α, and IL-10 was unaffected in caspase-1−/− mice. Although caspase-1 deficiency does significantly reduce GMCSF production, it is not to the same extent as seen in IL-1R−/− mice (Fig. 3). This might be the result of IL-1α, which can be produced independently of caspase-1 and inflammasome activation, providing compensatory IL-1 signaling. Overall, these findings clearly indicate that caspase-1 derived IL-1β can potently amplify T cell mediated GM-CSF production during the priming phase of EAE.
Figure 5. Caspase-1 induced production of IL-1β stimulates GM-CSF production.
WT and caspase-1−/− mice were immunized with MOG/CFA. (A) On day 10, dLN cells were stimulated with MOG peptide for 5 hrs followed by intracellular staining for GM-CSF. (B) Splenocytes on day 10 after immunization were stimulated for 48 hrs with MOG peptide and cytokines were measured by ELISA. Data are representative of three independent experiments with at least 4 mice per group. Data represent mean ± SEM. WT, caspase-1−/−, and IL-1β−/− were immunized with MOG/CFA. (C) On day 10, dLN homogenates were collected and IL-1β was measured by ELISA. (D) Cells were also stimulated with MOG peptide for 5 hrs and intracellular staining of GM-CSF was performed. (E) Absolute number of GM-CSF producing CD4+ T cells obtained from the dLNs at day 10 and stimulated with MOG peptide for 5 hrs. (F) Splenocytes were stimulated for 48 hrs with MOG peptide and cytokines were measured by ELISA. Data are representative of three independent experiments with at least 4 mice per group. Data represent mean ± SEM.
Caspase-1 mediated control of GM-CSF production is through IL-1β regulation
Caspase-1 activation following inflammasome complex formation results in the secretion of both IL-1β and IL-18. Both IL-1β and IL-18 can independently influence T cell responses including cytokine production and survival (19) (20). Furthermore caspase-1 can directly affect cell survival (21), which may influence the upstream control of GM-CSF by caspase-1. Thus we next examined whether caspase-1 imparts its function on GM-CSF production via the direct control IL-1β or through a secondary mechanism. To test this we compared the induction of GM-CSF+ MOG-specific CD4+ T cells in caspase-1−/− mice to mice that lack IL-1β. Genetic deletion of caspase-1 and IL-1β each led to considerable reductions in the amount of IL-1β that is secreted in the dLNs during EAE (Fig. 5C). Furthermore, the generation of GM-CSF producing CD4+ T cells and secretion of GM-CSF is abrogated to a similar extent in both caspase-1−/− and IL-1β−/− mice (Fig. 5D-5F). Collectively this data suggests that caspase-1 derived IL-1β is an important inducer of encephalitic GM-CSF+ T cells.
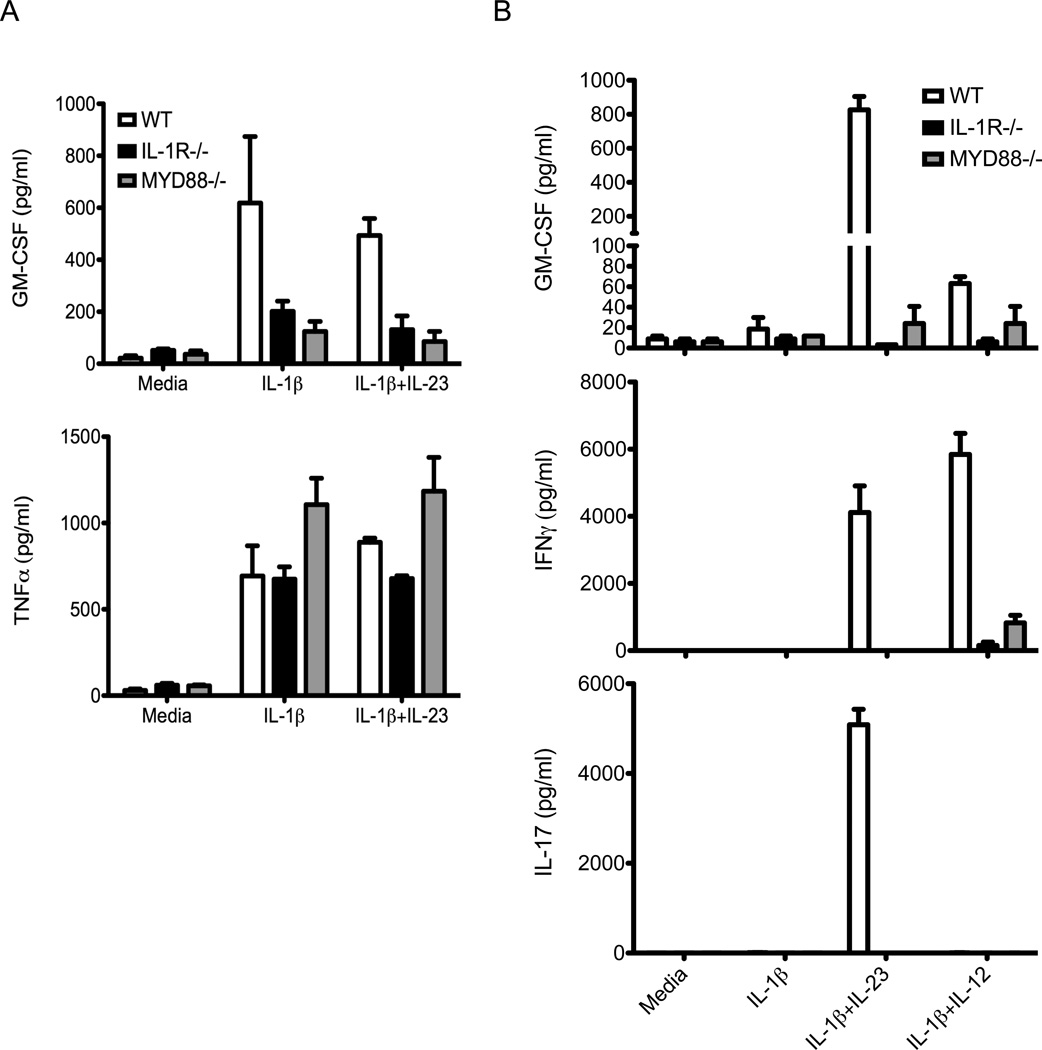
MYD88 controls GM-CSF production downstream of IL-1R
The downstream pathways that regulate IL-1R specific control of GM-CSF production by both conventional αβ and γδ T cells have not been fully characterized. MYD88 is a master regulator of innate immune responses including cytokine receptor signaling and cytokine production that results from pathogen recognition. However, recent findings suggest an important cell intrinsic role for MYD88 in T cell responses (22) (23) (24). To evaluate the role of MYD88 in the orchestration of IL-1R-dependent regulation of GM-CSF we FACs purified naïve T cells and γ δ T cells from WT, IL-1R−/−, and MYD88−/− mice and induced GM-CSF production with various stimuli. MYD88 was found to centrally influence GM-CSF production in T cells, as MYD88−/− T cells exhibited reduced secretion of GM-CSF in response to anti-CD3 stimulation and IL-1β treatment (Fig. 6A). Expression of TNF-α was not significantly altered in this assay suggesting that MYD88, similar to IL-1R, can exert specific control over GM-CSF production. In agreement with a central role for MYD88 in conventional T cells, MYD88 was also essential for the production of GM-CSF following stimulation with IL-1β and either IL-23 or IL-12 in γδ T cells (Fig. 6B). IL-1R−/− and MYD88−/− γδ T cells are similarly impaired in their ability to produce GM-CSF. Furthermore, cell autonomous deficiency in MYD88 renders γδ T cells unable to produce either IL-17 or IFN-γ in response to cytokine stimulation. This highlights an essential role for MYD88 in pathogenic cytokine production by γδ T cells. These data demonstrate that the IL-1R/MYD88 axis regulates GM-CSF production in both αβ and γδ T cells.
Figure 6. MYD88 directs IL-1R-mediated production of GM-CSF in αβ and γδ T cells.
Splenocytes and lymph node cells were harvested from WT, IL-1R−/−, or MYD88−/− mice. (A) Sorted naïve CD4+ T cells (CD4+CD44loCD25−) were cultured with WT bone marrow-derived dendritic cells (BMDCs) and stimulated with anti-CD3 alone or in the presence of IL-1β or combined IL-1β and IL-23. Supernatants were collected at 72 hrs and cytokines were measured by ELISA. (B) Sorted γδ T cells were stimulated with IL-1β, IL-1β and IL-23, or IL-1β and IL-12. Supernatants were collected after 72 hrs and cytokines were measured by ELISA. Data are representative of two independent experiments with 2–3 mice per group. Data represent mean ± SEM.
DISCUSSION
Recently, GM-CSF has emerged as a central pathogenic cytokine involved in the progression of experimental autoimmune encephalomyelitis (EAE) and other autoimmune and inflammatory diseases. Despite the important identification of the indispensible role of GM-CSF in the encephalitogenicity of both TH17 and TH1 cells (3, 4), the signaling pathways that promote the induction of GM-CSF in both cell lineages still remain to be formally elucidated. IL-1 was recently shown to enhance the production of GM-CSF by CD4+ T cells following in vitro stimulation (4). However, the absolute requirement for IL-1 signaling in the generation of GM-CSF secreting T cells under various stimulatory conditions was not addressed. Furthermore, prior to our report the in vivo requirement for IL-1 signaling in the induction and maintenance of GM-CSF responses remained unclear.
In this study, we show that signaling downstream of IL-1R is essential for the secretion of GM-CSF following polyclonal T cell stimulation with anti-CD3. Furthermore, IL-1 signaling was necessary for the induction of GM-CSF production following stimulation under TH1 (i.e. IL-12) and TH17 (i.e. IL-23) inducing conditions. Importantly, IL-1R was also required for optimal generation of GM-CSF producing T cell in vivo. These findings suggest that IL-1 signaling is a central regulator of GM-CSF induction in T cells. Upstream of IL-1R we identify inflammasome-derived IL-1β as an important amplifier of GM-CSF producing T cell responses. A recent study showed that GM-CSF can dramatically boost inflammasome-mediated IL-1β production in macrophages (25). Thus it is conceivable to envision that GM-CSF may promote additional production of IL-1β by myeloid cells and microglia in the inflamed CNS and that this creates a proinflammatory feedback loop that potentiates neuroinflammation during EAE and MS.
Recently, it was discovered that caspase-1 deficient mice also lack caspase-11 (26). It turns out that mouse strain 129 and 129-derived embryonic stem cells lack expression of caspase-11 due to a 5-base-pair deletion that impairs exon splicing and as a result caspase-1 null mice also lack casp11. In this study we find that the production of GM-CSF by autoreactive T cells is equally abrogated in both caspase-1 KO (actually deficient in both caspase-1 and caspase-11) and IL-1β KO mice. The fact that IL-1β−/− mice phenocopy the results generated utilizing caspase 1−/− mice suggest a specific role for caspase-1 and downstream IL-1β in the regulation of GM-CSF production during EAE.
Increasing evidence points to a central role for innate cell populations in many autoimmune diseases including EAE (18, 27). For instance, γδ T cells have been shown to exacerbate neuroinflammation during demyelinating autoimmune disease (28). Prior to our report, the ability of non-T cells to contribute to GM-CSF-mediated inflammation during EAE remained unknown. Herein, we demonstrate that γδ T cells are a major source of GM-CSF in the CNS during neuroinflammation. We find that IL-1β synergizes with either IL-23 or, to a lesser extent, IL-12 to promote GM-CSF production by γδ T cells. Furthermore, the IL-1R/MYD88 signaling axis was found to be indispensible for γδ T cell-mediated production of GM-CSF. Memory CD4+ T cells were also found to secrete GM-CSF in response to IL-1β and IL-23 in the absence TCR engagement, albeit at much lower levels than γδ T cells. Production of GM-CSF by memory CD4+ T cells was also dependent on IL-1 signaling. To our knowledge, our findings demonstrate for the first time that γδ T cells contribute GM-CSF during EAE in a manner that relies on IL-1 signaling.
Our findings suggest that GM-CSF production by autoreactive T cells is not restricted to discrete helper CD4+ T cell lineages, but is rather heterogeneously expressed in the effector T cell population. We found that approximately half of all GM-CSF producing T cells also produce either IL-17 or IFN-γ during the priming phase of EAE. This data helps to reconcile how TH17 and TH1 cells can still provoke demyelinating disease even in the absence of their signature cytokine, IL-17 and IFN-γ respectively (1) (2). Furthermore autoreactive CD4+ T cells that solely produce GM-CSF and that do not express either prototypical TH17 or TH1 cytokines were also detected. We also revealed that a substantial population of pathogenic CD4+ T cells co-express GM-CSF, IL-17, and IFN-γ, and that this population is highly enriched in the CNS of mice with severe demyelinating disease. Populations of CD4+ T cells that co-express IL-17 and IFN-γ have been isolated from MS patients with severe disease (29). Moreover, autoreactive CD4+ T cells that co-produce IL-17 and IFN-γ are highly pathogenic in many inflammatory diseases. Thus, expression of GM-CSF by myelin-reactive T cells that co-express IL-17 and IFN-γ may be responsible for the highly encephalitogenic nature of this population.
In conclusion, our studies reveal that inflammasome derived IL-1β and the IL-1R/MYD88 signaling axis control demyelinating disease during EAE through the regulation of autoreactive GM-CSF-producing T cells. Furthermore, the production of GM-CSF was not limited to a defined helper CD4+ T cell subset but was rather globally expressed by MOG-specific T cells in vivo. We identify IL-1β as the primary inflammasome induced cytokine that amplifies GM-CSF production during the priming phase of disease. IL-1 signaling also potentially contributes to disease progression by enhancing the production of GM-CSF from γδ T cells. We also demonstrate an essential role for MYD88 in IL-1R-mediated control of GM-CSF production in both conventional αβ and γδ T cells. The identification of the central pathways that influence IL-1R-mediated regulation of GM-CSF may provide potential targets in the treatment of numerous inflammatory and autoimmune diseases.
Supplementary Material
ACKNOWLEDGEMENTS
We thank Gordon Johnson and Kathleen Branscum for help with animal colony management and other support. We thank members of the St. Jude Immunology FACS core facility and the St. Jude Hartwell Center for their technical support. We thank Gabriel Nuñez (University of Michigan) and Richard Flavell (Yale) for generous supply of mutant mice.
This work is supported by US National Institutes of Health grants AR056296 and AI088177, and the American Lebanese Syrian Associated Charities to T-D. K.
Abbreviations
- CNS
central nervous system
- dLN
draining LN
- EAE
experimental autoimmune encephalomyelitis
- GM-CSF
granulocyte-macrophage colony-stimulating factor
- IL-1R
interleukin-1 receptor type 1
- IFN
interferon
- NLR
Nod-like receptor
- MOG
myelin oligodendrocyte glycoprotein
- MS
multiple sclerosis
- PMA
phorbol 12-myristate 13-acetate
Footnotes
The authors declare that they have no competing financial interests.
REFERENCES
- 1.Chu CQ, Wittmer S, Dalton DK. Failure to suppress the expansion of the activated CD4 T cell population in interferon gamma-deficient mice leads to exacerbation of experimental autoimmune encephalomyelitis. J Exp Med. 2000;192:123–128. doi: 10.1084/jem.192.1.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haak S, Croxford AL, Kreymborg K, Heppner FL, Pouly S, Becher B, Waisman A. IL-17A and IL-17F do not contribute vitally to autoimmune neuro-inflammation in mice. J Clin Invest. 2009;119:61–69. doi: 10.1172/JCI35997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Codarri L, Gyulveszi G, Tosevski V, Hesske L, Fontana A, Magnenat L, Suter T, Becher B. RORgammat drives production of the cytokine GM-CSF in helper T cells, which is essential for the effector phase of autoimmune neuroinflammation. Nat Immunol. 2011;12:560–567. doi: 10.1038/ni.2027. [DOI] [PubMed] [Google Scholar]
- 4.El-Behi M, Ciric B, Dai H, Yan Y, Cullimore M, Safavi F, Zhang GX, Dittel BN, Rostami A. The encephalitogenicity of T(H)17 cells is dependent on IL-1- and IL-23-induced production of the cytokine GM-CSF. Nat Immunol. 2011;12:568–575. doi: 10.1038/ni.2031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kroenke MA, Chensue SW, Segal BM. EAE mediated by a non-IFN-gamma/non-IL-17 pathway. Eur J Immunol. 2010;40:2340–2348. doi: 10.1002/eji.201040489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ponomarev ED, Shriver LP, Maresz K, Pedras-Vasconcelos J, Verthelyi D, Dittel BN. GM-CSF production by autoreactive T cells is required for the activation of microglial cells and the onset of experimental autoimmune encephalomyelitis. J Immunol. 2007;178:39–48. doi: 10.4049/jimmunol.178.1.39. [DOI] [PubMed] [Google Scholar]
- 7.Dinarello CA. Interleukin-1 in the pathogenesis and treatment of inflammatory diseases. Blood. 2011;117:3720–3732. doi: 10.1182/blood-2010-07-273417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lukens JR, Dixit VD, Kanneganti TD. Inflammasome activation in obesity-related inflammatory diseases and autoimmunity. Discov Med. 2011;12:65–74. [PMC free article] [PubMed] [Google Scholar]
- 9.Shaw PJ, McDermott MF, Kanneganti TD. Inflammasomes and autoimmunity. Trends Mol Med. 2011;17:57–64. doi: 10.1016/j.molmed.2010.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shaw PJ, Lukens JR, Burns S, Chi H, McGargill MA, Kanneganti TD. Cutting edge: critical role for PYCARD/ASC in the development of experimental autoimmune encephalomyelitis. J Immunol. 2010;184:4610–4614. doi: 10.4049/jimmunol.1000217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matsuki T, Nakae S, Sudo K, Horai R, Iwakura Y. Abnormal T cell activation caused by the imbalance of the IL-1/IL-1R antagonist system is responsible for the development of experimental autoimmune encephalomyelitis. Int Immunol. 2006;18:399–407. doi: 10.1093/intimm/dxh379. [DOI] [PubMed] [Google Scholar]
- 12.Furlan R, Martino G, Galbiati F, Poliani PL, Smiroldo S, Bergami A, Desina G, Comi G, Flavell R, Su MS, Adorini L. Caspase-1 regulates the inflammatory process leading to autoimmune demyelination. J Immunol. 1999;163:2403–2409. [PubMed] [Google Scholar]
- 13.Gris D, Ye Z, Iocca HA, Wen H, Craven RR, Gris P, Huang M, Schneider M, Miller SD, Ting JP. NLRP3 plays a critical role in the development of experimental autoimmune encephalomyelitis by mediating Th1 and Th17 responses. J Immunol. 2010;185:974–981. doi: 10.4049/jimmunol.0904145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lalor SJ, Dungan LS, Sutton CE, Basdeo SA, Fletcher JM, Mills KH. Caspase-1-processed cytokines IL-1beta and IL-18 promote IL-17 production by gammadelta and CD4 T cells that mediate autoimmunity. J Immunol. 2011;186:5738–5748. doi: 10.4049/jimmunol.1003597. [DOI] [PubMed] [Google Scholar]
- 15.Sutton C, Brereton C, Keogh B, Mills KH, Lavelle EC. A crucial role for interleukin (IL)-1 in the induction of IL-17-producing T cells that mediate autoimmune encephalomyelitis. J Exp Med. 2006;203:1685–1691. doi: 10.1084/jem.20060285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chung Y, Chang SH, Martinez GJ, Yang XO, Nurieva R, Kang HS, Ma L, Watowich SS, Jetten AM, Tian Q, Dong C. Critical regulation of early Th17 cell differentiation by interleukin-1 signaling. Immunity. 2009;30:576–587. doi: 10.1016/j.immuni.2009.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCandless EE, Budde M, Lees JR, Dorsey D, Lyng E, Klein RS. IL-1R signaling within the central nervous system regulates CXCL12 expression at the blood-brain barrier and disease severity during experimental autoimmune encephalomyelitis. J Immunol. 2009;183:613–620. doi: 10.4049/jimmunol.0802258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cua DJ, Tato CM. Innate IL-17-producing cells: the sentinels of the immune system. Nat Rev Immunol. 2010;10:479–489. doi: 10.1038/nri2800. [DOI] [PubMed] [Google Scholar]
- 19.Ben-Sasson SZ, Caucheteux S, Crank M, Hu-Li J, Paul WE. IL-1 acts on T cells to enhance the magnitude of in vivo immune responses. Cytokine. 2011;56:122–125. doi: 10.1016/j.cyto.2011.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nakanishi K, Yoshimoto T, Tsutsui H, Okamura H. Interleukin-18 regulates both Th1 and Th2 responses. Annu Rev Immunol. 2001;19:423–474. doi: 10.1146/annurev.immunol.19.1.423. [DOI] [PubMed] [Google Scholar]
- 21.Kufer TA, Sansonetti PJ. NLR functions beyond pathogen recognition. Nat Immunol. 2011;12:121–128. doi: 10.1038/ni.1985. [DOI] [PubMed] [Google Scholar]
- 22.Zhou S, Kurt-Jones EA, Cerny AM, Chan M, Bronson RT, Finberg RW. MyD88 intrinsically regulates CD4 T-cell responses. J Virol. 2009;83:1625–1634. doi: 10.1128/JVI.01770-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rahman AH, Cui W, Larosa DF, Taylor DK, Zhang J, Goldstein DR, Wherry EJ, Kaech SM, Turka LA. MyD88 plays a critical T cell-intrinsic role in supporting CD8 T cell expansion during acute lymphocytic choriomeningitis virus infection. J Immunol. 2008;181:3804–3810. doi: 10.4049/jimmunol.181.6.3804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.LaRosa DF, Stumhofer JS, Gelman AE, Rahman AH, Taylor DK, Hunter CA, Turka LA. T cell expression of MyD88 is required for resistance to Toxoplasma gondii. Proc Natl Acad Sci U S A. 2008;105:3855–3860. doi: 10.1073/pnas.0706663105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khameneh HJ, Isa SA, Min L, Nih FW, Ruedl C. GM-CSF signalling boosts dramatically IL-1 production. PLoS One. 2011;6:e23025. doi: 10.1371/journal.pone.0023025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kayagaki N, Warming S, Lamkanfi M, Vande Walle L, Louie S, Dong J, Newton K, Qu Y, Liu J, Heldens S, Zhang J, Lee WP, Roose-Girma M, Dixit VM. Non-canonical inflammasome activation targets caspase-11. Nature. 2011;479:117–121. doi: 10.1038/nature10558. [DOI] [PubMed] [Google Scholar]
- 27.Hayday AC. Gammadelta T cells and the lymphoid stress-surveillance response. Immunity. 2009;31:184–196. doi: 10.1016/j.immuni.2009.08.006. [DOI] [PubMed] [Google Scholar]
- 28.Sutton CE, Lalor SJ, Sweeney CM, Brereton CF, Lavelle EC, Mills KH. Interleukin-1 and IL-23 induce innate IL-17 production from gammadelta T cells, amplifying Th17 responses and autoimmunity. Immunity. 2009;31:331–341. doi: 10.1016/j.immuni.2009.08.001. [DOI] [PubMed] [Google Scholar]
- 29.Kebir H, Ifergan I, Alvarez JI, Bernard M, Poirier J, Arbour N, Duquette P, Prat A. Preferential recruitment of interferon-gamma-expressing TH17 cells in multiple sclerosis. Ann Neurol. 2009;66:390–402. doi: 10.1002/ana.21748. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.