Abstract
This community-based study examined physical activity (PA) in relation to cardiometabolic risk factors among 223 adult, immigrant Latina women who were overweight or obese. Participants were predominantly of Mexican descent, married and low-income. Data were obtained through accelerometer readings and clinical measures (e.g., BMI, waist circumference, blood pressure, lipid profile, fasting blood sugar). Findings showed that many women were active (mean step count = 8,575 ± 3,191); 27.6 % achieved 10,000 steps per day, and only 11 % were sedentary. They engaged in short bouts of moderate PA rather than long-sustained moderate-to-vigorous activity. Three or more MetS traits were present in 45.3 % of the women, raising concerns about risk for diabetes and cardiovascular disease. More active women had lower BMI, weight, waist circumference, and triglycerides levels. Results point to the importance of targeting maintenance of PA in active women and intervening with culturally tailored programs to promote healthier behavior in those who are sedentary or somewhat active.
Keywords: Physical activity, Cardiometabolic, Overweight, Latina, Women
Background
The obesity epidemic, a major public health challenge, dis-proportionately affects Latinos, the fastest growing ethnic minority population in the US. Compared to non-Latino whites (NLW), Latinos have a 21 % greater prevalence of obesity [1], while Mexican–American (MA) women are 1.5 times as likely to be obese as women in general [2]. Low-income Latina women, particularly those of Mexican descent, face increased risk for cardiovascular disease (CVD) and other chronic illnesses due to overweight/obesity, sedentary lifestyle [2, 3], and other risk factors such as type 2 diabetes (T2D), hypertension [4], and dyslipidemia [5]. Metabolic syndrome (MetS), the constellation of metabolic abnormalities including dyslipidemia, hypertension, hyperglycemia, and obesity, is associated with increased risk of diabetes [6] and CVD [7-9]. MA women are 1.5 times as likely to have MetS as NLW women [5], with abdominal obesity being the most common MetS trait reported in the former group [10].
MetS and its primary clinical manifestations, CVD and T2D, may be reduced by physical activity (PA) and diet [11]. Moderate-intensity PA for as little as 30 min a day, 5 days a week, reduces risk of CVD in adults [12]. Despite increasing awareness of this preventive health strategy in the general population, low levels of PA continue to pre- vail, particularly among MA women [2, 3, 13], of whom only 21.9 % meet federal PA recommendations [14].
Past studies demonstrate the health benefits of PA in increasing cardiovascular fitness, control of hypertension [15], and glycemic control [16, 17], and decreasing CVD risk [18]. Moreover, the benefits of PA, regardless of weight loss or category of body weight, are supported by large epidemiologic studies showing more active persons have reduced risk of CVD and all-cause mortality [19, 20]. Recent data indicate that engaging in light or moderate/vigorous PA is associated with a decrease in risk of CVD mortality of approximately 30 %, a relationship not notably weakened in the presence of metabolic risk factors such as dyslipidemia and obesity [21]. A Cochrane review noted that exercise resulted in only marginal weight loss in overweight/obese people but significantly improved lipids and blood pressure (BP) [22]. Similarly, the preponderance of evidence in another review indicated that aerobic exercise resulted in positive alterations in lipoproteins in both normolipidemic and dyslipidemic individuals, with most consistent findings demonstrated for increase in HDL-C [19]. Findings from the 2003–2006 National Health and Nutrition Examination Survey (NHANES) showed that moderate-to-vigorous PA was independently associated with HDL-C in predominantly overweight or obese adults [23]. The few studies examining the effects of PA interventions with Latinos reveal mixed findings [24]. Positive outcomes have included improvements in BMI [25], total cholesterol (Total-C) [26, 27], lower triglycerides (TG), higher fat-free mass, maximum aerobic fitness (VO2max) [28], and increased activity levels [29-31]. However, a limitation of many prior studies is self-report of PA levels [32]. Comparison of self-reported versus actual measured PA (by accelerometer, pedometer, or indirect methods) shows that women report significantly (183 %) higher PA than objectively measured [33]. Subjective over-reporting of PA has been confirmed in a recent study comparing Latino and NLW populations [34].
In response to the need for improved measurement of PA and its correlates as well as the limited research involving Latina women, we conducted a community-based investigation using accelerometer readings and objective clinical measures. We report PA levels in relation to MetS factors specified by the American Heart Association [35] in overweight/obese Latina women, predominantly of Mexican descent.
Methods
Data were obtained as part of a randomized controlled trial examining the effects of a 6-month lifestyle behavior intervention involving overweight/obese Latina women. Only baseline data (collected prior to initiation of intervention) are included in the current analyses. All research protocols were approved by the Institutional Review Board of the University of California, Los Angeles (UCLA).
Participants
Participants were recruited from December 2009 through July 2010 from community settings such as parent education centers, churches, laundromats, and organizations providing services to children and families (e.g., English-as-a-Second-Language classes, job training). These were located within two adjacent communities of Los Angeles County with similar sociodemographic profiles. The women met the following criteria: self-reported Latina, 35–64 years of age, Spanish- and/or English-speaking, and BMI of ≥25. Those with impaired physical mobility, type 1 diabetes, uncontrolled hypertension, or history of a heart attack or stroke were excluded.
Data Collection
The bilingual, bicultural team of data collectors included community health workers (promotoras) and a registered nurse who performed assessments of lipids, fasting blood sugar (FBS), and BP. Multiple morning data collection sessions were held to accommodate the schedules of participants and the fasting status necessary for blood sample collection. Questionnaires were administered via private one-to-one interviews in Spanish. Participants received a $25 gift card for the evaluation.
Measures
Physical activity
The Kenz Lifecorder Plus (Kenz, Nagoya, Japan), an accelerometer with established reliability and validity [36-40], was used to measure PA. This device measures vertical acceleration 10 times each second; data are aggregated over a 4-s interval (epoch), to generate a number of “counts,” providing a “real-time” index (every 2 min) of the amount of body movement. Freedson et al. [41] demonstrated that activity counts and steady-state oxygen consumption are highly correlated (r = 0.88). The Lifecorder activity counts were converted into METS (1 MET = 3.5 mL/kg min), thus enabling us to classify intensity according to accepted standards as well as calculate step counts. Participants were instructed to wear the monitor for 7 consecutive days during all waking hours except when bathing. After receiving verbal instructions to wear the accelerometer during all hours awake for 7 consecutive days and a demonstration on placement of the device, written protocols were provided with picture illustrations. Total activity level for each participant was averaged for each day and for the entire 7-day period. A minimum of 4 days of data (≥8 h/day) was required for inclusion in the analyses. Research findings on overweight and obese individuals show minimal difference in PA patterns using 8 to 12 h of data from 4 to 6 days of monitoring, with or without weekend days [42]. By recording PA with accelerometers for 21 consecutive days, Matthews and associates [43] demonstrated that as few as 3–4 days of monitoring was required to achieve 80 % reliability for measuring activity counts and time spent in moderate-to-vigorous activity. A subsequent review of accelerometer-based activity assessments showed 3–5 days of monitoring is sufficient for reliably estimating usual or habitual physical activity [44].
Cardiometabolic characteristics
We examined physiologic measures comprising the MetS in women, as defined by the US National Cholesterol Education Program-Adult Treatment Panel (NCEP-ATP III) [45]; these include (1) waist circumference> 88 cm; (2) serum TG ≥ 150 mg/dL; (3) high-density lipoprotein (HDL-C)<50 mg/dL; (4) BP ≥ 130/85 mm Hg; and (5) FBS ≥ 110 mg/dL. In classifying MetS traits, we included women being treated for diabetes or hypertension with medication in accordance with the revised NCEP definition [46]. Systolic and diastolic BP were taken following JNC7 [47] procedural guidelines, using a Welch Allyn and Tycos BP Kit with TR-2 ProCheck Home Aneroid and Stethoscope. This device meets the AAMI accuracy standard of 3 mmHg. Elevated BP readings were rechecked using a mercury sphygmomanometer (average of 3 readings) [47]. The FDA-approved Cholestech LDX System was used to measure Total-C, HDL-C, low-density lipoprotein (LDL-C), TG, and FBS. The Cholestech is Clinical Laboratory Improvement Amendments-waived and meets NCEP guidelines for precision and accuracy. The SECA 769 digital scale was used to measure weight with women wearing light clothing and no shoes. Height was measured using a SECA 220 Hite-Mobile Portable Stadiometer. BMI was calculated as weight in kilograms divided by the square of height in meters. Waist circumference was evaluated with a Gulick tape measure following National Obesity Expert Panel Report guidelines [48].
Background Questionnaire
Demographic and background information included age, ethnicity, place of birth, education, income, and health history (e.g., hypertension, diabetes, depression). The General Acculturation Index examined cultural orientation and level of involvement in Latino culture (α ≥ 0.80) [49]. The 5 items evaluated linguistic capabilities in speaking and reading English and Spanish, place of childhood residence, ethnic identity of friends, and level of pride in heritage. Item responses and overall scores ranged from Latino (1) to Anglo (5) orientation. Residence index was calculated by subtracting age from years in the US, with smaller negative number closer to zero indicating greater acculturation [50, 51].
Statistical Analysis
Data analyses were performed using SPSS Version 19. Average daily steps, minutes in moderate activity, and minutes in bouts of moderate activity (1 bout ≥10 consecutive minutes in continuous PA at ≥3 METS) were calculated from Lifecorder readings. Sedentary states were indicated by readings of 0.5 METS, whereas 0 METS indicated that the accelerometer was not being worn. Review of the data revealed no evidence of manipulated recordings due to device misuse (e.g., shaking device to increase PA intensity or step count). Thirteen participants were excluded from PA analyses because they did not meet the previously described accelerometer recording criteria. Pearson correlations were computed to examine the relationships of PA with cardiometabolic characteristics. To provide an additional perspective, differences in clinical variables among PA groups (<5,000, 5,000–7,499, 7,500–9,999, and ≥10,000 average daily steps) were evaluated using analysis of variance (ANOVA). A second set of these analyses controlled for age; however, because age-adjusted results did not result in substantive differences in interpretation (based on significance or effect sizes), only the simple (not age-adjusted results) are presented in this paper.
Results
Sociodemographic Background, Cardiometabolic Characteristics, and Physical Activity
Table 1 presents the sample characteristics of 223 Latina women: mean age 44.6 ± 7.9 years, predominantly low-income and of Mexican descent, partnered, unemployed, and with 8th grade education or less. Although acculturation level was low, the period of residence in the US was relatively long, as shown in the mean years living in the US and residence index. Mexico was the birthplace of 84.8 % of the participants and, as anticipated, 99 % of their parents. Diabetes and hypertension rates, based on our clinical data or use of medication, were 6.3 and 12.1 %, respectively. Twenty-three participants reported taking antihypertensive medications.
Table 1.
Sociodemographic characteristics of participants (N = 223)
| Characteristic | Mean ± SD | Range |
|---|---|---|
| Age (years) | 44.61 ± 7.92 | 35–64 |
| Acculturationa | 1.48 ± 0.45 | 1–3.40 |
| Mean years living in USb | 18.62 ± 8.26 | 1–40 |
| Residence indexc | −25.80 ± 8.13 | (−61)–(−5) |
| Frequency | Percent | |
|---|---|---|
| Birth place | ||
| Mexico | 187 | 83.9 |
| US (but raised in Mexico) | 4 | 1.8 |
| Other (Dominican, Central or South American) | 32 | 14.3 |
| Education | ||
| ≤8th grade | 117 | 52.6 |
| Some HS & high school graduate | 75 | 33.6 |
| Some college/trade school | 19 | 8.5 |
| College degree or higher | 9 | 4.0 |
| Refused/don’t know/missing | 3 | 1.3 |
| Marital status | ||
| Married/living with partner | 161 | 72.2 |
| Divorced/widowed/single | 62 | 27.8 |
| Income | ||
| ≤ 20,000 | 122 | 54.8 |
| $20,001-$40,000 | 64 | 28.7 |
| $40,001-$75,000 | 37 | 16.5 |
| Unemployed | 166 | 74.4 |
| Uninsured/no health insurance | 152 | 68.2 |
| Current smoker | 7 | 3.1 |
| Diabetes (FBS ≥126 mg/dL or on antidiabetic therapy) |
14 | 6.3 |
| Hypertension (BP ≥ 140/90 mmHg or on antihypertensive medications) |
27 | 12.1 |
Based on 1–5 questions with the rating scale: (1) only Spanish, (2) Spanish better than English, (3) both English and Spanish equally well, (4) English better than Spanish, (5) only English. Higher score means more acculturated
Based on responses of 204 women; excludes 11 (4.9 %) women responding >25 years and 8 who did not know or refused to respond
Residence index calculated as “years in US–age”; smaller negative number closer to zero indicates greater years in US and suggests higher acculturation
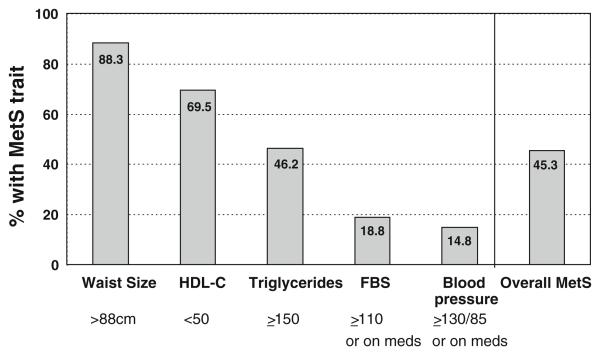
Table 2 presents cardiometabolic characteristics, and PA. The large majority of participants were classified as obese (n = 131, 58.7 %), with nearly 11 % of these reaching morbid obesity (class 3). Several individual MetS traits were prevalent (see Fig. 1); the most common (88.3 %) was elevated waist circumference, followed by low HDL-C and hypertriglyceridemia. Using the previously described NCEP-ATPIII criteria, 45.3 % of the women were classified as having MetS. The prevalence rose to 55.6 % when all of the revised MetS criteria for women were applied, i.e., FBS ≥ 100 mg/dL, waist circumference ≥88 cm [46].
Table 2.
Cardiometabolic characteristics and physical activity of participants (N = 223)
| Characteristic | Mean ± SD | Risk classification: frequency (%) |
|---|---|---|
| BMI (kg/m2) | 32.62 ± 5.68 | Overweight: 92 (41.3 %), obese I: 65 (29.1 %), obese II: 42 (18.8 %), obese III: 24(10.8 %) |
| Weight (lbs)st | 175.05 ± 32.60 | |
| Waist (cm) | 101.39 ± 11.47 | Over 88 cm (35 in): 197 (88.3 %) |
| Systolic BP (mmHg) | 114.08 ± 13.25 | SBP < 120: 150 (67.3 %), 120–129: 48 (21.5 %), 130–139: 18 (8.1 %), 140 or above: 7 (3.1 %) |
| Diastolic BP (mmHg) | 75.43 ± 8.98 | DBP < 85: 186 (83.4 %), 85–89: 26(11.7 %), 90 or above: 11 (4.9 %) |
| LDL-C (mg/dL)a | 111.56 ± 29.23 | LDL-C < 100: 73 (32.7 %), 100–129: 85 (38.1 %), 130–159: 45 (20.2 %), 160 or above: 11 (4.9 %), missing: 9 (4.0 %) |
| HDL-C (mg/dL) | 44.50 ± 13.37 | HDL-C 60 or above: 24 (10.8 %), 50–59: 43 (19.3 %), 40–49: 66 (29.6 %), < 40: 90 (40.3 %) |
| Total-C (mg/dL) | 188.44 ± 33.85 | TOTAL-C < 200: 150 (67.3), 200–239: 55 (24.7 %): 240 or above: 18 (8.1 %) |
| Triglycerides (mg/dL) | 164.96 ± 87.87 | TG < 150: 120 (53.8 %), 150–199: 48 (21.5 %), 200–499: 53 (23.8 %); 500 or above: 2 (0.9 %) |
| Fasting blood sugar (mg/dL) | 100.43 ± 18.78 | FBS 110 or above: 40 (17.9 %) |
| Physical activityb | ||
| Daily steps | 8,575 ± 3,191 | <5,000 (sedentary): 23 (11.0 %), 10,000 or above: 58 (27.6 %) |
| Daily minutes in moderate PA | 22.6 ± 18.9 | 30 min or more: 53 (25.2 %) |
| Daily minutes in bouts of moderate PA | 16.9 ± 20.5 |
Based on n = 214 because Cholestech unable to calculate LDL (n = 9) when triglycerides result is >400 mg/dL
Physical activity daily steps and daily minutes in moderate physical activity are based on n = 210
Fig. 1.
Percentage of participants with MetS traits (N = 223)
Levels of PA, as demonstrated by accelerometer step counts, were surprisingly high (8,575 ± 3,191), with 27.6 % of the women achieving 10,000 steps per day. Only 11 % were classified as “sedentary” based on an average daily step count <5,000, and 25.2 % were able to sustain moderate activity (≥3 METS) for 30 min or more daily. Women averaged 22.6 ± 18.9 min of moderate activity per day and 16.9 ± 20.5 min in bouts of moderate activity.
Correlations Between Physical Activity and Cardiometabolic Characteristics
Bivariate correlations between PA and clinical measures are reported in Table 3. BMI, weight, and waist circumference were inversely associated with average number of daily steps (p < 0.001, p < 0.001, p = 0.004, respectively). Average number of minutes in moderate PA was correlated with weight and waist circumference (p = 0.005, p = 0.026, respectively), indicating that greater PA was associated with more favorable anthropometric profiles. TG level was negatively correlated with average daily step count (p = 0.009). Positive associations were found between minutes in moderate PA and HDL-C (p = 0.038) and Total-C (p = 0.037).
Table 3.
Correlations between physical activity and cardiometabolic characteristics
| Clinical measure | Average daily steps |
Minutes in moderate physical activity |
Minutes in bouts of moderate physical activitya |
|||
|---|---|---|---|---|---|---|
| Pearson correlation | P | Pearson correlation | P | Pearson correlation | P | |
| Age | 0.007 | 0.920 | 0.058 | 0.401 | 0.097 | 0.163 |
| BMI | −0.295 | <0.001 | −0.135 | 0.051 | −0.116 | 0.092 |
| Weight (lbs) | −0.283 | <0.001 | −0.195 | 0.005 | −0.143 | 0.039 |
| Waist (cm) | −0.198 | 0.004 | −0.153 | 0.026 | −0.109 | 0.116 |
| Blood pressure | ||||||
| SBP | −0.099 | 0.154 | −0.023 | 0.737 | 0.033 | 0.626 |
| DBP | −0.107 | 0.124 | 0.061 | 0.381 | 0.058 | 0.403 |
| Cholesterol | ||||||
| LDL-C | 0.070 | 0.325 | 0.110 | 0.121 | 0.122 | 0.084 |
| HDL-C | 0.017 | 0.804 | 0.144 | 0.038 | 0.004 | 0.952 |
| Total-C | −0.039 | 0.571 | 0.144 | 0.037 | 0.043 | 0.534 |
| TG | −0.181 | 0.009 | 0.038 | 0.586 | −0.106 | 0.126 |
| FBS | −0.077 | 0.265 | −0.077 | 0.268 | −0.088 | 0.206 |
Bout of physical activity measured as ≥10 consecutive minutes at METS > 3
Bold values indicate significant findings
Differences in Cardiometabolic Characteristics by Step Category
Because PA is associated with lower risk for CVD and other chronic diseases, participants were classified into four groups based on average mean number of daily steps (Table 4). ANOVA revealed significant differences for BMI (F = 5.550, p < 0.001), weight (F = 5.877, p < 0.001) and TG (F = 3.108, p = 0.027), with those in the highest PA category exhibiting more favorable levels. Potential confounders were examined in two ways. Chi square and analysis of variance examined the relationship of baseline demographic characteristics on physical activity (step categories); findings revealed no significant differences and thus were not considered in the subsequent analysis. When cardiometabolic variables were entered as a set of independent variables in a binary logistic regression model (step categories collapsed to higher two versus lower two as dependent variable), the model was significant (χ2 = 17.287, df = 8, p = 0.027); weight and triglycerides were relatively strong correlates (p = 0.058 and p = 0.006, respectively), adjusting for other cardiometabolic variables. Waist circumference was not significant, as anticipated because of the high interrelationship with weight.
Table 4.
Cardiometabolic characteristics by step category
| Clinical Measures | 0–4,999 (n = 23) |
5,000-7,499 (n = 60) |
7,500–9,999 (n = 69) |
≥10,000 (n = 58) |
P value |
|---|---|---|---|---|---|
| Step category based on average # of daily steps | |||||
| Age | 44.5 | 45.7 | 44.1 | 44.8 | 0.731 |
| BMI | 34.9 | 33.3 | 32.0 | 30.7 | 0.001 |
| Weight (lb) | 191.5 | 177.7 | 172.3 | 163.3 | 0.001 |
| Waist (cm) | 104.0 | 102.9 | 100.4 | 98.4 | 0.072 |
| SBP | 117.3 | 113.1 | 115.0 | 111.8 | 0.277 |
| DBP | 78.9 | 74.9 | 75.6 | 74.3 | 0.205 |
| Total-C | 197.5 | 186.5 | 186.3 | 187.3 | 0.559 |
| LDL-C (n = 201) | 117.1 | 106.2 | 110.7 | 115.9 | 0.263 |
| HDL-C (n = 209) | 43.8 | 43.1 | 46.0 | 43.8 | 0.65 |
| TG (n = 208) | 181.5 | 186.1 | 154.1 | 141.8 | 0.027 |
| FBS | 97.7 | 102.6 | 101.2 | 97.6 | 0.46 |
Bold values indicate significant findings
Discussion
This study examined PA in relation to risk factors for CVD and MetS in Latina adults of predominantly Mexican descent living in an urban area of Southern California. Uniquely, participants were recruited at a grassroots level within the community rather than from clinics or hospitals. Their acculturation levels were low even with lengthy residence and exposure to US culture. Our findings challenge beliefs about sedentary lifestyles among Latina women. Despite overweight/obesity, only 11 % of the women were sedentary, and 28 % achieved a daily step count of 10,000 or higher. The average daily step count indicated that the women were fairly active. The women often engaged in short bouts of moderate PA rather than long-sustained moderate-to-vigorous activity. More active women generally had lower BMI, weight, waist circumference, and TG levels. Additionally, greater minutes in moderate PA were associated with higher HDL-C levels. In interpreting these findings, it is important to consider that aspects of movement reflected in step count differ from those in moderate PA, thus accounting for some of the variations in correlational findings. The absence of a relationship between PA and cardiometabolic indices such as BP and FBS may reflect the nature of the sample (i.e., predominantly normotensive and nondiabetic).
The high prevalence of MetS in our sample raises concern about the women developing T2D and CVD in later years. FBS in the range of 100–125 were evident in 86 (38.6 %) women. The most frequently observed MetS trait was large waist size. Research on correlates of MetS components in overweight/obese Latinos has shown that waist circumference is the only variable that predicts FBS, and BMI does not predict other cardiometabolic variables [52], suggesting that body weight per se is a poor predictor of metabolic health. Dyslipidemia was fairly prevalent as evidenced by low levels of HDL-C in ~70 % and elevated TG in ~46 % of the participants.
Regarding PA, in comparison to data from NHANES, the women in the present study exhibited higher daily step counts, and slightly fewer minutes in moderate activity as well as less in the sedentary category [53]. This finding about differences in step count was unexpected given the higher energy expenditure of overweight/obese women due to greater body mass and the expectation that they would modify their PA to accommodate their weight. Anecdotally, many of the women engaged in planned, purposeful PA while performing activities of daily living, such as household activities, childcare, and shopping. Furthermore, the differences we observed in BMI across varying PA categories are consistent with NHANES findings [53, 54].
Step counts were not correlated with any of the lipid markers except TG levels; however, greater minutes in moderate PA were associated with higher HDL-C and Total-C levels. The latter finding is not easily explained. In their review of studies examining the association between PA and health, Kokkinos and Meyers [19] reported the most consistent findings have been demonstrated for increases in HDL-C. Arsenault and colleagues [55] found no changes in lipid profile following a 6-month exercise intervention in metabolically healthy overweight or obese women with moderately elevated systolic BP.
Our findings suggest that the favorable health behavior of PA may at least partially contribute to the “Latino paradox.” Despite a burden of CVD risk factors similar to non-Latino whites and a higher prevalence of certain risk factors such as T2D, Latinos have lower CVD mortality [56]. Latina women have the highest life expectancy of all ethnic/racial groups at ~83 years, even in the presence of obesity [57]. Creating a physical environment believed to support PA is important in helping women to maintain high PA levels, particularly those who live in communities with limited socioeconomic resources and environmental risk factors (e.g., heavy traffic, crime, lack of park facilities, etc.). Research indicates that perceptions of neighborhood characteristics, such as the availability of PA facilities, impact residents’ levels of PA [58, 59].
Before further considering implications of our findings, we acknowledge a number of limitations. Because the sample was comprised of predominantly women of Mexican descent living in an urban setting, the findings cannot necessarily be generalized to include other US Latino subgroups or Mexican–Americans living in rural settings. In addition, the nature of the PA was not quantified (i.e., leisure-time vs. work-related), and data on daily caloric intake were not collected. Rates of T2D and hypertension were based on our clinical evaluations without medical record verification. The potential effects of antihypertensive drugs on outcomes of the small number of women being treated were not evaluated. Acculturation level and years of residence in the US were not explored as potential modifiers of PA and its correlates. Although this study yields important findings about cardiometabolic factors related to physical activity, causation can not be inferred.
Our findings point to the importance of targeting maintenance of PA in active immigrant women and intervening to promote healthier behaviors in those who are sedentary or somewhat active. Evidence-based guidelines for CVD prevention in women, developed by an American Heart Association expert panel, include regular PA as part of the healthy lifestyle behaviors ranked as Class I (highest recommendation) for CVD prevention [60]. Similarly, the JNC7 found the adoption of healthy lifestyles to be critical for the prevention of high BP and indispensable for the management of HTN [47]. The Department of Health and Human Services Physical Activity Report Guidelines also support that for otherwise healthy sedentary individuals, PA is beneficial, and performing activity ~1 h per week at moderate intensity will provide small increases in cardiorespiratory and muscular fitness [61]. Small changes, such as 5-min walking breaks from sedentary time, can yield beneficial effects on metabolic health variables [62]. Culturally tailored lifestyle interventions that build on the strengths of Latina women while helping them to overcome barriers to PA and gain support for becoming more active are urgently needed. While supporting strategies to promote higher levels of PA, health professionals should recognize that the goal of 10,000 steps or 30 min of moderate activity per day, encouraged in the media and in practice, may not be achievable by all groups. Alternatively, walking fewer steps with higher intensity strides may be considered. Daily step count recommendations vary across countries, and in fact, the US President’s Challenge on Physical Activity and Fitness Awards Program recommends 8,500 steps for adults [63]. Health professionals are encouraged to assess PA status routinely and to identify barriers and facilitators influencing this behavior. Strategies for overcoming barriers and securing needed support should be part of counseling. Family support towards PA among MA women and self-monitoring with pedometers may positively influence activity level [64, 65].
New Contribution to Literature
To our knowledge, this is the first study presenting a comprehensive analysis of accelerometer-derived indicators of PA and related cardiometabolic measures in a sample comprised solely of immigrant Latina women. Inclusion of objective measures more accurately evaluates PA than self-report, thereby strengthening the validity of our findings. Our results point to the need for comprehensive and culturally tailored lifestyle behavior programs for health promotion and disease prevention among over-weight/obese, immigrant Latina women. Such interventions have the potential for a positive impact on the health of the fastest growing ethnic minority population within our nation. Future research should examine whether the type of PA (leisure vs. work-related) influences cardiometabolic profile and other CVD risk factors. Large cross-sectional studies with diverse samples of Latina women are needed to compare differences for factors such as country of origin, urban versus rural residence, and level of acculturation. Finally, potential causality between changes in levels of PA activity and CVD benefits may be examined through longitudinal studies.
Acknowledgments
This research was supported with funds from the National Heart, Lung, and Blood Institute (R01 HL086931) and is part of a registered clinical trial (NCT01333241). We would like to acknowledge the assistance of Antronette Yancey, MD, MPH, James Sallis, Ph.D. and Christian Roberts, Ph.D. for their expert contributions on measurement of physical activity and Carmen Turner for her excellent editorial assistance with manuscript preparation. This study would not have been possible without the cooperation and contributions of the Latina women participants, community partners and research staff involved with the project.
References
- 1.Centers for Disease Control (CDC) [Accessed 19 Jun 2012];Differences in prevalence of obesity among black, white, and Hispanic adults—United States, 2006-2008. MMWR. 2009 58(27):740–4. Available at http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5827a2.htm. [PubMed] [Google Scholar]
- 2.The Office of Minority Health [Accessed 19 Jun 2012];Health status of Hispanic/Latino women. Available at http://minorityhealth.hhs.gov/templates/content.aspx?ID=3722.
- 3.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Makuc DM, Marcus GM, Marelli A, Matchar DB, Moy CS, Mozaffarian D, Mussolino ME, Nichol G, Paynter NP, Soliman EZ, Sorlie PD, Sotoodehnia N, Turan TN, Virani SS, Wong ND, Woo D. American Heart Association Statistics Committee and Stroke Statistics Sub-committee. Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation. 2012;125(1):e2–220. doi: 10.1161/CIR.0b013e31823ac046. Epub 2011 Dec 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boykin S, Diez-Roux AV, Carnethon M, Shrager S, Ni H, Whitt-Glover M. Racial/ethnic heterogeneity in the socioeconomic patterning of CVD risk factors in the United States: the multiethnic study of atherosclerosis. J Health Care Poor Underserved. 2011;22(1):111–27. doi: 10.1353/hpu.2011.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ervin RB. Prevalence of metabolic syndrome among adults 20 years of age and over, by sex, age, race and ethnicity, and body mass index: United States, 2003-2006. Natl Health Stat Rep. 2009;13:1–7. [PubMed] [Google Scholar]
- 6.Wannamethee SG, Shaper AG, Lennon L, Morris RW. Metabolic syndrome vs. Framingham risk score for prediction of coronary heart disease, stroke, and type 2 diabetes mellitus. Arch Intern Med. 2005;165(22):2644–50. doi: 10.1001/archinte.165.22.2644. [DOI] [PubMed] [Google Scholar]
- 7.Lorenzo C, Williams K, Hunt KJ, Haffner SM. Trends in the prevalence of the metabolic syndrome and its impact on cardiovascular disease incidence: the San Antonio heart study. Diabetes Care. 2006;29(3):625–30. doi: 10.2337/diacare.29.03.06.dc05-1755. [DOI] [PubMed] [Google Scholar]
- 8.Hunt KJ, Resendez RG, Williams K, Haffner SM. San Antonio heart study. National cholesterol education program versus World Health Organization metabolic syndrome in relation to all-cause and cardiovascular mortality in the San Antonio heart study. Circulation. 2004;110(10):1251–7. doi: 10.1161/01.CIR.0000140762.04598.F9. [DOI] [PubMed] [Google Scholar]
- 9.McNeill AM, Rosamond WD, Girman CJ, Golden SH, Schmidt MI, East HE, Ballantyne CM, Heiss G. The metabolic syndrome and 11-year risk of incident of cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care. 2005;28(2):385–90. doi: 10.2337/diacare.28.2.385. [DOI] [PubMed] [Google Scholar]
- 10.Nelson T, Perez A, Alcaraz J, Talavera G, McCarthy JJ. Family history of diabetes, acculturation, and the metabolic syndrome among Mexican Americans: proyecto SALSA. Metab Syndr Relat Disord. 2007;5(3):262–9. doi: 10.1089/met.2006.0035. [DOI] [PubMed] [Google Scholar]
- 11.Roberts CK, Barnard RJ. Effects of exercise and diet on chronic disease. J Appl Physiol. 2005;98(1):3–30. doi: 10.1152/japplphysiol.00852.2004. [DOI] [PubMed] [Google Scholar]
- 12.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1081–93. doi: 10.1161/CIRCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 13.Parra-Medina D, Hilfinger Messias DK. Promotion of physical activity among Mexican-origin women in Texas and South Carolina: an examination of social, cultural, economic, and environmental factors. Quest. 2011;63(1):100–17. doi: 10.1080/00336297.2011.10483668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.American Heart Association . Heart Disease and Stroke Statistics— 2010 Update. American Heart Association; Dallas, TX: [Accessed May 14 2012]. 2010. Available at: http://circ.ahajournals.org/content/121/7/e46.full.pdf. [Google Scholar]
- 15.Hu FB, Willett CW, Li T, Stampfer MJ, Colditz GA, Manson JE. Adiposity as compared with physical activity in predicting mortality among women. N Engl J Med. 2004;351(26):2694–703. doi: 10.1056/NEJMoa042135. [DOI] [PubMed] [Google Scholar]
- 16.Colberg SR, Sigal RJ, Fernhall B, Regensteiner JG, Blissmer BJ, Rubin RR, Chasan-Taber L, Albright AL, American College of Sports Medicine; American Diabetes Association Exercise and type 2 diabetes: the American College of Sports Medicine and the American Diabetes Association: joint position statement. Diabetes Care. 2010;33(12):e147–67. doi: 10.2337/dc10-9990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ilanne-Parikka P, Laaksonen DE, Eriksson JG, Lakka TA, Lindstr J, Peltonen M, Aunola S, Keinánen-Kiukaanniemi S, Uusitupa M, Finnish Diabetes Prevention Study Group Leisure-time physical activity and the metabolic syndrome in the Finnish diabetes prevention study. Diabetes Care. 2010;33(7):1610–7. doi: 10.2337/dc09-2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blair SN, Kohl HW, Barlow CE, Paffenbarger RS, Jr, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA. 1995;273(14):1093–8. [PubMed] [Google Scholar]
- 19.Kokkinos P, Myers J. Exercise and physical activity: clinical outcomes and applications. Circulation. 2010;122(16):1637–48. doi: 10.1161/CIRCULATIONAHA.110.948349. [DOI] [PubMed] [Google Scholar]
- 20.Mora S, Cook N, Buring JE, Ridker PM, Lee IM. Physical activity and reduced risk of cardiovascular events: potential mediating mechanisms. Circulation. 2007;116(19):2110–8. doi: 10.1161/CIRCULATIONAHA.107.729939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reddigan JI, Ardern CI, Riddell MC, Kuk JL. Relation of physical activity to cardiovascular disease mortality and the influence of cardiometabolic risk factors. Am J Cardiol. 2011;108(10):1426–31. doi: 10.1016/j.amjcard.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 22.Shaw KA, Gennat HC, O’Rourke P, Del Mar C. [Accessed July 8 2012];Exercise for overweight or obesity. The Cochrane Collaboration, 2009. Available at http://onlinelibrary.wiley.com/o/cochrane/clsysrev/articles/CD003817/pdf_fs.html.
- 23.Atienza AA, Moser RP, Perna F, Dodd K, Ballard-Barbash R, Troiano RP, Berrigan D. Self-reported and objectively-measured activity related to biomarkers using NHANES. Med Sci Sports Exerc. 2011;43(5):815–21. doi: 10.1249/MSS.0b013e3181fdfc32. [DOI] [PubMed] [Google Scholar]
- 24.Perez A, Fleury J, Keller C. Review of intervention studies promoting physical activity in Hispanic women. WJNR. 2009;32(3):341–62. doi: 10.1177/0193945909351300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Keller CS, Cantue A. Camina por Salud: walking in Mexican-American women. Appl Nurs Res. 2008;21(2):110–3. doi: 10.1016/j.apnr.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Avila P, Hovell MF. Physical activity training for weight loss in Latinas: a controlled trial. Int J Obes Relat Metab Disord. 1994;18(7):476–82. [PubMed] [Google Scholar]
- 27.Keller C, Trevino RP. Effects of two frequencies of walking on cardiovascular risk factor reduction in Mexican American women. RINAH. 2001;24(5):390–401. doi: 10.1002/nur.1039. [DOI] [PubMed] [Google Scholar]
- 28.Vella CA, Ontiveros D, Zubia RY, Dalleck L. Physical activity recommendations and cardiovascular disease risk factors in young Hispanic women. J Sports Sci. 2011;29(1):37–45. doi: 10.1080/02640414.2010.520727. [DOI] [PubMed] [Google Scholar]
- 29.Albright CL, Pruitt L, Castro C, Gonzalez A, Woo S, King AC. Modifying physical activity in a multiethnic sample of low-income women: one year results from IMPACT (increasing motivation for physical activity) project. Ann Behav Med. 2005;30(3):191–200. doi: 10.1207/s15324796abm3003_3. [DOI] [PubMed] [Google Scholar]
- 30.Hovell MF, Mulvihill MM, Buono MJ, Liles S, Schade DH, Washington TA. Culturally tailored aerobic exercise intervention for low-income Latinas. Am J Health Promot. 2008;22(3):155–63. doi: 10.4278/ajhp.22.3.155. [DOI] [PubMed] [Google Scholar]
- 31.Pekmezi DW, Neighbors CJ, Lee CS, Gans KM, Bock BC, Morrow KM, Marquez B, Dunsiger S, Marcus BH. A culturally adapted physical activity intervention for Latinas: a randomized controlled trial. Am J Prev Med. 2009;37(6):495–500. doi: 10.1016/j.amepre.2009.08.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pekmezi D, Marquez B, Marcus-Blank J. Health promotion in Latinos. Am J Lifestyle Med. 2010;4(2):151–65. [Google Scholar]
- 33.Prince SA, Adamo KB, Hamel ME, Hardt J, Gorber SC, Tremblay M. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Evenson KR, Buchner DM, Morland KB. Objective measurement of physical activity and sedentary behavior among US adults aged 60 years or older. Prev Chronic Dis. 2012;9:E26. Epub 2011 Dec 15. [PMC free article] [PubMed] [Google Scholar]
- 35.Cornier MA, Després JP, Davis N, Grossniklaus DA, Klein S, Lamarche B, Lopez-Jimenez F, Rao G, St-Onge MP, Towfighi A, American Heart Association Obesity Committee of the Council on Nutrition; Physical Activity and Metabolism; Council on Arteriosclerosis; Thrombosis and Vascular Biology; Council on Cardiovascular Disease in the Young; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing, Council on Epidemiology and Prevention; Council on the Kidney in Cardiovascular Disease, and Stroke Council Assessing adiposity: a scientific statement from the American Heart Association. Circulation. 2011;124(18):1996–2019. doi: 10.1161/CIR.0b013e318233bc6a. [DOI] [PubMed] [Google Scholar]
- 36.Niinomi M, TakeuchiY Nakamura R, et al. Evaluation of physical activity by using the body energy expenditure recording device with accelerometers and expanded memory (in Japanese) Jpn J Pract Diabetes. 1998;15:433–8. [Google Scholar]
- 37.Suzuki I, Kawasaki N, Shimizu H. Accuracy of calorie counter method to assess daily energy expenditure and physical activities in athletes and nonathletes. J Sports Med Phys Fit. 1997;37:131–6. [PubMed] [Google Scholar]
- 38.Furukawa F, Kazuma K, Kawa M, Miyashita M, Niiro K, Kusukawa R, Kojima M. Effects of an off-site walking program on energy expenditure, serum lipids, and glucose metabolism in middle-aged women. Biol Res Nurs. 2003;4(181):181–92. doi: 10.1177/1099800402239623. [DOI] [PubMed] [Google Scholar]
- 39.Thompson DL, Rakow J, Perdue SM. Relationship between accumulated walking and body composition in middle-aged women. Med Sci Sports Exerc. 2004;36(5):911–4. doi: 10.1249/01.mss.0000126787.14165.b3. [DOI] [PubMed] [Google Scholar]
- 40.Yokoyama Y, Kawamura T, Tamakoshi A, Noda A, Hirai M, Saito H, Ohno Y. Comparison of accelerometry and oxymetry for measuring daily physical activity. Circ J. 2002;66(8):751–4. doi: 10.1253/circj.66.751. [DOI] [PubMed] [Google Scholar]
- 41.Freedson PS, Melanson E, Sirard J. Calibration of the computer science and applications, Inc. accelerometer. Med Sci Sports Exerc. 1998;30(5):777–81. doi: 10.1097/00005768-199805000-00021. [DOI] [PubMed] [Google Scholar]
- 42.Miller GD, Jakicic JM, Rejeski WJ, Whit-Glover MC, Lang W, Walkup MP, Hodges ML. Effect of varying accelerometry criteria on physical activity: the look AHEAD study. Obesity (Silver Spring) 2012 May 4; doi: 10.1038/oby.2012.118. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Matthews CE, Ainsworth BE, Thompson RW, Bassett DR., Jr. Sources of variance in daily physical activity levels as measured by an accelerometer. Med Sci Sports Exerc. 2002;34(8):1376–81. doi: 10.1097/00005768-200208000-00021. [DOI] [PubMed] [Google Scholar]
- 44.Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37(11 Suppl):S531–43. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- 45.Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel ***) Final Report. Circulation. 2002;106(25):3143–421. [PubMed] [Google Scholar]
- 46.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC, Jr, Spertus JA. Fernando Costa. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement: executive summary. Crit Pathw Cardiol. 2005;4(4):198–203. doi: 10.1097/00132577-200512000-00018. [DOI] [PubMed] [Google Scholar]
- 47.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ, National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289(19):2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 48.NHLBI . The practical guide: identification, evaluation, and treatment of overweight and obesity in adults. NHLBI obesity education initiative. Public Health Service, National Institutes of Health; Bethesda, MD: 2000. NIH Publication No. 00-4084. [Google Scholar]
- 49.Balcázar H, Krull JL. Cancer risk reduction in Mexican American women: the role of acculturation, education, and health risk factors. Health Educ Q. 1995;22(1):61–84. doi: 10.1177/109019819502200107. [DOI] [PubMed] [Google Scholar]
- 50.Alegria M, Shrout PE, Woo M, Guarnaccia P, Sribney W, Vila D, Polo A, Cao Z, Mulveney N, Torres M, Canono G. Understanding differences in past year psychiatric disorders for Latinos living in the U.S. Soc Sci Med. 2007;65(2):214–30. doi: 10.1016/j.socscimed.2007.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ruiz RJ, Marti CN, Pickler R, Murphey C, Wommack J, Brown CE. Acculturation, depressive symptoms, estriol, progesterone, and preterm birth in Hispanic women. Arch Womens Ment Health. 2012;15(1):57–67. doi: 10.1007/s00737-012-0258-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Perry A, Wang X, Kuo YT. Anthropometric correlates of metabolic syndrome components in a diverse sample of overweight/obese women. Ethn Dis. 2008;18(2):163–8. [PubMed] [Google Scholar]
- 53.Tudor-Locke C, Brashear MM, Johnson WD, Katzmarzyk PT. Accelerometer profiles of physical activity and inactivity in normal weight, overweight, and obese U.S. men and women. Sports Med. 2004;34:1–8. doi: 10.1186/1479-5868-7-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sisson SB, Camhi SM, Tudor-Locke C, Johnson WD, Katzmarzyk PT. Characteristics of step-defined physical activity categories in U.S. adults. Am J Health Promot. 2012;26(3):152–9. doi: 10.4278/ajhp.100326-QUAN-95. [DOI] [PubMed] [Google Scholar]
- 55.Arsenault BJ, Côté M, Cartier A, Lemieux I, Després JP, Ross R, Earnest CP, Blair SN, Church TS. Effect of exercise training on cardiometabolic risk markers among sedentary, but metabolically healthy overweight or obese post-menopausal women with elevated blood pressure. Atherosclerosis. 2009;207(2):530–3. doi: 10.1016/j.atherosclerosis.2009.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mosca L, Benjamin EJ, Berra K, Bezanson JL, Dolor RJ, Lloyd-Jones DM, Newby LK, Piña IL, Roger VL, Shaw LJ, Zhao D, Beckie TM, Bushnell C, D’Armiento J, Kris-Etherton PM, Fang J, Ganiats TG, Gomes AS, Gracia CR, Haan CK, Jackson EA, Judelson DR, Kelepouris E, Lavie CJ, Moore A, Nussmeier NA, Ofili E, Oparil S, Ouyang P, Pinn VW, Sherif K, Smith SC, Jr, Sopko G, Chandra-Strobos N, Urbina EM, Vaccarino V, Wenger NK, American Heart Association Effectiveness-based guidelines for the prevention of cardiovascular disease in women-2011 update: a guideline from the American Heart Association. J Am Coll Cardiol. 2011;57(12):1404–23. doi: 10.1016/j.jacc.2011.02.005. Erratum in: J Am Coll Cardiol. 2012;59:1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Arias E. United states life tables by hispanic origin. National Center for Health Statistics; Washington, DC: 2010. [PubMed] [Google Scholar]
- 58.Duncan MJ, Spence JC, Mummery WK. Perceived environment and physical activity: a meta-analysis of selected environmental characteristics. Int J Behav Nutr Phys Act. 2005;2:11. doi: 10.1186/1479-5868-2-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Marquez DX, McAuley E. Social cognitive correlates of leisure time physical activity among Latinos. J Behav Med. 2006;29(3):281–9. doi: 10.1007/s10865-006-9055-6. [DOI] [PubMed] [Google Scholar]
- 60.Expert Panel Writing Group. Mosca L, Appel LJ, Benjamin EJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women. J Am Coll Cardiol. 2004;43(5):900–921. doi: 10.1016/j.jacc.2004.02.001. [DOI] [PubMed] [Google Scholar]
- 61.USDHHS [Accessed July 6 2012];Physical Activity Guidelines for Americans. 2008 :E–24. Available: http://www.health.gov/paguidelines/guidelines/default.aspx.
- 62.Swartz AM, Squires L, Strath SJ. Energy expenditure of interruptions to sedentary behavior. Int J Behav Nutr Phys Act. 2011;8:69. doi: 10.1186/1479-5868-8-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. [Accessed July 8 2012];The President’s Challenge. Available at http://www.presidentschallenge.org/challenge/active/index.shtmlwebsite.
- 64.Mier N, Ory MG, Medina AA. Anatomy of culturally sensitive interventions promoting nutrition and exercise in Hispanics: a critical examination of existing literature. Health Promot Pract. 2010;11(4):541–54. doi: 10.1177/1524839908328991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Kang M, Marshall SJ, Barreira TV, Lee JO. Effect of pedometer-based physical activity interventions: a meta-analysis. Res Q Exerc Sport. 2009;80(3):648–55. doi: 10.1080/02701367.2009.10599604. [DOI] [PubMed] [Google Scholar]