Abstract
Objective
To assess the influence of drug, dosing regimen, and traditional, non-traditional, and genetic risk factors on the incidence of choroidal neovascularization (CNV) in the fellow eye of patients treated for CNV with ranibizumab or bevacizumab.
Design
Cohort study of patients enrolled in a multicenter randomized clinical trial.
Participants
Patients with no CNV in the fellow eye at the time of enrollment in the Comparison of Age-related Macular Degeneration Treatments Trials (CATT).
Methods
Eligibility criteria for the clinical trial required that study eyes have evidence on fluorescein angiography and optical coherence tomography (OCT) of CNV secondary to age-related macular degeneration (AMD) and visual acuity between 20/25 and 20/320. Treatment for the study eye was assigned randomly to either ranibizumab or bevacizumab and to three different regimens for dosing over a two-year period. The genotypes for four single nucleotide polymorphisms (SNPS) associated with risk of AMD were determined. Only patients without CNV in the fellow eye at baseline were considered at risk. CATT ophthalmologists examined patients every four weeks through two years and recorded treatment for CNV in the fellow eye.
Main Outcome Measures
Development of CNV in the fellow eye.
Results
Among 1185 CATT participants, 727 (61%) had no CNV in the fellow eye at enrollment. At two years, CNV had developed in 75 (20.6%) of 365 patients treated with ranibizumab and 60 (16.6%) of 362 patients treated with bevacizumab (absolute difference 4.0%, 95% confidence interval (−1.7%, 9.6%); p=0.17). The risk ratio for pro re nata (PRN) dosing relative to monthly dosing was 1.1 (95% confidence interval (0.8, 1.6)). Greater elevation of the retinal pigment epithelium and fluid in the foveal center of the study eye were associated with increased incidence of CNV in the fellow eye. Incidence was not associated with genotype on rs1061170 (CFH), rs10490924 (ARMS2), rs11200638 (HTRA1), and rs2230199 (C3) (p > 0.35).
Conclusion
Through two years, there was no statistically significant difference between ranibizumab and bevacizumab in incidence of CNV in the fellow eye. Genotype on four SNPs previously found to be associated with AMD did not affect the risk of CNV in the fellow eye among CATT patients.
INTRODUCTION
The presence of choroidal neovascularization (CNV) in one eye of a patient with age-related macular degeneration (AMD) is an established and strong risk factor for development of CNV in the contralateral (fellow) eye.1–5 In previous large-scale studies, the annual incidence of CNV in fellow eyes has ranged from 4% to 19%.3,4,6–8 Variation in incidence rates may reflect differences in the method of identifying CNV; e.g., clinical examination versus reading center interpretation, as well as differences among patient groups with respect to risk factors such as large drusen, pigmentary abnormalities, genetic background, and intake of foods or supplements with high levels of anti-oxidant vitamins and zinc.9
Between 2005 and 2011, nearly all patients with newly diagnosed CNV secondary to AMD in the United States were treated with intravitreal injection of ranibizumab (Lucentis, Genentech) or bevacizumab (Avastin, Genentech).10,11 These drugs bind vascular endothelial growth factor (VEGF) and are derived from similar monoclonal antibodies. Results from the Comparison of AMD Treatments Trials (CATT), a multicenter randomized clinical trial of the efficacy and safety of ranibizumab and bevacizumab for the treatment of CNV secondary to AMD, showed that through two years of treatment, the drugs have equivalent effects on visual acuity and that dosing on a pro re nata (PRN) basis resulted in less gain in visual acuity (mean of 2.4 letters) than monthly dosing.12,13
However, the effects of the drugs differed in several areas. At one and two years after initiation of treatment, eyes treated with ranibizumab had less fluid on optical coherence tomography and had less retinal thickness.12,13 In addition, CATT patients treated with bevacizumab had more serious adverse events during two years than patients treated with ranibizumab (39.9% vs. 31.7%; p=0.004). In a multicenter clinical trial conducted in Great Britain with a study design similar to CATT, patients with bevacizumab had more serious adverse events within one year than those treated with ranibizumab, but not to a statistically significant degree (12.5% vs. 9.6%; p=0.25).14 In CATT, the majority of adverse events were conditions that have not been associated with VEGF inhibition in clinical trials for patients with cancer. As a consequence, the interpretation of the adverse event findings was not clear but raised the question of different systemic effects with the two drugs.
The possibility that ranibizumab and bevacizumab may have systemic effects has prompted interest in possible therapeutic effects in the fellow eye after intravitreal injection in one eye. A retrospective evaluation of the incidence of CNV in fellow eyes from two clinical trials involving sham injections or treatment with photodynamic therapy, which has no known effect on VEGF, found no evidence of a reduction in incident CNV with monthly injections of ranibizumab.7 However, there are reports of resolution of retinal neovascularization, diabetic macular edema, and uveitic cystoid macular edema in the fellow eye after unilateral intravitreal treatment with bevacizumab.15–17
The data collected on patients participating in CATT provide the opportunity to explore whether systemic effects of intravitreal injections on the incidence of CNV in the fellow eye differ between ranibizumab and bevacizumab. In addition, morphologic features of the study eye and genotypes of SNPs within genes associated with AMD may be evaluated as risk factors.
METHODS
Study Population for the Clinical Trial
Details of the design and methods for CATT have been published previously.12 Only features relevant to the evaluation of incidence of CNV in the fellow eye are noted here. Patients enrolled through 43 clinical centers in the United States between February 2008 and December 2009. Only one eye per patient, the study eye, needed to be eligible for the clinical trial and only that eye was assigned. Inclusion criteria included age ≥ 50 years, presence in the study eye of previously untreated active CNV secondary to AMD, and visual acuity between 20/25 and 20/320 in the study eye. Active CNV was considered present when both leakage on fluorescein angiography and fluid on time-domain optical coherence tomography (OCT) were documented through central review of images. Fluid on OCT could be within or beneath the retina or beneath the retinal pigment epithelium (RPE). Either neovascularization, fluid, or hemorrhage needed to be under the fovea. For the CNV to be considered secondary to AMD, at least one druse > 63 μ needed to be present in either the study eye or fellow eye, or the fellow eye needed to have CNV or geographic atrophy. The study was approved by an institutional review board associated with each center. All patients provided written informed consent.
Treatment of the Study Eye
At enrollment, patients were assigned with equal probability to one of four treatment groups defined by drug (ranibizumab or bevacizumab) and by dosing regimen (monthly or PRN). At one year, patients initially assigned to monthly treatment retained their drug assignment but were re-assigned randomly, with equal probability, to either monthly or PRN treatment. Patients initially assigned to PRN treatment had no change in assignment; i.e., they retained both their drug assignment and PRN dosing regimen for year 2.
Study Procedures
During the initial visit, patients provided a medical history and were examined by a study-certified ophthalmologist. The ophthalmologist indicated whether there was a history of CNV or active CNV in the non-study eye. Patients had bilateral color stereoscopic fundus photography and fluorescein angiography that included stereo images of the macula of the fellow eye at two and 10 minutes after dye injection. Study eyes were also imaged at the initial visit with time domain OCT. Follow-up examinations were scheduled every 28 days for two years. During each examination, the study ophthalmologist completed case report forms with specific questions regarding whether there had been any treatment for CNV in the non-study eye since the last CATT examination or whether treatment was scheduled on the day of the examination. Color fundus photography and fluorescein angiography were performed at 52 weeks and 104 weeks.
Certified graders at the CATT Fundus Photograph Reading Center and the CATT OCT Reading Center reviewed images acquired at the initial and follow-up visits. Morphologic features of the study eyes at baseline were evaluated.18,19 Graders at the Photograph Reading Center were required to indicate whether there were signs at the initial visit of CNV or scar in the fellow eye or to indicate that no determination could be made because of missing or poor quality images. The following signs were considered evidence of CNV or scar: leakage or late staining of fluorescein on angiography or fibrous tissue on color photographs.
Between July 2010 and September 2011, CATT patients were invited to provide blood samples for genetic studies. Blood samples from patients were sent to the CATT Genetics Laboratory for DNA extraction. Four single nucleotide polymorphisms (SNPs) previously associated with risk and progression of AMD were evaluated: (1) complement factor H (CFH) Y402H (rs1061170), (2) age-related maculopathy susceptibility 2 (ARMS2, also called LOC387715) A69S (rs10490924), (3) high temperature requirement factor A2 (HTRA1) (rs11200638), and (4) complement component 3 (C3) R80G (rs2230199).20,21
Definitions of Patients at Risk and Development of CNV
Patients were at risk of incident CNV if there was documentation of CNV secondary to AMD in the study eye and neither the enrolling ophthalmologist nor the reading center graders detected evidence of CNV or scar in the fellow eye. CNV in the fellow eye was considered present at the earliest follow-up visit when the examining ophthalmologist indicated that treatment for CNV in the fellow eye had occurred since the last study examination or would occur on the day of the study visit.
Statistical Analyses
Estimates of the cumulative proportion of patients developing CNV in the fellow eye were calculated by the Kaplan-Meier method and differences between treatment groups were assessed with the logrank test. The discrete time Cox proportional hazards model, with the exact method for handling ties in time of onset of CNV, was used to estimate relative hazard rates. Dosing regimen was a time-dependent covariate to accommodate the re-randomization at one year of patients assigned to monthly treatment at the time of enrollment. The proportional hazards assumption for drugs was tested by including an interaction term involving drug and log (t +4) where t is the number of weeks since baseline. The following factors were included in the models as established, traditional risk factors for developing CNV: older age, female gender, cigarette smoking, the Age-Related Eye Disease Study (AREDS) simple risk score, and not taking beta carotene, vitamin C, vitamin E, and zinc.22 Genotype was summarized as the number of risk alleles present. Statistical computations were performed with SAS 9.3 (SAS Institute, Inc., Cary, NC).
RESULTS
A total of 135 (18.6%) patients developed CNV in the fellow eye among the 727 patients who were at risk. At one year, the proportion of patients with CNV was similar among those treated with ranibizumab (7.9%) and bevacizumab (7.2%; p=0.76). At two years, 75 of 365 (20.6%) patients in the ranibizumab group and 60 of 362 (16.6%) patients in the bevacizumab treatment group had developed CNV in the fellow eye. The difference in rates was 4.0% (95% confidence interval = [−1.7%, 9.6%]; p=0.17). The Kaplan-Meier estimates of cumulative incidence show that most of the difference between drug groups occurred during year 2 (Figure 1; p=0.20). In an analysis of time to CNV with the Cox model, the hazard ratio for CNV among those treated with bevacizumab compared to those treated with ranibizumab was 0.8 (95% confidence interval (0.6, 1.2); Table 1). Adjustment for factors previously associated with incidence of CNV had little influence on the estimates. Among the factors, only female gender, higher AREDS risk score, and use of dietary supplements were associated significantly with higher incidence of CNV in the fellow eye. The hazard ratio in the multivariate model for CNV among those treated PRN compared to those treated monthly was 1.1 (95% confidence interval (0.8, 1.6)).
Figure 1.
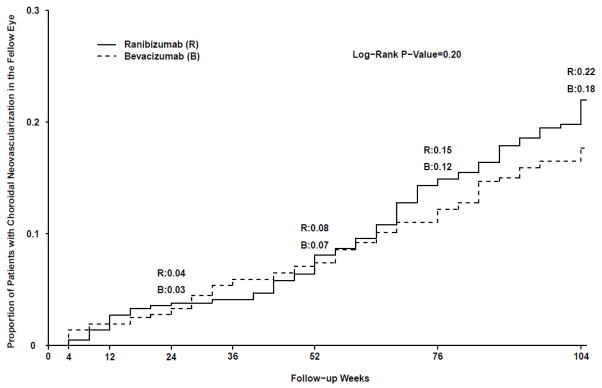
Kaplan-Meier Estimates of Cumulative Incidence of Choroidal Neovascularization in the Fellow Eye by Assigned Drug
Table 1.
Risk Factors for Incidence of Choroidal Neovascularization in the Fellow Eye from the Cox Proportional Hazards Model
| Characteristic | N | CNV n ( % ) | Model with Traditional Risk Factors Only | Model with All Risk Factors | ||
|---|---|---|---|---|---|---|
| Rate Ratio (95% CI) | P* | Rate Ratio (95% CI) | P* | |||
| Drug | ||||||
| Ranibizumab | 365 | 75 (20.6%) | 1.0 | 0.32 | 1.0 | 0.34 |
| Bevacizumab | 362 | 60 (16.6%) | 0.8 (0.6, 1.2) | 0.8 (0.6, 1.2) | ||
| Dosing regimen† | ||||||
| Monthly | 358 | 66 (18.4%) | 1.0 | 0.61 | 1.0 | 0.62 |
| PRN | 369 | 69 (18.7%) | 1.1 (0.8, 1.6) | 1.1 (0.8, 1.6) | ||
| Ag1e, years | ||||||
| 50–69 | 96 | 14 (14.6%) | 1.0 | 0.29 | 1.0 | 0.39 |
| 70–79 | 268 | 49 (18.3%) | 1.4 (0.7, 2.5) | 1.2 (0.7, 2.3) | ||
| 80–89 | 323 | 64 (19.8%) | 1.5 (0.8, 2.7) | 1.3 (0.7, 2.4) | ||
| >=90 | 40 | 8 (20.0%) | 1.4 (0.6, 3.8) | 1.4 (0.6, 3.3) | ||
| Gender | ||||||
| Female | 446 | 98 (22.0%) | 1.0 | 0.01 | 1.0 | 0.03 |
| Male | 281 | 37 (13.2%) | 0.6 (0.4, 0.9) | 0.6 (0.4, 0.95) | ||
| Cigarette smoking | ||||||
| Never | 297 | 56 (18.9%) | 1.0 | 0.44 | 1.0 | 0.32 |
| Quit | 369 | 67 (18.2%) | 1.3 (0.9, 1.8) | 1.2 (0.9, 1.8) | ||
| Current | 61 | 12 (19.7%) | 1.3 (0.7, 2.6) | 1.6 (0.8, 3.0) | ||
| Definite hypertension | ||||||
| Normal | 166 | 28 (16.9%) | 1.0 | 0.62 | 1.0 | 0.61 |
| Suspect | 58 | 12 (20.7%) | 1.4 (0.7, 2.8) | 1.4 (0.7, 2.8) | ||
| Definite | 503 | 95 (18.9%) | 1.1 (0.7, 1.6) | 1.2 (0.7, 1.8) | ||
| AREDS risk score | ||||||
| 0 | 37 | 2 ( 5.4%) | 1.0 | 0.004 | 1.0 | 0.01 |
| 1 | 111 | 12 (10.8%) | 2.0 (0.4, 8.9) | 1.9 (0.4, 8.6) | ||
| 2 | 552 | 117 (21.2%) | 3.9 (1.0, 15.8) | 3.6 (0.9, 14.5) | ||
| Dietary supplements | ||||||
| None | 70 | 6 ( 8.6%) | 1.0 | 0.02 | 1.0 | 0.01 |
| Anti-oxidants** and zinc | 464 | 81 (17.5%) | 1.7 (0.7, 4.0) | 1.7 (0.7, 4.0) | ||
| Other supplements | 193 | 48 (24.9%) | 2.6 (1.1, 6.0) | 2.8 (1.2, 6.6) | ||
| Fluid in foveal center | ||||||
| No | 136 | 14 (10.3%) | --- | --- | 1.0 | 0.03 |
| Yes | 590 | 121 (20.5%) | --- | 1.9 (1.1, 3.3) | ||
| RPE elevation, mm | ||||||
| <=3.0 | 215 | 27 (12.6%) | --- | --- | 1.0 | 0.01 |
| >3.0 to ≤5.0 | 138 | 23 (16.7%) | --- | 1.2 (0.7, 2.0) | ||
| >5.0 to ≤11.5 | 175 | 38 (21.7%) | --- | 1.4 (0.9, 2.4) | ||
| >11.5 | 175 | 45 (25.7%) | --- | 1.8 (1.1, 3.0) | ||
N and percentage based on the original dosing assignment; hazard ratio, confidence interval and p value based on dosing regimen as a time-dependent covariate in the model.
P value for test of linear trend for age, AREDS risk score, and RPE elevation.
Anti-oxidants: beta carotene, vitamin C, and vitamin E.
CNV = choroidal neovascularization; CI=confidence interval; PRN= pro re nata; AREDS= Age-Related Eye Disease Study; RPE = retinal pigment epithelium
Morphologic characteristics of the study eye at the initial visit, as captured on color fundus photography, fluorescein angiography, and OCT, were evaluated as risk factors for development of CNV in the fellow eye. The characteristics evaluated included area of CNV, area of the CNV lesion, subfoveal CNV, angiographic type of CNV (occult, classic, both), CNV lesion composition, presence of retinal angiomatous proliferation, area of hemorrhage associated with the CNV lesion, geographic atrophy in the study eye, retinal thickness, subretinal thickness, sub-RPE thickness, presence of intraretinal fluid, presence of subretinal fluid, sub-RPE fluid, presence of fluid in the foveal center on OCT, maximum height of RPE elevation, and presences of subretinal hyper-reflective material. Among these only the presence of fluid in the fovea and greater height of RPE elevation were associated with increased risk of CNV in the fellow eye after adjustment for other known risk factors (Table 1, last two columns).
The association between development of CNV and genotype for four SNPs previously associated with risk and progression of AMD was evaluated within the 518 patients who had genotyping (Table 2). Overall, the proportion of patients developing CNV in the fellow eye did not decrease with a lower number of risk alleles. Adjusting for the age, gender, and smoking habits of patient did not alter the results.
Table 2.
The Association of Choroidal Neovascularization in Fellow Eye with Genotype for Four Single Nucleotide Polymorphisms Associated with Age-related Macular Degeneration
| Single Nucleotide Polymorphism | Genotype* | N (518) | Choroidal Neovascularization n (%) | Survival Analysis
|
|
|---|---|---|---|---|---|
| Unadjusted Rate Ratio (95% CI)† | Adjusted Rate Ratio(95% CI)‡ | ||||
| CFH (rs1061170) | CC | 174 | 28 (16.1%) | 1.0 | 1.0 |
| TC | 246 | 57 (23.2%) | 1.5 (1.0, 2.4) | 1.4 (0.9, 2.2) | |
| TT | 98 | 19 (19.4%) | 1.2 (0.7, 2.2) | 1.2 (0.7, 2.1) | |
| P | 0.36 | 0.48 | |||
|
| |||||
| ARMS2 (rs10490924) | TT | 99 | 21 (21.2%) | 1.0 | 1.0 |
| GT | 249 | 50 (20.1%) | 0.9 (0.6, 1.5) | 0.9 (0.6, 1.6) | |
| GG | 170 | 33 (19.4%) | 0.9 (0.5, 1.5) | 0.8 (0.5, 1.4) | |
| P | 0.64 | 0.48 | |||
|
| |||||
| HTRA1 (rs11200638) | AA | 95 | 21 (22.1%) | 1.0 | 1.0 |
| AG | 245 | 49 (20.0%) | 0.9 (0.5, 1.5) | 0.9 (0.5, 1.5) | |
| GG | 178 | 34 (19.1%) | 0.8 (0.5, 1.4) | 0.8 (0.4, 1.4) | |
| P | 0.51 | 0.38 | |||
|
| |||||
| C3 (rs2230199) | GG | 41 | 7 (17.1%) | 1.0 | 1.0 |
| CG | 188 | 36 (19.2%) | 1.1 (0.5, 2.5) | 1.0 (0.4, 2.2) | |
| CC | 289 | 61 (21.1%) 1.2 (0.6, 2.7) 1.0 (0.4, 2.2) | |||
| P | 0.49 | 0.91 | |||
|
| |||||
| Number of Risk Alleles | 0–1 | 79 | 15 (19.0%) | 1.0 | 1.0 |
| 2 | 84 | 20 (23.8%) | 1.3 (0.7, 2.5) | 1.4 (0.7, 2.7) | |
| 3 | 113 | 21 (18.6%) | 1.0 (0.5, 1.9) | 1.1 (0.6, 2.1) | |
| 4 | 104 | 20 (19.2%) | 1.0 (0.5, 2.0) | 1.1 (0.6, 2.2) | |
| >=5 | 138 | 28 (20.3%) | 1.1 (0.6, 2.1) | 1.3 (0.7, 2.5) | |
| P | 0.86 | 0.74 | |||
The risk alleles are C for CFH, T for ARMS2, A for HTRA1, G for C3.
Cox model with genotype coded according to the number of risk alleles.
Cox model adjusted for age, gender and smoking status.
CI=confidence interval
DISCUSSION
The overall incidence of CNV in the fellow eye among CATT patients was approximately 10% per year, comparable to the rates observed in large scale studies relying on central interpretation of photographs for identifying CNV.2–6 Comparison of the 2-year incidence of CNV in fellow eyes of CATT patients treated unilaterally with either ranibizumab or bevacizumab did not reveal a statistically significant difference between drugs. At one year, the rates for ranibizumab (7.9%) and bevacizumab (7.2%) were virtually identical. By two years, the rate for ranibizumab (20.6%) was numerically higher than for bevacizumab (16.6%), but not to a statistically significant degree (4.0% absolute difference, 95% confidence interval (−1.7%, 9.6%)). Nonetheless, the difference is intriguing because of reports of higher systemic VEGF suppression by bevacizumab than ranibizumab and the plausibility of a lag-time between the initiation of therapy and an effect on clinically apparent neovascularization.14,23–25
Several findings from other studies support the plausibility that intravitreal bevacizumab may have an effect in the fellow eye that is different from that of ranibizumab.23,24 In animals, bevacizumab has a longer half-life in the vitreous and only bevacizumab has been found in fellow eyes of animals receiving unilateral injections.23,24,26–32 Once the drugs reach the bloodstream, there is a sizable difference between the serum elimination half-lives of ranibizumab (about 2 hours) and bevacizumab (20 days).33 In humans, serum VEGF levels are reduced after intravitreal injections of bevacizumab in patients with proliferative diabetic retinopathy, retinopathy of prematurity, and neovascular AMD.34–38 In a comparative study of 62 patients, the plasma level of VEGF among those treated for neovascular AMD with three consecutive monthly injections decreased in patients treated with bevacizumab but not in patients treated with ranibizumab.25 In the “alternative treatments to Inhibit VEGF in Age-related choroidal Neovascularization” (IVAN), a randomized clinical trial of 610 patients, serum levels of VEGF were reduced with both ranibizumab and bevacizumab after one year of treatment; however, the levels in patients treated with bevacizumab were approximately half those in patients treated with ranibizumab AND.14
Among the traditional risk factors evaluated, the strongest gradient in risk was seen with the AREDS risk score based on large drusen and pigmentary abnormalities (Table 1). Females had higher risk than males; female gender has been an inconsistent risk factor for CNV in previous studies. 20 Although the risk ratios for developing CNV increased with age and current smoking, these factors were not statistically significant within this group of patients with unilateral CNV at baseline. The range of risk within CATT is restricted because there are no low-risk eyes. The constrained differences in risk between groups and the relatively small proportion of eyes that developed CNV limit the power to detect statistically significant effects of traditional, as well as non-traditional, risk factors. Both patients who took beta carotene, vitamin C, vitamin E, and zinc in some amount and patients who used other dietary supplements had higher rates of CNV. This finding appears contradictory to the results of AREDS in which patients randomly assigned to these anti-oxidant vitamins and zinc had decreased risk of developing late AMD.9 Patients who choose to take these supplements may have worse health or other factors that both increase their risk of developing CNV in the fellow eye and increase the likelihood that they take supplements.
Two morphologic features of the study eye at baseline were identified as risk factors from among 17 features evaluated. Eyes with greater RPE elevation or fluid in the foveal center on OCT had higher rates of CNV in the fellow eye. Replication of these findings is required before these two features can be established as true risk factors.
Patients within CATT with more risk alleles for each of four SNPs associated with increased risk of AMD (CFH, ARMS2, HTRA1, and C3) did not have increased risk of developing CNV in the fellow eye. Findings from a recent report involving 207 Japanese patients showed a strong association of incidence of CNV in the fellow eye with ARMS2 A69S.39 Patients with a TT genotype had a much higher risk than those with a GG genotype (rate ratio 2.7; 95% confidence interval (1.4, 5.5)). Approximately 60% of the CNV in the study group was polypoidal choroidal vasculopathy, a form of neovascular macular degeneration much more common in Asian populations than other racial groups. The results from a study of 108 patients from the Netherlands did not find an association between genotype for CFH, ARMS2, or C3 and risk of CNV In the fellow eye.40 In CATT, the confidence intervals for the rate ratios comparing those with no risk alleles to those with two risk alleles included 0.5 (approximately a halving of risk), as well as 2.0 (approximately a doubling of risk). It is possible that one or more of the SNPs evaluated may have a clinically meaningful impact on risk of fellow eye involvement that was not detected with the CATT data.
The strengths of this investigation include being able to exclude fellow eyes identified by the examining ophthalmologist or the reading center graders as already having CNV at baseline, having close monitoring of the fellow eye through monthly examination of patients, and having accurate information on several important risk factors for CNV. One weakness of this study is that there were no untreated patients for comparison. Another weakness is the limited precision in estimating risk provided by CATT’s sample size. The confidence intervals show that large differences in risk between drugs, risk factor levels, or genotypes are unlikely, but that modest increases or decreases in risk may truly exist.
Analysis of the data on incidence of CNV in the fellow eye of CATT patients through two years did not identify a differential effect of ranibizumab and bevacizumab or effects of genotype on four previously identified risk alleles. The components of the AREDS simple scale, large drusen and pigmentary abnormalities, were again shown to be strong predictors of risk and are easily available to ophthalmologists when discussing prognosis with patients having one eye with CNV.
Supplementary Material
Acknowledgments
Dr. Avery is a member of the scientific advisory board for Replenish; is a consultant for Alcon, Allergan, Genentech, Novartis, Ophthotech, Replenish, QLT, and Regeneron; receives grant funding from Allergan, Genentech, Ophthotech, Novartis, and Regeneron, receives payment for lectures from Alcon, Genentech, and Novartis; has a patent with and receives royalties from Replenish, and owns stock in Alcon, Novartis, Replenish, Regeneron, and Alexion. Dr. Bakri is a consultant to Allergan, Genentech, and Regeneron; and receives grant funding from Genentech and Regeneron. Dr. Castellarin receives grant funding and payment for lectures from Genentech. Dr. Roth is a consultant for Allergan, Regeneron, and Genentech; receives payment for lectures from Allergan; Genentech, and Regeneron; owns stock in Forsight Labs; and receives payment for travel from Allergan.
Supported by cooperative agreements U10 EY017823, U10 EY017825, U10 EY017826, and U10 EY017828 from the National Eye Institute, National Institutes of Health, Department of Health and Human Services.
APPENDIX 1. Credit Roster for the Comparison of AMD Treatments Trials
Clinical Centers (Ordered by Number of Patients Enrolled)
Certified Roles at Clinical Centers
Clinic Coordinator (CC), Data Entry Staff (DE), Participating Ophthalmologist (O), Ophthalmic Photographer (OP); Optical Coherent Tomography Technician (OCT), Principal Investigator (PI), Refractionist (R), Visual Acuity Examiner (VA)
VitreoRetinal Surgery, PA (Edina, MN)
David F. Williams, MD (PI); Sara Beardsley, COA (VA/R); Steven Bennett, MD (O); Herbert Cantrill, MD (O); Carmen Chan-Tram, COA (VA/R); Holly Cheshier, CRA, COT, OCTC (OP); Kathyrn Damato, COT (VA); John Davies, MD (O); Sundeep Dev, MD (O); Julianne Enloe, CCRP, COA (CC); Gennaro Follano (OP/OCT); Peggy Gilbert, COA (VA/R); Jill Johnson, MD (O); Tori Jones, COA (OCT); Lisa Mayleben, COMT (CC/VA/R/OCT); Robert Mittra, MD (O); Martha Moos, COMT, OSA (VA/R); Ryan Neist, COMT (VA/R); Neal Oestreich, COT (CC); Polly Quiram, MD (O); Robert Ramsay, MD (O); Edwin Ryan, MD (O); Stephanie Schindeldecker, OA (VA/R); John Snater, COA (VA); Trenise Steele, COA (VA); Dwight Selders, COA (VA/R); Jessica Tonsfeldt, AO (OP/OCT); Shelly Valardi, COT (VA/R).
Texas Retina Associates (Dallas, TX)
Gary Edd Fish, MD (PI); Hank A. Aguado, CRA (OP/OCT); Sally Arceneaux (CC/VA/R); Jean Arnwine (CC); Kim Bell, COA (VA/R); Tina Bell (CC/OCT); Bob Boleman (OP); Patricia Bradley, COT (CC); David Callanan, MD (O); Lori Coors, MD (O); Jodi Creighton, COA (VA/R); Timothy Crew, COA (OCT); Kimberly Cummings (OP/OCT); Christopher Dock (OCT); Karen Duignan, COT (VA/R); Dwain Fuller, MD (O); Keith Gray (OP/OCT); Betsy Hendrix, COT, ROUB (OCT); Nicholas Hesse (OCT); Diana Jaramillo, COA (OCT); Bradley Jost, MD (O); Sandy Lash (VA/R); Laura Lonsdale, CCRP (DE); Michael Mackens (OP/OCT); Karin Mutz, COA (CC); Michael Potts (VA/R); Brenda Sanchez (VA/R); William Snyder, MD (O); Wayne Solley, MD (O); Carrie Tarter (VA/R); Robert Wang, MD (O); Patrick Williams, MD (O).
Southeastern Retina Associates (Knoxville, TN)
Stephen L. Perkins, MD (PI); Nicholas Anderson, MD (O); Ann Arnold, COT (VA/R); Paul Blais (OP/OCT); Joseph Googe, MD (O); Tina T. Higdon, (CC); Cecile Hunt (VA/R); Mary Johnson, COA (VA/R); James Miller, MD (O); Misty Moore (VA/R); Charity K. Morris, RN (CC); Christopher Morris (OP/OCT); Sarah Oelrich, COT (OP/OCT); Kristina Oliver, COA (VA/R); Vicky Seitz, COT (VA/R); Jerry Whetstone (OP/OCT).
Retina Vitreous Consultants (Pittsburgh, PA)
Bernard H. Doft (PI); Jay Bedel, RN, (CC); Robert Bergren, MD (O); Ann Borthwick (VA/R); Paul Conrad, MD, PHD (O); Amanda Fec (OCT); Christina Fulwylie (VA/R); Willia Ingram (DE); Shawnique Latham (VA/R); Gina Lester (VA/R); Judy Liu, MD (O); Louis Lobes, MD (O); Nicole M. Lucko, (CC); Holly Mechling (CC); Lori Merlotti, MS, CCRC (CC); Keith McBroom (OCT); Karl Olsen, MD (O); Danielle Puskas, COA (VA/R); Pamela Rath, MD (O); Maria Schmucker (CC); Lynn Schueckler (OCT); Christina Schultz (CC/VA/R); Heather Shultz (OP/OCT); David Steinberg, CRA (OP/OCT); Avni Vyas, MD (O); Kim Whale (VA/R); Kimberly Yeckel, COA, COT (VA/R).
Ingalls Memorial Hospital/Illinois Retina Associates (Harvey, IL)
David H. Orth, MD (PI); Linda S. Arredondo, RN (CC/VA); Susan Brown (VA/R); Barbara J. Ciscato (CC/VA); Joseph M. Civantos, MD (O); Celeste Figliulo (VA/R); Sohail Hasan, MD (O); Belinda Kosinski, COA (VA/R); Dan Muir (OP/OCT); Kiersten Nelson (OP/OCT); Kirk Packo, MD (O); John S. Pollack, MD (O); Kourous Rezaei, MD (O); Gina Shelton (VA); Shannya Townsend-Patrick (OP/OCT); Marian Walsh, CRA (OP/OCT).
West Coast Retina Medical Group, Inc. (San Francisco, CA)
H. Richard McDonald, MD (PI); Nina Ansari (VA/R/OCT); Amanda Bye, (OP/OCT); Arthur D. Fu, MD (O); Sean Grout (OP/OCT); Chad Indermill (OCT); Robert N. Johnson, MD (O); J. Michael Jumper, MD (O); Silvia Linares (VA/R); Brandon J. Lujan, MD (O); Ames Munden (OP/OCT); Meredith Persons (CC); Rosa Rodriguez (CC); Jennifer M. Rose (CC); Brandi Teske, COA (VA/R); Yesmin Urias (OCT); Stephen Young (OP/OCT).
Retina Northwest, P.C. (Portland, OR)
Richard F. Dreyer, MD (PI); Howard Daniel (OP/OCT); Michele Connaughton, CRA (OP/OCT); Irvin Handelman, MD (O); Stephen Hobbs (VA/R/OCT); Christine Hoerner (OP/OCT); Dawn Hudson (VA/R/OCT); Marcia Kopfer, COT (CC/VA/R/OCT); Michael Lee, MD (O); Craig Lemley, MD (O); Joe Logan, COA (OP/OCT); Colin Ma, MD (O); Christophe Mallet (VA/R); Amanda Milliron (VA/R); Mark Peters, MD (O); Harry Wohlsein, COA (OP).
Retinal Consultants Medical Group, Inc. (Sacramento, CA)
Joel A. Pearlman, MD, PHD (PI); Margo Andrews (OP/OCT); Melissa Bartlett (OCT); Nanette Carlson (CC/OCT); Emily Cox (VA/R); Robert Equi, MD (O); Marta Gonzalez (VA/R/OCT); Sophia Griffin (OP/OCT); Fran Hogue (VA/R); Lance Kennedy (OP/OCT); Lana Kryuchkov (OCT); Carmen Lopez (VA/R); Danny Lopez (OP/OCT); Bertha Luevano (VA/R); Erin McKenna, (CC); Arun Patel, MD (O); Brian Reed, MD (O); Nyla Secor (CC/OCT); Iris R. Sison (CC); Tony Tsai, MD (O); Nina Varghis, (CC); Brooke Waller (OCT); Robert Wendel, MD (O); Reina Yebra (OCT).
Retina Vitreous Center, PA (New Brunswick, NJ)
Daniel B. Roth, MD (PI); Jane Deinzer, RN (CC/VA/R); Howard Fine, MD MHSC (O); Flory Green (VA/R); Stuart Green, MD (O); Bruce Keyser, MD (O); Steven Leff, MD (O); Amy Leviton (VA/R); Amy Martir (OCT); Kristin Mosenthine (VA/R/OCT); Starr Muscle, RN (CC); Linda Okoren (VA/R); Sandy Parker (VA/R); Jonathan Prenner, MD (O); Nancy Price (CC); Deana Rogers (OP/OCT); Linda Rosas (OP/OCT); Alex Schlosser (OP/OCT); Loretta Studenko (DE); Thea Tantum (CC); Harold Wheatley, MD (O).
Vision Research Foundation/Associated Retinal Consultants, P.C. (Royal Oak, MI)
Michael T. Trese, MD (PI); Thomas Aaberg, MD (O); Tina Bell (VA/R/OP/OCT); Denis Bezaire, CRA (OP/OCT); Craig Bridges, CRA (OP/OCT); Doug Bryant, CRA (OP/OCT); Antonio Capone, MD (O); Michelle Coleman, RN (CC); Christina Consolo, CRA, COT (OP/OCT); Cindy Cook, RN (CC); Candice DuLong (VA/R); Bruce Garretson, MD (O); Tracy Grooten (VA/R); Julie Hammersley, RN (CC); Tarek Hassan, MD (O); Heather Jessick (OP/OCT); Nanette Jones (VA/R/OP/OCT); Crystal Kinsman (VA/R); Jennifer Krumlauf (VA/R); Sandy Lewis, COT (VA/R/OP/OCT); Heather Locke (VA/R); Alan Margherio, MD (O); Debra Markus, COT (CC/VA/R/OP/OCT); Tanya Marsh, COA (OP/OCT); Serena Neal (CC); Amy Noffke, MD (O); Kean Oh, MD (O); Clarence Pence (OP/OCT); Lisa Preston (VA/R); Paul Raphaelian, MD (O); Virginia R. Regan, RN, CCRP (VA/R); Peter Roberts (OP/OCT); Alan Ruby, MD (O); Ramin Sarrafizadeh, MD, PHD (O); Marissa Scherf (OP/OCT); Sarita Scott (VA/R); Scott Sneed, MD (O); Lisa Staples (CC); Brad Terry (VA/R/OP/OCT); Matthew T. Trese (OCT); Joan Videtich, RN (VA/R); George Williams, MD (O); Mary Zajechowski, COT, CCRC (CC/VA/R).
Barnes Retina Institute (St. Louis, MO)
Daniel P. Joseph, MD (PI); Kevin Blinder, MD (O); Lynda Boyd, COT (VA/R); Sarah Buckley (OP/OCT); Meaghan Crow (VA/R); Amanda Dinatale, (OCT); Nicholas Engelbrecht, MD (O); Bridget Forke (OP/OCT); Dana Gabel (OP/OCT); Gilbert Grand, MD (O); Jennifer Grillion-Cerone (VA/R); Nancy Holekamp, MD (O); Charlotte Kelly, COA (VA/R); Ginny Nobel, COT (CC); Kelly Pepple (VA/R); Matt Raeber, (OP/OCT); P. Kumar Rao, MD (O); Tammy Ressel, COT (VA/R); Steven Schremp (OCT); Merrilee Sgorlon (VA/R); Shantia Shears, MA (CC); Matthew Thomas, MD (O); Cathy Timma (VA/R); Annette Vaughn,(OP/OCT); Carolyn Walters, COT (CC/VA/R); Rhonda Weeks, CRC (CC/VA/R); Jarrod Wehmeier (OP/OCT); Tim Wright (OCT).
The Retina Group of Washington (Chevy Chase, MD)
Daniel M. Berinstein, MD (PI); Aida Ayyad (VA/R); Mohammed K. Barazi, MD (O); Erica Bickhart (CC/VA/R); Tracey Brady (OCT); Lisa Byank, MA (CC); Alysia Cronise, COA (VA/R); Vanessa Denny (VA/R); Courtney Dunn (VA/R); Michael Flory (OP/OCT); Robert Frantz (OP/OCT); Richard A. Garfinkel, MD (O); William Gilbert, MD (O); Michael M. Lai, MD, PHD (O); Alexander Melamud, MD (O); Janine Newgen (VA/R); Shamekia Newton (CC); Debbie Oliver (CC); Michael Osman, MD (O); Reginald Sanders, MD (O); Manfred von Fricken, MD (O).
Retinal Consultants of Arizona (Phoenix, AZ)
Pravin Dugel, MD (PI); Sandra Arenas (CC); Gabe Balea (OCT); Dayna Bartoli (OP/OCT); John Bucci (OP/OCT); Jennifer A. Cornelius (CC); Scheleen Dickens, (CC); Don Doherty (OP/OCT); Heather Dunlap, COA (VA/R); David Goldenberg, MD (O); Karim Jamal, MD (O); Norma Jimenez (OP/OCT); Nicole Kavanagh (VA/R); Derek Kunimoto, MD (O); John Martin (OP/OCT); Jessica Miner, RN (VA/R); Sarah Mobley, CCRC (CC/VA/R); Donald Park, MD (O); Edward Quinlan, MD (O); Jack Sipperley, MD (O); Carol Slagle (R); Danielle Smith (OP/OCT); Miguelina Yafchak (OCT); Rohana Yager, COA (OP/OCT).
Casey Eye Institute (Portland, OR)
Christina J. Flaxel, MD (PI); Steven Bailey, MD (O); Peter Francis, MD, PHD (O); Chris Howell, (OCT); Thomas Hwang, MD (O); Shirley Ira, COT (VA/R); Michael Klein, MD (O); Andreas Lauer, MD (O); Teresa Liesegang, COT (CC/VA/R); Ann Lundquist, (CC/VA/R); Sarah Nolte (DE); Susan K. Nolte (VA/R); Scott Pickell (OP/OCT); Susan Pope, COT (VA/R); Joseph Rossi (OP/OCT); Mitchell Schain (VA/R); Peter Steinkamp, MS (OP/OCT); Maureen D. Toomey (CC/VA/R); Debora Vahrenwald, COT (VA/R); Kelly West (OP/OCT).
Emory Eye Center (Atlanta, GA)
Baker Hubbard, MD (PI); Stacey Andelman, MMSC, COMT (CC/VA/R); Chris Bergstrom, MD (O); Judy Brower, COMT (CC/VA/R); Blaine Cribbs, MD (O); Linda Curtis (VA/R); Jannah Dobbs (OP/OCT); Lindreth DuBois, MED, MMSC, CO, COMT (CC/VA/R); Jessica Gaultney (OCT); Deborah Gibbs, COMT, CCRC (VA/R); Debora Jordan, CRA (OP/OCT); Donna Leef, MMSC, COMT (VA/R); Daniel F. Martin, MD (O); Robert Myles, CRA (OP); Timothy Olsen, MD (O); Bryan Schwent, MD (O); Sunil Srivastava, MD (O); Rhonda Waldron, MMSC, COMT, CRA, RDMS (OCT).
Charlotte Eye, Ear, Nose & Throat Associates/Southeast Clinical Research (Charlotte, NC)
Andrew N. Antoszyk, MD (PI); Uma Balasubramaniam, COA (OCT); Danielle Brooks, CCRP (VA/R); Justin Brown, MD (O); David Browning, MD, PHD (O); Loraine Clark, COA (OP/OCT); Sarah Ennis, CCRC (VA/R); Susannah Held (OCT); Jennifer V. Helms, CCRC,(CC); Jenna Herby, CCRC (CC); Angie Karow, CCRP (VA/R); Pearl Leotaud, CRA (OP/OCT); Caterina Massimino (OCT); Donna McClain, COA (OP/OCT); Michael McOwen, CRA (OP/OCT); Jennifer Mindel, CRA, COA (OP/OCT); Candace Pereira, CRC (CC); Rachel Pierce, COA (VA/R); Michele Powers (OP/OCT); Angela Price, MPH, CCRC (CC); Jason Rohrer (CC); Jason Sanders, MD (O).
California Retina Consultants (Santa Barbara, CA)
Robert L. Avery, MD (PI); Kelly Avery (VA/R); Jessica Basefsky (CC/OCT); Liz Beckner (OP); Alessandro Castellarin, MD (O); Stephen Couvillion, MD (O); Jack Giust (CC/OCT); Matthew Giust (OP); Maan Nasir, MD (O); Dante Pieramici, MD (O); Melvin Rabena (VA/R); Sarah Risard (VA/R/OCT/DE); Robert See, MD (O); Jerry Smith (VA/R); Lisha Wan (VA/R).
Mayo Clinic (Rochester, MN)
Sophie J. Bakri, MD (PI); Nakhleh Abu-Yaghi, MD (O); Andrew Barkmeier, MD (O); Karin Berg, COA (VA/R); Jean Burrington, COA (VA/R); Albert Edwards, MD (O); Shannon Goddard, COA (OP/OCT); Shannon Howard (VA/R); Raymond Iezzi, MD (O); Denise Lewison, COA (OP/OCT); Thomas Link, CRA (OP/OCT); Colin A. McCannel, MD (O); Joan Overend (VA/R); John Pach, MD (O); Margaret Ruszczyk, CCRP (CC); Ryan Shultz, MD (O); Cindy Stephan, COT (VA/R); Diane Vogen (CC).
Dean A. McGee Eye Institute (Oklahoma City, OK)
Reagan H. Bradford Jr, MD (PI); Vanessa Bergman, COA, CCRC (CC); Russ Burris (OP/OCT); Amanda Butt, CRA (OP/OCT); Beth Daniels, COA (CC); Connie Dwiggins, CCRC (CC); Stephen Fransen, MD (O); Tiffany Guerrero (CC/DE); Darin Haivala, MD (O); Amy Harris (CC); Sonny Icks (CC/DE); Ronald Kingsley, MD (O); Lena Redden (VA/R); Rob Richmond (OP/OCT); Brittany Ross (VA/R); Kammerin White, CCRC (VA/R); Misty Youngberg, COA, CCRC (VA/R).
Ophthalmic Consultants of Boston (Boston, MA)
Trexler M. Topping, MD (PI); Steve Bennett (OCT); Sandy Chong (VA/R); Mary Ciotti, COA (CC); Tina Cleary, MD (O); Emily Corey (VA/R); Dennis Donovan (OP/OCT); Albert Frederick, MD (O); Lesley Freese (CC/VA/R); Margaret Graham (OP/OCT); Natalya Gud, COA (VA/R); Taneika Howard (VA/R); Mike Jones (OP/OCT); Michael Morley, MD (O); Katie Moses (VA/R); Jen Stone (VA/R); Robin Ty, COA (VA/R); Torsten Wiegand, PHD, MD (O); Lindsey Williams (CC); Beth Winder (CC).
Tennessee Retina, P.C. (Nashville, TN)
Carl C. Awh, MD (PI); Michelle Amonette (OCT); Everton Arrindell, MD (O); Dena Beck (OCT); Brandon Busbee, MD (O); Amy Dilback (OP/OCT); Sara Downs (VA/R); Allison Guidry, COA (VA/R); Gary Gutow, MD (O); Jackey Hardin (VA/R); Sarah Hines, COA (CC); Emily Hutchins (VA/R); Kim LaCivita, MA (OP/OCT); Ashley Lester (OP/OCT); Larry Malott (OP/OCT); MaryAnn McCain, RN, CNOR (CC); Jayme Miracle (VA/R); Kenneth Moffat, MD (O); Lacy Palazzotta (VA/R); Kelly Robinson, COA (VA/R); Peter Sonkin, MD (O); Alecia Travis (OP/OCT); Roy Trent Wallace, MD (O); Kelly J. Winters, COA (CC); Julia Wray (OP/OCT).
Retina Associates Southwest, P.C. (Tucson, AZ)
April E. Harris, MD (PI); Mari Bunnell (OCT); Katrina Crooks (VA/R); Rebecca Fitzgerald, CCRC (CC/OCT); Cameron Javid, MD (O); Corin Kew (VA/R); Erica Kill, VAE (VA/R); Patricia Kline (VA/R); Janet Kreienkamp (VA/R); Maricruz Martinez (CC/OCT); Roy Ann Moore, OMA (CC/OCT); Egbert Saavedra, MD (O); LuAnne Taylor, CSC (CC/OCT); Mark Walsh, MD (O); Larry Wilson (OP).
Midwest Eye Institute (Indianapolis, IN)
Thomas A. Ciulla, MD (PI); Ellen Coyle, COMT (VA/R); Tonya Harrington, COA (VA/R); Charlotte Harris, COA (VA/OCT); Cindi Hood (OCT); Ingrid Kerr, COA (VA/R); Raj Maturi, MD (O); Dawn Moore (OCT); Stephanie Morrow, COA (OP); Jennifer Savage, COA (VA); Bethany Sink, COA (CC/VA/R); Tom Steele, CRA (OP); Neelam Thukral, CCRC (CC/OCT); Janet Wilburn, COA (CC).
National Ophthalmic Research Institute (Fort Myers, FL)
Joseph P. Walker, MD (PI); Jennifer Banks (VA/R); Debbie Ciampaglia (OP/OCT); Danielle Dyshanowitz (VA/R); Jennifer Frederick, CRC (CC); A. Tom Ghuman, MD (O); Richard Grodin, MD (O); Cheryl Kiesel, CCRC (CC); Eileen Knips, RN, CCRC, CRA (OP/OCT); Jonathan McCue (VA/R); Maria Ortiz (VA/R); Crystal Peters, CCRC (CC); Paul Raskauskas, MD (O); Etienne Schoeman (OP/OCT); Ashish Sharma, MD (O); Glenn Wing, MD (O), Rebecca Youngblood (CC).
University of Wisconsin Madison (Madison, WI)
Suresh R. Chandra, MD (PI); Michael Altaweel, MD (O); Barbara Blodi, MD (O); Kathryn Burke, BA (VA/R); Kristine A. Dietzman, (CC); Justin Gottlieb, MD (O); Gene Knutson (OP/OCT); Denise Krolnik (OP/OCT); T. Michael Nork, MD (O); Shelly Olson (VA/R); John Peterson, CRA (OP/OCT); Sandra Reed (OP/OCT); Barbara Soderling (VA/R); Guy Somers (VA/R); Thomas Stevens, MD (O); Angela Wealti, (CC).
Duke University Eye Center (Durham, NC)
Srilaxmi Bearelly, MD (PI); Brenda Branchaud (VA/R); Joyce W. Bryant, COT, CPT (CC/VA/R); Sara Crowell (CC/VA); Sharon Fekrat, MD (O); Merritt Gammage (OP/OCT); Cheala Harrison, COA (VA/R); Sarah Jones (VA); Noreen McClain, COT, CPT, CCRC (VA/R); Brooks McCuen, MD (O); Prithvi Mruthyunjaya, MD (O); Jeanne Queen, CPT (OP/OCT); Neeru Sarin, MBBS (VA/R); Cindy Skalak, RN, COT (VA/R); Marriner Skelly, CRA (OP/OCT); Ivan Suner, MD (O); Ronnie Tomany (OP/OCT); Lauren Welch (OP/OCT).
University of California-Davis Medical Center (Sacramento, CA)
Susanna S. Park, MD, PHD (PI); Allison Cassidy (VA/R); Karishma Chandra (OP/OCT); Idalew Good (VA/R); Katrina Imson (CC); Sashi Kaur (OP/OCT); Helen Metzler, COA, CCRP (CC/VA/R); Lawrence Morse, MD, PHD (O); Ellen Redenbo, ROUB (OP/OCT); Marisa Salvador (VA/R); David Telander, MD (O); Mark Thomas, CRA (OCT); Cindy Wallace, COA (CC).
University of Louisville School of Medicine, KY (Louisville, KY)
Charles C. Barr, MD (PI); Amanda Battcher (VA/R); Michelle Bottorff, COA (CC/OCT); Mary Chasteen (VA/R); Kelly Clark (VA/R); Diane Denning, COT (OCT); Debra Schoen (OP); Amy Schultz (OP); Evie Tempel, CRA, COA (OP); Lisa Wheeler, COT (VA/R); Greg K. Whittington, MPS, PSY (CC).
Retina Associates of Kentucky (Lexington, KY)
Thomas W. Stone, MD (PI); Todd Blevins (OP/OCT); Michelle Buck, COT, (VA/R/OCT); Lynn Cruz, COT (CC); Wanda Heath (VA/R); Diana Holcomb (VA/R); Rick Isernhagen, MD (O); Terri Kidd, COA (OCT); John Kitchens, MD (O); Cathy Sears, CST, COA (VA/R); Ed Slade, CRA, COA (OP/OCT); Jeanne Van Arsdall, COA (VA/R); Brenda VanHoose, COA (VA/R); Jenny Wolfe, RN (CC); William Wood, MD (O).
Colorado Retina Associates (Denver, CO)
John Zilis, MD (PI); Carol Crooks, COA (VA/R); Larry Disney (VA/R); Mimi Liu, MD (O); Stephen Petty, MD (O); Sandra Sall, ROUB, COA (CC/VA/R/OP/OCT).
University of Iowa Hospitals & Clinics (Iowa City, IA)
James C. Folk, MD (PI); Tracy Aly, CRA (OP/OCT); Abby Brotherton (VA); Douglas Critser, CRA (OP/OCT); Connie J. Hinz, COT, CCRC (CC/VA/R); Stefani Karakas, CRA (OP/OCT); Valerie Kirschner (VA); Cheyanne Lester (VA/R); Cindy Montague, CRA (OP/OCT); Stephen Russell, MD (O); Heather Stockman (VA/R); Barbara Taylor, CCRC (VA/R); Randy Verdick, FOPS (OP/OCT), Jean Walshire (CC).
Retina Specialists (Towson, MD)
John T. Thompson, MD (PI); Barbara Connell (VA/R); Maryanth Constantine (CC); John L. Davis Jr (VA/R); Gwen Holsapple (VA/R); Lisa Hunter (OP/OCT); C. Nicki Lenane (CC/VA/R/OP/OCT); Robin Mitchell (CC); Leslie Russel, CRA (OP/OCT); Raymond Sjaarda, MD (O).
Retina Consultants of Houston (Houston, TX)
David M. Brown, MD (PI); Matthew Benz, MD (O); Llewellyn Burns (OCT); JoLene G. Carranza, COA, CCRC (CC); Richard Fish, MD (O); Debra Goates (VA/R); Shayla Hay (VA/R); Theresa Jeffers, COT (VA/R); Eric Kegley, CRA, COA (OP/OCT); Dallas Kubecka (VA/R); Stacy McGilvra (VA/R); Beau Richter (OCT); Veronica Sneed, COA (VA/R); Cary Stoever (OCT); Isabell Tellez (VA/R); Tien Wong, MD (O).
Massachusetts Eye and Ear Infirmary/Harvard Vanguard Medical Associates (Boston, MA)
Ivana Kim, MD (PI); Christopher Andreoli, MD (O); Leslie Barresi, CRA, COA, OCT-C (VA/OP/OCT); Sarah Brett (OP); Charlene Callahan (OP); Karen Capaccioli (OCT); William Carli, COA (VA/R/OCT); Matthew Coppola, COA (VA); Nicholas Emmanuel (CC); Claudia Evans, OD (VA/R); Anna Fagan, COA (VA/R); Marcia Grillo (OCT); John Head, CRA, OCT-C (OP/OCT); Troy Kieser, COA, OCT-C (CC/VA/R); Elaine Lee, COA (VA); Ursula Lord, OD (VA/R); Edward Miretsky (CC); Kate Palitsch (OP/OCT); Todd Petrin, RN (OCT); Liz Reader (CC); Svetlana Reznichenko, COA (VA); Mary Robertson, COA (VA); Justin Smith, OD (VA/R); Demetrios Vavvas, MD, PHD (O).
Palmetto Retina Center (West Columbia, SC)
John Wells, MD (PI); Cassie Cahill (VA/R); W. Lloyd Clark, MD (O); Kayla Henry (VA/R); David Johnson, MD (O); Peggy Miller (CC/VA/R); LaDetrick Oliver, COT (OP/OCT); Robbin Spivey (OP/OCT); Tiffany Swinford (VA/R); Mallie Taylor (CC).
Retina and Vitreous of Texas (Houston, TX)
Michael Lambert, MD (PI); Kris Chase (OP/OCT); Debbie Fredrickson, COA (VA/R); Joseph Khawly, MD, FACS (O); Valerie Lazarte (VA/R); Donald Lowd (OP/OCT); Pam Miller (CC); Arthur Willis, MD (O).
Long Island Vitreoretinal Consultants (Great Neck, NY)
Philip J. Ferrone, MD (PI); Miguel Almonte (OCT); Rachel Arnott, (CC); Ingrid Aviles (VA/R/OCT); Sheri Carbon (VA/R); Michael Chitjian (OP/OCT); Kristen DAmore (CC); Christin Elliott (VA/R); David Fastenberg, MD (O); Barry Golub, MD (O); Kenneth Graham, MD (O); AnnMarie Lavorna (CC); Laura Murphy (VA/R); Amanda Palomo (VA/R); Christina Puglisi (VA/R); David Rhee, MD (O); Juan Romero, MD (O); Brett Rosenblatt, MD (O); Glenda Salcedo (OP/OCT); Marianne Schlameuss, RN (CC); Eric Shakin, MD (O); Vasanti Sookhai (VA/R).
Wills Eye Institute/Mid Atlantic Retina (Philadelphia, PA)
Richard Kaiser, MD (PI); Elizabeth Affel, MS, OCT-C (OCT); Gary Brown, MD (O); Christina Centinaro (CC); Deborah Fine, COA (OCT); Mitchell Fineman, MD (O); Michele Formoso (CC); Sunir Garg, MD (O); Lisa Grande (VA/R); Carolyn Herbert (VA/R); Allen Ho, MD (O); Jason Hsu, MD (O); Maryann Jay (OCT); Lisa Lavetsky (OCT); Elaine Liebenbaum (OP); Joseph Maguire, MD (O); Julia Monsonego (OP/OCT); Lucia O’Connor (OCT); Lisa Pierce (CC); Carl Regillo, MD (O); Maria Rosario (DE); Marc Spirn, MD (O); James Vander, MD (O); Jennifer Walsh (VA/R).
Ohio State University Eye Physicians & Surgeons-Retina Division (Dublin, OH)
Frederick H. Davidorf, MD (PI); Amanda Barnett (OP/OCT); Susie Chang, MD (O); John Christoforidis, MD (O); Joy Elliott (CC); Heather Justice (VA/R); Alan Letson, MD (O); Kathryne McKinney, COMT (CC); Jeri Perry, COT (VA/R); Jill A. Salerno, COA (CC); Scott Savage (OP); Stephen Shelley (OCT).
Retina Associates of Cleveland (Beachwood, OH)
Lawrence J. Singerman, MD (PI); Joseph Coney, MD (O); John DuBois (OP/OCT); Kimberly DuBois, LPN, CCRP, COA (VA/R); Gregg Greanoff, CRA (OP/OCT); Dianne Himmelman, RN, CCRC (CC); Mary Ilc, COT (VA/R); Elizabeth Mcnamara (VA/R/OP); Michael Novak, MD (O); Scott Pendergast, MD (O); Susan Rath, PA-C (CC); Sheila Smith-Brewer, CRA (OP/OCT); Vivian Tanner, COT, CCRP (VA/R); Diane E. Weiss, RN, (CC); Hernando Zegarra, MD (O).
Retina Group of Florida (Fort Lauderdale, FL)
Lawrence Halperin, MD (PI); Patricia Aramayo (OCT); Mandeep Dhalla, MD (O); Brian Fernandez, MD (OP/OCT); Cindy Fernandez, MD (CC); Jaclyn Lopez (CC); Monica Lopez (OCT); Jamie Mariano, COA (VA/R); Kellie Murphy, COA (OCT); Clifford Sherley, COA (VA/R); Rita Veksler, COA (OP/OCT).
Retina-Vitreous Associates Medical Group (Beverly Hills, CA)
Firas Rahhal, MD (PI); Razmig Babikian (DE); David Boyer, MD (O); Sepideh Hami (DE); Jeff Kessinger (OP/OCT); Janet Kurokouchi (CC); Saba Mukarram (VA/R); Sarah Pachman (VA/R); Eric Protacio (OCT); Julio Sierra (VA/R); Homayoun Tabandeh, MD, MS, FRCP (O); Adam Zamboni (VA/R).
Elman Retina Group, P.A. (Baltimore, MD)
Michael Elman, MD (PI); Jennifer Belz (CC); Tammy Butcher (CC); Theresa Cain (OP/OCT); Teresa Coffey, COA (VA/R); Dena Firestone (VA/R); Nancy Gore (VA/R); Pamela Singletary (VA/R); Peter Sotirakos (OP/OCT); JoAnn Starr (CC).
University of North Carolina at Chapel Hill (Chapel Hill, NC)
Travis A. Meredith, MD (PI); Cassandra J. Barnhart, MPH (CC/VA/R); Debra Cantrell, COA (VA/R/OP/OCT); RonaLyn Esquejo-Leon (OP/OCT); Odette Houghton, MD (O); Harpreet Kaur (VA/R); Fatoumatta NDure, COA (CC).
Ophthalmologists Enrolling Patients but No Longer Affiliated with a CATT Center
Ronald Glatzer, MD (O); Leonard Joffe, MD (O); Reid Schindler, MD (O).
Resource Centers
Chairman’s Office (Cleveland Clinic, Cleveland, OH)
Daniel F. Martin, MD (Chair); Stuart L. Fine, MD (Vice-Chair; University of Colorado, Denver, CO); Marilyn Katz (Executive Assistant).
Coordinating Center (University of Pennsylvania, Philadelphia, PA)
Maureen G. Maguire, PhD (PI); Mary Brightwell-Arnold, SCP (Systems Analyst); Ruchira Glaser, MD (Medical Monitor); Judith Hall (Protocol Monitor); Sandra Harkins (Staff Assistant); Jiayan Huang, MS (Biostatistician); Alexander Khvatov, MS (Systems Analyst); Kathy McWilliams, CCRP (Protocol Monitor); Susan K. Nolte (Protocol Monitor); Ellen Peskin, MA, CCRP (Project Director); Maxwell Pistilli, MS, MEd (Biostatistician); Susan Ryan (Financial Administrator); Allison Schnader (Administrative Coordinator); Gui-Shuang Ying, PhD (Senior Biostatistician).
OCT Reading Center (Duke University, Durham, NC)
Glenn Jaffe, MD (PI); Jennifer Afrani-Sakyi (CATT PowerPoint Presentations); Brannon Balsley (OCT Technician Certifications); Linda S. Bennett (Project Manager); Adam Brooks (Reader/SD-Reader); Adrienne Brower-Lingsch (Reader); Lori Bruce (Data Verification); Russell Burns (Senior Technical Analyst/Senior Reader/SD Reader/OCT Technician Certifications); Dee Busian (Reader); John Choong (Reader); Lindsey Cloaninger (Reader Reliability Studies/Document Creation/CATT PPT Files); Francis Char DeCroos (Research Associate); Emily DuBois (Data Entry); Mays El-Dairi (Reader/SD-Reader); Sarah Gach (Reader); Katelyn Hall (Project Manager/Reader Reliability Studies/Data Verification/Document Creation); Terry Hawks (Reader); ChengChenh Huang (Reader); Cindy Heydary (Senior Reader/Quality Assurance Coordinator/SD Reader/Data Verification); Alexander Ho (Reader, Transcription); Shashi Kini (Data Entry/Transcription); Michelle McCall (Data Verification); Daaimah Muhammad (Reader Feedback); Jayne Nicholson (Data Verification); Jeanne Queen (Reader/SD-Reader); Pamela Rieves (Transcription); Kelly Shields (Senior Reader); Cindy Skalak (Reader); Adam Specker (Reader); Sandra Stinnett (Biostatistician); Sujatha Subramaniam (Reader); Patrick Tenbrink (Reader); Cynthia Toth, MD (Director of Grading); Aaron Towe (Reader); Kimberly Welch (Data Verification); Natasha Williams (Data Verification); Katrina Winter (Senior Reader); Ellen Young (Senior Project Manager).
Fundus Photograph Reading Center (University of Pennsylvania, Philadelphia, PA)
Juan E. Grunwald, MD (PI); Judith Alexander (Director); Ebenezer Daniel, MBBS, MS, MPH, PhD (Director); Elisabeth Flannagan (Administrative Coordinator); E. Revell Martin (Reader); Candace Parker (Reader); Krista Sepielli (Reader); Tom Shannon (Systems Analyst); Claressa Whearry (Data Coordinator).
National Eye Institute, National Institutes of Health
Maryann Redford, DDS, MPH (Program Officer).
Committees
Executive Committee
Daniel F. Martin, MD (chair); Robert L. Avery, MD; Sophie J. Bakri, MD; Ebenezer Daniel, MBBS, MS, MPH; Stuart L. Fine, MD; Juan E. Grunwald, MD; Glenn Jaffe, MD, Marcia R. Kopfer, BS, COT; Maureen G. Maguire, PhD; Travis A. Meredith, MD; Ellen Peskin, MA, CCRP; Maryann Redford, DDS, MPH; David F. Williams, MD.
Operations Committee
Daniel F. Martin, MD (chair); Linda S. Bennett; Ebenezer Daniel, MBBS, MS, MPH; Frederick L. Ferris III, MD; Stuart L. Fine, MD; Juan E. Grunwald, MD; Glenn Jaffe, MD; Maureen G. Maguire, PhD; Ellen Peskin, MA, CCRP; Maryann Redford, DDS, MPH; Cynthia Toth, MD.
Clinic Monitoring Committee
Ellen Peskin, MA, CCRP (chair); Mary Brightwell-Arnold, SCP; Joan DuPont; Maureen G. Maguire, PhD; Kathy McWilliams, CCRP; Susan K. Nolte.
Data and Safety Monitoring Committee
Lawrence M. Friedman, MD (chair); Susan B. Bressler, MD; David L. DeMets, PhD; Martin Friedlander, MD, PhD; Mark W. Johnson, MD; Anne Lindblad, PhD; Douglas W. Losordo, MD, FACC; Franklin G. Miller, PhD.
Footnotes
ClinicalTrials.gov number, NCT00593450
Presented in part at the Association for Research in Vision and Ophthalmology Meeting. Ft. Lauderdale, Florida, May 8, 2012.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Age-Related Eye Disease Study Research Group. The Age-Related Eye Disease Study severity scale for age-related macular degeneration: AREDS report no. 17. Arch Ophthalmol. 2005;123:1484–98. doi: 10.1001/archopht.123.11.1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Age-Related Eye Disease Study Research Group. A simplified severity scale for age-related macular degeneration: AREDS report no. 18. Arch Ophthalmol. 2005;123:1570–4. doi: 10.1001/archopht.123.11.1570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Macular Photocoagulation Study Group. Risk factors for choroidal neovascularization in the second eye of patients with juxtafoveal or subfoveal choroidal neovascularization secondary to age-related macular degeneration. Arch Ophthalmol. 1997;115:741–7. doi: 10.1001/archopht.1997.01100150743009. [DOI] [PubMed] [Google Scholar]
- 4.Pieramici DJ, Bressler SB. Age-related macular degeneration and risk factors for the development of choroidal neovascularization in the fellow eye. Curr Opin Ophthalmol. 1998;9:38–46. doi: 10.1097/00055735-199806000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Prenner JL, Rosenblatt BJ, Tolentino MJ, et al. CNVPT Research Group. Risk factors for choroidal neovascularization and vision loss in the fellow eye study of CNVPT. Retina. 2003;23:307–14. doi: 10.1097/00006982-200306000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Submacular Surgery Trials Research Group. Incident choroidal neovascularization in fellow eyes of patients with unilateral subfoveal choroidal neovascularization secondary to age-related macular degeneration: SST report no. 20 from the Submacular Surgery Trials Research Group. Arch Ophthalmol. 2007;125:1323– 30. doi: 10.1001/archopht.125.10.1323. [DOI] [PubMed] [Google Scholar]
- 7.Barbazetto IA, Saroj N, Shapiro H, et al. Incidence of new choroidal neovascularization in fellow eyes of patients treated in the MARINA and ANCHOR trials. Am J Ophthalmol. 2010;149:939–46. doi: 10.1016/j.ajo.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 8.Wang JJ, Rochtchina E, Lee AJ, et al. Ten-year incidence and progression of age-related maculopathy: the Blue Mountains Eye Study. Ophthalmology. 2007;114:92–8. doi: 10.1016/j.ophtha.2006.07.017. [DOI] [PubMed] [Google Scholar]
- 9.Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol. 2001;119:1417–36. doi: 10.1001/archopht.119.10.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Curtis LH, Hammill BG, Schulman KA, Cousins SW. Risks of mortality, myocardial infarction, bleeding, and stroke associated with therapies for age-related macular degeneration. Arch Ophthalmol. 2010;128:1273–9. doi: 10.1001/archophthalmol.2010.223. [DOI] [PubMed] [Google Scholar]
- 11.Brechner RJ, Rosenfeld PJ, Babish JD, Caplan S. Pharmacotherapy for neovascular age-related macular degeneration: an analysis of the 100% 2008 Medicare fee-for-service Part B claims file. Am J Ophthalmol. 2011;151:887–95. doi: 10.1016/j.ajo.2010.11.017. [DOI] [PubMed] [Google Scholar]
- 12.CATT Research Group. Ranibizumab and bevacizumab for neovascular age-related macular degeneration. N Engl J Med. 2011;364:1897–908. doi: 10.1056/NEJMoa1102673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Martin DF, Mabuire MG, Fine SL, et al. Comparison of Age-related Macular Degeneration Treatments Trials (CATT) Research Group. Ranibizumab and bevacizumab for treatment of neovascular age-related macular degeneration: two-year results. Ophthalmology. 2012;119:1388–98. doi: 10.1016/j.ophtha.2012.03.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chakravarthy U, Harding SP, Rogers CA, et al. IVAN Study Investigators. Ranibizumab versus bevacizumab to treat neovascular age-related macular degeneration: one-year findings from the IVAN randomized trial. Ophthalmology. 2012;119:1399–411. doi: 10.1016/j.ophtha.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 15.Avery RL, Pearlman J, Pieramici DJ, et al. Intravitreal bevacizumab (Avastin) in the treatment of proliferative diabetic retinopathy. Ophthalmology. 2006;113:1695–705. doi: 10.1016/j.ophtha.2006.05.064. [DOI] [PubMed] [Google Scholar]
- 16.Acharya NR, Sittivarakul W, Qian Y, et al. Bilateral effect of unilateral ranibizumab in patients with uveitis-related macular edema. Retina. 2011;31:1871–6. doi: 10.1097/IAE.0b013e318213da43. [DOI] [PubMed] [Google Scholar]
- 17.Al-Dhibi H, Khan AO. Bilateral response following unilateral intravitreal bevacizumab injection in a child with uveitic cystoid macular edema. J AAPOS. 2009;13:400–2. doi: 10.1016/j.jaapos.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 18.Grunwald JE, Daniel E, Ying GS, et al. CATT Research Group. Photographic assessment of baseline fundus morphologic features in the Comparison of Age-Related Macular Degeneration Treatments Trials. Ophthalmology. 2012;119:1634–41. doi: 10.1016/j.ophtha.2012.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.DeCroos FC, Toth CA, Stinnett SS, et al. CATT Research Group. Optical coherence tomography grading reproducibility during the Comparison of Age-Related Macular Degeneration Treatments Trials. Ophthalmology. 2012;119:2549–57. doi: 10.1016/j.ophtha.2012.06.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Deangelis MM, Silveira AC, Carr EA, Kim IK. Genetics of age-related macular degeneration: current concepts, future directions. Semin Ophthalmol. 2011;26:77–93. doi: 10.3109/08820538.2011.577129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hagstrom SA, Ying GS, Pauer GJ, et al. Comparison of AMD Treatments Trials Research Group. Pharmacogenetics for genes associated with age-related macular degeneration in the Comparison of AMD Treatments Trials (CATT) Ophthalmology. doi: 10.1016/j.ophtha.2012.11.037. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lim LS, Mitchell P, Seddon JM, et al. Age-related macular degeneration. Lancet. 2012;379:1728–38. doi: 10.1016/S0140-6736(12)60282-7. [DOI] [PubMed] [Google Scholar]
- 23.Avery RL. Bevacizumab (Avastin) for retinopathy of prematurity: wrong dose, wrong drug, or both? J AAPOS. 2012;16:2–4. doi: 10.1016/j.jaapos.2011.11.002. [DOI] [PubMed] [Google Scholar]
- 24.Meyer CH, Holz FG. Preclinical aspects of anti-VEGF agents for the treatment of wet AMD: ranibizumab and bevacizumab. Eye (Lond) 2011;25:661–72. doi: 10.1038/eye.2011.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Carneiro AM, Costa R, Falcao MS, et al. Vascular endothelial growth factor plasma levels before and after treatment of neovascular age-related macular degeneration with bevacizumab or ranibizumab [report online] Acta Ophthalmol. 2012;90:e25–30. doi: 10.1111/j.1755-3768.2011.02240.x. [DOI] [PubMed] [Google Scholar]
- 26.Bakri SJ, Snyder MR, Reid JM, et al. Pharmacokinetics of intravitreal bevacizumab (Avastin) Ophthalmology. 2007;114:855–9. doi: 10.1016/j.ophtha.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 27.Bakri SJ, Snyder MR, Reid JM, et al. Pharmacokinetics of intravitreal ranibizumab (Lucentis) Ophthalmology. 2007;114:2179–82. doi: 10.1016/j.ophtha.2007.09.012. [DOI] [PubMed] [Google Scholar]
- 28.Gaudreault J, Fei D, Rusit J, et al. Preclinical pharmacokinetics of ranibizumab (rhuFabV2) after a single intravitreal administration. Invest Ophthalmol Vis Sci. 2005;46:726–33. doi: 10.1167/iovs.04-0601. [DOI] [PubMed] [Google Scholar]
- 29.Gaudreault J, Fei D, Beyer JC, et al. Pharmacokinetics and retinal distribution of ranibizumab, a humanized antibody fragment directed against VEGF-A, following intravitreal administration in rabbits. Retina. 2007;9:1260–6. doi: 10.1097/IAE.0b013e318134eecd. [DOI] [PubMed] [Google Scholar]
- 30.Nomoto H, Shiraga F, Kuno N, et al. Pharmacokinetics of bevacizumab after topical, subconjunctival, and intravitreal administration in rabbits. Invest Ophthalmol Vis Sci. 2009;50:4807–13. doi: 10.1167/iovs.08-3148. [DOI] [PubMed] [Google Scholar]
- 31.Lucentis (ranibizumab injection) [package insert] San Francisco, CA: Genentech Inc; 2013. [Accessed March 6, 2013]. Available at: http://www.gene.com/gene/products/information/pdf/lucentis-prescribing.pdf. AQ: note URL displays updated package insert, review to confirm information being cited is still present. [Google Scholar]
- 32.Sinapis CI, Routsias JG, Sinapis AI, et al. Pharmacokinetics of intravitreal bevacizumab (Avastin) in rabbits. Clin Ophthalmol. 2011;5:697–704. doi: 10.2147/OPTH.S19555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tolentino M. Systemic and ocular safety of intravitreal anti-VEGF therapies for ocular neovascular disease. Surv Ophthalmol. 2011;56:95–113. doi: 10.1016/j.survophthal.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 34.Matsuyama K, Ogata N, Matsuoka M, et al. Plasma levels of vascular endothelial growth factor and pigment epithelium-derived factor before and after intravitreal injection of bevacizumab. Br J Ophthalmol. 2010;94:1215–8. doi: 10.1136/bjo.2008.156810. [DOI] [PubMed] [Google Scholar]
- 35.Qian J, Lu Q, Tao Y, Jiang YR. Vitreous and plasma concentrations of apelin and vascular endothelial growth factor after intravitreal bevacizumab in eyes with proliferative diabetic retinopathy. Retina. 2011;31:161–8. doi: 10.1097/IAE.0b013e3181e46ad8. [DOI] [PubMed] [Google Scholar]
- 36.Davidovic SP, Nikolic SV, Curic NJ, et al. Changes of serum VEGF concentration after intravitreal injection of Avastin in treatment of diabetic retinopathy. Eur J Ophthalmol. 2012;22:792–8. doi: 10.5301/ejo.5000118. [DOI] [PubMed] [Google Scholar]
- 37.Sato T, Wada K, Arahori H, et al. Serum concentrations of bevacizumab (Avastin) and vascular endothelial growth factor in infants with retinopathy of prematurity. Am J Ophthalmol. 2012;153:327–33. doi: 10.1016/j.ajo.2011.07.005. [DOI] [PubMed] [Google Scholar]
- 38.Ziemssen F, Zhu Q, Peters S, et al. Tuebingen Bevacizumab Study Group. Intensified monitoring of circadian blood pressure and heart rate before and after intravitreous injection of bevacizumab: preliminary findings of a pilot study. Int Ophthalmol. 2009;29:213–24. doi: 10.1007/s10792-008-9221-7. [DOI] [PubMed] [Google Scholar]
- 39.Tamura H, Tsujikawa A, Yamashiro K, et al. Association of ARMS2 genotype with bilateral involvement of exudative age-related macular degeneration. Am J Ophthalmol. 2012;154:542–8. doi: 10.1016/j.ajo.2012.03.042. [DOI] [PubMed] [Google Scholar]
- 40.Lechanteur YT, van de Ven JP, Smailhodzic D, et al. Genetic, behavioral, and sociodemographic risk factors for second eye progression in age-related macular degeneration. Invest Ophthalmol Vis Sci. 2012;53:5846–52. doi: 10.1167/iovs.11-7731. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


