Abstract
Background
Resilience is a positive health outcome identified by the Committee on Future Direction for Behavioral and Social Sciences as a research priority for the National Institutes of Health. The Resilience in Illness Model (RIM) was developed from a series of qualitative and quantitative studies, to increase understanding of how positive health protective factors (i.e. social integration, family environment, courageous coping and derived meaning) may influence resilience outcomes. The RIM also includes two risk factors, illness-related distress and defensive coping.
Objective
The purpose of this two-part paper is to report on evaluation of the RIM for adolescents/young adults with cancer (AYA). Here, in Part 1, our purpose is to describe the exploratory RIM evaluation and in Part 2 we describe the confirmatory RIM evaluation.
Methods
An exploratory evaluation of RIM was done using exploratory latent variable structural equation modeling with a combined sample from two studies of pre-adolescents, and AYA with cancer ages 10 -26 years (n=202).
Results
Results, including goodness-of-fit indices, support the RIM as a theory with a high level of explained variance for outcomes of resilience (67%) and self-transcendence (63%). Variance explained for proximal outcomes ranged from 18% to 76%.
Conclusions
Findings indicate that, following confirmatory testing, the RIM may be a useful guide to developing targeted interventions that are grounded in the experiences of the AYA.
Implications for Practice
Increased understanding of the AYA cancer experience to improve holistic care.
In 2001, the Committee on Future Directions for Behavioral Health and Social Science Research at the National Institutes of Health urged increased research on positive health, defined as the “biological, behavioral and psychosocial factors that contribute to resilience, disease resistance, and wellness” (p.3).1 Specific to resilience, the committee recommended investigations to advance knowledge of resilience in the face of life adversity, giving particular emphasis to studies of protective resources that influence resilience and quality of life.1 Since 2001, increased research has enhanced our understanding of resilience, which is now primarily considered from a systems perspective, examined through multilevel analysis, and focused on understanding dynamics of how individuals adapt and change. 2–4 The purpose of this two-part paper is to report on evaluation of the Resilience in Illness Model (RIM), formerly named the Adolescent Resilience Model.5 Through a series of qualitative and quantitative studies conducted over 27 years, the RIM was developed to understand positive health processes and outcomes of adolescents and young adults with chronic illness, especially cancer.5–9 In Part 1, we describe the exploratory RIM evaluation and in Part 2 we describe the confirmatory RIM evaluation.
BACKGROUND
Cancer-related Concerns of Adolescents and Young Adults with Cancer
Adolescents and young adults with cancer (AYA) are a significant, yet neglected population that straddles both pediatric and adult cancer communities. Cancer is the leading cause of death by disease for AYA in the United States, and outcomes for AYA with cancer are not as good as those of younger children and some adults.10 Adolescents and young adults encounter numerous stressors specific to their cancer diagnosis, its treatment, and its potential late effects. Research indicates AYA have ongoing uncertainty about cancer-related concerns, and experience numerous unpleasant symptoms, altered body image and identity issues, social isolation, increased dependency, and decreased cognitive and academic abilities.11–14 In addition, AYA cancer survivors have more adverse general health, mental health, and functional impairment than their siblings without cancer, and high fear of recurrence.15–17 Adolescent cancer survivors also have greater identity status concerns related to disclosing their cancer diagnosis, as well as more symptoms of post-traumatic stress disorder than younger childhood cancer survivors.17
The poor outcomes for AYA with cancer are attributed to several factors, including lower enrollment in appropriate clinical trials and unique developmental and psychosocial issues.10 Adolescents and young adults pose a special challenge for health care providers because of their decreased adherence to treatment.18 Similar to their healthy cohort, they may also choose to be involved in high risk behaviors long-term.18 Adolescents and young adults generally do not receive adequate psychosocial services and very little theoretically based research has been conducted on interventions to help AYA with cancer positively adjust to the cancer experience.17,19
Protective Factors Fostering Resilience in Adolescents and Young Adults
While cancer-related stressors clearly have the potential to negatively influence outcomes, research also indicates there are protective factors that can buffer the adverse effects of having cancer. Support from health care providers, family, and friends are identified as ways to buffer concerns of adolescents/young adults with cancer.20–22 In addition, there is consistent evidence that individual protective factors of positive coping, spirituality, hope, purpose in life, and optimism contribute to better psychosocial adjustment.23–25
Development of the Resilience in Illness Model
Development of the RIM is guided by two worldviews
First, Lifespan Development provides a worldview that universally occurring development (e.g., puberty) is only one influencing factor on maturity;26,27 other factors include individual experience, global historical events, and contemporary contexts. Relevant to resilience is the influence of unique individual experiences that can accelerate maturity (e.g. receiving a cancer diagnosis at age 15 and facing the possibility of death), global historical events (e.g. ways the 911 attack on the USA influences age cohorts differently) and, contemporary contexts (e.g. the influence of new social media on ways adolescents interact with peers).27 Second, the Meaning-based Model worldview proposes that, to effectively predict and influence health outcomes, it is insufficient to merely consider the impact of disease on function. 28 A holistic understanding of an individual’s perceptions of their situation, (i.e., one’s meanings, patterns, and experiences of illness and one’s autonomy, beliefs, choices, and relationships with others) are also necessary.28
Model Development and Preliminary Model Evaluation
Using mixed methods research approaches described by Haase and colleagues,9 several studies were done to: 1) develop the RIM through inductive approaches; and 2) evaluate the RIM through instrument and model testing.7–9,29 Briefly, to assure adolescent/young adult experiences of dealing with chronic illness were accurately reflected and measured in the model, we conducted RIM development studies using phenomenology, simultaneous concept analysis, and instrumentation methods. Participants in these studies included adolescents/young adults with life-threatening and non-life threatening chronic illnesses (primarily cancer, but also asthma, cystic fibrosis, and scoliosis) between 11 and 21 years. Based on these RIM development studies, we defined resilience as “the process of identifying or developing resources and strengths to flexibly manage stressors to gain a positive outcome, a sense of confidence, mastery, and self-esteem” (p.125).7
Model evaluation is a step-wise process of testing and refining alternative exploratory models and then, using data from a different sample, doing a confirmatory analysis of the best fitting exploratory model. For RIM evaluation, we used a latent variable structural equation modeling approach. This advanced statistical approach provides a way to more fully capture the complexity of human experiences by combining multiple measures of constructs into latent variables.9
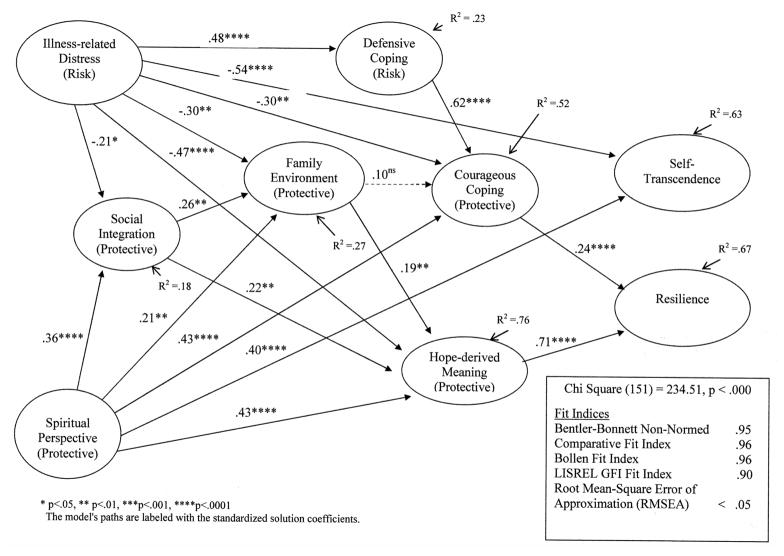
Our first RIM tests were done to assess the psychometric properties of the measures and specify a latent variable model.9 From these studies, protective and risk factors and their relationships to resilience outcomes were specified as depicted in Figure 1; definitions for each latent variable are in Table 1. Briefly, the RIM latent variables that were hypothesized to positively affect resilience outcomes directly or through other variables included the protective factors of social integration, family environment, courageous coping, and derived meaning. The RIM latent variables hypothesized to negatively affect resilience directly or through other variables included the risk factors of illness-related distress and defensive coping. The outcome latent variable for the RIM was resilience, which was hypothesized to include three indicators: a sense of confidence, self-esteem, and self-transcendence.a
Figure 1.
Hypothesized Exploratory Resilience in Illness Model (RIM) Latent Variables and Relationships
Table 1.
Exploratory Resilience in Illness Model (RIM) Latent Variables and Definitions
| Illness-related Distress (Risk) | The degree of illness-related uncertainty and disease and symptom-related distress perceived by the AYA. |
| Social Integration (Protective) | The degree to which the AYA perceives a sense of connectedness with and support from friends and health care providers in the midst of having cancer. |
| Family Environment (Protective) | The degree to which the AYA perceives the family as adaptable, cohesive, effectively communicating, and having family strengths. |
| Defensive Coping (Risk) | The degree to which the AYA uses evasive and emotive coping strategies to deal with the cancer experience. |
| Courageous Coping (Protective) | The degree to which the AYA uses confrontive, optimistic, and supportant coping strategies to deal with the cancer experience. |
| Derived Meaning (Protective) | The degree to which the AYA uses hope and spiritual perspective to derive meaning from the cancer experience. |
| Resilience (Process and Outcome) | The process of identifying or developing resources and strengths to flexibly manage stressors to gain a positive outcome, a sense of confidence/mastery, self-transcendence, and self-esteem. |
DESIGN AND METHODS
The exploratory model test reported here used a cross-sectional, theory-evaluation design. To have an adequate sample size to test the full model depicted in Figure 1, data were combined from two studies, hereafter called RIM 1 and RIM 2. RIM 1 was cross-sectional. RIM 2 was done with a repeated-measures design, however only baseline data obtained at diagnosis were used for the RIM evaluation.
Sample and Setting
Demographic information for RIM 1 and RIM 2 are summarized in Table 2. RIM 1, completed in 1999, used a convenience sample of non-hospitalized, English-speaking pre-adolescents/adolescents/young adults with cancer, ages 10 to 26, whose time since diagnosis ranged from <1 year to 18 years.9 RIM 2, completed in 2004, used a convenience sample of hospitalized or non-hospitalized, English-speaking pre-adolescents/adolescents/young adults who were newly diagnosed with cancer. There were no restrictions on the type or stage of cancer in either study. Adolescents and young adults with cognitive disabilities were excluded. Following institutional human subjects approvals, participants were recruited from study-eligible adolescents/young adults seen in large medical centers in Oklahoma, South Carolina, and Vancouver, British Columbia (for RIM 1 only); Arizona, California, and Indiana (for RIM 2 only). With the exception of two sites, all had a children’s hospital and all sites provided tertiary care in metropolitan areas that serve large catchments with culturally diverse urban and rural populations.
Table 2.
Frequency Distribution of Demographic Data for RIM1 (n=128) and RIM 2 (n=74) Studies
| Variable | Study1 N (%) | Study 2 N (%) |
|---|---|---|
| Sex | ||
| Males | 67 (52.3) | 44 (59.5) |
| Females | 60 (46.9) | 30 (40.5) |
| Missing | 1 (.8) | 0 (0.0) |
| Current Age | ||
| 10 thru 13 years | 23 (18.0) | 19 (25.7) |
| 14 thru 15 years | 26 (20.3) | 31 (41.9) |
| 16 thru 17 years | 36 (28.1) | 19 (25.7) |
| 18 thru 19 years | 27 (21.1) | 4 (5.4) |
| 20 thru 26 years | 15 (11.7) | 1 (1.4) |
| Missing | 1 (.8) | 0 (0.0) |
| Age at Diagnosis | ||
| Birth thru 9 years | 49 (38.3) | -- |
| 10 thru 13 years | 38 (29.7) | 19 (25.7) |
| 14 thru 15 years | 20 (15.6) | 31 (41.9) |
| 16 thru 17 years | 13 (10.2) | 19 (25.7) |
| 18 thru 21 years | 5 (3.9) | 5 (6.8) |
| Missing | 3 (2.3) | 0 (0.0) |
| Time Since Diagnosis | ||
| Newly diagnosed | 7 (5.5) | 74 (100.0) |
| 1 year | 14 (10.9) | |
| 2 thru 3 years | 25 (19.5) | |
| 4 thru 6 years | 29 (22.7) | |
| 7 thru 18 years | 49 (38.3) | |
| Missing | 4 (3.1) | |
| Religious Preference | ||
| Catholic | 43 (33.6) | 15 (20.3) |
| Jewish | 4 (3.1) | 2 (2.7) |
| Muslim | 1 (.8) | -- |
| Protestant | 47 (36.7) | 21 (28.4) |
| Other | 12 (9.4) | 15 (20.3) |
| No Preference | 20 (15.6) | 18 (24.3) |
| Missing | 1 (.8) | 3 (4.1) |
| Race or Ethnic Background | ||
| Asian American | 6 (4.7) | 4 (5.4) |
| African American/Black | 12 (9.4) | 3 (4.1) |
| Hispanic/Latino American | 35 (27.3) | 10 (13.5) |
| Native American | 3 (2.3) | 5 (6.8) |
| Non-Hispanic Caucasian American | 62 (48.4) | 46 (62.2) |
| Other | 5 (3.9) | 2 (2.7) |
| Missing | 5 (3.9) | 4 (5.4) |
| Religious Participation Missing | ||
| Inactive | 32 (25.0) | 19 (25.7) |
| 1 to 2 times per year | 19 (14.8) | 16 (21.6) |
| More than 4 times per year | 29 (22.7) | 12 (16.2) |
| Weekly year round | 44 (34.4) | 24 (32.4) |
| Missing | 4 (3.1) | 3 (4.1) |
| Annual Family Income | ||
| Less than $20,000 | 38 (29.7) | -- |
| $20,000 to $49,000 | 42 (32.8) | -- |
| Greater than $50,000 | 29 (22.7) | -- |
| Missing | 19 (14.8) | -- |
Procedures
Each participant, and a parent or guardian in the case of minors, was approached about the study by a clinical nurse specialist or social worker who worked in the setting. Among those who were eligible and approached, refusal rates across the study sites ranged from 10 to 15 percent. Examples of reasons for declining to participate included lack of time and feeling too sick. After giving informed consent and/or assent to participate, the AYA in both studies completed a booklet of RIM instruments while in the health care setting or at home following a period of instruction. The booklet was designed to be user-friendly and included encouraging comments and ethnic- and gender-varied pictures. The study participants were asked to complete the questionnaires without discussion with parents or others. For participants who completed the booklet in the health care setting, the data collector was available to answer questions about format or meanings of words. For participants who took the booklets home to complete, arrangements were made for a follow-up phone call to answer questions. Participants were encouraged to record questions that arose as they were completing the booklet. The booklet of instruments was to be completed and returned in a stamped, self-addressed envelope within a 24-hour period. In a few cases, the AYA was too ill to complete in the timeframe; in these cases they returned the questionnaires when they could complete it within a two week period. The estimated time-on-task to complete the booklet was between 45 and 120 minutes. A monetary incentive of $5.00 was provided in RIM 1 and $10.00 in RIM 2 for each data collection time.
Measures
Summary psychometric properties, including reliability, of the indicators used in this final (best fitting) exploratory measurement model are presented in Table 3. Each measure was selected from established measures or developed when necessary, depending on whether potential established measures’ were congruent with the qualitatively derived theme categories from our preliminary model generating studies.7,9 As evidence of internal consistency reliability, Cronbach alpha coefficients for full measures were in an acceptable range from .78 to .94. As expected, four subscale indicators that included only 4 to 5 items had lower Cronbach alpha coefficients (.64 to .65). In addition to Cronbach alpha evidence of internal consistency, the fit of the final exploratory measurement model (Figure 2) supports the construct validity of the individual measures. The following brief descriptions of the instruments are ordered according to latent variables in the final exploratory RIM (See Figure 1).
Table 3.
Summary Psychometric Properties of Final Exploratory RIM Measurement Model Indicators
| Factor/Indicator | Number of Items | N | Alpha Reliability | Score Range | Mean (SD) |
|---|---|---|---|---|---|
| Illness-related Distress (Risk) | |||||
| McCorkle Symptom Distress Scale | 11 | 195 | .82 | 1.00 to 3.73 | 1.75 (.57) |
| Mishel Uncertainty - Mean of Complexity/Ambiguity | _a | 200 | NA | 1.09 to 3.60 | 2.25 (.61) |
| Complexity - Reverse Coded | 11 | 200 | .79 | 1.00 to 3.64 | 2.21 (.62) |
| Ambuiguity – Reverse Coded | 16 | 200 | .88 | 1.00 to 4.19 | 2.30 (.70) |
| Spiritual Perspective (Protective) | |||||
| Spirituality – Frequency | 4 | 201 | .83 | 1.00 to 6.00 | 3.93 (1.37) |
| Spirituality – Beliefs | 6 | 201 | .94 | 1.00 to 6.00 | 4.14 (1.58) |
| Social Integration (Protective) | |||||
| Perceived Social Support from Healthcare Professionals | 20 | 202 | .93 | 1.21 to 9.00b | 5.98 (2.12)b |
| Perceived Social--Support from Friends | 20 | 202 | .93 | 1.00 to 9.00b | 6.65 (2.04)b |
| Family Environment (Protective) | |||||
| Family Cohesiveness | 16 | 202 | .90 | 1.25 to 4.94 | 3.51 (.76) |
| Family Adaptability | 13 | 202 | .85 | 1.00 to 4.75 | 3.32 (.74) |
| Communication Unproblematic with Parents–Mean of Mother & Father | _a | 201 | NA | 1.00 to 5.00 | 3.27 (.81) |
| Unproblematic Communication with Mother | 9 | 198 | .78 | 1.00 to 5.00 | 3.32 (.85) |
| Unproblematic Communication with Father | 9 | 172 | .81 | 1.00 to 5.00 | 3.29 (.89) |
| Communication Open with Parents – Mean of Mother & Father | _a | 201 | NA | 1.00 to 5.00 | 3.76 (.85) |
| Communication Open with Mother | 10 | 198 | .91 | 1.50 to 5.00 | 3.94 (.89) |
| Communication Open with Father | 10 | 172 | .93 | 1.00 to 5.00 | 3.57 (1.00) |
| Family Strengths | 12 | 200 | .90 | 1.25 to 5.00 | 3.56 (.80) |
| Social Support- Family | 20 | 202 | .94 | 1.21 to 9.00b | 6.47 (2.25)b |
| Defensive Coping (Risk) | |||||
| Use Defensive Coping - Mean of Evasive & Emotive | _a | 201 | NA | 0.00 to 2.83 | 1.30 (.60) |
| Use Evasive Coping | 13 | 201 | .80 | 0.00 to 3.00 | 1.38 (.60) |
| Use Emotive Coping | 5 | 201 | .65 | 0.00 to 3.00 | 1.22 (.69) |
| Courageous Coping (Protective) | |||||
| Use Confrontive Coping | 10 | 201 | .82 | 0.00 to 3.00 | 1.59 (.67) |
| Use Optimistic Coping | 9 | 201 | .82 | 0.00 to 9.00b | 4.66 (2.27)b |
| Use Supportant Coping | 5 | 201 | .65 | 0.00 to 3.00 | 1.68 (.68) |
| Hope-derived Meaning (Protective) | |||||
| Herth Hope: Positive Readiness/Expectancy | 4 | 201 | .64 | 1.75 to 4.00 | 3.35 (.52) |
| Herth Hope: Interconnectedness | 4 | 201 | .65 | 1.75 to 4.00 | 3.37 (.52) |
| Self-transcendence (Outcome) | |||||
| Reed Self-Transcendence | 13 | 200 | .83 | 1.75 to 4.00 | 3.22 (.50) |
| Resilience (Outcome) | |||||
| Haase Resilience in Illness Scale | 12 | 202 | .87 | 2.01 to 36.00b | 25.51 (6.21)b |
Values represent the score distribution after applying the square transformation to produce a more nearly normal distribution.
This summary scale score is a mean of its two subscale scores, and each of the subscale scores is a mean over items in that subscale.
Values represent results of squared scores
Figure 2.
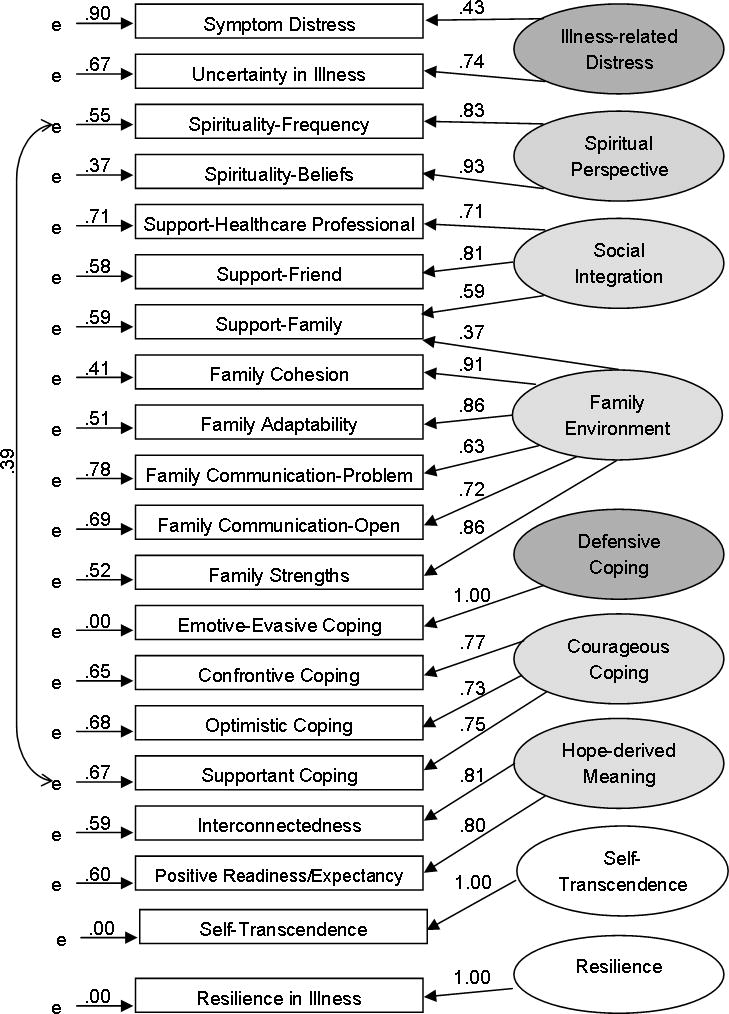
Final Exploratory RIM Measurement Model
Illness-related Distress (Risk Factor) included measures of symptom distress and uncertainty in illness. The Symptom Distress Scale 30 assesses 10 symptoms, such as pain, nausea, and insomnia. Verbal anchors describe symptom intensity, with a higher score indicating higher distress. The Mishel Uncertainty in Illness Scale-Revised31 consists of two factors: complexity and ambiguity. When the measurement model was initially run as specified, the complexity subscale captured the majority of the variance in uncertainty associated with Illness-Related Distress. To retain the theoretically derived and holistic meaning of uncertainty in illness conceptualized by Mishel,31 we used a mean score of the complexity and ambiguity subscales for this study.
Social Integration (Protective Factor) included two one-dimensional measures, Perceived Social Support from Friends32 and Perceived Social Support from Health Care Providers. The latter scale was adapted from items on the Perceived Social Support-Friends scale and items reflect characteristics of health care provider relationships described by participants in our qualitative studies.
Family Environment(Protective Factor) included three measures that are central to family environment: adaptability and cohesion, communication, and family strengths 33 and one indicator of perceived social support from family.32 The Family Adaptability and Cohesion Scale II measures perceived adaptability and cohesion of family members. The Parent -Adolescent Communication scale measures adolescents’ views regarding their perceptions and experiences of communicating with each parent rated separately. The two subscales, Open Family Communication and Problems in Family Communication respectively measure positive and negative aspects of communications within a family. For this study, when the AYA completed forms for both father and mother, a total communication with parents scores were computed by averaging the mean scores from communication with the mother and the father. By combining the mean scores, important information was retained that would have otherwise been lost because of different family configurations (single versus dual parent households) and we were then able to examine combined parent influence. Family Strengths measures pride and loyalty (the individual’s perception of the family as a worthy group) and accord (attitudes relating to a family sense of mastery). Perceived Social Support - Family measures the extent to which individuals perceive their needs for support, information, and feedback are fulfilled by family.
Defensive Coping (Risk Factor) and Courageous Coping (Protective Factor)were measured by subscales of the Jalowiec Coping Scale-Revised, selected based on preliminary analysis of psychometric properties.34 Defensive coping was measured by emotive and evasive subscales. Courageous coping was measured by confrontive, optimistic, and supportant subscales. Although coping items are scored once for use and then for effectiveness, only the use scores were included in this analysis. Also, based on our previous work, we found that emotive coping captured the majority of the variance in defensive coping. However, in order to retain the qualitatively and theoretically derived meaning of defensive coping, a mean of the emotive and evasive subscales scores was used in this and subsequent analyses.
Derived Meaning (Protective Factor) included indicators of hope and spiritual perspective. The Herth Hope Index consists of three subscales: Temporality/Future, Positive Readiness, and Expectancy/Interconnectedness.35 Based on small loadings in our preliminary analyses to identify the best fitting measurement model, the Temporality/Future subscale was not included in the final exploratory measurement model used to test the full model. Spiritual Perspective was measured by the Reed Spiritual Perspective Scale which has two parts: frequency of spiritual practices/behaviors in the respondent’s life and spiritual beliefs.36
Outcomes in the final measurement model were measured by indicators of self-transcendence and resilience. The Reed Self-Transcendence Scale measures activities and perspectives individuals engage in to expand their boundaries. 37 This scale was originally developed for older adults and we dropped one item that decreased the Cronbach alpha coefficient in our preliminary analysis of psychometric properties. The item, “reflecting on the past,” is apparently not reflective of AYA experiences. The Resilience in Illness Scale was developed to reflect findings from the theme category titled “Resolution” in our qualitative study of courage in which resolution was characterized by a sense of mastery, competence, and accomplishment, as well as a feeling of growth having taken place and motivation to continue to maintain and improve the situation and help and inspire others. A feeling of acceptance is also evident as the individual acknowledges that the experience has contributed to whom and what he/she is.7
Although we initially included measures of self-esteem and confidence/mastery as indicators of resilience, these measures were not included in the final exploratory measurement model. Self-esteem was highly correlated with multiple indicators and had strong cross-loadings on multiple factors. The global measure of confidence competed with the context-specific Resilience in Illness scale to capture variance, so we opted to use only the more context specific Resilience in Illness measure in the final exploratory measurement model.
Analysis
Data analysis occurred in three phases: preliminary demographic and psychometric analysis, development of the measurement model, and test of the structural model.
Phase 1
In preliminary analysis, item and scale analyses were conducted using SPSS for Windows 11.5.2.1. Psychometric properties of reliability and validity of each of the scales and subscales were estimated for the sample. Sums and means were computed for scales that demonstrated adequate internal consistency reliability (Cronbach alpha coefficient >.70) and construct validity (exploratory and confirmatory factor analysis procedures). Descriptive statistics were then used to examine scores for each of the scales (e.g. range, mean, standard deviation, skewness, and kurtosis). Transformations to improve normal distribution curves were considered. Next, parametric statistics (e.g. t-test and ANOVA) were used to explore differences between subsets of the sample based on group membership for each of the variables (e.g., study [RIM 1 vs. RIM 2], age, sex, race, age at onset of diagnosis, time since diagnosis, and household income). Then, bivariate correlations were examined to obtain a preliminary sense of the nature and strength of relationships (Table 4). Finally, a covariance matrix was generated for use in the exploratory structural equation models.
Table 4.
Intercorrelations and Level of Significance among RIM manifest variables (n=189)
| Scale | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Symptom Distress | .36a | .03 | −.05 | .02 | −.06 | −.03 | −.05 | −.11 | −.15b | −.07 | −.13 | .20a | .02 | −.06 | .09 | −.20a | −.14 | −.28a | −.36a | −.13 | −.27a |
| 2. Uncertainty | −.06 | .01 | −.15b | −.13 | −.16b | −.21a | −.22a | −.23a | −.18b | −.26a | .37a | .02 | −.09 | .01 | −.39a | −.14a | −.45a | −.48a | −.32a | −.40a | |
| 3. Spirituality- Frequency | .78a | .21a | .27a | .19b | .23a | .26a | .08 | .13 | .18b | −.03 | .19a | .32a | .47a | .31a | .46a | .19b | .20a | .37a | .49a | ||
| 4. Spirituality- Belief | .28a | .29a | .28a | .28a | .30a | .12 | .23a | .23a | .03 | .26a | .33a | .40a | .37a | .48a | .20a | .25a | .49a | .47a | |||
| 5. Support-Provider | .57a | .54b | .28a | .29a | .12 | .23a | .22a | −.05 | .14 | .28a | .20a | .30a | .24a | .17b | .22a | .33a | .22a | ||||
| 6. Support-Friend | .59a | .30a | .34a | .14b | .22a | .19b | −.19a | .07 | .19a | .07 | .44a | .40a | .26a | .26a | .32a | .31a | |||||
| 7. Support-Family | .54a | .55a | .38a | .51a | .47a | −.17b | .03 | .21a | .08 | .40a | .41a | .33a | .33a | .42a | .18b | ||||||
| 8. Family Cohesion | .79a | .56a | .63a | .80a | −.26a | .07 | .16b | .16b | .33a | .48a | .27a | .37a | .40a | .30a | |||||||
| 9. Family Adaptability | .51a | .67a | .70a | −.21a | .08 | .21a | .16b | .36a | .52a | .33a | .46a | .46a | .38a | ||||||||
| 10. Family Communication- Problem | .45a | .60a | −.28a | .03 | .04 | .02 | .27a | .31a | .23a | .37a | .24a | .24a | |||||||||
| 11. Family Communication- Open | .61a | −.11 | .08 | .17b | .15b | .31a | .36a | .34a | .33a | .43a | .27a | ||||||||||
| 12. Family Strengths | −.23a | .04 | .13 | .10 | .32a | .47a | .27a | .39a | .34a | .30a | |||||||||||
| 13. Defensive Coping | .41a | .23a | .34a | −.19a | −.25a | −.20a | −.30a | −.07 | −.12 | ||||||||||||
| 14. Confrontive Coping | .59a | .53a | .16b | .17b | .25a | .10 | .31a | .31a | |||||||||||||
| 15. Optimistic Coping | .55a | .33a | .24a | .34a | .20a | .43a | .34a | ||||||||||||||
| 16. Supportant Coping | .18b | .26a | .08 | .04 | .30a | .40a | |||||||||||||||
| 17. Derived Meaning: Positive Readiness | .63a | .50a | .56a | .69a | .53a | ||||||||||||||||
| 18. Derived Meaning: Expect/Interconnected | .40a | .48a | .61a | .56a | |||||||||||||||||
| 19. Confidencec | .52a | .56a | .52a | ||||||||||||||||||
| 20. Self-Esteemc | .48a | .48a | |||||||||||||||||||
| 21. Resilience | .56a | ||||||||||||||||||||
| 22. Self-Transcendence | - | ||||||||||||||||||||
Correlation is significant at the 0.01 level (2-tailed).
Correlation is significant at the 0.05 level (2-tailed).
Measures not included in Best-Fit RIM Model.
Phase 2
For both phase 2 and phase 3, measurement and full structural model testing was done using the EQS 6.1 for Windows program.38 Maximum likelihood estimation was performed on the covariance matrix from subjects for whom complete data were obtained on relevant variables (n=189); this was 94% of the participants in the combined RIM1 and RIM2 sample. Subjects excluded from the analysis due to missing data were similar to those included with regard to health and demographic characteristics.
Confirmatory factor analysis was done to estimate the goodness-of-fit of the hypothesized indicators in the measurement model. With all parameters appearing in order and no special problems encountered during optimization, the chi-square test (criteria chi-square > .05 indicating the model does not significantly differ from the data) and measures for goodness-of-fit (values between .95 and 1.0 indicating an acceptable fit) were reviewed, e.g., the Non-Normed Fit Index (NNFI); the Comparative Fit Index (CFI); and the Bollen Fit Index (IFI). 39,40 These goodness-of-fit indices are estimates of the proportion of information in the covariance matrix that is explained by the model. These indices all range from 0 to 1, with values .95 or above indicating good fit.41 Another fit index, the Root-Mean-Square Error of Approximation (RMSEA), is a value that ideally should be <.05.42
Next, the number of iterations for convergence and largest standardized residuals were considered. The critical ratio levels (z-score > 1.96) indicating the level of significance (p < .05) of the factor loadings for each of the indicators, the variances of the independent factors and error terms, and correlations between each of the factors were reviewed. The Wald test for dropping parameters and the Lagrange Multiplier test for adding parameters were considered. The path loading from the unique error term and the path loading from the factor to the specified indicator were placed in the best fitting measurement model.
Phase 3
The best fitting measurement model was then used to examine the hypothesized structural model. Paths loadings and disturbance (error) terms were specified for each latent variable in the structural model and examined iteratively using the same procedures and criteria described above for the measurement model. The path loadings and amount of variance explained (R2) are reported in the standardized solution. These values were then placed in the best fitting structural model.
Evaluation of model fit
Because the chi-square goodness-of-fit test, under adequate sample sizes, has sufficient power to detect minor unimportant deviations from good fit, we like many SEM practitioners place much greater importance on the fit indices (which serve as effect sizes) than on the p-value from the chi-square goodness of fit due to the influence of sample size on the p-value.
RESULTS
Sample Characteristics
In the combined sample (N=202) (Table 2), ages of the participants ranged from 10 (within 6 months of turning 11) to 26 years (M=15.83, SD=2.70). Age at time of diagnosis ranged from less than one month to 21 years (M=12.11, SD=4.58). Time from diagnosis to data collection ranged from less than one month to 18 years (M=3.76, SD=4.60). Preliminary analysis revealed that none of the 20 variables in the final (best fitting) SEM model differed by sex, race, current age, or household income. The only Bonferroni-adjusted significant (.05 alpha/140 comparisons = .000357) differences on any of the 20 variables were between perceived social support and the study group, age at diagnosis, and time since diagnosis subgroups. These statistically significant magnitudes of differences were small and clinically unimportant, and were therefore not included in the measurement or structural models; nor was the SEM model estimated by subgroups, given the lack of differences by subgroups.
Measurement and Full Model Evaluation
The measurement model was estimated with the proposed indicators to assess the measurement of the constructs and the strengths of the associations among them. Results are shown in Figure 2. We decided to allow one indicator, family support, to load on more than one latent variable since theory supported cross-loading of perceived social support from family on both social integration and family environment. Each indicator was found to load significantly on its construct (p < .0001). All measures had strong loadings. Modification indices did not suggest any meaningful changes that would improve the fit. Both the Bentler-Bonnett Non-normed Fit Index and Comparative Fit Index for the measurement model were .95 and the Bollen Fit Index was .96, indicating a good fit. These findings indicated that the measurement model fit well with the data, although the chi-square test could be statistically rejected as a perfect fit (χ2 = (df = 142, n = 189) = 233.09, p < .00).
Having established a well-fitting measurement model, the structural model was then estimated. When the structural model was tested as hypothesized, the chi-square test indicated that the path model could be rejected as a perfect fit with fit indices that indicated only marginally good fit. In a series of sequential runs using Wald and Lagrange tests, five hypothesized paths were systematically dropped. In efforts to improve the fit between the covariance structure of the data and the model, the outcome variable resilience was separated into two manifest variables, self-transcendence and resilience. Derived meaning was similarly separated into spiritual perspective and hope-derived meaning. Again using theory to guide decision-making, five corresponding paths were systematically added. Results of the final, best fitting exploratory model are displayed in Figure 3.
Figure 3.
Final Exploratory RIM Structural Model
For the structural model, the Bentler-Bonnett Non-normed Fit Index was .95 and the Comparative Fit Index and Bollen Fit Index were .96, indicating the model is a reasonable approximation to the data, although the chi-square test indicated that the path model could be statistically rejected as a perfect fit (χ2 = (df = 152, n = 189) = 234.53, p < .00.). The RMSEA was < .05. All the paths in the model were statistically significant at p < .05, except the path from family functioning to courageous coping, which did not reach significance (p = .21). The coefficients of all paths had the predicted signs.
DISCUSSION
Based on meeting all the criteria for goodness-of-fit of the several indices, the final exploratory model was a reasonable approximation (although not perfect) to the data and explained a high level of the variance for the separate distal outcomes of resilience (67%) and self-transcendence (63%). These results supported our moving forward with a confirmatory evaluation of the RIM that is described in Part 2 of this paper. Variance explained for proximal RIM outcomes was also high: 52% of courageous coping and 76% of hope-derived meaning. Thus, the findings suggest that confirmation of the best-fitting RIM may provide a valid basis for understanding about the resilience process and specifying potential target variables for interventions. There were some changes in paths and indicators of latent variables from the hypothesized RIM; as a result, the best fitting exploratory model does not accurately reflect the definition of resilience proposed by Haase (2009) and used in this study. Based on results of the confirmatory measurement and full models, the definition of resilience may need to be revised to more clearly distinguish between resilience as process and resilience resolution as outcome. In the following sections, we discuss the findings for each factor in the RIM measurement model and each factor and path in the RIM structural model, starting with distal outcomes on the right in Figure 3 and progressing to independent variables on the left. We also discuss study limitations.
Implications of Findings for Each RIM Factor
Resilience and Self-Transcendence
Although our preliminary qualitative work indicated that self-esteem and confidence/mastery were indicators of resilience, neither self-esteem or confidence/mastery measures fit well as indicators in the best fitting exploratory RIM measurement model. Self-esteem measures are generally global, and may not be sensitive enough to differentiate context-specific self-esteem (e.g. pride in how well one has navigated the cancer journey) that AYA described in our qualitative studies. 7,29 Our confidence/mastery measure was also global. Thus, we elected to use only the context specific resilience measure in our test of the full model. Further study is recommended on the sensitivity of global versus context-specific measures.
In the best-fitting exploratory structural model, the hypothesized resilience latent variable was separated into two variables, resilience and self-transcendence. It is plausible that resilience and self-transcendence play different roles as outcomes. The results indicate that, whereas courageous coping contributes to both resilience and self-transcendence, self-transcendence is strongly related to illness-related distress and resilience is related to hope-derived meaning. The direct path from illness-related distress to resilience was picked up by self-transcendence, again suggesting that, when illness-related distress is severe or not adequately clinically managed, it may be more difficult to transcend the treatment and symptom-related concerns.
Four hypothesized paths to resilience —those from defensive coping, social integration, illness-related distress, and family environment —were dropped in the final structural model. This was possibly due to the strong mediating effects of courageous coping. These findings support much of the literature on coping indicating that strategies that are positive, such as confrontive, optimistic and supportant, enhance positive outcomes.43
Hope-derived Meaning
In the final structural model, the latent variable initially labeled derived meaning was separated into two variables, hope-derived meaning and spiritual perspective. Seventy-six percent of the variance in hope-derived meaning was directly accounted for by illness-related distress, spiritual perspective, social integration, and family environment. The significant paths from social integration and family environment are consistent with findings from our qualitative studies. For example, participants told us of specific ways that family, health care providers and friends fostered hope.7,29
We did not hypothesize a direct path from illness-related distress to hope. The literature on hope is also unclear about the relationship of illness-related distress and derived meaning. Further study is warranted to determine the patterns of hope-fostering mechanisms. The paths from social integration and family environment support our qualitative research studies findings, whereby participants in several studies told us of specific ways that family, health care providers and friends fostered hope, such as re-assuring them of their own hope for positive outcomes and praying for them.7,29
Positive and Courageous Coping
Fifty-two percent of the variance in courageous coping was explained in the final exploratory RIM. The hypothesized path from social integration to courageous coping was dropped and the illness-related distress path was added. The hypothesized path from defensive coping was supported in a positive direction with defensive coping serving as a mediator between illness-related distress and courageous coping. The final model supports previous research that indicated defensive ways of coping are necessary strategies used for protection of self in threatening situations.43
Family Environment
The five indicators of family environment focused primarily on within-family components (cohesiveness, adaptability, communication patterns, perceived family strengths, and family support). Although 27% of variance was accounted for by these within-family components, more work needs to be done to explore the external-family resources that support the family as they support the AYA with cancer. In addition, the hypothesized path from family environment to courageous coping did not rise to the level of significance. Family members may not know how to provide support for courageous coping in the context of a new and stressful situation they are all facing, and further exploration of patterns of family support over time is warranted. Research indicates that families struggle with communication around the experiences of cancer and this is likely to be particularly difficult for AYA and their family members. Family communication refers to family members’ ability to communicate openly and clearly with one another, especially with regard to stressful issues (e.g., prognosis). Effective ways of communicating with adolescents/young adults is key to their psychological well-being.44
Social Integration
Indicators of social integration—perceived social support from health care providers and friends—explained 18% of variance in the final exploratory RIM. These findings support previous research indicating perceived social support reduces symptom distress.22,45 Other research also indicates that adolescents/young adults with cancer who have strong social supports also have greater courageous coping and family cohesion and are better able to adapt to the cancer experience and resume “normal” lives.21
Illness-related Distress
In the final exploratory RIM, illness-related distress, consisting of symptom distress and uncertainty in illness, was significantly and positively related to defensive coping and negatively related to social integration, derived meaning, family environment, and transcendence. These findings indicate that illness-related distress is central to the process of adjustment to cancer in terms of resilience and transcendence. High uncertainty in cancer has been consistently linked to negative psychosocial outcomes, including poor family relationships, psychological distress, anxiety, impaired sense of mastery, and lowered quality of life.25,31,46
Spiritual Perspective
We had originally hypothesized in the measurement model that spiritual perspective, consisting of beliefs and practices, was an indicator of derived meaning; however, we were not able to achieve a good-fitting model with spiritual perspective as part of derived meaning. We then examined two alternative models, one with and one without spiritual perspective as an independent variable. Both models had acceptable fit indices; however the model that included spiritual perspective as an independent variable was slightly better and explained more variance. In the final RIM, spiritual perspective had significant direct positive relationships with social integration, family environment, courageous coping, hope-derived meaning, and self-transcendence and an indirect relationship with resilience. These findings support other literature indicating that spirituality is increasingly recognized as an important aspect of holistic care for cancer patients; it is consistently positively related to courageous coping and quality of life.47
Study Limitations
There are several limitations to this exploratory model test of the RIM. The test of the model was based on combined data from two samples. These studies were completed in 1999 and 2004. While these data sets may not be reflective of current AYA experiences with cancer, it is likely that the magnitude of relationships, rather than the processes themselves would differ. The cross-sectional nature of the data is a limitation, in that the hypothesized relationships may not hold across time. Although longitudinal data were obtained from the RIM 2 study, we did not have an adequate sample size to examine the model with this group separately or over time. The combined sample from RIM 1 and RIM 2 was heterogeneous in terms of types of cancer, age at diagnosis, and time since diagnosis; a heterogeneous sample may be beneficial in initial stages of theory testing, to reduce the risk of bias and increase generalizability.48 We report information on several demographic variables to provide the reader with additional sample information.
All measures used were paper-and-pencil self-report scales. Self-report measures contain inherent limitations, including distortion in recall, lack of objectivity, and social desirability.48 However, self-report measures have value and are of interest in conveying perceptions of experiences. The normal distribution patterns of the measures indicate that social desirability was not a concern. The literature also indicates there is concern about the truthfulness of responses provided by AYA self-reports.49 In our previous studies and the RIM-related studies reported here, adolescents/young adults indicated they appreciated the opportunity to participate as indicated by offers to forego the monetary incentive, thank-you notes for the opportunity to think about some of their experiences, and pictures drawn on return envelopes. This apparent high level of engagement in the study may be attributed to links of the model and measures to the experiences of AYA derived from the model generating studies.
Implications
Much of the research currently conducted with AYA focuses on medical concerns; we have limited understanding of the role that positive health- and strengths-based perspectives contribute to AYA outcomes. More research is needed to fully understand and enhance positive health in AYA. We have previously published on the multiple ways RIM might be used to guide positive health research.5 The following examples focus on positive health: within social integration, we recommend research on ways AYA connect with healthcare providers and interventions to improve AYA/provider communication; within family environment, we recommend interventions to improve family communication as a way to support AYA; and, given the highly significant contributions of spiritual perspective to positive health outcomes, much work is needed to describe and support AYA as they clarify their spiritual perspectives in the context of illness.
Based on this exploratory RIM, it is clear that illness-related distress needs to be addressed in order improve outcomes. A pathology approach focuses primarily on symptom management. However, physical symptoms are only one of many contributors to illness-related distress. Interventions for uncertainty management for adults have been developed and tested and could be adapted and evaluated for AYA with cancer.46,50
In summary, in this study we explored the fit of the Resilience in Illness Model to data obtained from AYA with cancer. The model fit well with the data and supported most hypothesized latent variables and paths. The revised model explained a large amount of variance (.63-.76) in outcome variables of resilience and self-transcendence, and in the mediating variable of hope-derived meaning. Small to moderate amounts of variance (.18 -.52) were explained for the mediating variables of defensive coping, family environment, and social integration. Part 2 of this paper describes results of a confirmatory test of the model in AYA undergoing stem cell transplant for cancer and discusses implications for clinical practice.
Acknowledgments
Grant Sponsor: National Institutes of Health/National Institute of Nursing Research NIH/NINR 1R29 NR03882, Resilience and Quality of Life in Adolescents with Cancer
Walther Cancer Institute, Indianapolis, IN, Factors Affecting Quality of Life Outcomes for Adolescents with Cancer
Footnotes
It should be noted that a second outcome variable, quality of life, defined as sense of well-being, included in previously published papers on the RIM, was omitted in this evaluation of the RIM due to inadequate sample size to accommodate this additional distal variable.
The authors have no conflicts of interest to disclose.
References
- 1.Singer B, Ryff CD. New horizons in health: An integrative approach. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 2.Masten AS. Resilience in developing systems: progress and promise as the fourth wave rises. Dev Psychopathol. 2007 Summer;19(3):921–930. doi: 10.1017/S0954579407000442. [DOI] [PubMed] [Google Scholar]
- 3.Cicchetti D, Blender JA. A multiple-levels-of-analysis perspective on resilience: implications for the developing brain, neural plasticity, and preventive interventions. Ann N Y Acad Sci. 2006 Dec;1094:248–258. doi: 10.1196/annals.1376.029. [DOI] [PubMed] [Google Scholar]
- 4.McAllister M, McKinnon J. The importance of teaching and learning resilience in the health disciplines: a critical review of the literature. Nurse Educ Today. 2009 May;29(4):371–379. doi: 10.1016/j.nedt.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 5.Haase JE. The adolescent resilience model as a guide to interventions. Journal of pediatric oncology nursing: official journal of the Association of Pediatric Oncology Nurses. 2004 Sep-Oct;21(5):289–299. doi: 10.1177/1043454204267922. discussion 300-284. [DOI] [PubMed] [Google Scholar]
- 6.Haase J. Resilience. In: Bredlow P, editor. Middle Range Theories: Application to Nursing Research. Philadelphia: Lippincott; 2004. pp. 341–367. [Google Scholar]
- 7.Haase JE. Components of courage in chronically ill adolescents: a phenomenological study. ANS Adv Nurs Sci. 1987 Jan;9(2):64–80. doi: 10.1097/00012272-198701000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Haase JE, Britt T, Coward DD, Leidy NK, Penn PE. Simultaneous concept analysis of spiritual perspective, hope, acceptance and self-transcendence. Image J Nurs Sch. 1992 Summer;24(2):141–147. doi: 10.1111/j.1547-5069.1992.tb00239.x. [DOI] [PubMed] [Google Scholar]
- 9.Haase JE, Heiney SP, Ruccione KS, Stutzer C. Research triangulation to derive meaning-based quality-of-life theory: Adolescent resilience model and instrument development. Int J Cancer Suppl. 1999;12:125–131. doi: 10.1002/(sici)1097-0215(1999)83:12+<125::aid-ijc22>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 10.Institute NC. [Accessed October 30, 2012];Adolescents and Young Adults with Cancer. http://www.cancer.gov/cancertopics/aya.
- 11.Docherty SL. Symptom experiences of children and adolescents with cancer. Annual Review of Nursing Research. 2003;21:123–149. [PubMed] [Google Scholar]
- 12.Stegenga K, Ward-Smith P. On receiving the diagnosis of cancer: the adolescent perspective. Journal of Pediatric Oncology Nursing. 2009 Mar-Apr;26(2):75–80. doi: 10.1177/1043454208328767. [DOI] [PubMed] [Google Scholar]
- 13.Stewart JL, Mishel MH, Lynn MR, Terhorst L. Test of a conceptual model of uncertainty in children and adolescents with cancer. Research in Nursing & Health. 2010 Jun;33(3):179–191. doi: 10.1002/nur.20374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wicks L, Mitchell A. The adolescent cancer experience: loss of control and benefit finding. Eur J Cancer Care (Engl) 2010 Nov;19(6):778–785. doi: 10.1111/j.1365-2354.2009.01139.x. [DOI] [PubMed] [Google Scholar]
- 15.Sundberg KK, Lampic C, Bjork O, Arvidson J, Wettergren L. Positive and negative consequences of childhood cancer influencing the lives of young adults. Eur J Oncol Nurs. 2009 Jul;13(3):164–170. doi: 10.1016/j.ejon.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 16.Thompson K, Palmer S, Dyson G. Adolescents & young adults: issues in transition from active therapy into follow-up care. Eur J Oncol Nurs. 2009 Jul;13(3):207–212. doi: 10.1016/j.ejon.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 17.Hudson MM, Mertens AC, Yasui Y, et al. Health status of adult long-term survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Jama. 2003 Sep 24;290(12):1583–1592. doi: 10.1001/jama.290.12.1583. [DOI] [PubMed] [Google Scholar]
- 18.Spinetta JJ, Masera G, Eden T, et al. Refusal, non-compliance, and abandonment of treatment in children and adolescents with cancer: a report of the SIOP Working Committee on Phychosocial Issues in Pediatric Oncology. Med Pediatr Oncol. 2002 Feb;38(2):114–117. doi: 10.1002/mpo.1283. [DOI] [PubMed] [Google Scholar]
- 19.Hinds PS. Shifting perspectives: adolescent-focused oncology nursing research. Oncology Nursing Forum. 2004 Mar-Apr;31(2):281–287. doi: 10.1188/04.ONF.281-287. [DOI] [PubMed] [Google Scholar]
- 20.Corey AL, Haase JE, Azzouz F, Monahan PO. Social support and symptom distress in adolescents/young adults with cancer. J Pediatr Oncol Nurs. 2008 Sep-Oct;25(5):275–284. doi: 10.1177/1043454208321117. [DOI] [PubMed] [Google Scholar]
- 21.Trask PC, Paterson AG, Trask CL, Bares CB, Birt J, Maan C. Parent and adolescent adjustment to pediatric cancer: associations with coping, social support, and family function. J Pediatr Oncol Nurs. 2003 Jan-Feb;20(1):36–47. doi: 10.1053/jpon.2003.5. [DOI] [PubMed] [Google Scholar]
- 22.Woodgate RL. The importance of being there: perspectives of social support by adolescents with cancer. Journal of pediatric oncology nursing: official journal of the Association of Pediatric Oncology Nurses. 2006 May-Jun;23(3):122–134. doi: 10.1177/1043454206287396. [DOI] [PubMed] [Google Scholar]
- 23.Ritchie MA. Sources of emotional support for adolescents with cancer. Journal of Pediatric Oncology Nursing. 2001 May-Jun;18(3):105–110. doi: 10.1177/104345420101800303. [DOI] [PubMed] [Google Scholar]
- 24.Hinds PS. Fostering coping by adolescents with newly diagnosed cancer. Seminars in Oncology Nursing. 2000 Nov;16(4):317–327. doi: 10.1053/sonu.2000.16590. discussion 328–336. [DOI] [PubMed] [Google Scholar]
- 25.Zebrack BJ, Chesler MA. Quality of life in childhood cancer survivors. Psycho-Oncology. 2002 Mar-Apr;11(2):132–141. doi: 10.1002/pon.569. [DOI] [PubMed] [Google Scholar]
- 26.Hultsch D, Deutsch F. Adult development and aging: A life-span perspecctive. New York: McGraw-Hill; 1981. [Google Scholar]
- 27.Weekes DP. Application of the life-span developmental perspective to nursing research with adolescents. Journal of Pediatric Nursing. 1991 Feb;6(1):38–48. [PubMed] [Google Scholar]
- 28.Costain K, Hewison J, Howes M. Comparison of function-based model and a meaning-based model of quality of life in oncology: Multidimensionality examined. Journal of Psychosocial Oncology. 1993;11(4):17–37. [Google Scholar]
- 29.Haase JE, Rostad M. Experiences of completing cancer therapy: children’s perspectives. Oncol Nurs Forum. 1994 Oct;21(9):1483–1492. discussion 1493-1484. [PubMed] [Google Scholar]
- 30.McCorkle R. The measurement of symptom distress. Seminars in Oncology Nursing. 1987 Nov;3(4):248–256. doi: 10.1016/s0749-2081(87)80015-3. [DOI] [PubMed] [Google Scholar]
- 31.Mishel MH. Reconceptualization of the uncertainty in illness theory. Image J Nurs Sch. 1990 Winter;22(4):256–262. doi: 10.1111/j.1547-5069.1990.tb00225.x. [DOI] [PubMed] [Google Scholar]
- 32.Procidano ME, Heller K. Measures of perceived social support from friends and from family: three validation studies. Am J Community Psychol. 1983 Feb;11(1):1–24. doi: 10.1007/BF00898416. [DOI] [PubMed] [Google Scholar]
- 33.Olson Dea. Family inventories. St. Paul, MN: Family Social Science, University of Minnesota; 1985. [Google Scholar]
- 34.Jalowiec A, Murphy SP, Powers MJ. Psychometric assessment of the Jalowiec Coping Scale. Nursing research. 1984 May-Jun;33(3):157–161. [PubMed] [Google Scholar]
- 35.Herth K. Development and refinement of an instrument to measure hope. Sch Inq Nurs Pract. 1991 Spring;5(1):39–51. discussion 53-36. [PubMed] [Google Scholar]
- 36.Reed P. Spirituality and well-being in terminally ill and healthy adults. Research in Nursing & Health. 1986;9:35–42. doi: 10.1002/nur.4770090107. [DOI] [PubMed] [Google Scholar]
- 37.Reed PG. Mental health of older adults. Western journal of nursing research. 1989 Apr;11(2):143–157. doi: 10.1177/019394598901100202. discussion 158–163. [DOI] [PubMed] [Google Scholar]
- 38.Bentler P. EQS Structural Equations Program Manual. Encino, CA: Multivariate Software, Inc; 1995. [Google Scholar]
- 39.Bollen KA. Structural equations with latent variables. New York: John Wiley & Sons; 1989. [Google Scholar]
- 40.Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990 Mar;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 41.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Convential criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- 42.Byrne BM. Structural equation modeling with AMOS: Basic concepts, applications, and programming. Mahwah, NJ: Erlbaum; 2001. [Google Scholar]
- 43.Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: problems, progress, and potential in theory and research. Psychological Bulletin. 2001;127(1):87–127. [PubMed] [Google Scholar]
- 44.Zebrack B, Chesler MA, Kaplan S. To foster healing among adolescents and young adults with cancer: What helps? What hurts? Supportive Cancer Care. 2010;18(1):131–135. doi: 10.1007/s00520-009-0719-y. [DOI] [PubMed] [Google Scholar]
- 45.Enskar K, Carlsson M, Golsater M, Hamrin E, Kreuger A. Life situation and problems as reported by children with cancer and their parents. Journal of pediatric oncology nursing: official journal of the Association of Pediatric Oncology Nurses. 1997 Jan;14(1):18–26. doi: 10.1177/104345429701400104. [DOI] [PubMed] [Google Scholar]
- 46.Mishel MH, Germino BB, Gil KM, et al. Benefits from an uncertainty management intervention for African-American and Caucasian older long-term breast cancer survivors. Psycho-Oncology. 2005 Nov;14(11):962–978. doi: 10.1002/pon.909. [DOI] [PubMed] [Google Scholar]
- 47.Hendricks-Ferguson V. Hope and spiritual well-being in adolescents with cancer. Western journal of nursing research. 2008 Apr;30(3):385–401. doi: 10.1177/0193945907303045. discussion 402-387. [DOI] [PubMed] [Google Scholar]
- 48.Burns N, Grove SK. The Practice of Nursing Research: Appraisal, Synthesis, and Generation of Evidence. 6. St. Louis, MO: Saunders; 2008. [Google Scholar]
- 49.Hinds PS, Gattuso JS. Measuring hopefulness in adolescents. Journal of pediatric oncology nursing: official journal of the Association of Pediatric Oncology Nurses. 1991 Apr;8(2):92–94. doi: 10.1177/104345429100800241. [DOI] [PubMed] [Google Scholar]
- 50.Lee YL, Gau BS, Hsu WM, Chang HH. A model linking uncertainty, post-traumatic stress, and health behaviors in childhood cancer survivors. Oncology Nursing Forum. 2009 Jan;36(1):E20–30. doi: 10.1188/09.ONF.E20-E30. [DOI] [PubMed] [Google Scholar]